L10: Open Fractures & Osteomyelitis
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
32 Terms
Describe the surgical aspect of treatment for osteomyelitis.
Treatment involves surgical debridement to remove necrotic tissue, sequestrum (piece of dead bone), and foreign material (implants); removal of implants is required to resolve infection if there’s biofilm formation on it. In addition, there should be lavage and drainage of the wound.
What does it mean if a fracture is not healing with concurrent osteomyelitis?
If the fracture is not healed, it means rigid stabilization is required - bone will heal in the face of infection as long as it’s stable!

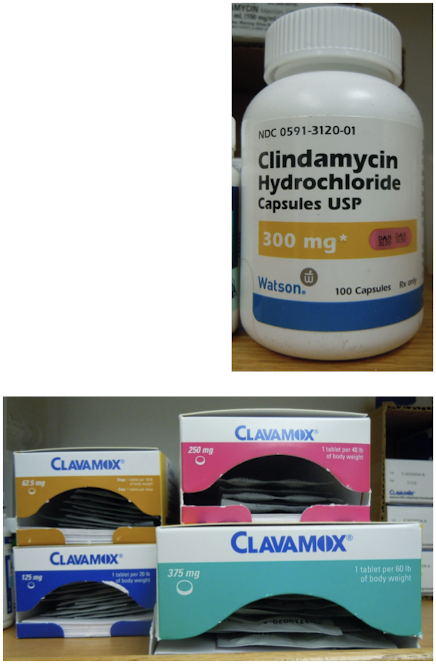
Describe the antibiotic aspect of treatment for osteomyelitis.
Antibiotics should be chosen based on C&S results. Prior to C&S results, assume Staphylococcus sp. or mixed infection. Initially they should be given IV and orally for long term; treatment should be continued for 6-8 weeks.
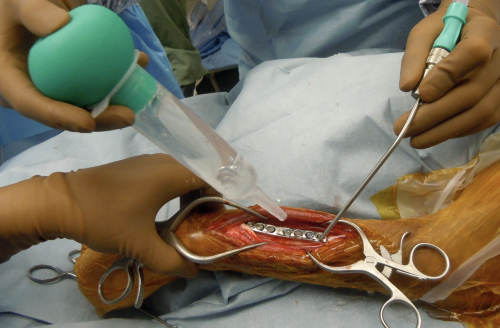
For areas with a large amount of soft tissue, we can use local delivery systems.
Antibiotics alone will NOT eradicate the infection if biofilm is present.
What are antibiotic beads and when are they used?
Antibiotic beads are a type of local delivery system. They deliver high local concentrations of antibiotics in ischemic areas with minimal or no systemic side effects. They are usually not used as the initial treatment and can have variable elution.
This method is beneficial in cases where systemic antibiotic therapy may be less effective due to biofilm formation or when the infection is surrounded by a large amount of necrotic or damaged tissue. They are particularly useful in conjunction with surgical debridement.

Following a fracture, where does the bone get the majority of its blood supply?
After being fractured, bone gets the majority of its blood supply from surrounding soft tissue.
What is an open fracture? Are they all contaminated or infected?
A fracture of bone with exposure to the environment.
They are all contaminated but NOT all are infected or will become infected.

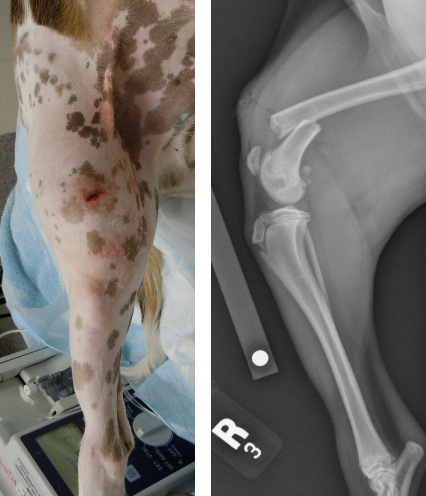
What are the different classification of open fractures? What is this classification based on?
The different classification of open fractures are Type I, II, IIIa, IIIb, and IIIc.
They are classified based on the mechanism of injury, degree of soft tissue damage, configuration of the fracture, and the degree of contamination.
What is a Type I open fracture? What typically causes them?
The wound is less than 1cm, caused from the inside (bone poking out).
Typically seen with low energy traumatic impacts - simple fracture patterns and minimal soft tissue damage.
Of the open fractures, Type I fractures have the least amount of wound contamination, with low infection and complication rates.
What is a Type II open fracture? What typically causes them?
The wound is greater than 2cm, typically caused by external trauma (outside to inside).
There's mild to moderate soft tissue damage and a simple or comminuted fracture pattern with mild contamination.

