04 - Cornea 1 (corneal ulceratio
1/60
Earn XP
Description and Tags
Be familiar with the normal anatomy of the cornea and its appearance on histology • Be able to define corneal ulceration and have a basic understanding of normal corneal healing • Know the common clinical signs and causes of corneal ulcers • Understand how to distinguish uncomplicated superficial ulcers from deeper stromal ulcers and descemetocoeles • Know how to recognise SCCEDs, and be familiar with the use of diamond burrs and soft corneal bandage lenses in the treatment of this condition • Understand how ulcers may progress and deepen, and how to perform corneal cytology • Be familiar with the use of antimicrobials and anticollagenases in the medical management of stromal ulcers • Be able to recognise keratomalacia (melting) • Know when to recommend referral for treatment of ulcerative keratitis, and how to recognise corneal perforation
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
61 Terms

corneal anat
name the 4 lters
1) Epithelium
2) Stroma
3) Descemets membrane
4) Endothelium
corneo-scleral coat
outermost fibrous coat of the eye
junction between the cornea and sclera
limbus
avascular cornea nutrient supply
aqueous,
perilimbal capillaries
tear film
cornea redlex
reflection of light in the cornea
sharp and clear indicating an uninterrupted surface
clear, smooth tear film
epithelium
Non-keratinised, stratified squamous epithelium
Rapid turnover of cells
Forms a natural barrier to ingress of water from the
tear film.Protects from colonization with bacteria/fungi
Dependent on a normal and properly distributed tear
film to function well.Basal cells attach to a thin basement membrane via
hemidesmosomes, anchoring the epithelium to the
underlying stroma
Stroma
90% of corneal thickness
composed of collagen lamellae, separated by ground substance and modified fibroblasts (keratocyte).
regular arrangement of lamellae is critical for transparency—> cornea must be kept dehydrated
superficial stroma richly innervated by opthalmic division of CN V (trigeminal)
descemients membrane
basement membrane of the endothelium,
produced throughout life,
elastic and fairly strong,
does not stain with fluorescein
endothelium
Maintains corneal dehydration through active transport of sodium into the aqueous humour (Na+/K+ ATPases).
Poor regenerative capacity
Decreased cell numbers with age
corneal epithelium importance
provide protective barrier
resistant to bacterial colonisation
prevents water entering the cornea
corneal ulcer
Loss of full thickness of the epithelium (most often as a result of mechanical trauma) exposes the underlying stroma (± loss of stroma)
can progress to full thickness and perforation
cornela ulcer stain
mechanism
use fluorescein stian
only strins exposed stroma.
Epithelium or detdcements don’t stain fluorescein
limbus is where corea meet sclera where all stem cells are.
ulcer: simple and complicated
siple: within 7 days. non-infected, no ongoing underlying cause
complicated: fail to heal within 7days ,(ongoing re-eplitheliadlsica)
basic understanding of normal corneal healing
how logng should superficial ulcer need to heal
epithelial defect healing usually rapid
migration of adjacent epithelial cell coevering defect
then replicate to restore full thickness
superficial should heal within few days
stromal defect healing— scute superficial
Avascular healing (acute superficial stromal loss):
Neutrophil infiltration
New collagen secretion from activated keratocytes at the wound margin
deep/ chronic/ infected stromal ulcer healing
vascular healing
extensive early cellular infiltration
subequent vascualr invasion—> fibrovacualr granultion tissue at ulcer site
corneal ulceration: clinical signs
marked pain and discomfort (blepharospasm)
care with CNV damage-→ sensation may be affected
discharfege, epiphora and photophobia
+ lacrimation—> epiphora
mucoid/ mucopurulent discharge common in melting/ infected ulcers
Conjunctival hyperaemia.
Variable localised corneal oedema I
irregularity of the surface.
