Drug Induced Diseases Geriatric Considerations
1/21
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
22 Terms
ID and recognize mechanisms for PK interactions: pH interaction on absorption
Drug changes acidity of stomach, changing absorption of other drugs
Ex. proton-pump inhibitors increase gastric pH decreasing absorption
ID and recognize mechanisms for PK interactions: Adsorption interaction on absorption
Two drugs bind together (make complex), leading to drug-drug interactions
Ex. Calcium binds to Fluoroquinolones, preventing it from binding to receptors
ID and recognize mechanisms for PK interactions: GI Motility interaction on absorption
Drugs may interact w rate of gastric emptying, impacting absorption (faster motility = faster rate of absorption)
Reglan speeds rate of gastric emptying
Opiates decerase rate of gastric emptying
ID and recognize mechanisms for PK interactions: Gut Flora interaction on absorption
Dysfunctions impact metabolism and absorption - Gut bacteria are responsible for the metabolism of some drugs during absorption, disrupting gut flora (antibiotics) influences absorption
Antibiotics change gut flora will decrease con (effectiveness) of active ingredient of Birth Control
ID and recognize mechanisms for PK interactions: First Pass Effect on absorption
Oral drugs metabolized prior to entering circulation (decreases absorption amount and distribution)
Physiological dysfunctions (leading to increased first pass effect) may require higher drug con
ID and recognize mechanisms for PK interactions: Antagonism for Protein Binding interaction on distribution
Drugs compete for protein binding, influencing distribution
Drugs w higher affinity wins and binds to protein / Drugs w lower affinity remain unbound and in circulation
ID and recognize mechanisms for PK interactions: CYP Isoenzymes on metabolism interactions
Drugs can inhibit/induce CYP Isoenzymes, slowing or increasing rate of metabolism (influenced via affinity). If the parent compound has toxic potential, check that other drugs don’t have a strong affinity to the same Isoenzyme
Genetic Variation in CYP Isoenzymes + Isoenzyme Induction (increase # of enzymes, increase met) + Isoenzyme Inhibition (decrease met of drugs)
Prodrugs are useless if no isoenzymes
ID and recognize mechanisms for PK interactions: Renal pH on Elimination
Reabsorption from kidneys into bloodstream (type of elim reabsorption). Renal pH = the pH of urine and kidneys affects reabsorption of drugs from kidneys into the bloodstream. pH affects ionized state.
Define and differentiate competitive and noncompetitive inhibition and induction of an enzyme
Competitive: antagonist competes w agonist for receptor sites. Concentration dependent (highest affinity wins). Binding can be reversible
Non - antagonist binds to receptor and stays bound (blocks other drugs, no affect on receptor
