12. anthrax (bacillus)
1/18
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
19 Terms
bacillus anthracis morphology
gram positive rods
spore-forming
how is sporulation triggered?
can be triggered by low oxygen, oxidative stress response, nutrient limitation, etc.
predisposing environmental conditions to anthrax
alkaline soils; outbreaks associated with flooding
dry warm seasons followed by moderate to heavy rain events
post-flood organic detritus and/or short, dry grazing grasses
topological lows (waterholes or riverbanks)
loose, unconsolidated soils rich in calcium and nutrient content
how is anthrax transmitted?
ingestion of spores in environment
peracute clinical signs
sudden death and rapid decomposition
incomplete rigor mortis
**ruminants most susceptible, but can happen in horses
acute clinical signs
edema, bleeding from body orifices, poor clotting
fever, staggering, trembling, convulsions, excitation/depression
difficult/increased respiration
horses: swelling neck — colic signs
subacute/chronic clinical signs
localization in pharyngeal tissues
anorexia, vomiting, and diarrhea
**pigs, dogs, cats
anthrax transmission cycle
animal grazing in infested field ingests anthrax spores → anthrax infection in animal → animal death & bleeding from orifices contaminates environment → b. anthracis bacteria convert into spores and infest agricultural fields
**spores can survive for decades
anthrax pathogenesis
ingested spores invade epithelium directly or are phagocytosed → cross epithelium by transcytosis through epithelial cell or within phagocyte → travel to lymph nodes → germinate into vegetative bacteria → produce capsule and exotoxins → cause edema and clotting disorders to rapid death
**neutrophils are not involved in the pathogenesis of anthrax
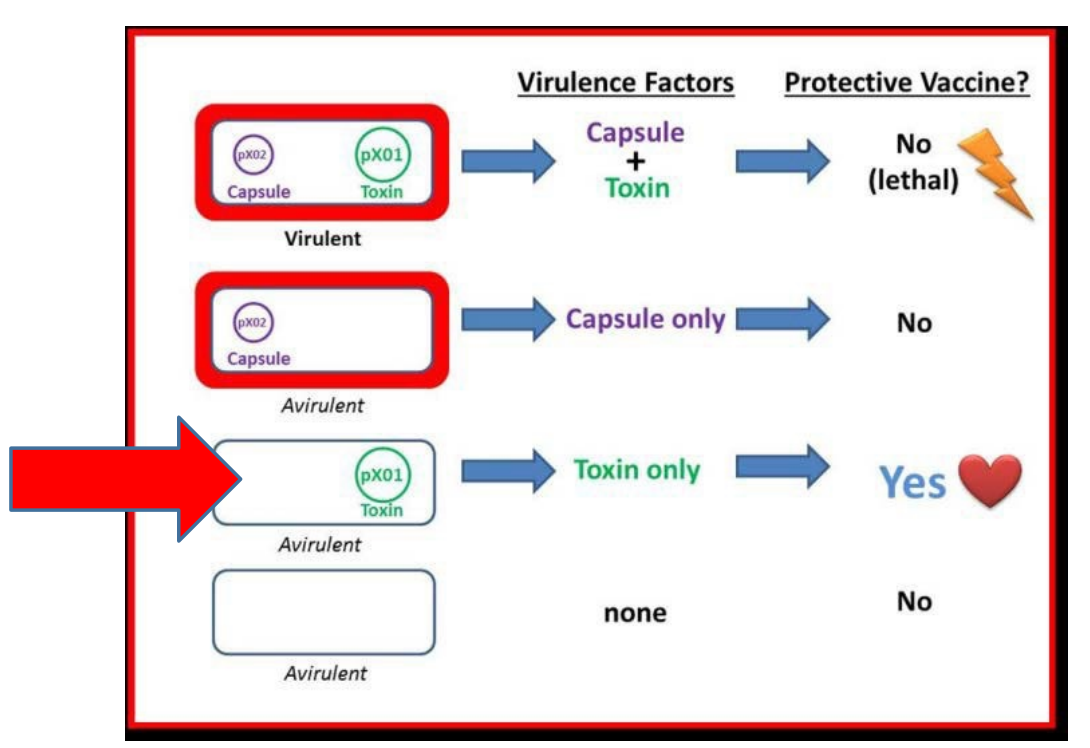
what plasmids are essential for B. anthracis to be virulent?
pXO2 — capsule gene (antiphagocytic)
pXO1 — contains protective antigen, lethal factor, and edema factor → expresses lethal toxins
what 3 genes in pXO1 contribute to toxin production?
protective antigen (PA): binds to host cells & helps introduce toxins into host cell
lethal factor (LF): toxin that inhibits host cell signaling → cell death
edema factor (EF): edema toxin also disrupts host cell signaling
in vivo, responsible for hemorrhagic lesions in multiple organs
major anthrax clinical signs (from summary slide)
sudden death
bleeding from orifices
diagnosing anthrax
necropsy NOT recommended!!! (contaminate environment)
gram stain & capsule stain of blood and organ smears
culture
PCR assays to detect plasmid genes
REPORTABLE DISEASE
anthrax treatment/prevention
treatment: penicillin & vaccination
prevention: annual vaccination recommended — Sterne’s modified live vaccine
what is sterne’s spore vaccine?
live, avirulent strain of anthrax
produces exotoxin (pXO1) but NOT capsule (missing pXO2)
delivered as spore suspension (immunogenic)
germinates, releasing exotoxin → immune response to toxin and surface antigens
not suitable for human use
why doesn’t the sterne’s spore vaccine cause severe disease/death?
infection is controlled and eliminated by the animal because the agent is missing a key virulence factor, the capsule that resists phagocytosis (pXO2)
bacillus cereus source
environment; causes opportunistic infections
bacillus cereus virulence factors
produces enterotoxin (hemolysin) & emetic toxin (cereulide)
what kinds of diseases can bacillus cereus cause?
acutely gangrenous mastitis in cows
predisposing factors = surgery or intramammary infusions that introduce bacteria into gland
food poisoning