Gastrointestinal Physiology: Liver and Bile
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
83 Terms
Describe the blood supply of the liver
dual blood supply = 25% of cardiac output
-portal vein --> carries the blood from the entire capillary system of the stomach, spleen, pancreas, & intestine (75% of liver's blood supply)
-hepatic artery --> 25% of the liver's blood supply
What is the function of the the portal vein?
carries the blood from the entire capillary system of the stomach, spleen, pancreas, & intestine
*75% of liver's blood supply
Why is the liver known as the gatekeeper of the GI?
nutrients absorbed by the GI pass thru the liver via the portal vein prior to entering general circulation ==> enables the liver to regulate & maintain viable levels of nutrients in the blood in spite of variations in dietary intake & feeding frequency --> keeps substances in the blood within homeostatic limits
What are the primary functions of the liver?
-bile production & excretion
-excretion of bilirubin, cholesterol, hormones, & drugs
-metabolism of fats, proteins, & carbohydrates
-enzyme activation
-storage of glycogen, vitamins, & minerals
-synthesis of plasma proteins --> albumin & clotting factors
-blood detox & purification
Liver disease can increase the risk of hemorrhaging. Why?
b/c the liver synthesizes clotting factors
What are the major organic compound within bile?
-bile acids--> cholic acid & chenodeoxycholic acid
-phospholipids --> lecithins
-cholesterol
-bile pigments --> bilirubin
bilirubin
bile pigment that's a product of hemoglobin breakdown
*not produced by the liver --> produced in the spleen & processed in the liver
Name some important substances that the liver stores.
-glucose --> stored as glycogen
-fat-soluble vitamins--> A, D, E, K, folate, B12
-minerals --> iron, copper
Why is vitamin B12 stored in the liver at greater amounts than any other vitamin?
b/c vitamin B12 is needed for synthesis of RBC
Why does it usually take years before vitamin B12 deficiency becomes apparent?
b/c the liver stores B12 at high levels --> body fxns for years until storage is depleted
What's the world's most common cause of anemia?
iron deficiency
Where does iron absorption occur predominantly?
duodenum & upper jejunum
True or False: The liver stores enough iron as ferritin to last for 2-3 years.
True
What are some dietary sources of iron?
-meat
-legumes
-iron-fortified grains
True or False: Any changes in the function of the duodenum or how food passes through it can effect iron uptake.
True
True or False: The liver synthesizes all 20 amino acids required for protein, hormone, & neurotransmitters
False ==> only synthesizes 11 of the 20 AAs, the other 9 need to be obtained thru diet (essential AAs)
What organ produces circulating plasma proteins like albumin & clotting factors?
liver
True or False: Immunoglobulins are produced in the liver
False ==> produced by plasma cells (mature B cells)
Where is hemoglobin produced?
bone marrow
What is the most abundant protein in plasma?
albumin
What is the role of albumin?
plasma protein that
-maintains oncotic pressure
-transports steroids & other hormones
Where is ammonia produced?
-small intestine --> due to amino acid breakdown
-large intestine --> caused by bacterial breakdown of amino acids & urea
*produced in equal amounts by small and large intestine
True or False: The small intestine produces ammonia in greater amounts
False==> produced in equal amounts in both the small & large intestine
Why is the regulation of ammonia via the urea cycle an important function of the liver?
b/c ammonia is a neurotoxin ==> elevated levels of circulating ammonia (hyperammonemia) can result in serious consequences to CNS & death
*liver is the only organ that has the urea cycle, so it's the only organ that can metabolize NH3 to urea for excretion
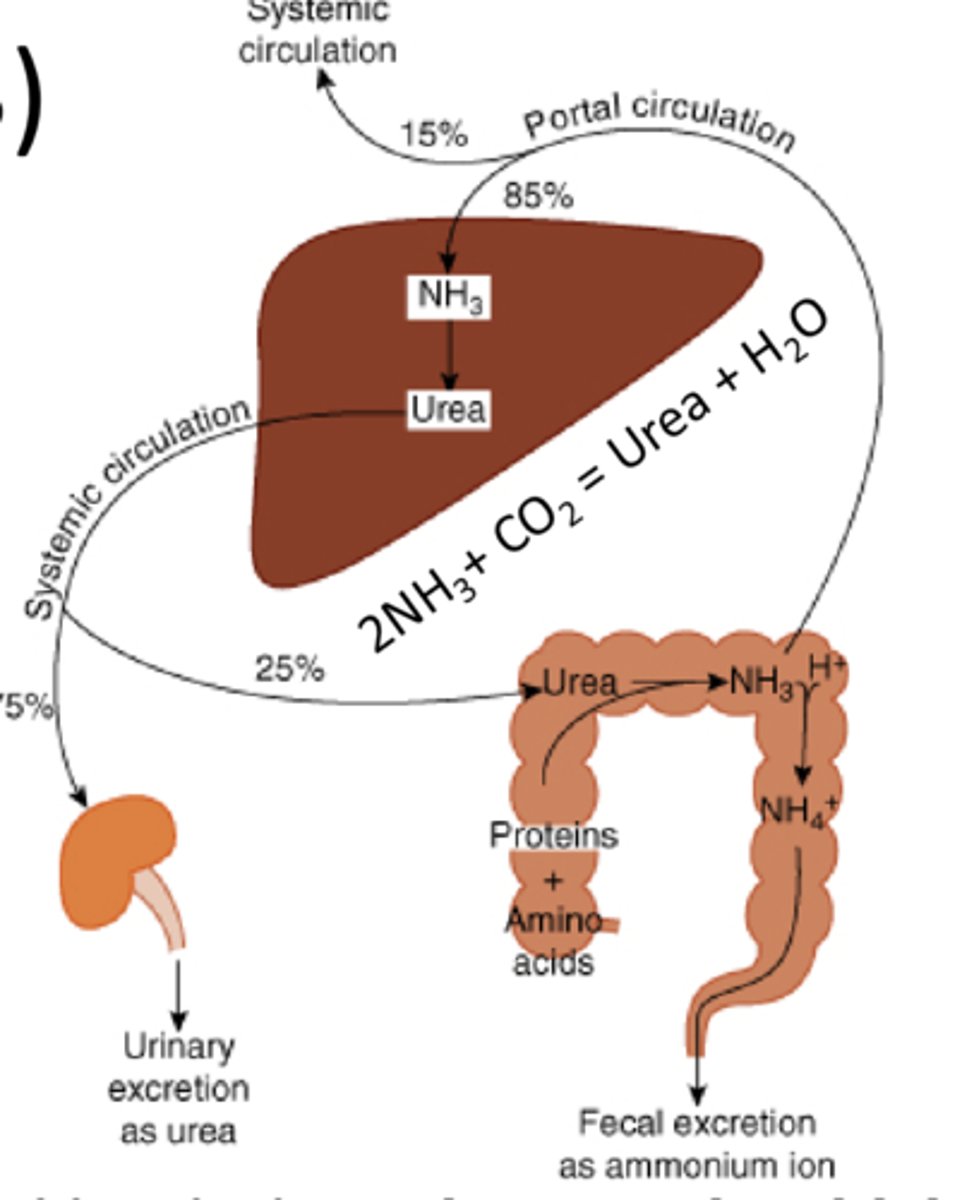
How does hyperammonemia affect the CNS?
disrupts that metabolism & fxn of astrocytes (protective glial cells)
glycogen
stable storage form of glucose found in the liver and muscle tissue
glycogenesis
storage of glucose as glycogen in liver & muscle
glycogenolysis
liver breaks down stored glycogen to maintain blood glucose levels
gluconeogenesis
liver synthesizes glucose from proteins and fats to maintain blood glucose levels.
Where are the majority of lipoproteins synthesized?
liver
True or False: The liver converts excess carbohydrates and proteins into fatty acids & triglycerides
True
True or False: The liver synthesizes large quantities of cholesterol & phospholipids.
True
-some of cholesterol & phospholipids are packaged and made available to the rest of the body
-some excreted in bile as cholesterol or converted to bile acids
How does the liver regulate the levels of circulating compounds?
eliminates hormones, vitamins, inflammatory molecules, signaling compounds, & etc by the same enzymatic detoxification systems that protect the body from environmental toxins, or clear drugs from circulation
Why do females with liver disease typically develop spider-like angiomas on their skin?
spider-like angiomas due to increased serum estrogen levels ==> liver typically regulates serum estrogen levels so estrogen levels are dysregulated during liver disease

How are drugs, hormones, toxins, etc removed/inactivated?
as blood from the GI organs passes thru the hepatic portal circulation, hepatocytes monitor the contents of the blood & removes or modifies many potentially toxic substances
*enzymes in hepatocytes metabolize many of these toxins/hormones/drugs to their inactive metabolites --> breakdown or transformation into less harmful compounds --> excreted into the bile or circulation --> removed from the body in stool via bile or in urine via the kidneys
first-pass effect
hepatic metabolism of a pharmacological agent when it's absorbed from the gut & delivered to the gut via portal circulation
*the greater the 1st pass effect, the less of the agent will reach the systemic circulation when the agent is administered orally
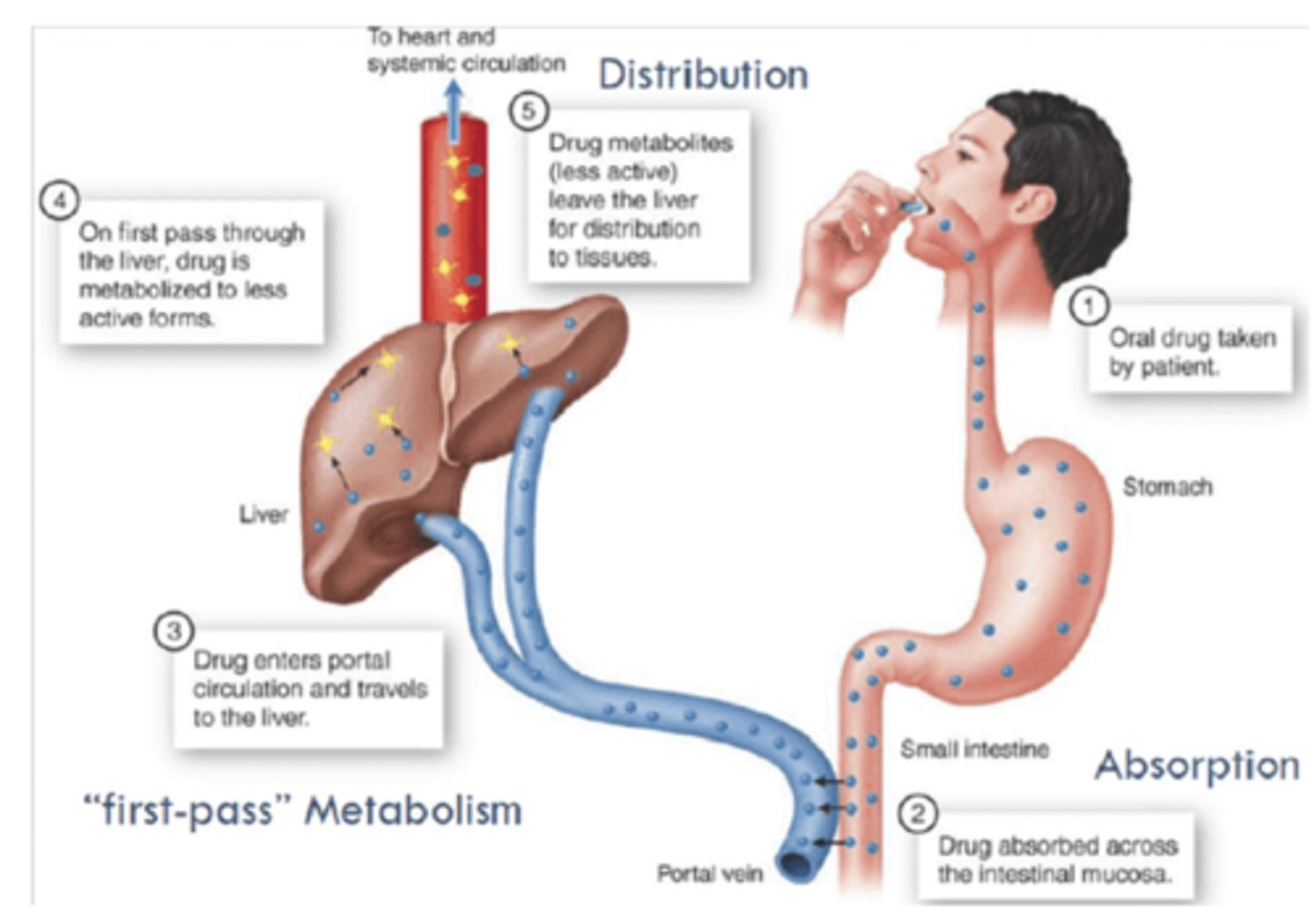
True or False: Drugs given intravenously encounter the first pass effect so less of it will make it to systemic circulation
False ==> IV drugs avoid first pass (all administered makes it to systemic administration) and have direct access to the body
True or False: Typically if a drug is administered orally , a lower concentration than the concentration administered makes it to systemic circulation.