Neovascularisation and cellular infiltration of the cornea is common with chronicity
Reflex anterior uveitis
Causes of corneal ulcers
External trauma / FB
Hair/eyelash trauma – entropion+trichiasis, distichiasis, ectopic cilia
Infection (secondary) – feline herpesvirus, bacterial colonization n
Tear film abnormalities (KCS)
Exposure keratopathy
SCCED
epithelial bullae rupture (secondary to marked corneal oedema)
cholesterol/ calcium deposit—> erosion (rare)
cause of cornela ulcer
trauma due to suture contact
• Nylon suture in the upper eyelid
• As the dog blinks, the suture abrades the cornea
• granulation tissue—> going on for a considerable time
cause of cornela ulcer
trauma due to hair contacting the corneal surface
• Trichiasis due to entropion is a common cause of ulceration

cause of corneal ulcer?
ectopic cillia—> contacting corneal surface
less commonly, but usually cause a corneal ulcer when they do
Young dogs, usually upper lid
Linear corneal ulcer in the cornea corresponding to the cilia
gunk and mucus trapping fluorescence around area
cause of corneal ulcer?
Nasal fold trichiasis and distichiasis (lashes on meibomian galnd) are common
aren’t always associated with corneal ulceration

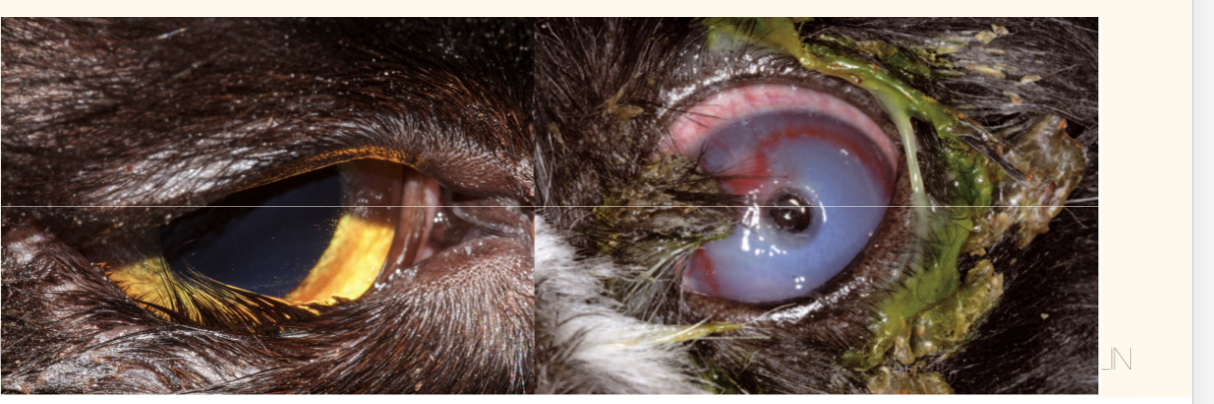
cause of corneal ulcer?
exposure keratopathy
Central corneal damage
due to inadequate protection of thencornea
by the eyelids and/or third eyelid
compounded by inadequacy of pr-renal tear film
causes of exposure keratopathy
Prominent globe with poor lid closure
brachycephalic breeds often lagophthalmos – an inability to close the eyelids
chronic glaucoma: buphthalmus (globe enlargement)
retrobulbar masses—> exophthalmos
Facial nerve CN7 paralysis
more prominent more severely affected
loss of motor function to eyeylid—> cannot bink
Trigeminal nerve cN5 paralysis (check PPR, direct + indirect)
absent corneal sensation —> severe keratitis
Common complication of globe proptosis as nerve gets stretched.
brachycephalic breeds have reduced corneal sensation.