What is a Type III open fracture? What typically causes them?
Excessive soft tissue damage, highly comminuted, major contamination, typically caused by outside-to-inside high energy trauma (e.g., gunshot).
There are three subtypes of type III open fractures.

What characterizes a Type III-A open fracture?
Adequate soft tissue coverage despite extensive laceration or soft tissue flaps.
What characterizes a Type III-B open fracture?
Soft tissue loss and inadequate soft tissue coverage with periosteal stripping and exposure of bone.

What characterizes a Type III-C open fracture?
Extensive soft tissue damage with damage to the arterial blood supply - arterial blood supply must be repaired to salvage the limb!

What are the principles of management for open fractures?
Prevent infection, soft tissue and bone healing, restoration of anatomy, and functional recovery.
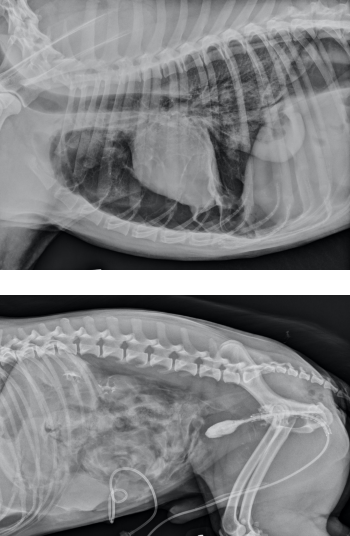
How would you evaluate and stabilize a patient presenting with open fractures?
Obtain a complete history and physical exam. Perform emergency management of life-threatening injuries first.
Many patients with open fractures have multiple injuries. Assess for other injuries and the neurovascular structures.
Open wounds are covered with a sterile dressing and splint to prevent further soft tissue damage and contamination; most open fractures are contaminated with nosocomial organisms.
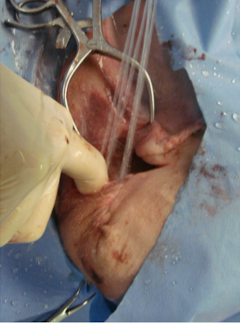
Describe initial wound management and the goal of it.
Initial care is essential to the ultimate outcome of the patient! Open musculoskeletal injuries are emergency surgeries and initial wound management should occur as soon as possible.
The goal is to convert from a severely contaminated wound with avascular tissue to a cleaner wound with improved blood supply.

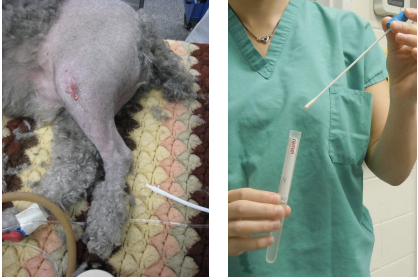
What should be done during initial debridement of the wound?
During initial debridement, deep tissue cultures should be obtained. Do not just swab the wound and skin; a sample of tissue should be submitted along with the swab.
A copious lavage with balanced sterile electrolyte solution should be sustained through the debridement process.

Describe the fundamentals of wound management.
Strict aseptic technique should be practiced. First, the hair is clipped and sterile water soluble jelly is applied to protect the wound. Sterilely prepare the limb for surgery with copious lavage, debridement, and sterile bandaging.
What should be removed during initial debridement of a wound?
Fat and fascia should be aggressively removed while being more conservative with muscle and skin. Tissue with questionable vitality should be preserved and re-evaluated. Bone, ligaments, and tendons should be preserved unless removal is absolutely necessary.

Describe antibiotic therapy for open fracture treatment. What are the general guidelines?
Appropriate and effective antibiotic therapy is paramount and should be started immediately and adjusted after obtaining a culture and sensitivity. Antibiotics ideally should be given IV for the first 72 hours.
Before C&S results come back, patients are started on antibiotics based on general guidelines. Type I open fractures usually involve contamination with aerobic, gram positive bacteria and are treated with a first generation cephalosporin. Patients with type II & III open fractures should be started on broad spectrum antibiotics.