True ==> drugs given orally encounter first-pass effect where drug metabolism can occur
How should the dosage of a orally administered drug be adjusted for a patient with liver disease?
dosage should be decreased b/c liver won't be able to metabolize some of it for excretion = increased conc of drug in blood = increased potential for toxicity
Would you expect to see an increased or decreased serum concentration of an oral administered drug in liver disease patients?
increased ==> first pass system decreased b/c liver fxn is decreased
Why are drugs typically lipophilic?
so they can pass plasma membranes of cells & reach the site of action
How is a drug typically metabolized?
liver enzymes introduce hydrophilic functionalities onto the drug molecule to make them less lipophilic & facilitate their excretion from the body
*Undergo Phase I & Phase II rxns before excretion
-phase I --> add a fxnal group to make it more hydrophilic
-phase II --> conjugate to compound that makes it more susceptible to excretion
Phase I Metabolism of Drugs
reaction that introduces a fxnal group to a drug/toxin/hormone or exposes a fxnal group to make the compound more hydrophilic
*makes compound more susceptible to excretion
Phase II Metabolism of Drugs
reaction that conjugates glucoronic acid, sulfonates, glutathione, or amino acids to the drug/toxin/hormone
*makes the compound more susceptible to excretion
What is the role of efflux cell membrane transporters in drug metabolism/excretion?
move the parent drug & metabolites of some drugs out of the cell
*contributes to drug resistance by diminishing the desired therapeutic or biologic effect
Where are most of the component that make up bile synthesized?
liver
How is the majority of bilirubin produced?
degradation of hemoglobin from erythrocytes undergoing normal senescence (approx 250 million turnover each day)
Why is high bilirubin levels more common in newborns?
b/c it takes so time afterbirth for an infant to start efficiently metabolizing bilirubin and excreting it in their stool
Describe how bilirubin is excreted.
extravascular or intravascular hemolysis (breakdown of RBC) --> unconjugated bilirubin in blood -->>> enters hepatic sinusoid --> enters hepatocyte--> conjugated to glucaronic acid -->excreted in bile --> enter small intestine --> converted into urobilinogen via bacterial proteases --> 90% eliminated in feces + 10% enters portal system --> enters hepatocyte --> reabsorbed into blood --> travels to kidneys --> excreted in urine
*urobilinogen is the reason for the color of pee pee & boo boo
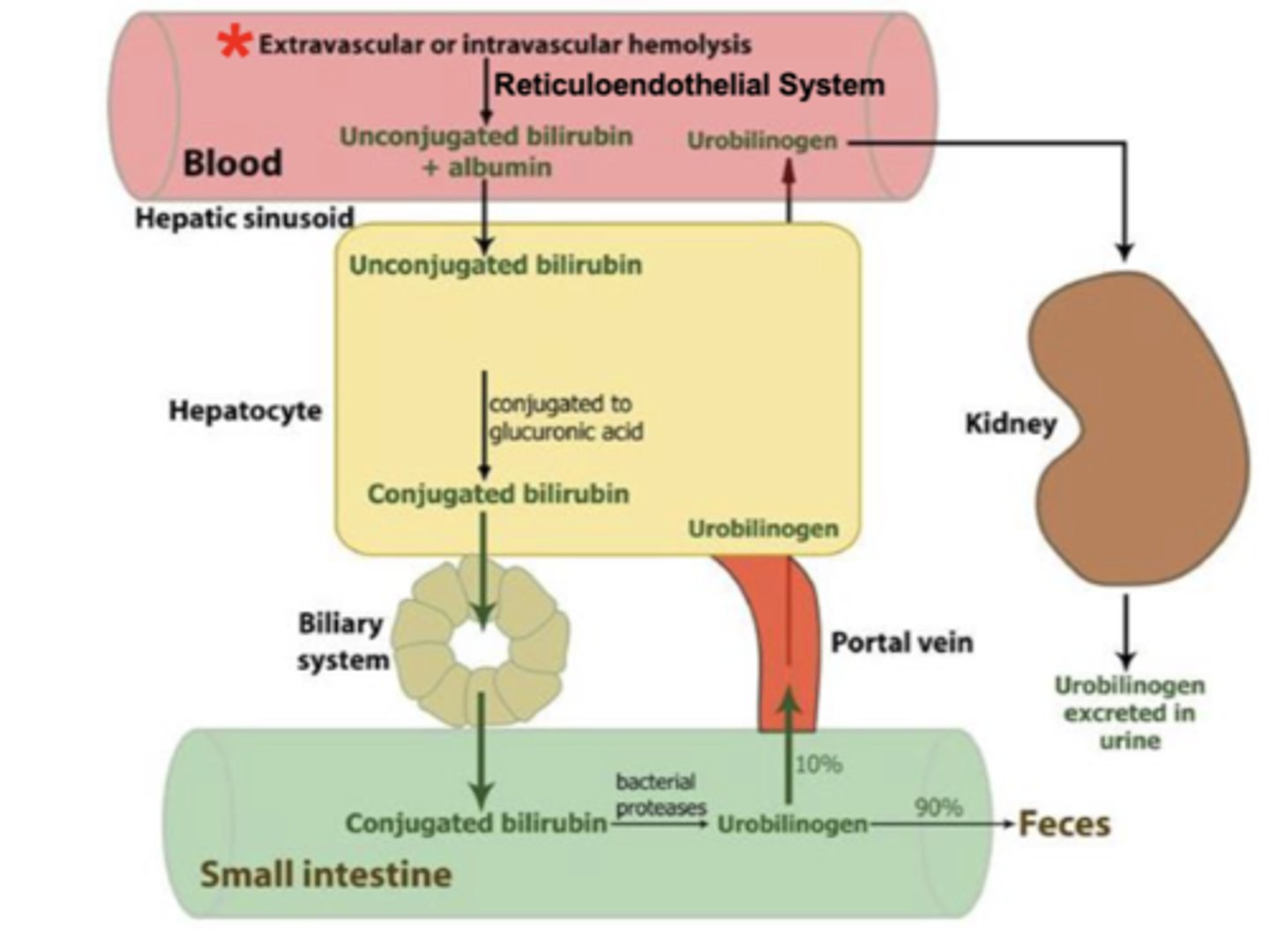
Why does urine have its distinctive yellow color?
urobilinogen = metabolite of bilirubin
True or False: The color of feces is a result of hemolysis.
True ==> hemolysis (RBC destruction) --> release bilirubin --> metabolized to urobilinogen that creates the color
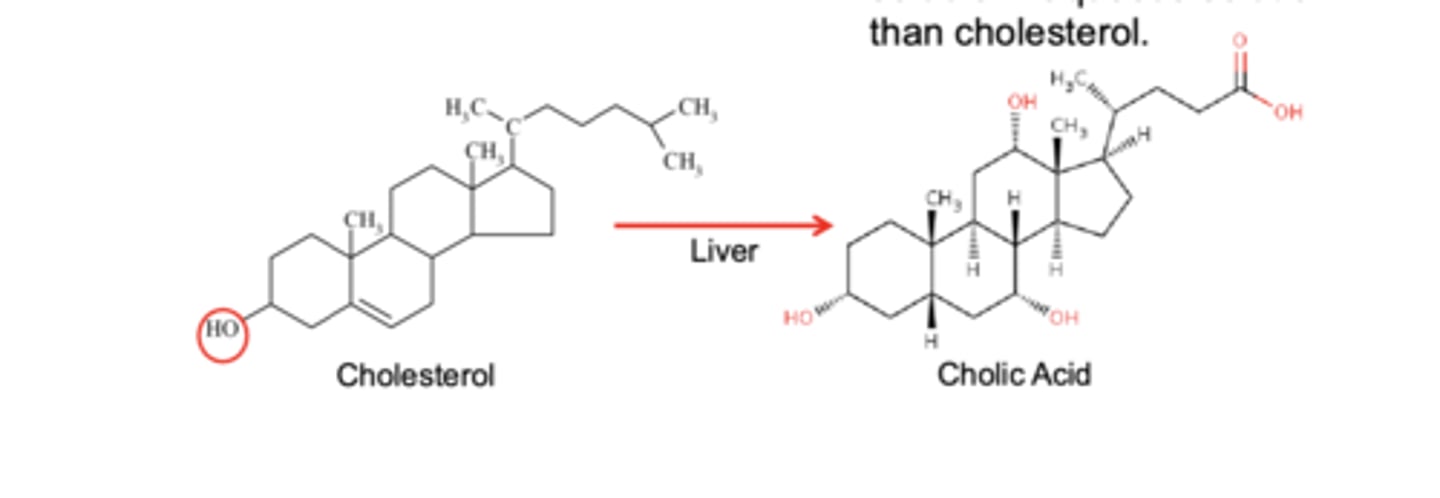
If cholic acid and cholesterol molecules have similar ring structure, why is cholic acid very more soluble in aqueous solution than cholesterol?
cholic acid has 5 charged groups ==> 7253x more aq soluble
*liver converts cholesterol into colic acid = bile salt
Name the primary bile acids.