entropion, trichiasis, distichiasis
how does ruptured epithelial bulla cause corneal ulceration and what do you expect upon investigation
large area of corneal oedema
restricted area of fluorescein uptake—> small ulcer, likely a ruptured sub-epithelial bulla
Fluorescein staining is less intense when there is corneal oedema
what is this cause of corneal ulcer
corneal cholesterol/calcium deposit:
rare, refer
Superficial ulcer- only the epithelium is los
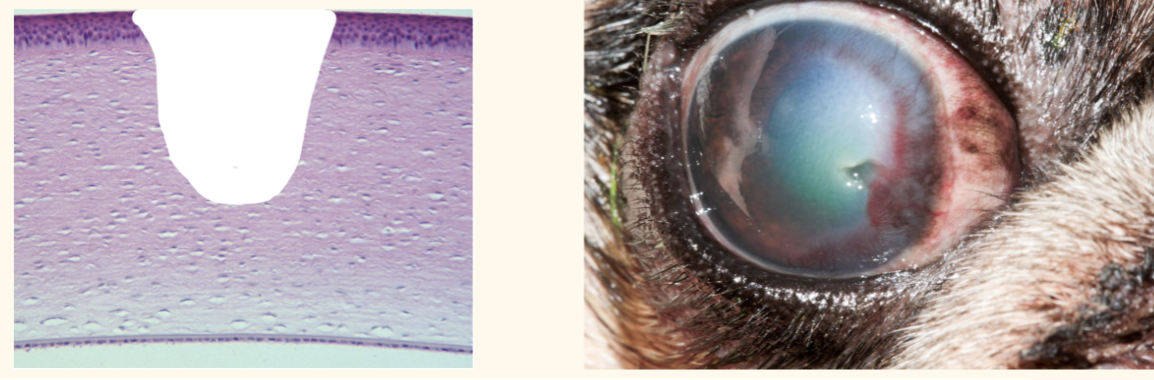
stromal ulcer/ deep ulce
ulcer is deeper than just the epithelium
varying degrees of stromal loss
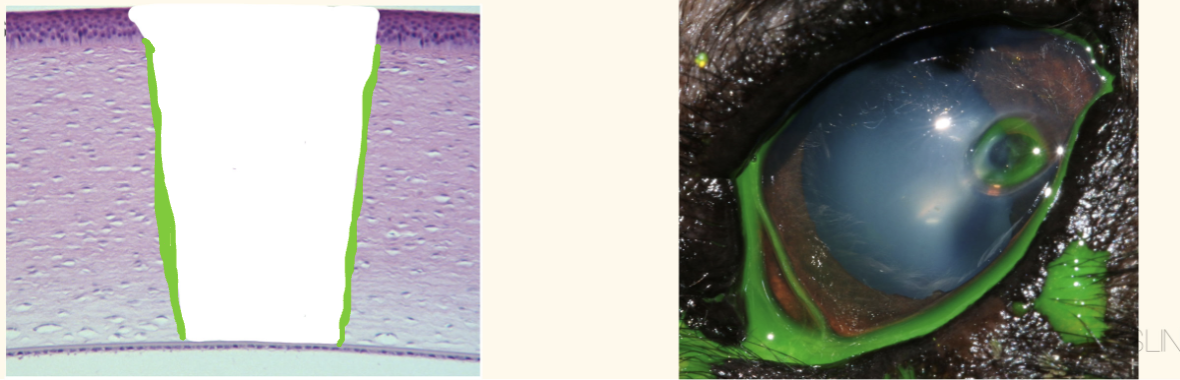
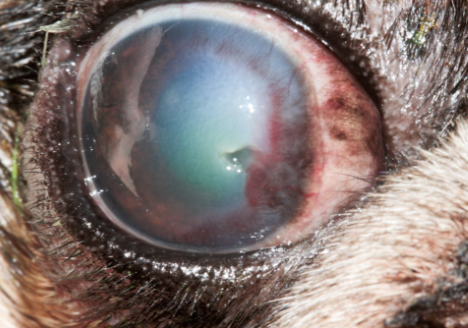
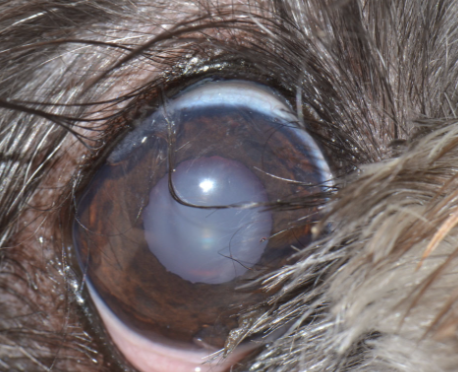
Descemetocoele
ulcer extends through the entire stroma
reach Descemets membrane
descement membrane does not take up fluoroscien—> ring shape uptake
