5-Hypothalamus and Pituitary Gland
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
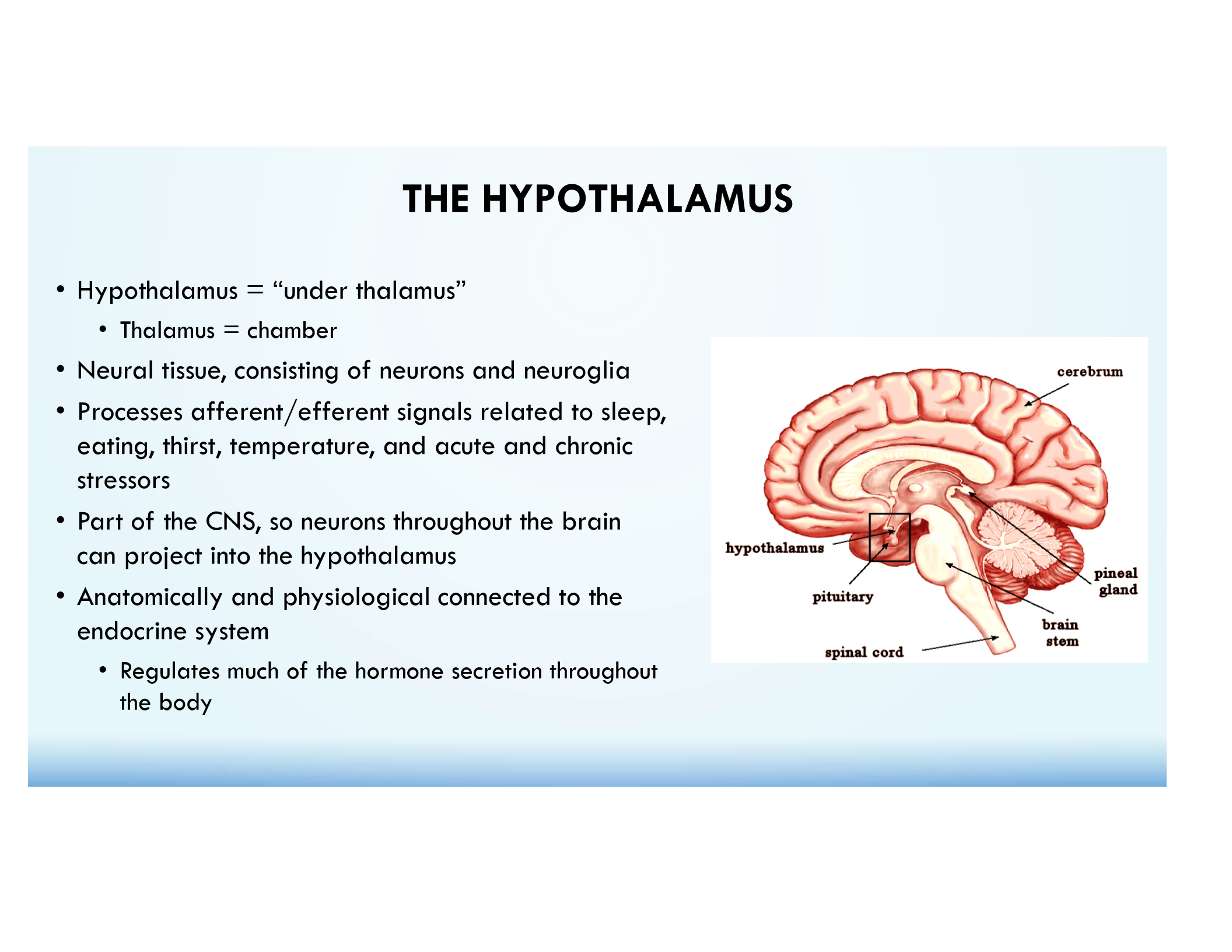
Hypothalamus
Neural tissue that regulates hormone secretion, temperature, thirst, hunger, sleep, and stress.