-cholic acid
-chenodeoxycholic acid
*synthesized by the liver from cholesterol
How are secondary bile acids produced?
primary bile acids modified in the gut by bacteria--> form the secondary bile acids (deoxycholic acid & lithocholic acid) --> conjugated to glycine or taurine to become functionally equivalent to primary bile salts
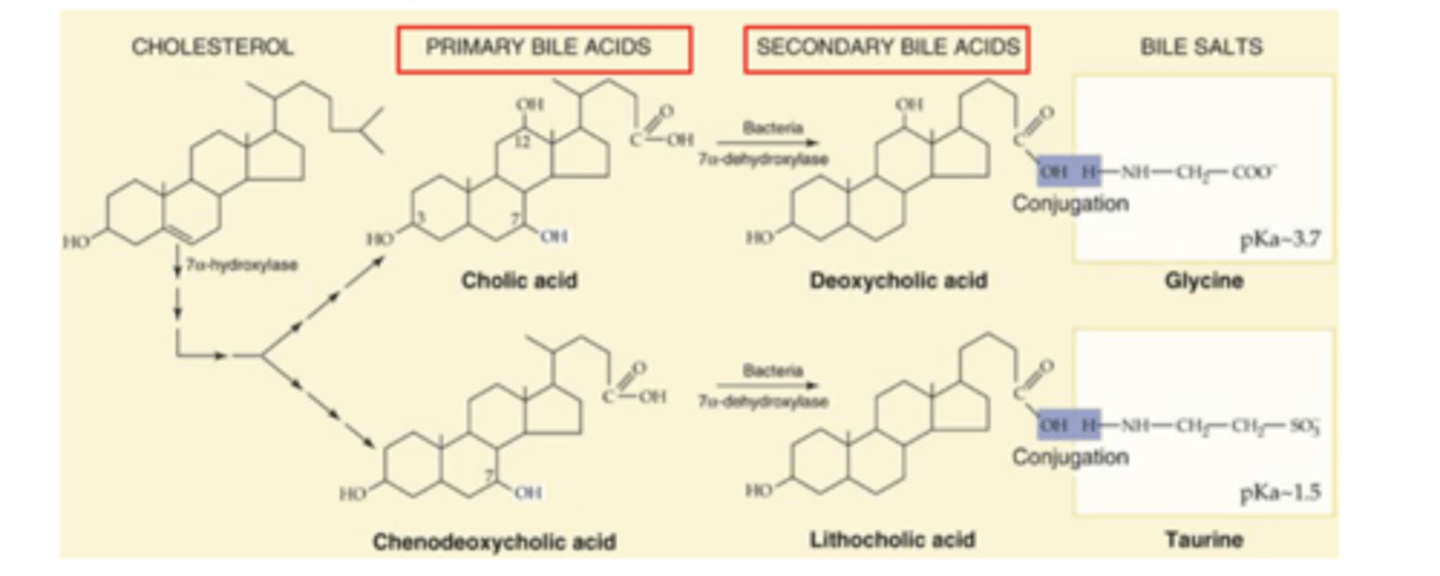
Name the secondary bile salts.
-deoxycholic acid
-lithocholic acid
which primary bile salt is a precursor to deoxycholic acid?
cholic acid
which primary bile salt is a precursor to lithocholic acid?
chenodeoxycholic acid
cholic acid is the precursor to which secondary bile salt?
deoxycholic acid
chenodeoxycholic acid is the precursor to which secondary bile salt?
lithocholic acid
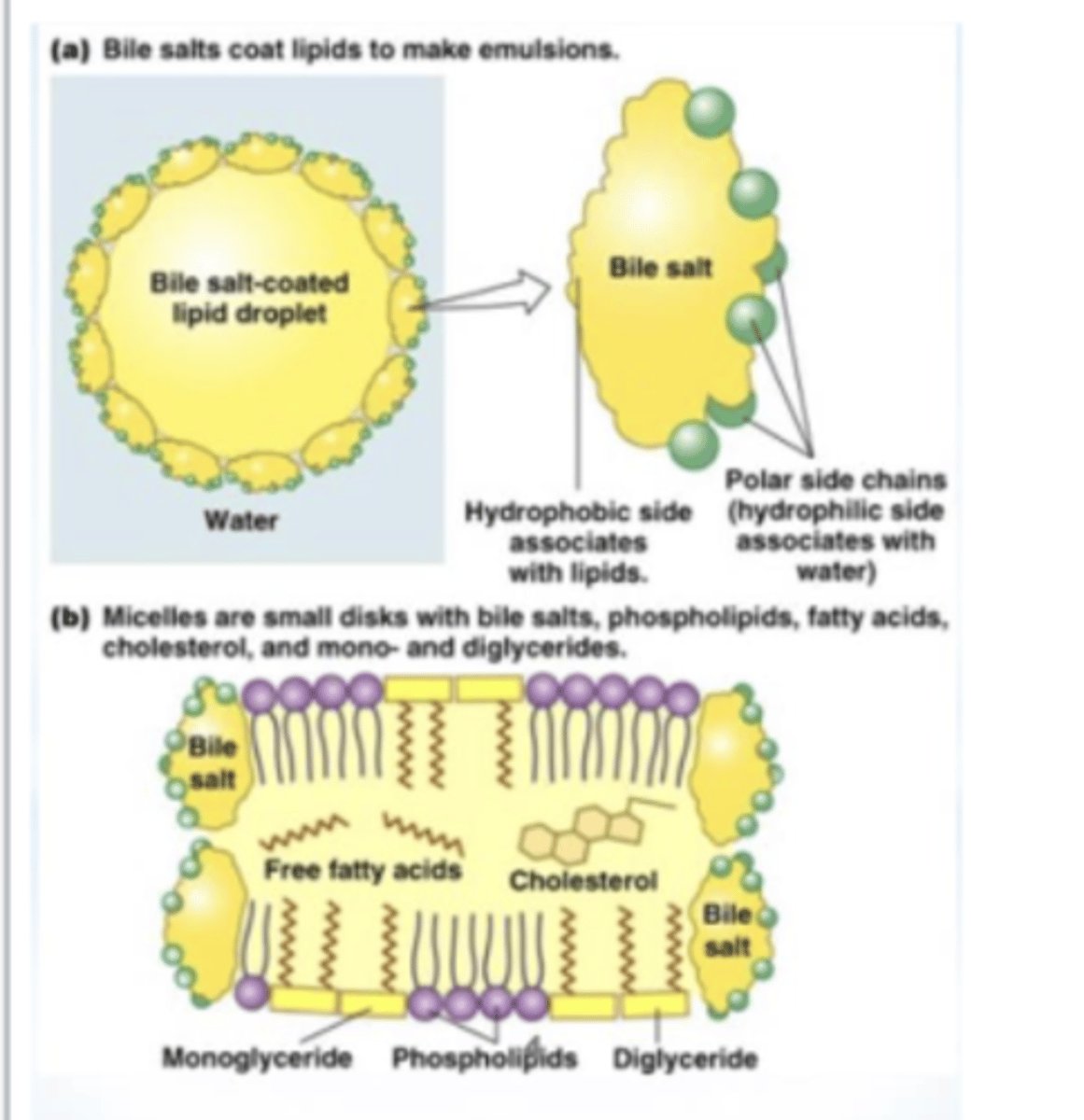
How are bile salts able to facilitate emulsifying fats and the formation of micelles?
bile salts contain a hydrophilic & hydrophobic face (amphipathic) ==> this property allows them to facilitate emulsifying fats & the formation of micelles
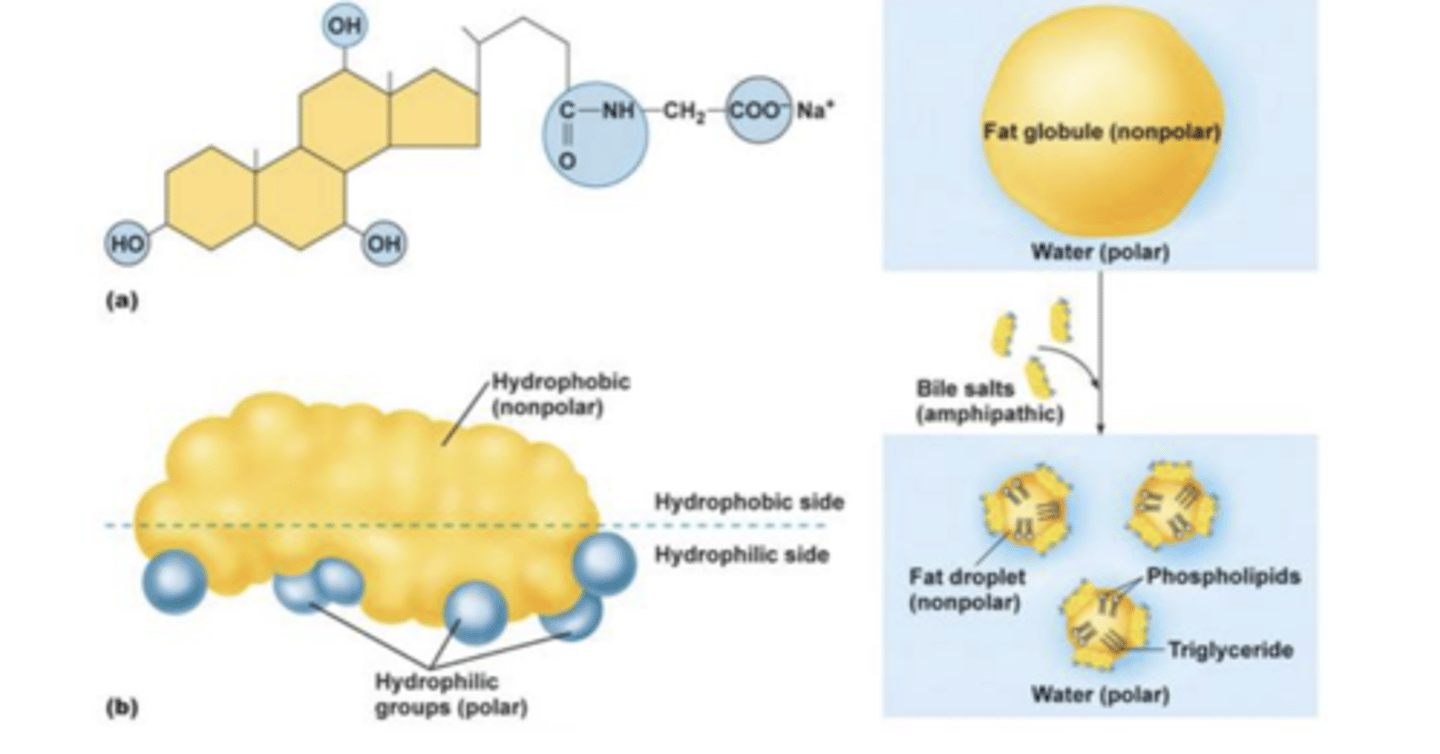
micelles
small disks with bile salts, phospholipds, fatty acids, cholesterol, monoglycerides, & diglycerides
*makes lipids more polar ==> greatly increases their rate of diffusion thru epi of small intestine (increases absorption of lipids)