cornea is in imminent danger of rupture
how deos ulcer progress
Progressive loss of stroma: enzymatic degradation (collagenases and proteases)
Some naturally produced by neutrophils; others are from infection (bacteria; especially Pseudomonas and Streptococcus)
potentiated by corticosteroids
ulcer vs steroid
contraindication
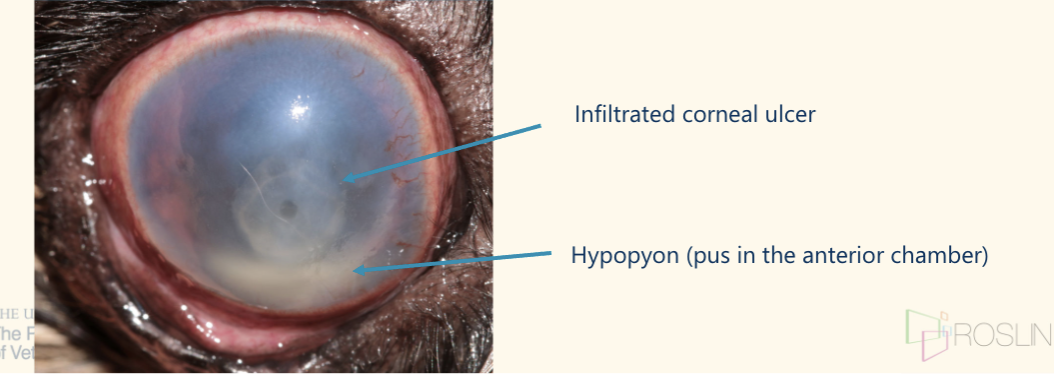
____ with _____ or ________ results in a ______-tinged appearance
Infiltration with bacteria or neutrophils results in a yellow-tinged
appearance
how do you know bacteria present
Corneal cytology
topical analgesia
roll ‘Cytobrush’ or bacteriology swab along ulcer
along the edge, avoiding the deeper centre;
care in very deep ulcers/ Descemetocoeles
Roll swab onto a glass slide and ‘Diff Quick’
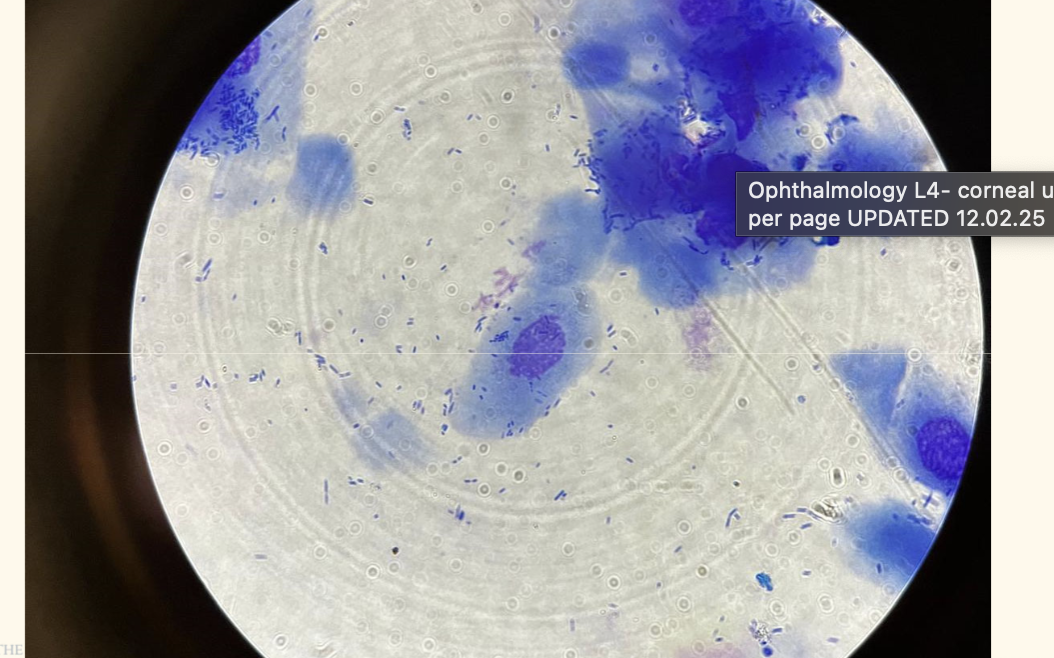
what do you do folowing corneal cytology
what Abx will you give if cone/ rods?