Anterior Pituitary (Adenohypophysis)
True endocrine tissue; synthesizes & secretes hormones in response to hypothalamic signals.
Main blood supply = Superior Hypophyseal aa.
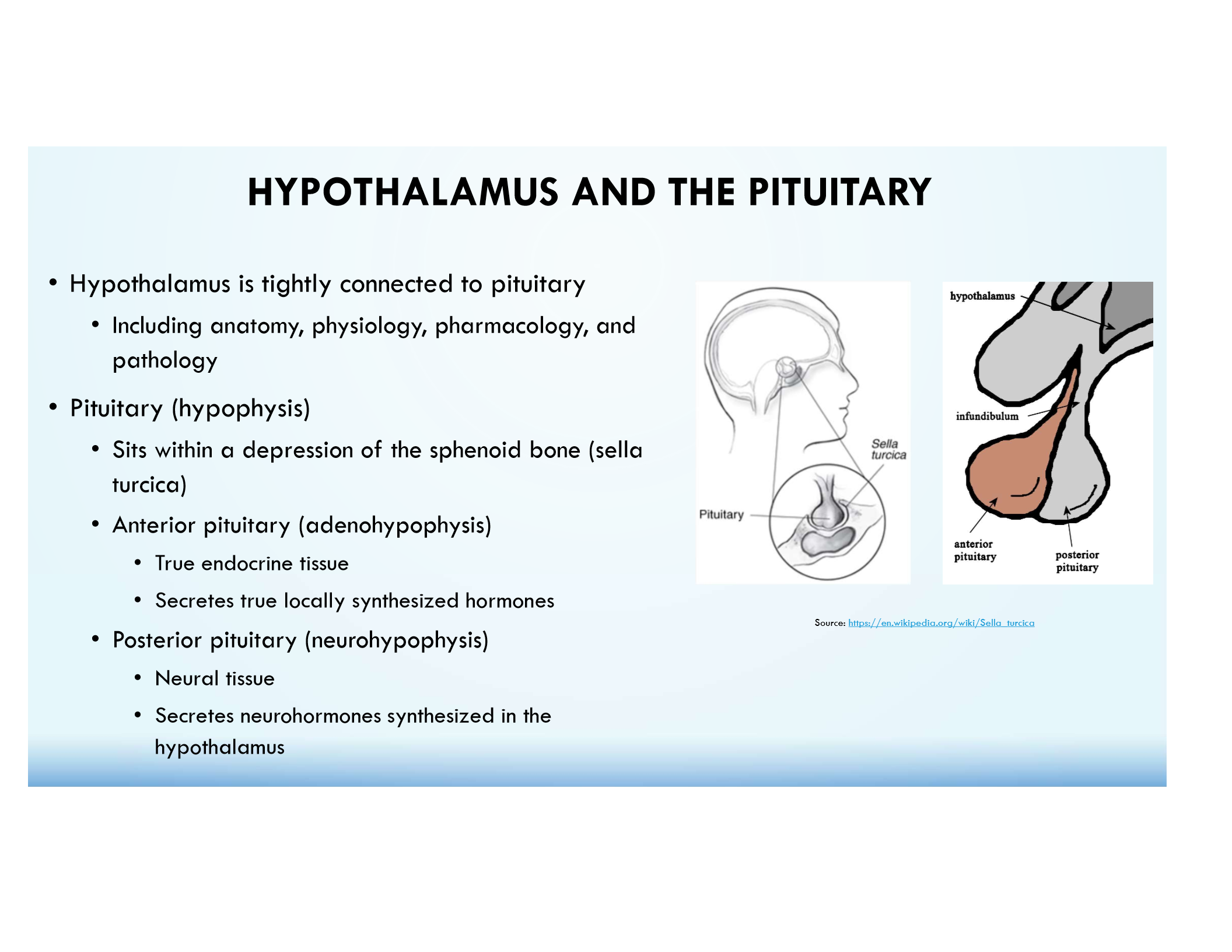
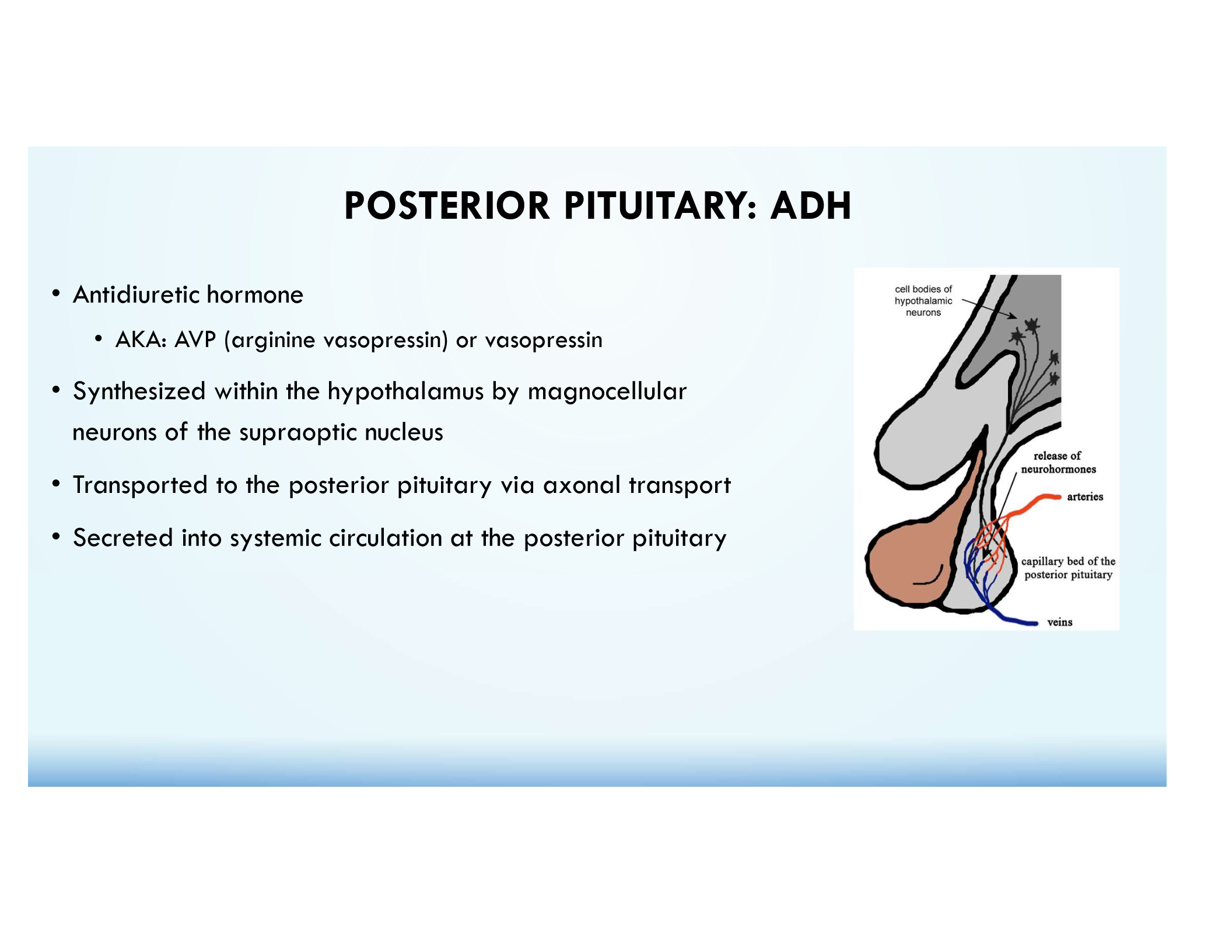
Posterior Pituitary (Neurohypophysis)
Neural tissue that stores & releases hypothalamic neurohormones (ADH & Oxytocin).