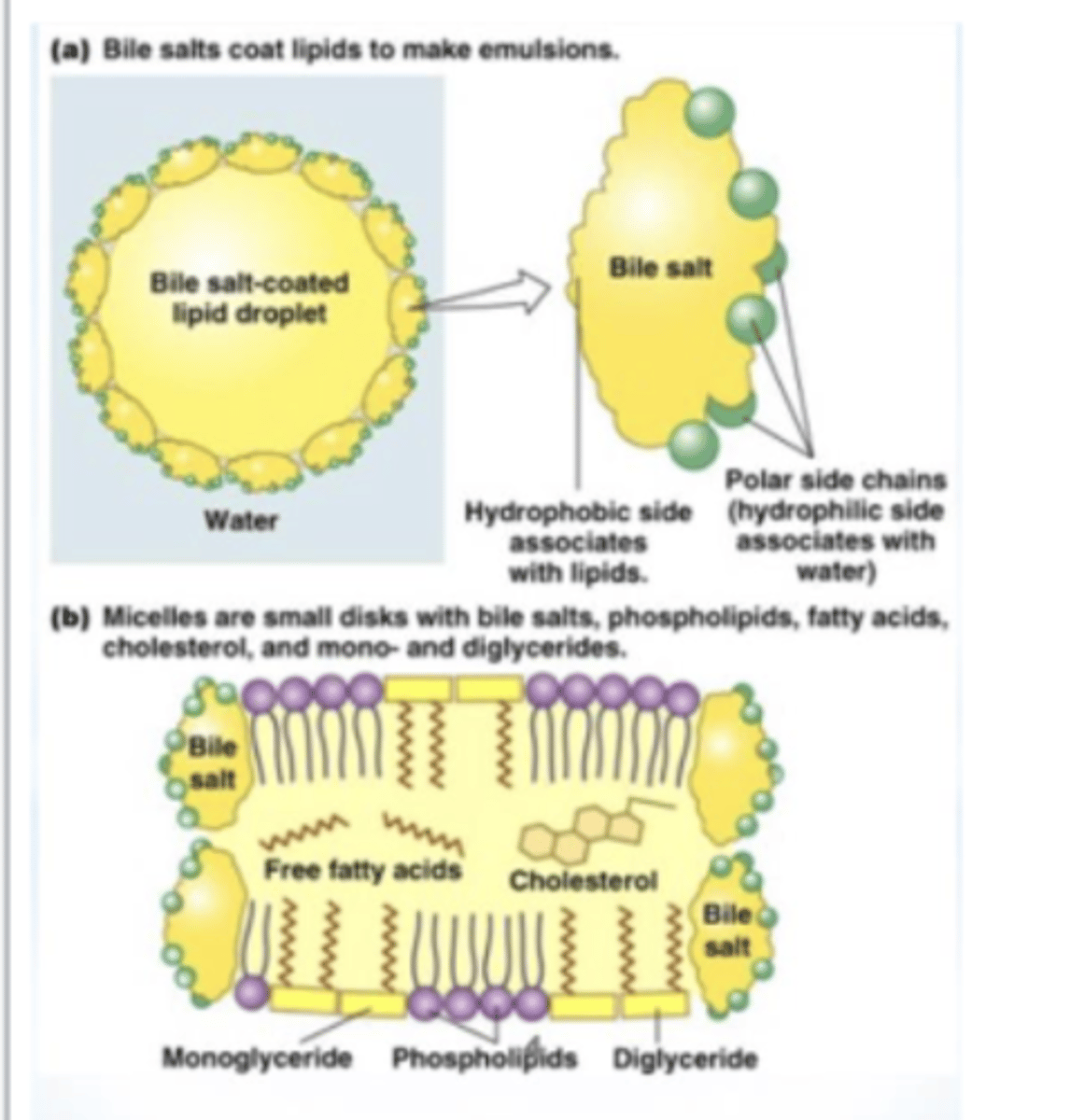
Why is micellar solubilization essential for efficient absorption of lipids?
makes lipids more polar ==> greatly increases their rate of diffusion thru epi of small intestine (increases absorption of lipids)
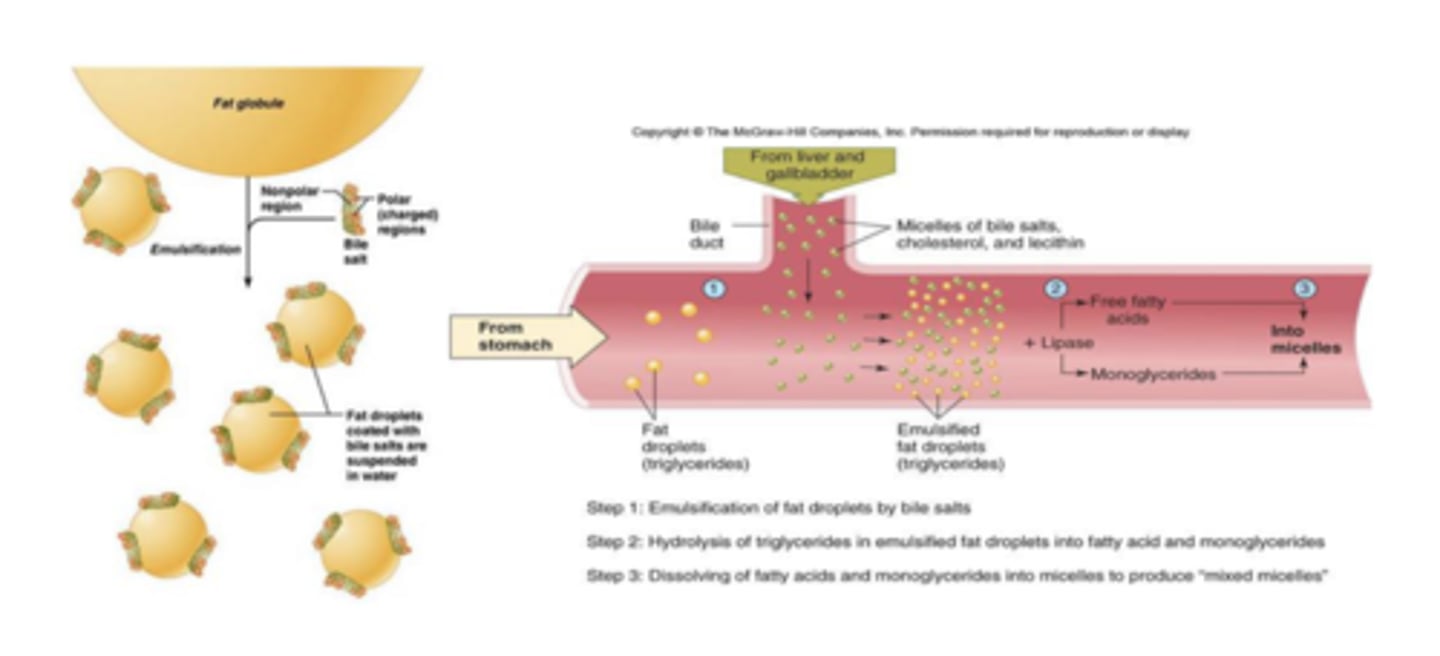
Describe how bile acids function in digestion.
emulsification of fat droplets by bile salts --> hydrolysis if triglycerides in emulsified fat droplets into fatty acid & monoglycerides --> dissolving of fatty acids & monoglycerides into micelles to produce mixed micelles
Enterohepatic Circulation
recycling of bile salts after they are synthesized in the liver ==> excreted in bile --> exit bile ducts/common bile duct --> enter duodenum --> travel to distal ileum --> absorbed into capillaries --> travel back to liver in portal vein -->>> liver removes bile salts from circulation & secretes them back into the bile
-only 15-30% of bile salt pool are excreted every day, the rest of bile salts remains in enterohepatic circulation (70-85%)*
-circulates 6-10x per day
-bile salt pool is 2-4g
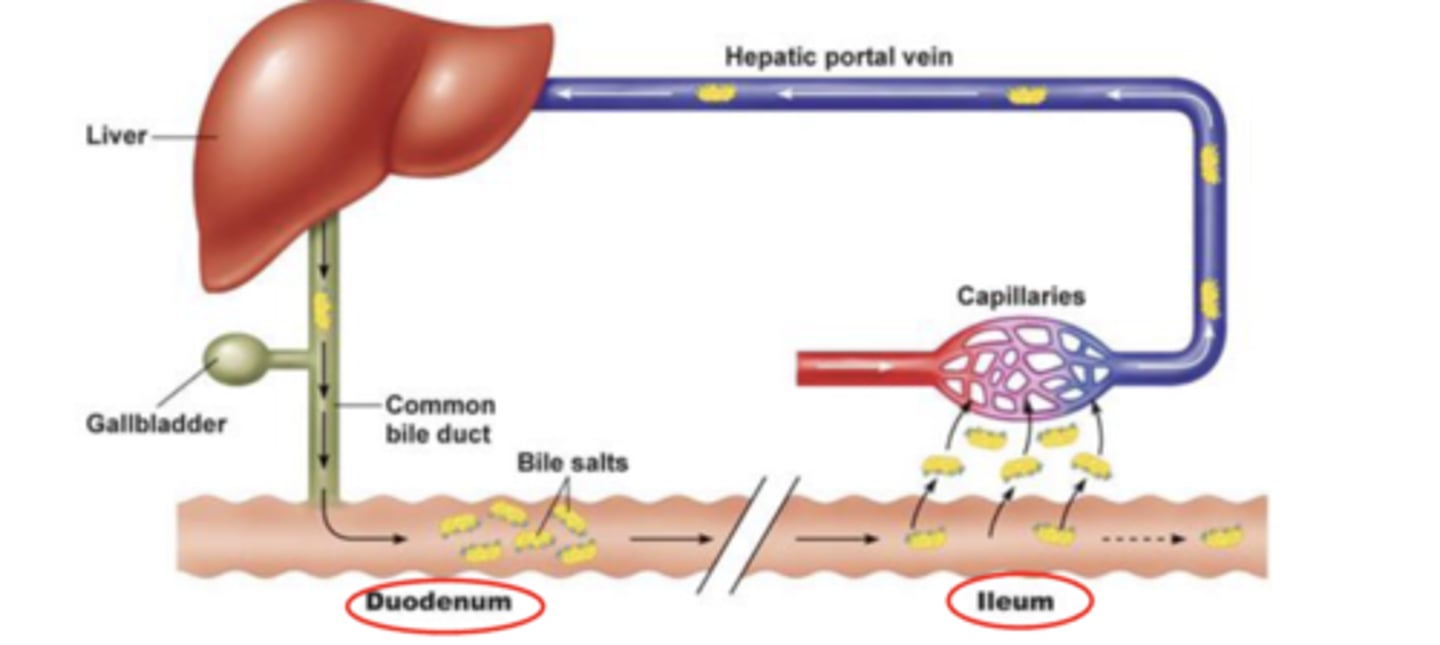
How often do bile salts circulate in enterohepatic circulation per day?
6-10x
How much bile salt is within the bile salt pool?
2-4g
How much of the bile salt pool is lost each day to excretion?