Directs immediate antibiotic use whilst awaiting culture and
sensitivity results
cocci: chloramphenicol drop
rods: : fluoroquinolone (ofloxacin aka exocin)
name most comon secondary bacterilainfection. name 2 gram +ve and 2 gram -ve
Gram positive cocci:
Staphylococci
Streptococci
Gram negative rods
Pseudomonas
E.coli

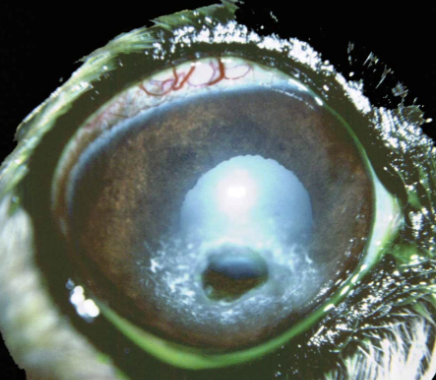
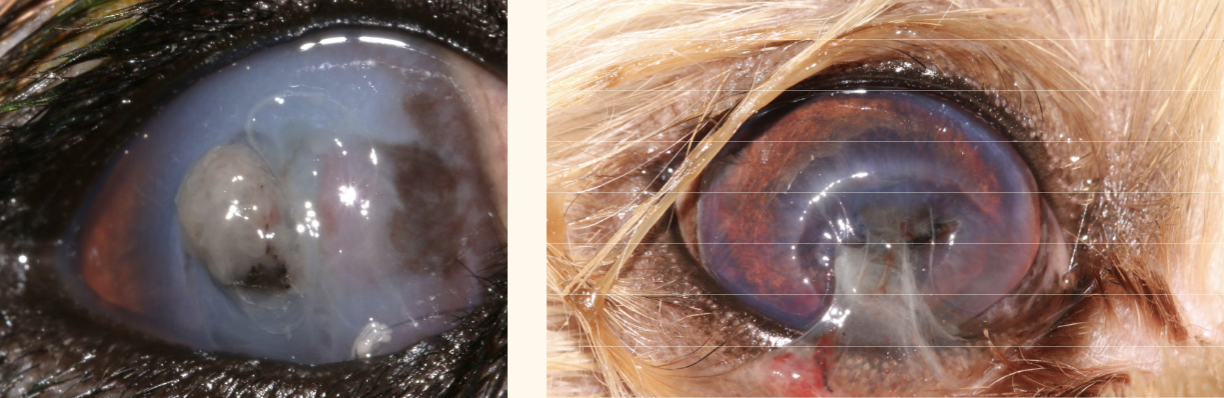
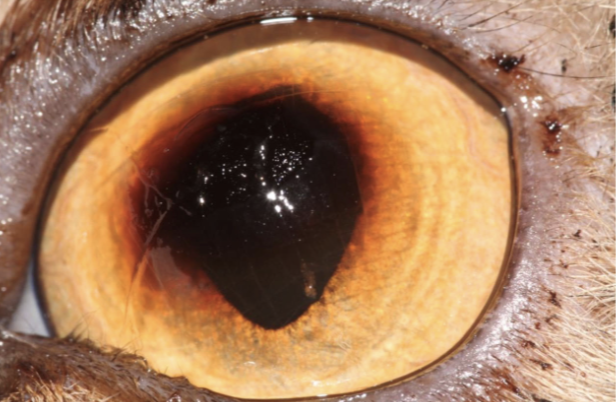
how would you describe thiss
melting ulcer, keratomalacia
melting ulcer aka keratomalacia
edge of ulcer: ____
deteriorate _____
edges of the ulcer appear gelatinous
can start when ulcer still shallow—→ acutely deteriorate
simple cornela ulcer tx: 6
most acute superficial ulcer heals quickly once cause is removed
however infection consequences are serious—> topical Abx until fluorascene negative.
Chloramphenicol drops 4x daily (or ointment 2x daily)
Analgesia
Systemic NSAID unless contraindicated
+/- paracetamol, tramadol, gabapentin if required
proxymetacaine contraindicated—> delay corneal healing, decrease protective mechanism like tearinng and blinking
Topical lubricant
increase rate reepithelialisation
+/- single drop of atropine (pupal dilation)
– Improves ‘reflex uveitis’
– reduce tear production—> contraindicate if KCSProtective collar
Recheck in 2-5 days
simple corneal ulcer fails to heal within 7 days
re‐classified as a complicated’ corneal ulcer
underlying reason for failure of re‐epithelialisation identified and addressed
why could a simple ulcer not heal?
The underlyingcause has not been addressed
Ongoing trauma? (entropion, ectopic cilia, foreign body etc.)
KCS?
Exposure keratopathy?