Main blood supply = Inferior Hypophyseal aa.
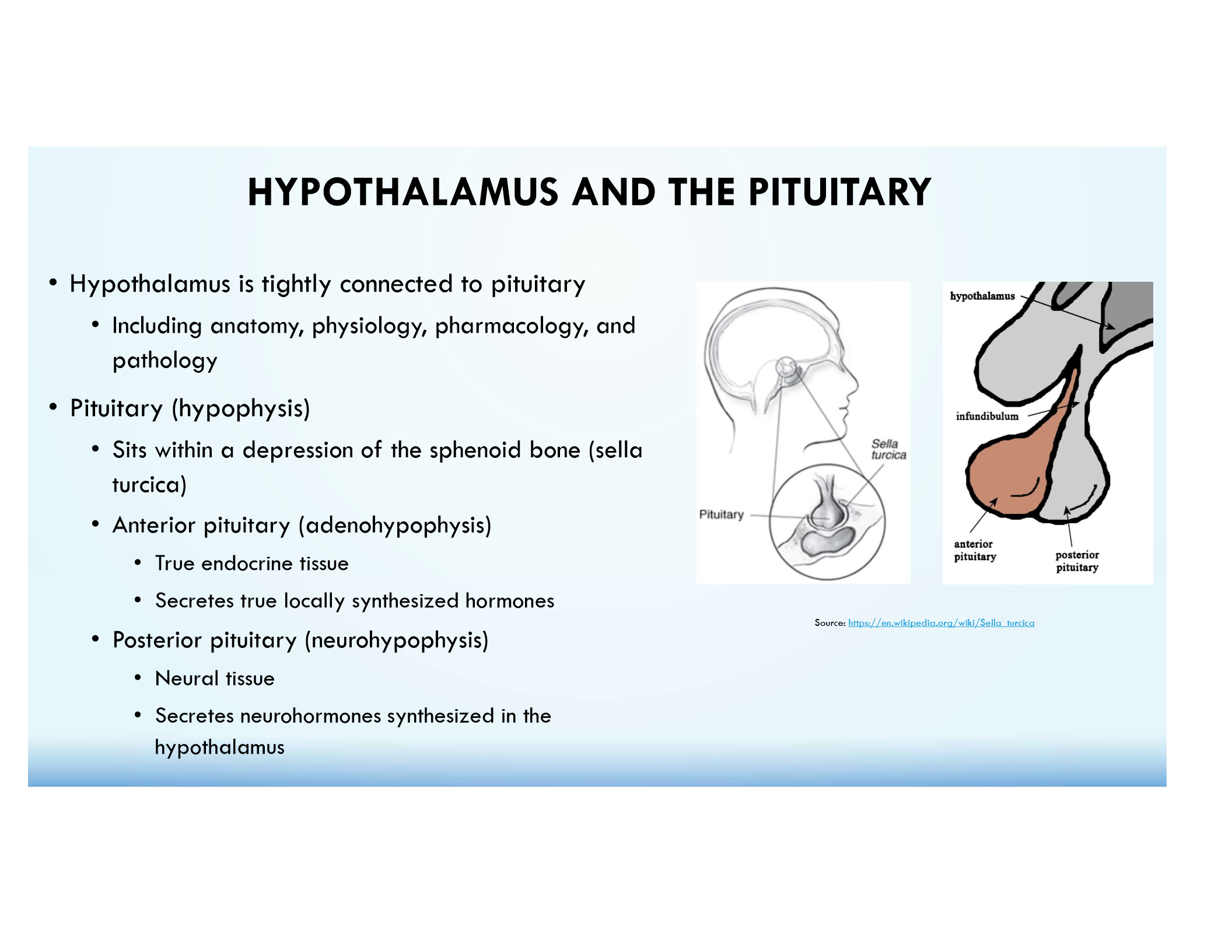
Sella Turcica
Depression in the sphenoid bone where the pituitary sits.