15-30%
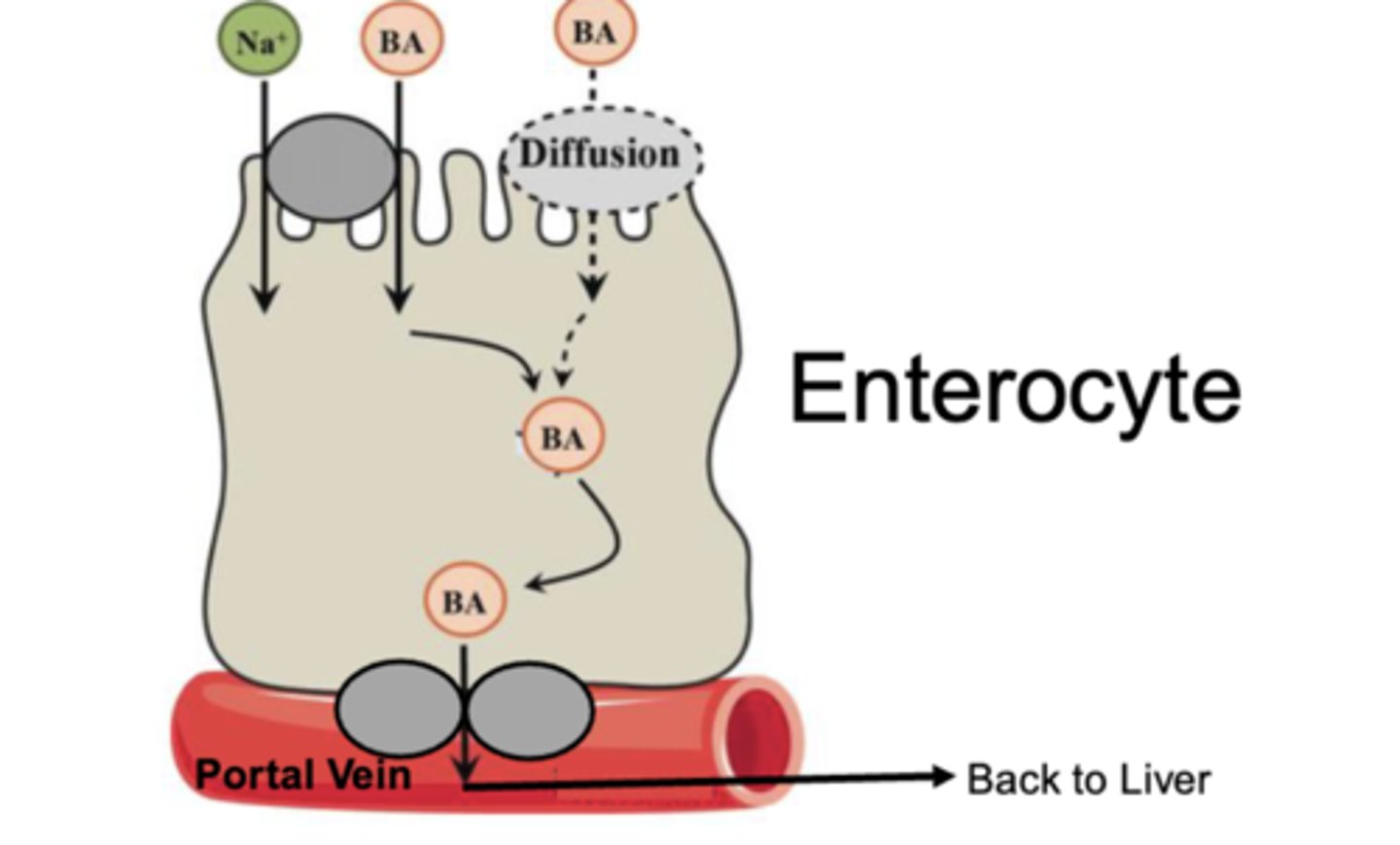
In enterohepatic circulation, bile salts are absorbed by __________.
the distal ileum
What are the 2 method by which bile salts are taken up by enterocytes?
-Na+ dependent symporter
-diffusion across the cell membrane (using the hydrophobic surface of the bile acid to fuse the lipid of the cell membrane)
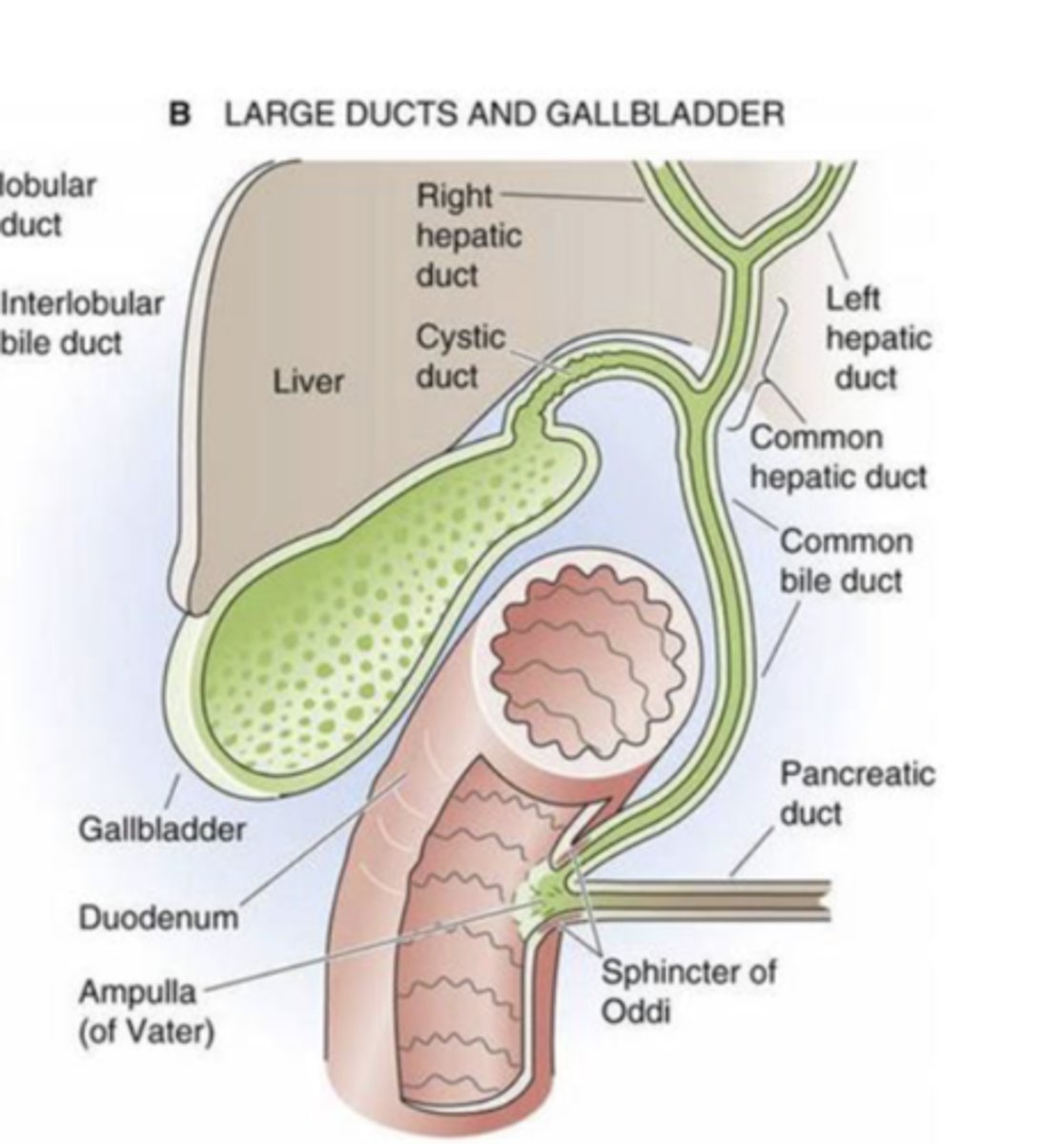
Describe bile flow within the liver
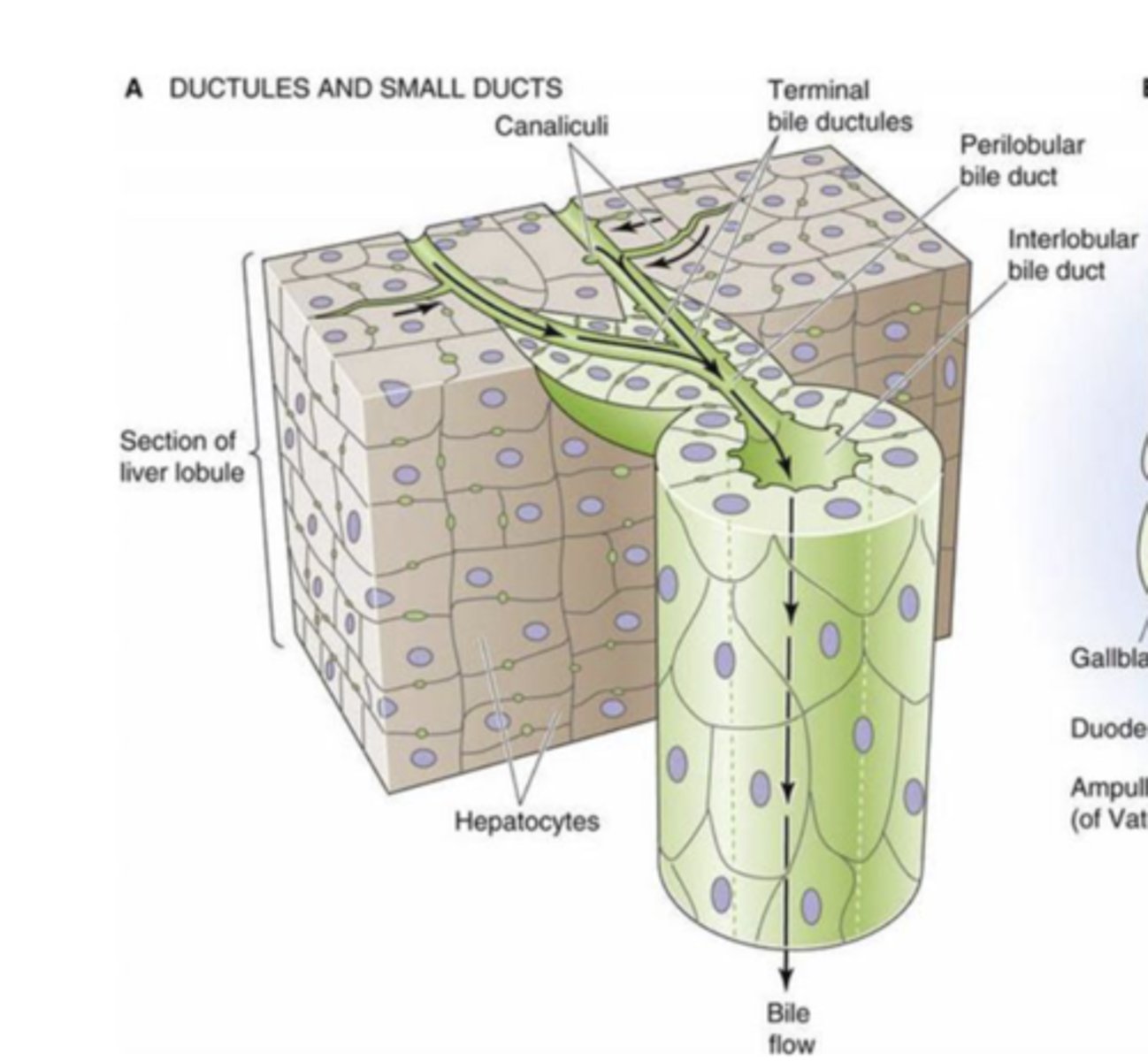
Describe bile flow through the large ducts to gallbladder to the small intestine
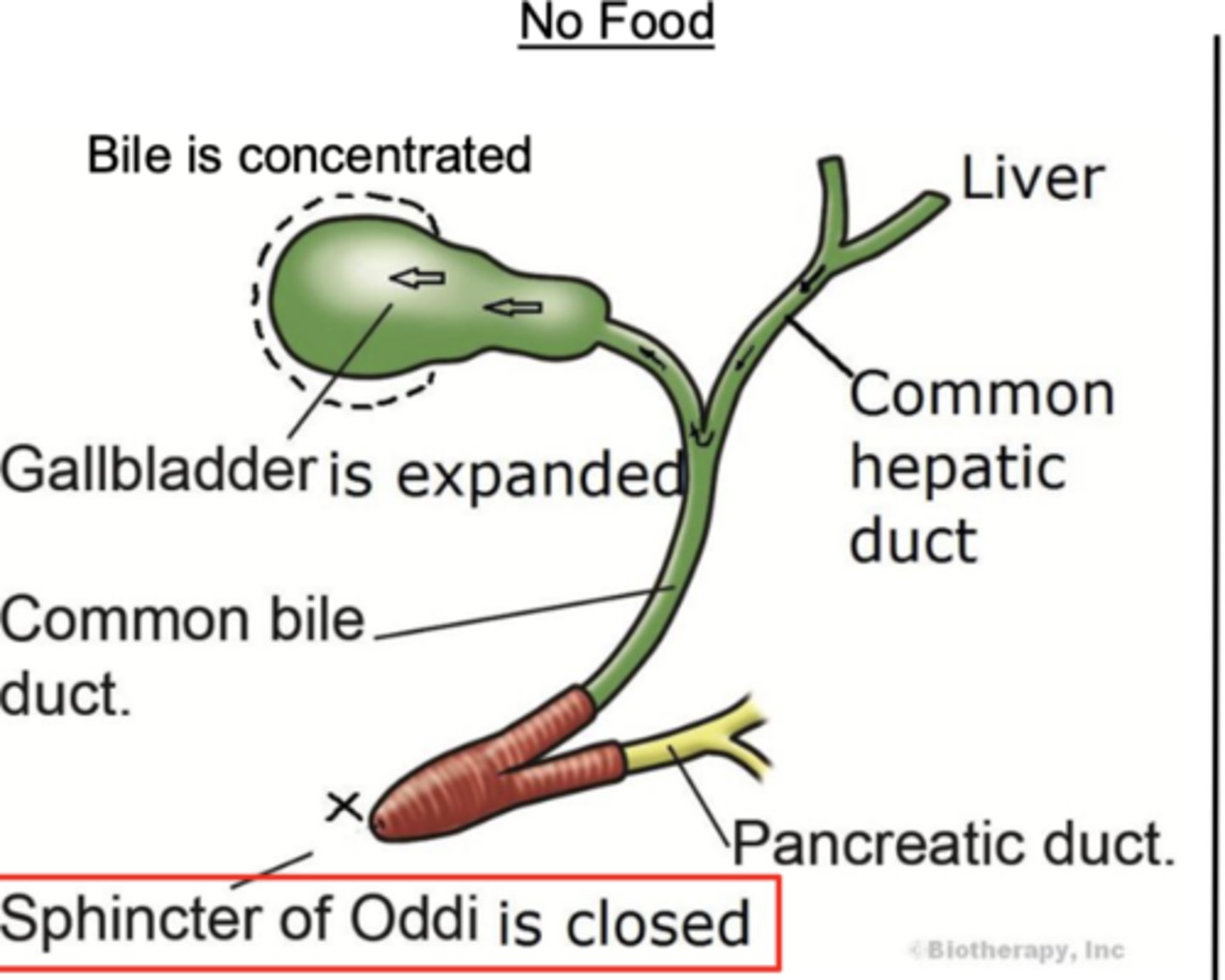