Secondary infection with bacteria (or fungi)
corneal cytology
ulcer is SCCED
The patient is immunosuppressed/ immunocompromised
Superficial to mid-stromal ulcers can usually be managed ____.
what else would you do?
medically, but can progress quicky
hospitalisation for close monitoring
intensive topical treatment
injectable analgesia (e.g. opioids)
typical regime for a stromal cornela ulcer ** exam
most common cause of stromal ulcer progression: secondary infection
—>corneal cytology and broad spec abx while C+C. chloramphenicol and ofloxacin can be used together if indicated.
Antibiotic drops:
base on cytology result, q 2-4 hours
fuscidic acid (Isathal) NOT an appropriate choice for stromal or malacic ulcers
**Anti-collagenase:
Autologous serum/plasma is the anti-collagenase of choice
Apply 10 minutes after the antibiotic, same frequency
Analgesia
Oral NSAID +/- paracetamol, gabapentin, tramadol etc.
+/- opioid if required
Topical atropine to effect (q24h until pupil is dilated); care in KCS
monitor q24-48h
malacia, deep ulcer (>50%) and descemetocoele
refer as emergency
may require corneal graft sx
what is SCCED
Spontaneous chronic corneal epithelial defect (‘indolent’ or ‘Boxer ulcer’)
superficial ulcer
failure of adhesion of epithelium to underlying stroma—> peel back readily
rarely infected
middle age to older animal
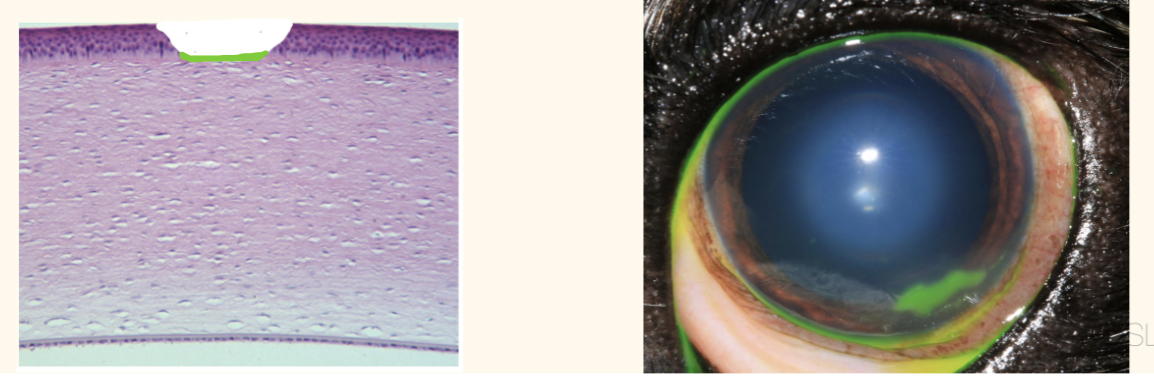
histopathology of SCCED
failure of adhesion of the epithelium to the superficial stroma
abnormal, thin, hyaline membrane on the exposed stromal surface, effacing the normal epithelial BM.