Enzyme Induction - Increasing the # of enzymes, increasing metabolism
Recognize the impact of affinity and concentration on metabolic drug interactions
Affinity: Determines “winner” in competitive inhibitor interactions. Drugs with higher affinity will bind to plasma proteins and CYP450 enzymes over drugs with lower affinity. The other drug will remain unbound, continue circulation, increasing rate of distribution, metabolism, and excretion
Concentration: Drugs must reach a threshold to exceed or inhibit enzyme action (metabolism interaction) Ex. Cimetidine a weak inhibitor at low dose, but inhibits 2 isoenzymes at high dose
ID the impact of P-Glycoprotein on drug interactions
P-Glycoprotein: An efflux transporter in intestines, liver, and kidney that pick up drugs absorbed through intestines and carry it back INSIDE to intestine (RECIRCULATION)
Inhibit - more drug absored
Induce - less drug absorbed
ID and recognize mechanisms of pharmacodynamic interactions
Synergistic Effects: Two drugs acting together, their actions add together. Ex: 2 sedatives have synergistic effects
Changes in body chemistry: Drug interactions may affect body chemistry, causing adversity (electrochemical potentials/gradients): Arrhythmias - ACE inhibitors and K sparing diuretics raise potassium lvls
Opposing Effects: drug interaction cancels out the effect of a drug or botch drugs
ID the impact of and common “drug-food”, and drug-disease interactions
Drug Food Interactions:
Absorption - food in gut and gut motility alters extent of absorption, altering rate
Adsorption - Milk based products and Fluoroquinolones
Food creating physical barrier, preventing absorption - Azithromycin has reduced bioavailability when taken with food and should be taken 2 hours apart
Metabolism - Certain foods may alter P450 enzyme (grapefruit juice is inhibiter of 3A4 enzyme
Excretion - Fruit juices may alter urinary pH (acidic juices increase urinary pH)
ID the impact of and common drug-food, and “drug-disease” interactions
Drug-disease Interactions:
Absorption - GI function (fast/slow) affects absorption (B12 needs stomach acid to be absorbed, stomach surgery indicative)
Distribution - Disease causing albumin lvls to fluctuate, affecting protein binding (burn patience have decreased albumin)
Metabolism/Excretion - Liver and Kidney disease impact metabolism and excretion / Alc intake potential for hypoglycemia in diabetics if drug interact w alc met
Define and differentiate between adverse drug reactions, side-effects, and medication error
Adverse Drug Event: Adversity resulting during inappropriate or appropriate use of drug. May be caused by reactions or med errors
Adverse Drug Reaction: A type of adverse drug event of a physiological adverse reaction/harm despite appropriate dosing. USUALLY PREVENTABLE. ID high risk patients, comm w other providers, extensive med history, special patient populations