Why is most of the bile secreted by the liver stored and concentrated in the gallbladder between meals?
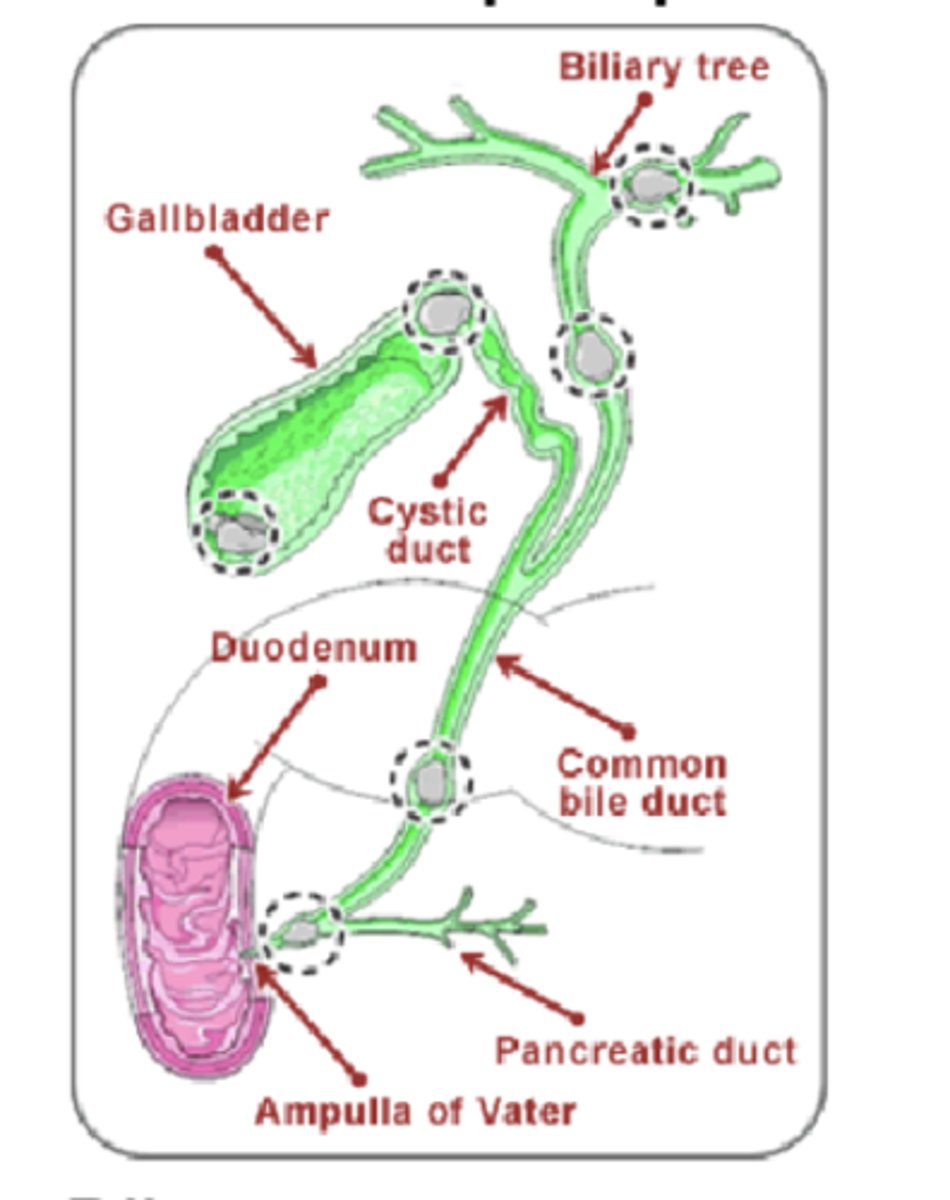
b/c the Sphincter of Oddi is closed ==> S of Oddi is the opening of the common hepatic duct (& pancreatic duct) into the duodenum --> if closed, the bile flow is directed back up towards the gallbladder
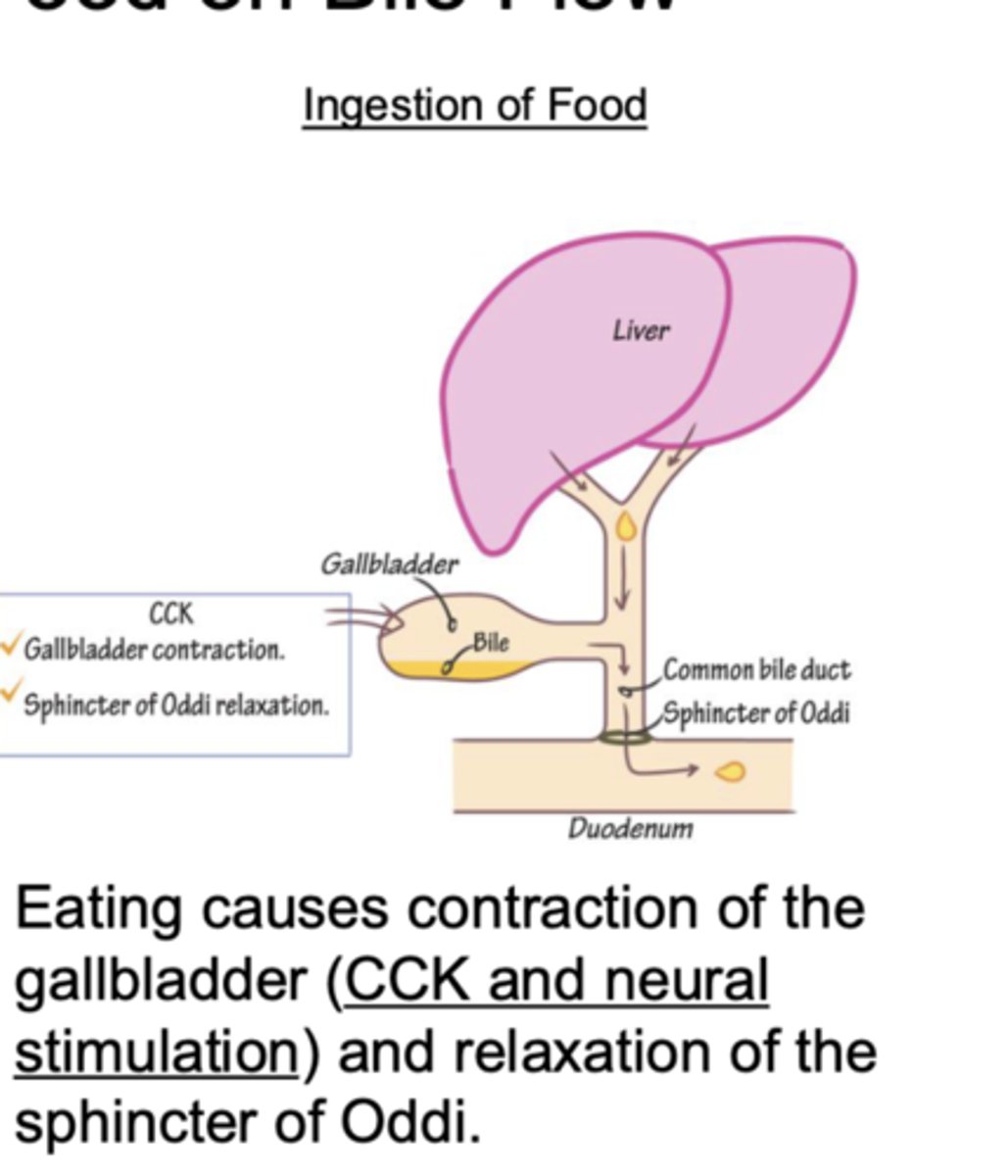
Describe the effect CCK has on bile flow
increases bile flow
-gallbladder contraction
- relaxes the Sphincter of Oddi (opening of duodenum where the common bile duct terminates)
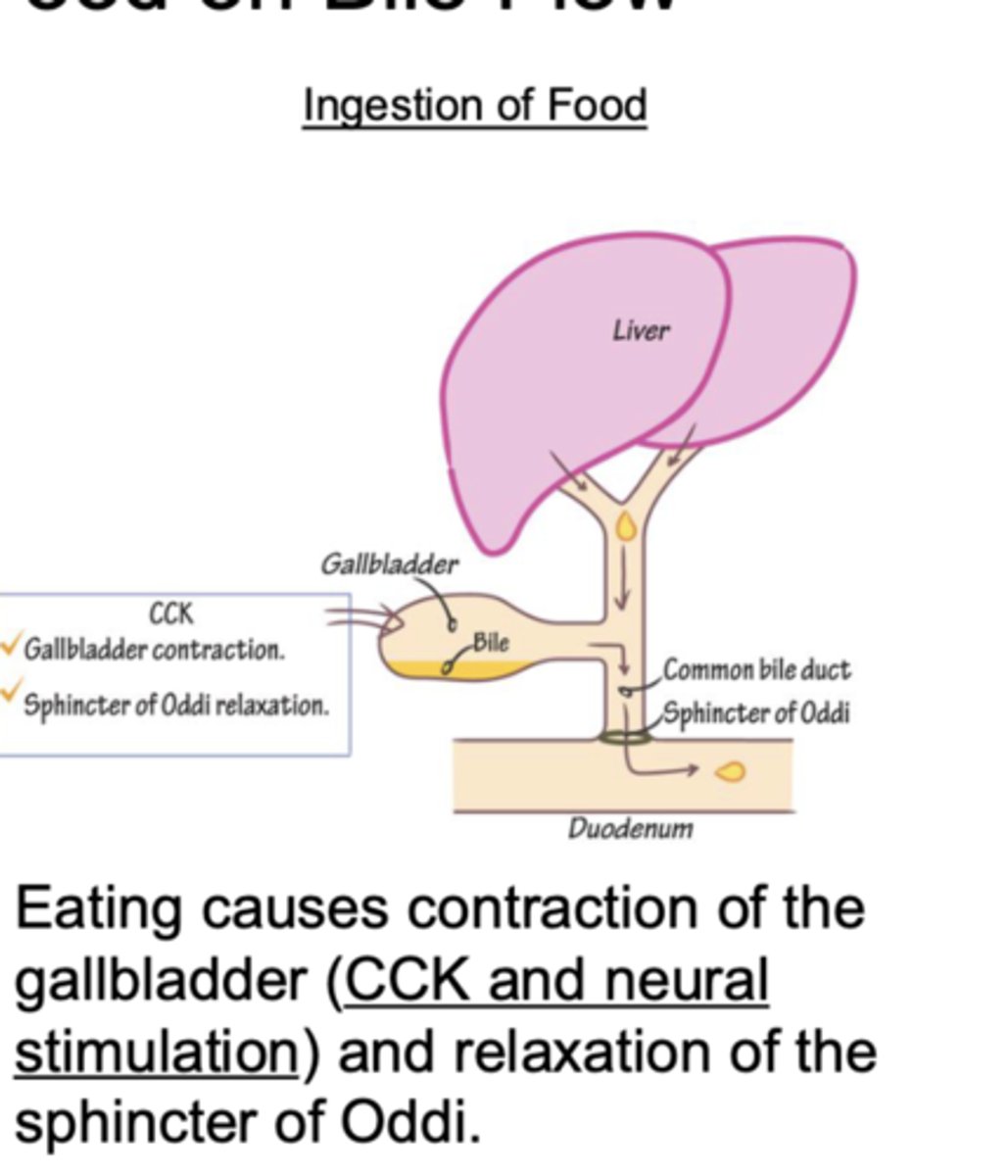