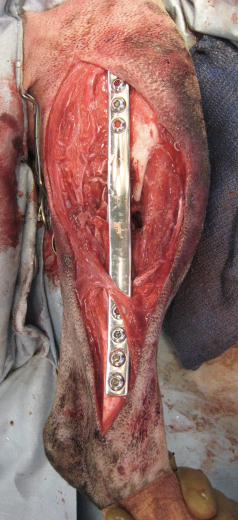
What is the optimal method for fracture repair?
There is no optimal method, but plates/screws and ESF are good choices, while casts/splints and pins/cerclage should be avoided.
ESF has many advantages, including stability with pins relatively distant from wounds, easy access to the wound, can be placed minimally invasively (decreased trauma to soft tissue), and implants can be removed once fracture is healed.

Describe open wound management for open fractures.
Every time the dressing is changed/replaced, sterile aseptic technique should be used.
Repeat debridement and lavage. Bandage changes should be done more frequently in the beginning, especially for Type II open fractures.

What should be considered during fracture repair and bandaging in terms of post-op care? What is the goal of post-op care?
Planning of fracture repair and bandage should allow for the ability to perform rehabilitation exercises, which optimize joint and soft tissue function during healing.
The goal of post-op care is early return to function.

What is osteomyelitis? How can it be classified?
Inflammatory condition affecting bone, usually due to an infectious cause such as bacterial (most common), fungal, or occasionally viral.
They can be hematogenous (tend to be young animals with weak immune systems) or post-traumatic (acute vs. chronic).

What is the pathogenesis of osteomyelitis? What are some host risk factors?
Due to ischemic event (e.g., fracture, surgery) and concurrent bacterial colonization.
Systemic host risk factors are hypovolemia, malnutrition, obesity, endocrine diseases, and immunosuppression.
Local host risk factors are unstable fracture, tissue metabolism, foreign material, and dead space.

What is a bacterial glycocalyx? What is the process?
A network of polysaccharides lying outside the outer membrane of the gram-negative cells and outside the peptidoglycan of gram-positive cells.
The bacteria produce exopolysaccharide polymers which assist the cell to firmly adhere to tissues or implants. Bacteria produce inside the glycocalyx and form colonies that coalesce to form a biofilm.
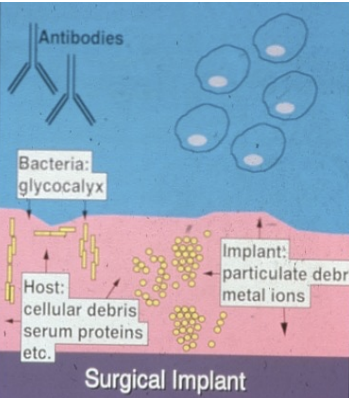
What happens when a biofilm forms? How does this affect antimicrobial therapy?
Biofilms modify the local environment in favor of the microbe. They concentrate nutrients and prevent identification of surface antigens, protecting bacteria from surfactants, opsonic antibodies, and phagocytes.
They protect the bacteria from antimicrobial therapy and influence antibiotic sensitivity. Biofilm bacteria are more resistant, perfusion of antibiotics is impeded, and there's a quiescent growth pattern of biofilm microbes.

Describe chronic post-traumatic osteomyelitis.
It’s the most common form of osteomyelitis.
It’s a disease caused by ischemia and bacteria inoculating the fracture site. It develops weeks to years from the time of contamination.
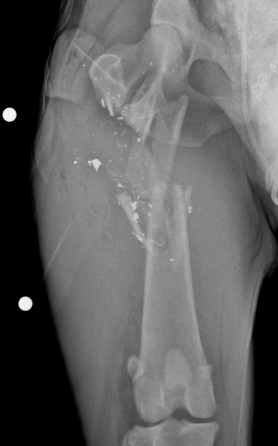
Explain the diagnosis of osteomyelitis.
Diagnosis is made through history (infection, trauma, surgery), clinical signs, changes on radiographs, and culture and sensitivity (definitive diagnosis).
There is rarely systemic changes and signs tend to be localized (e.g., draining tracts, lameness, pain).
Advanced diagnostics are not commonly used to diagnose osteomyelitis.
What are some changes seen on radiographs for osteomyelitis?
Variable changes are seen in the early stages. This includes bone lysis, periosteal proliferation, loose bone, broken implants, and non-viable bone fragments.
When should open fractures be repaired? What does this constitute?
Fracture repair can occur immediately following wound debridement or once stable and a healthy soft tissue envelope is constructed.
To prevent reinfection, fracture repair should be treated as a “new” surgery, meaning new equipment, drapes, gowns, gloves, etc.
Describe the process of obtaining a sample for C&S for osteomyelitis.
Do NOT culture skin the skin, but rather obtain deep tissue samples! Sterile aspiration can performed using ultrasound if needed.