Medication Errors: Inappropriate med dosing, administration, adherence, or other factors. PREVENTABLE
ID reporting program for drug interactions and adverse drug reactions
FDA
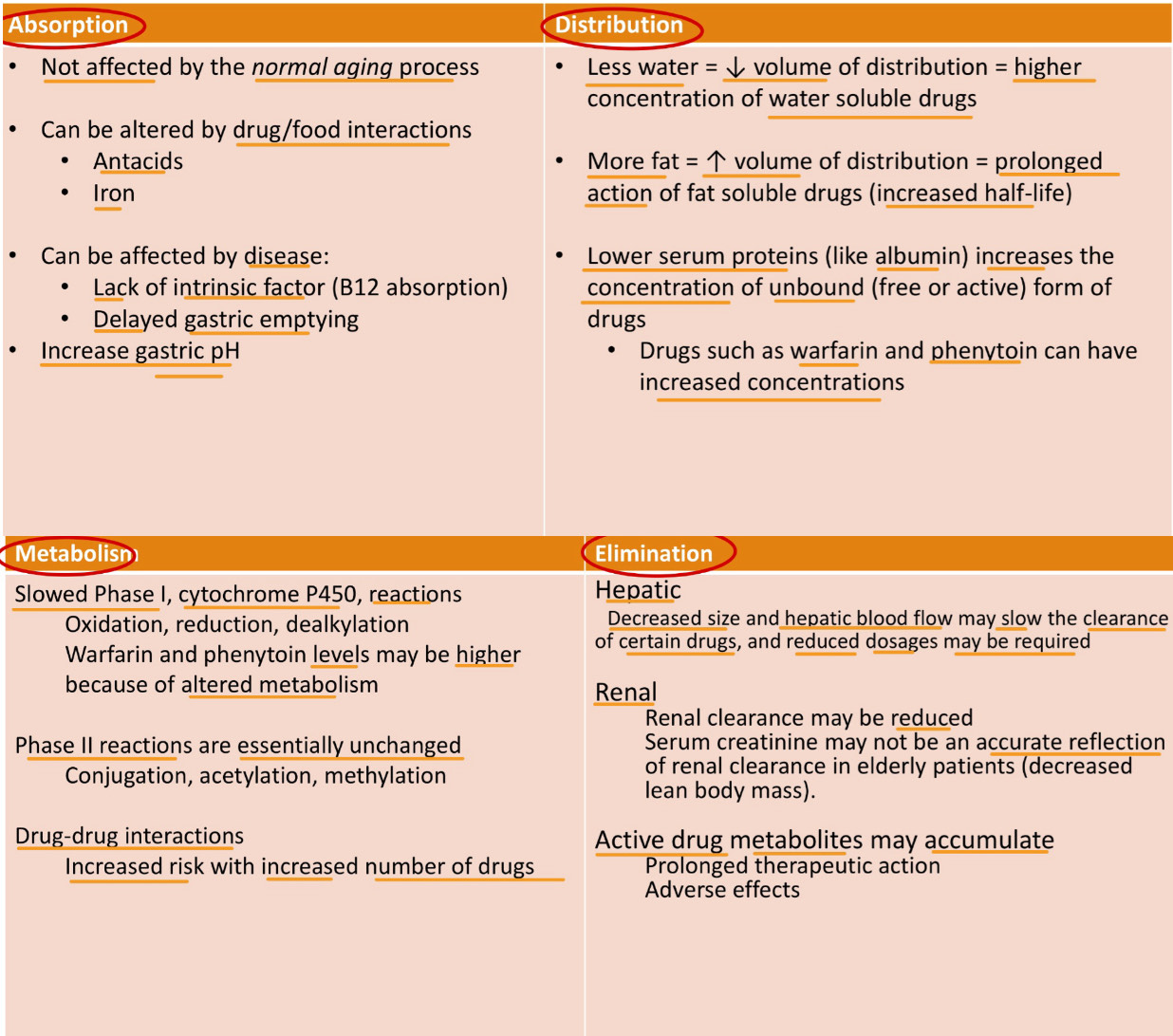
ID and describe the physiologic changes that occur in older adults that impact pharmacokinetic and pharmacodynamic responses
ID and describe the goal of and the commonly prescribed med classes on the AGS BEERS criteria
AGC BEERS criteria - guideline for prescriptions of geriatric patients, allows view of risk to weigh risk vs therapeutic effect
AGS Beers Drug Classes:
Anticholinergic Meds - risk of confusion, constipation, and urinary retention
Cardiovascular Meds - hypotension, CNS effects
Benzodiazepines - increased risk of falls and cognitive impairment, increased sensitivity sim effects to alc
Sedative-Hypnotics - Nonbenzodiazepine Hypnotics
Antipsychotic Meds - risk of stroke and mortality in dementia patients (avoid for dementia)
Pain Meds - risk of sedation, falls, and constipation (opiods)
ID and describe the mechanism of at least four potentially harmful medications for geriatric patients
Anticholinergic Agents - block acetylcholine receptors, leading to decreased secretions and muscle contractions. Can cause confusion, dry mouth, constipation, and urinary retention
Cardiovascular Meds - avoid alpha-1 blockers, alpha agonists (high risk of hypotension / CNS effects) & Spironolactone - higher risk of hyperkalemia
Benzodiazepines - enhance the effect of the GABA neurotransmitter, leading to sedation effects. Increased risk of falls, fractures, and cognitive impairment
Sedative Hypnotics - similar to benzos
Antipsychotic Meds - avoid using for problems associated w dementia
Pain Meds - NSAIDS - GI bleeding, peptic ulcer, & Indomethacin
ID and recognize factors that contribute to non-adherence of medications in the older population
Multiple medical conditions
Multiple medications/polypharmacy
Adverse Drug Reactions
Multiple Prescribers
Cognitive Decline
Recognize potential medication adverse events when an older adult presents with a new condition or complaint on a new medication
Adverse Drug Reactions - symptoms may be misattributed to aging rather than medication effects
Drug interactions - Increased risk due to polypharmacy
Exacerbation of Existing Conditions - New meds may worsen pre-existing health conditions
Given a clinical scenario that includes a geriatric patient, apply guidelines for safe prescribing to avoid adverse reactions
Start Low, Go Slow - begin w lower doses, titrate slowly to minimize adverse effects
Review Meds Regularly - conduct regular med review to asses necessity and effectiveness of each drug
Consider non-pharm options
Educate patients and caregivers - provide clear instructions, strategies for adherence
Monitor for adverse effects - be vigilant for signs, especially when starting a new med