what effect does the ingestion of food have on bile flow?
increases bile flow
-increased contraction of gallbladder via CCK & neural stimulation
-relaxation of Sphincter of Oddi (opening of duodenum where the common bile duct terminates)
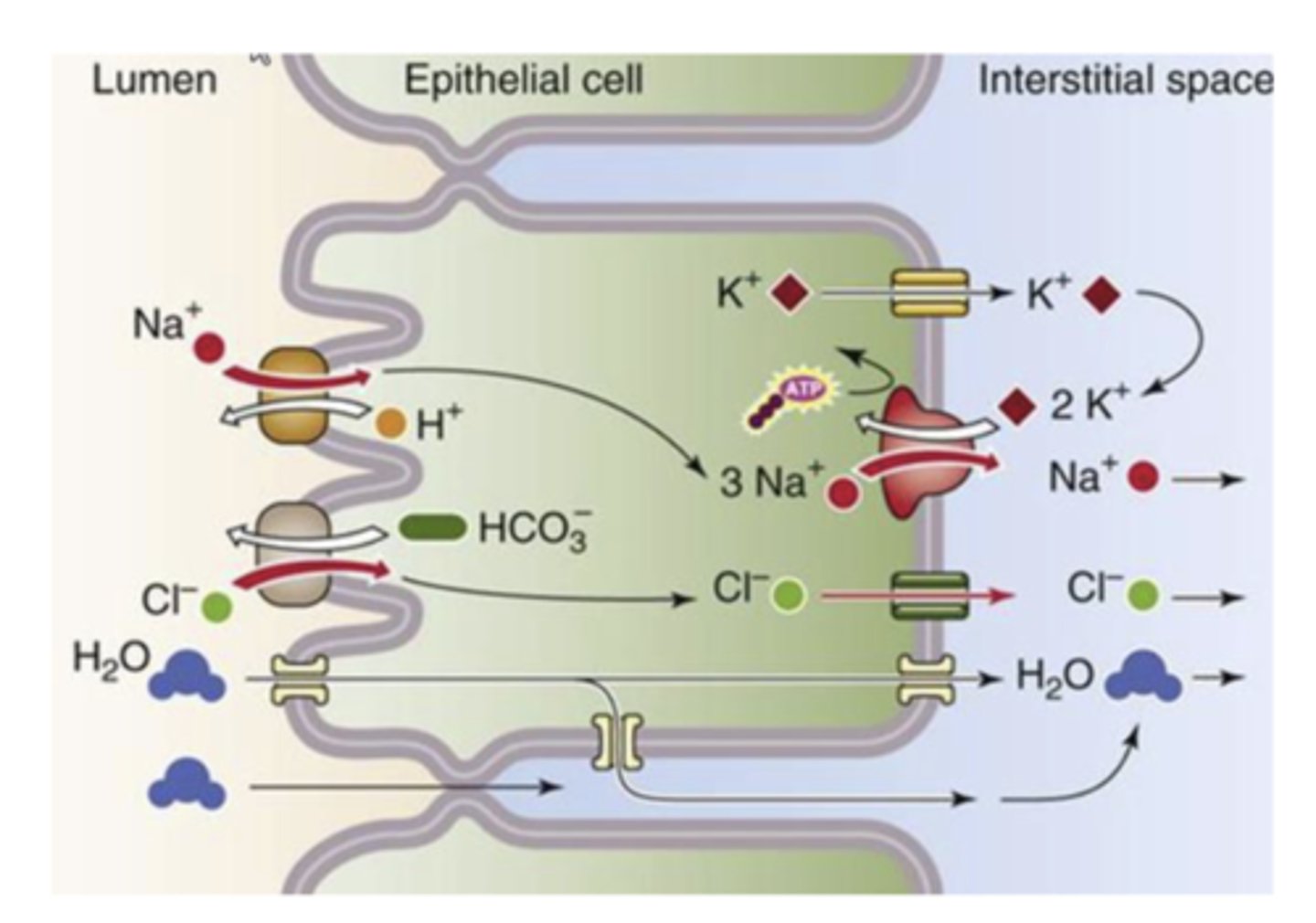
How is bile concentrated in the gallbladder?
ions removed from the bile in gallbladder & secreted into the interstitial space --> conc of ions in interstitial space increases --> water flows out of bile into the interstitial space (passively down osmotic gradient)
*concentrates bile by 10-20x
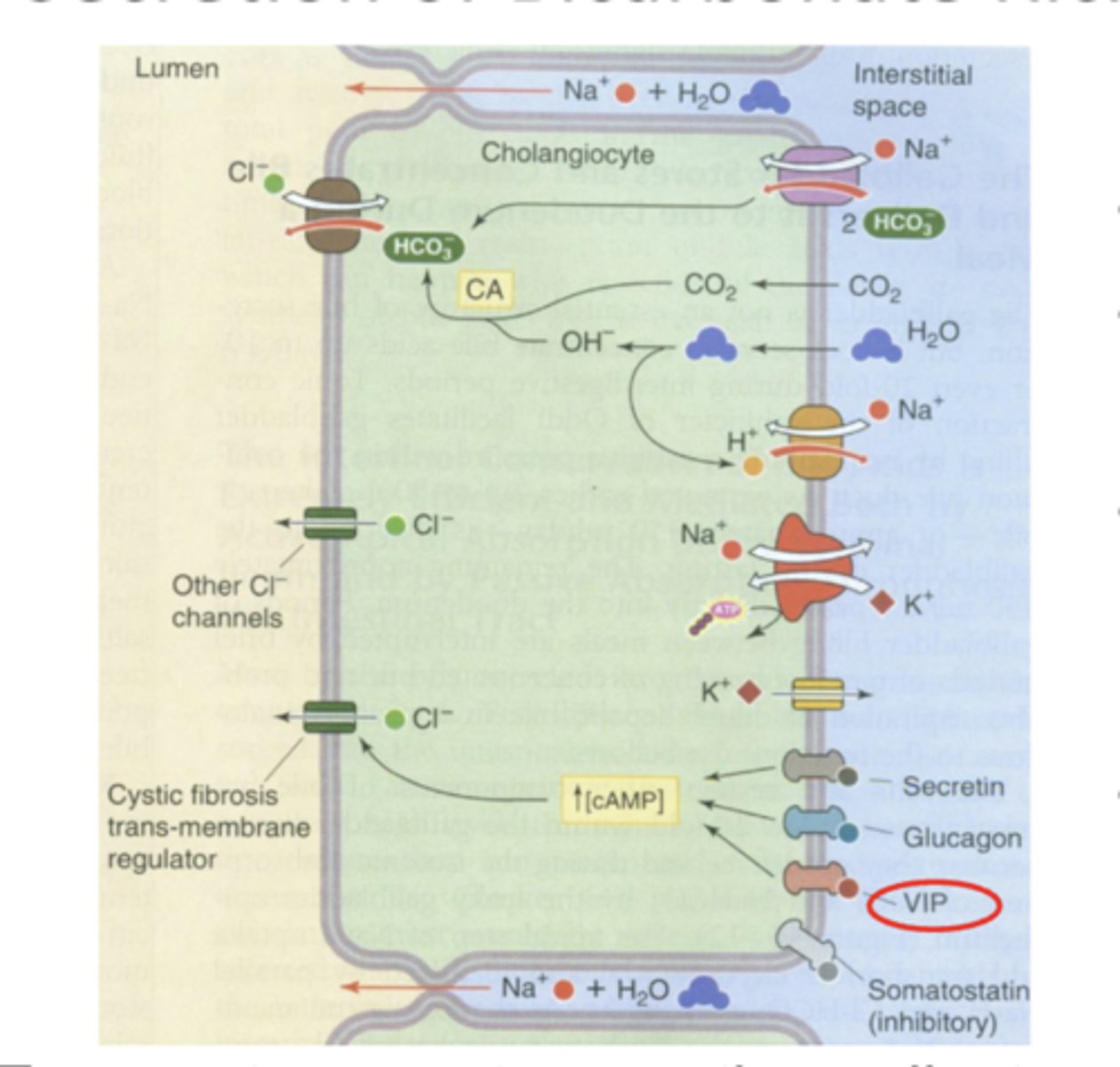
Why is bile bicarbonate rich?