flap or underrun edge at the ulcer margin
in 3 words describe scced tx
medical, surgical, ±contact lens
SCCED treatment : medical, surgical, others
same as simple crneal ulcercorneal medically
Chloramphenicol drops 4x daily (or ointment 2x daily)
Analgesia
Systemic NSAID unless contraindicated
+/- paracetamol, tramadol, gabapentin if required
proxymetacaine contraindicated—> delay corneal healing, decrease protective mechanism like tearinng and blinking
Topical lubricant
increase rate reepithelialisation
+/- single drop of atropine (pupal dilation)
– Improves ‘reflex uveitis’
– reduce tear production—> contraindicate if KCSProtective collar
Recheck in 2-5 days
SCCED treatment: surgical
prep cornea prep the cornea with 1:50 povidone iodine solution
debribement of loose epithelium (mostly done in dogs, cats develop sequestrum easily esp with grid keratotomy
Debride with cotton buds ~50% success
Keratotomy (grid or punctate) ~80% success
Diamond burr debridement ~80% success
Superficial keratectomy
±soft contact lens in conjunction
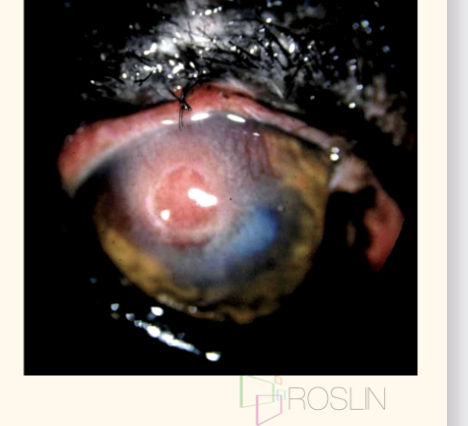
recognising corneal perforation
Acutely painful
yelp in pain, keep eye completely closed
Excessive ‘tearing’ or wetting of the face below ulcer
Perforation site often plugged with clotted aqueous (+/- haemorrhage)
iris Appears as tan, red or pigmented bulging mass at the centre of an ulcer
—>Refer as an emergency for corneal graft or enucleate
care in cotton bud debribement
must remove all loose epithelium
ulcer size increase is ok, dont worry
normal epithelium should firmly attach
Superficial grid keratotomy
25G needle to produce superficial scratches in a grid pattern
Scarring may result

Contraindicagion: grad keratotomy in cats
cats will often develop sequestrum post grad keratotomy
Diamond burr debridement
Easy to use in a conscious patient
Relatively ‘safe’ option
Rarely, melting ulcer is a complication
Soft corneal bandage lens use in tx
Improves comfort
Reduces healing time
Retention can be an issue
temporary tarsorrhaphy suture to improve if needed
contraindication for SCBL
stromal/ malacic/ infected ulcers
at least how long to is needed between debridement?
at least 7-10 days
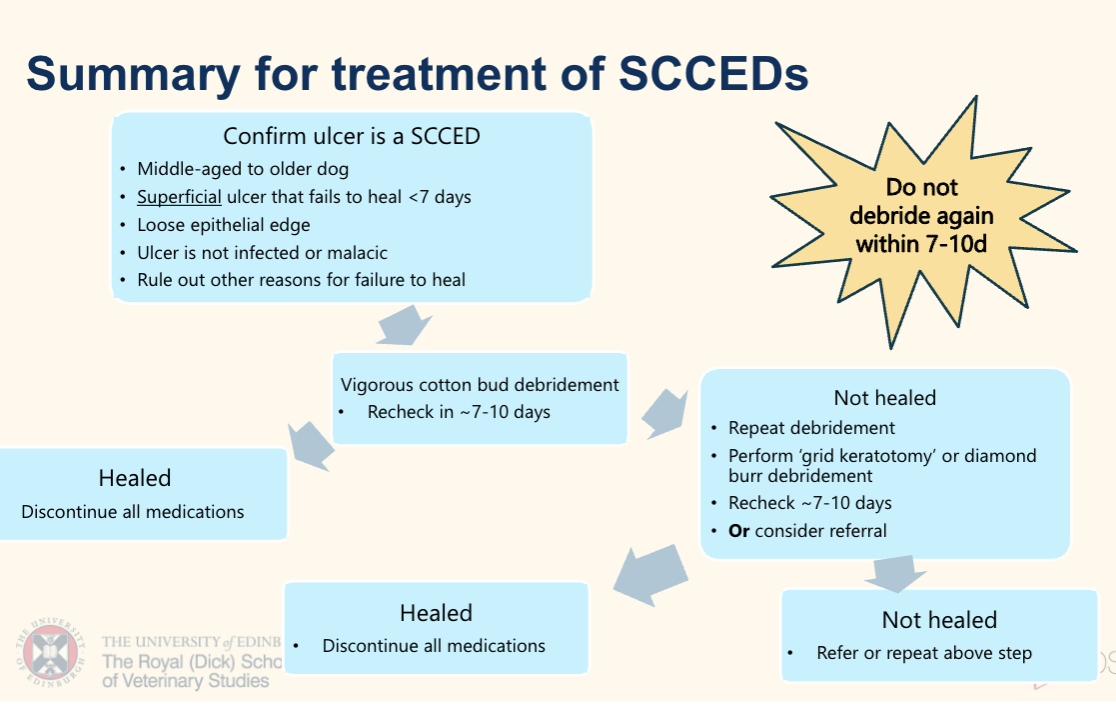
describe SCCED tx in diagram