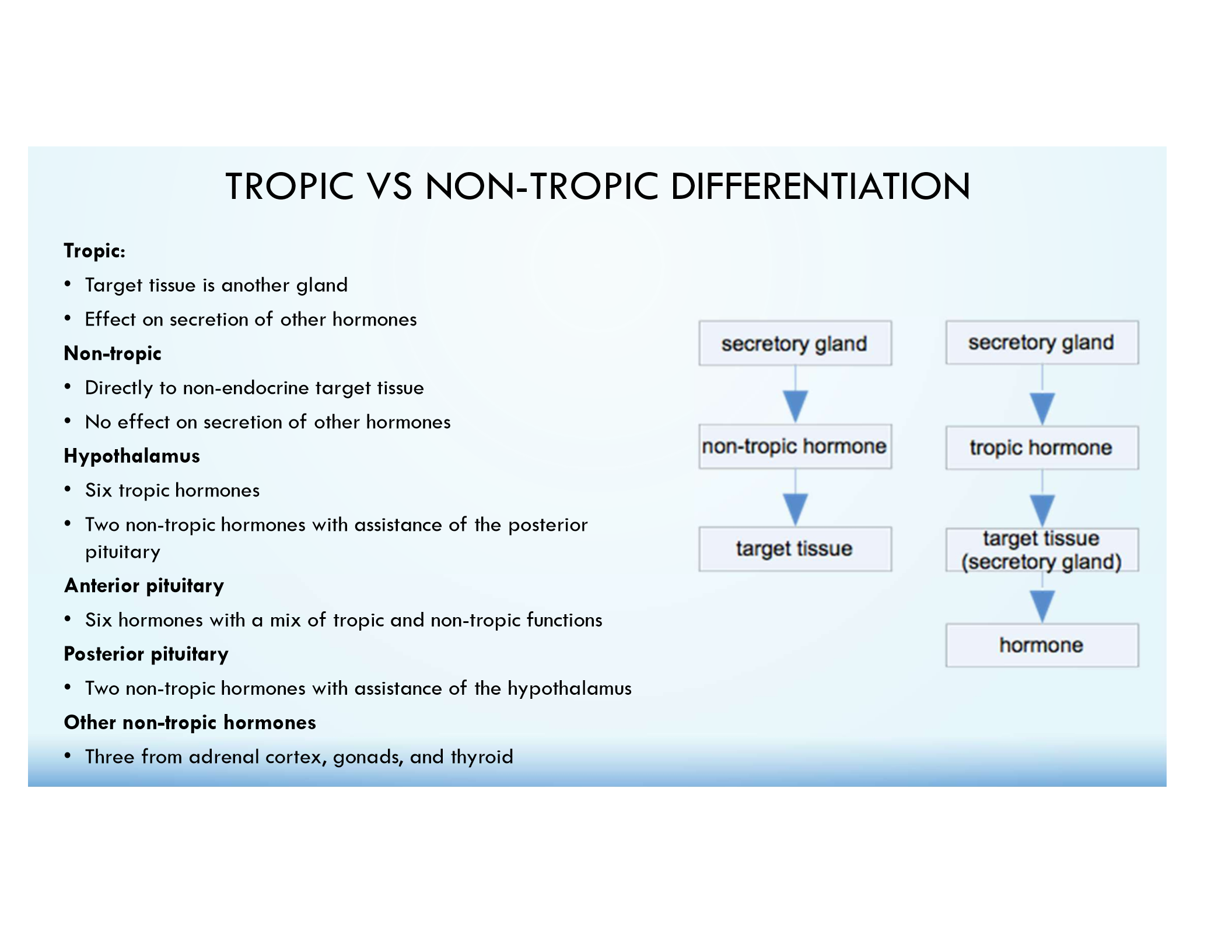
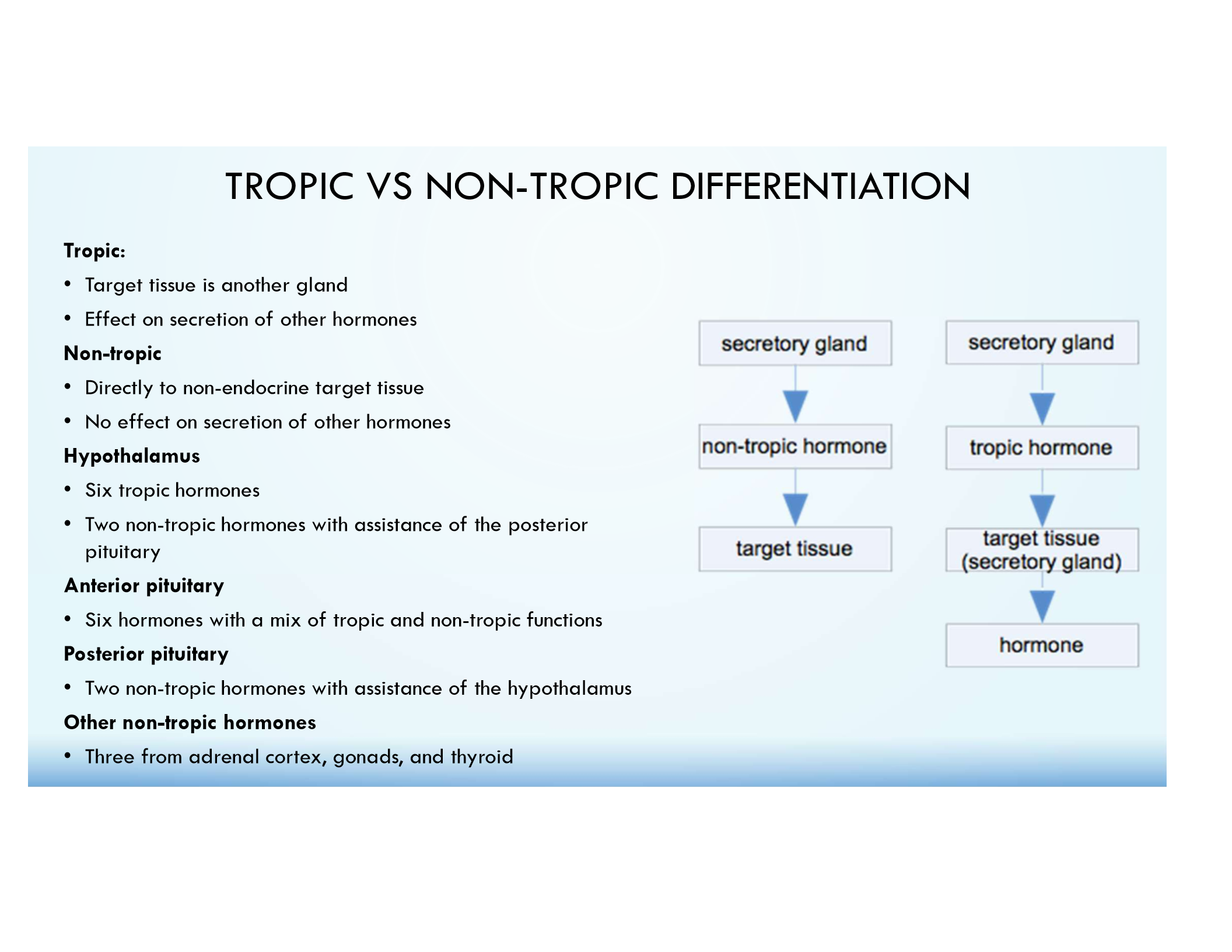