b/c cholangiocytes (bile duct cells) secrete bicarbonate rich fluid into bile
*HCO3- enters cell at basolateral membrane via Na+/HCO3- cotransporter + CO2 diffuses into cell --> CO2 converted to HCO3- via carbonic anhydrase --> HCO3- exits cell at apical membrane via HCO3-/Cl- exchanger
-Cl- recycles through a Cl- channel**
*transporters create osmotic gradients w/in bile canalicu;ar lumen that provide the driving force for movement of fluid into the lumen via aquaporins
cholelithiasis
process of gallstone formation
*slow process that generally causes no pain or other symptoms
What are the common causes of cholelithasis
-too much absorption of water from bile
-too much absorption of bile acids from bile
-too much cholesterol in bile
-inflammation of epithelium
Where can gallstones form?
can develop anywhere in the biliary tract where bile is present (w/in the liver, gallbladder, & common bile duct)
What are the majority of gallstones made out of?
cholesterol (70%)
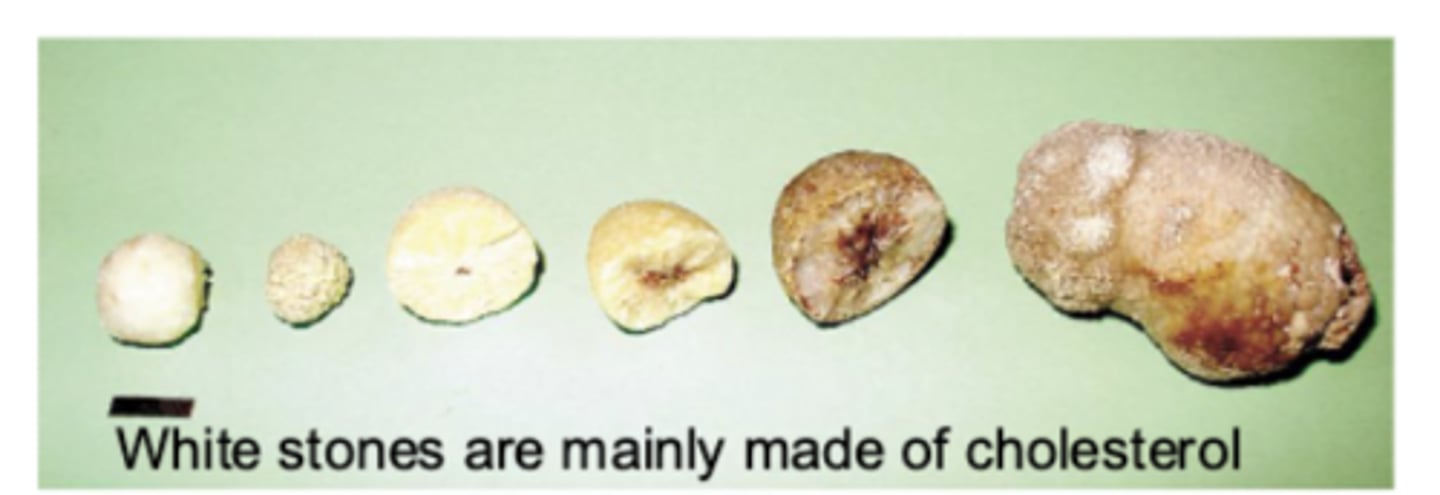
What accounts for the other 30% of gallstones? (cholesterol makes up 70%)
pigment stones ==> contain bilirubin
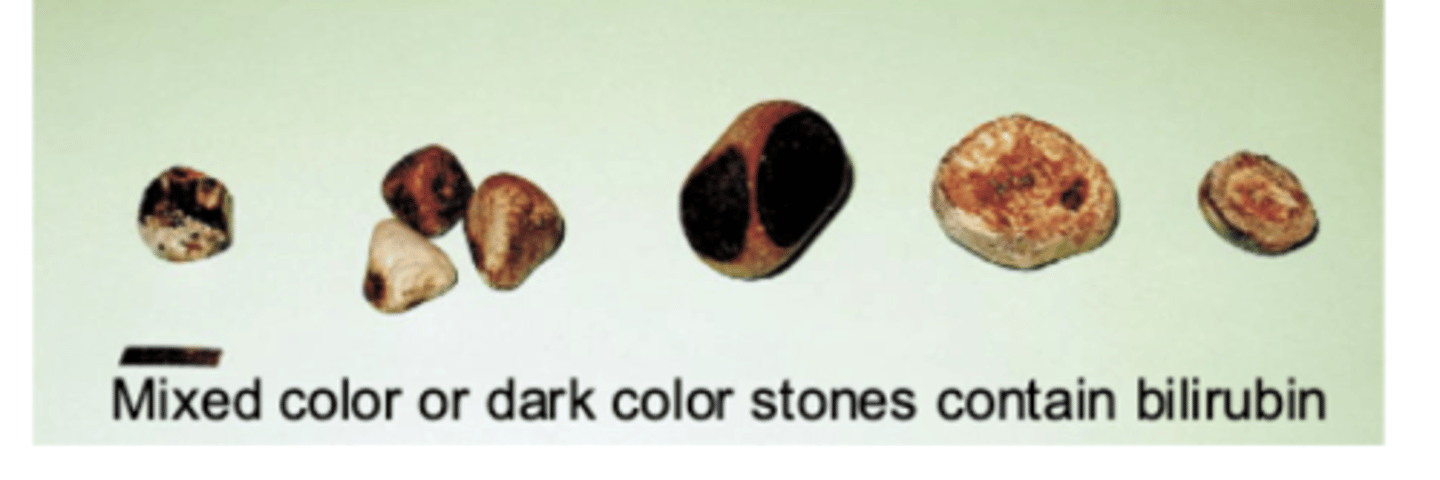
True or False: Patients can have a mix of cholesterol and pigment gallstones
True
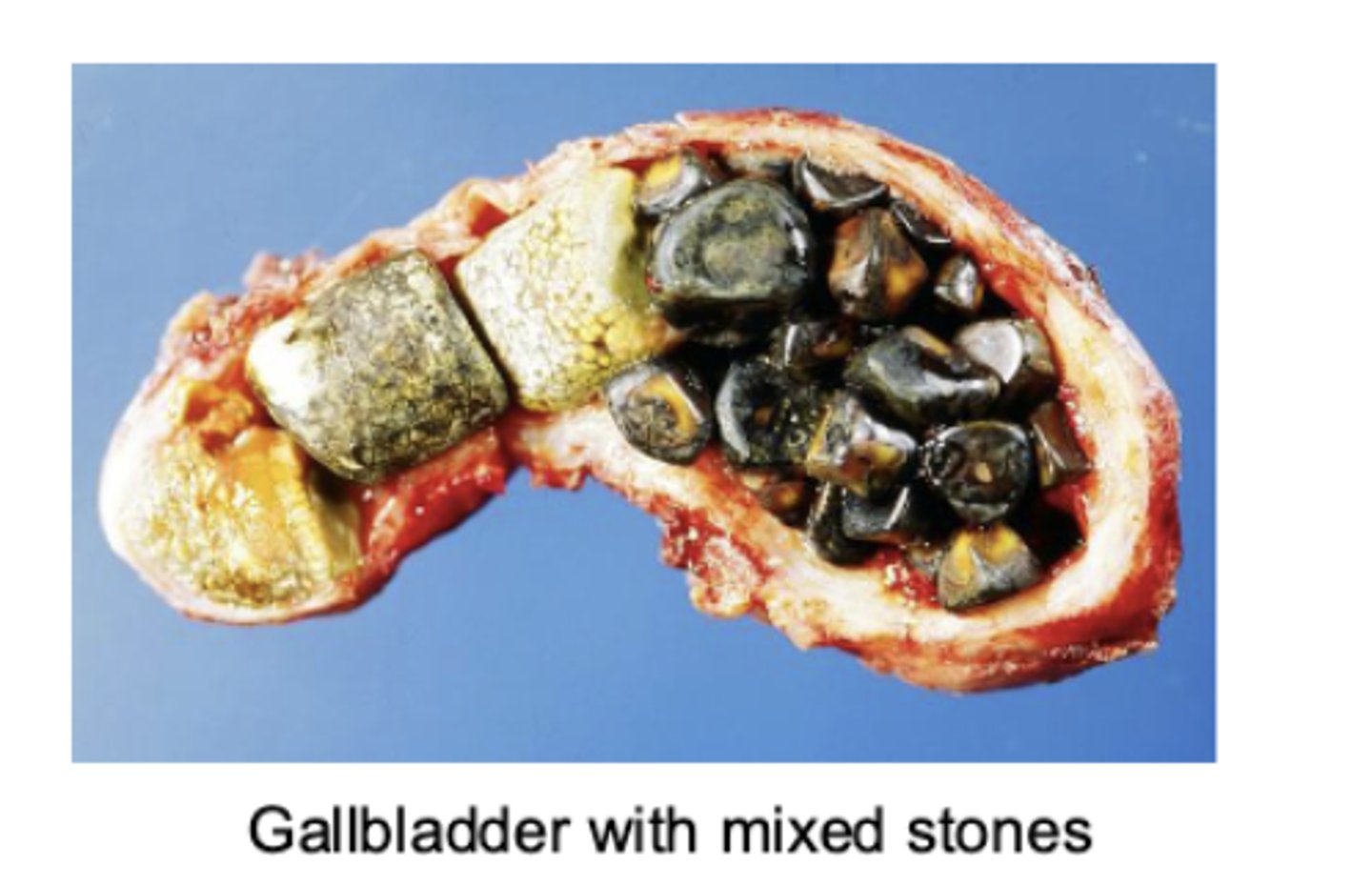
What are some complications of gallstones?
-pancreatitis (majority)--> due to blockage pancreatic duct; painful inflammation of pancreas
-inflammation of gallbladder
-blockage of biliary flow anywhere in biliary tree if large enough