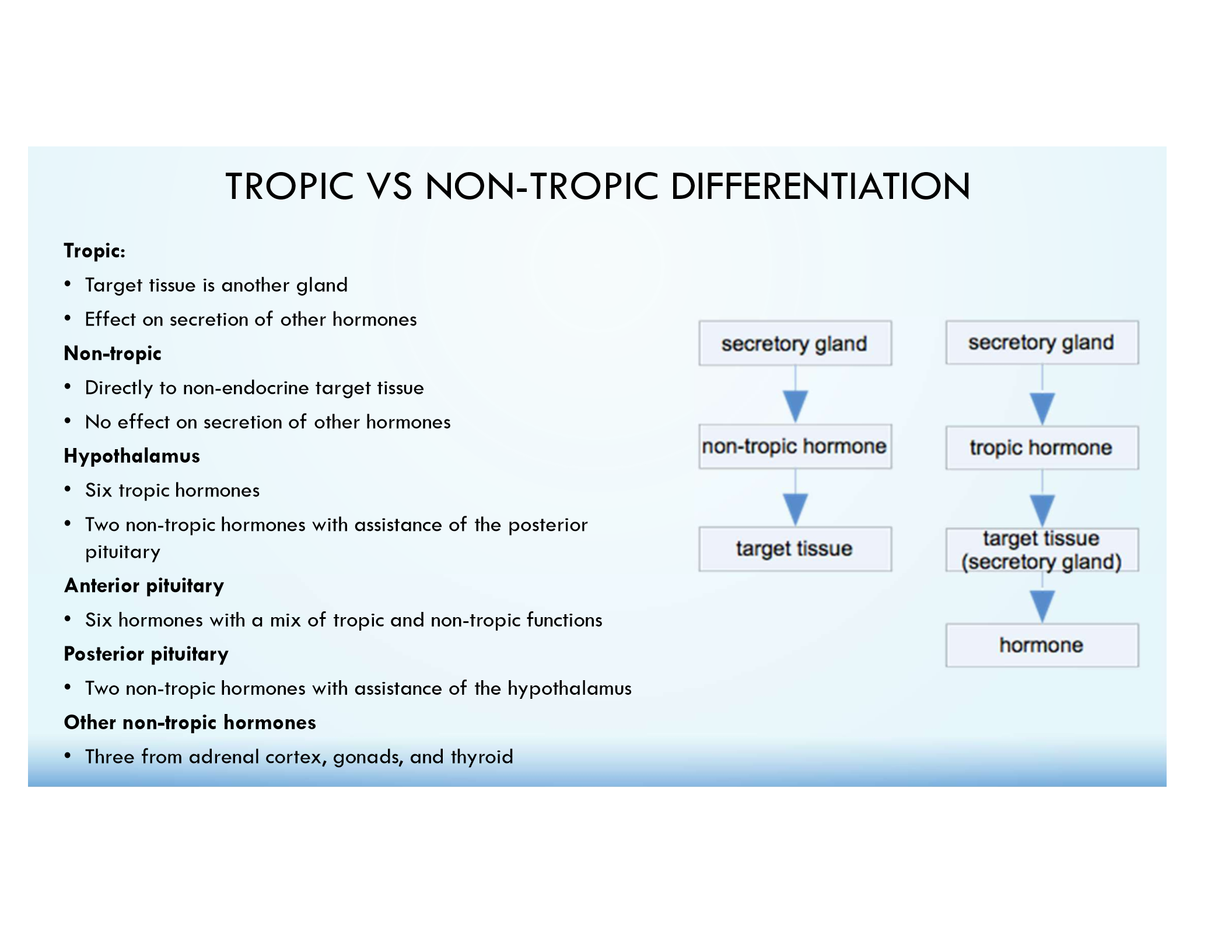
Tropic Hormones
Act on other endocrine glands to stimulate hormone release.
Examples of Tropic Hormones
TRH
CRH
GnRH
GHRH
TSH
ACTH
FSH
LH
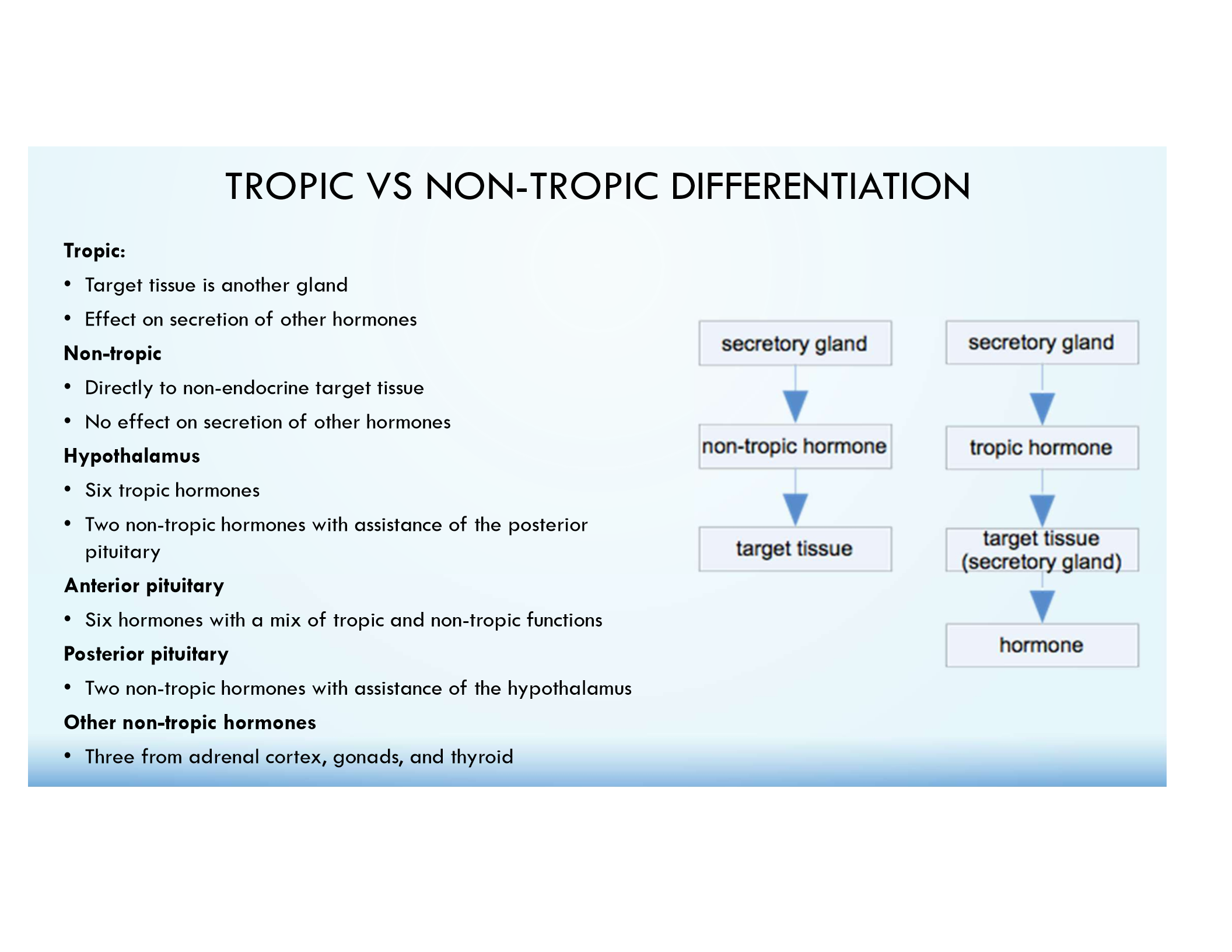
Non-Tropic Hormones
Act directly on target tissues.
Examples of Non-Tropic Hormones
Prolactin (PRL)
Oxytocin
ADH
GH (direct effects)
Cortisol
Estrogen
Testosterone
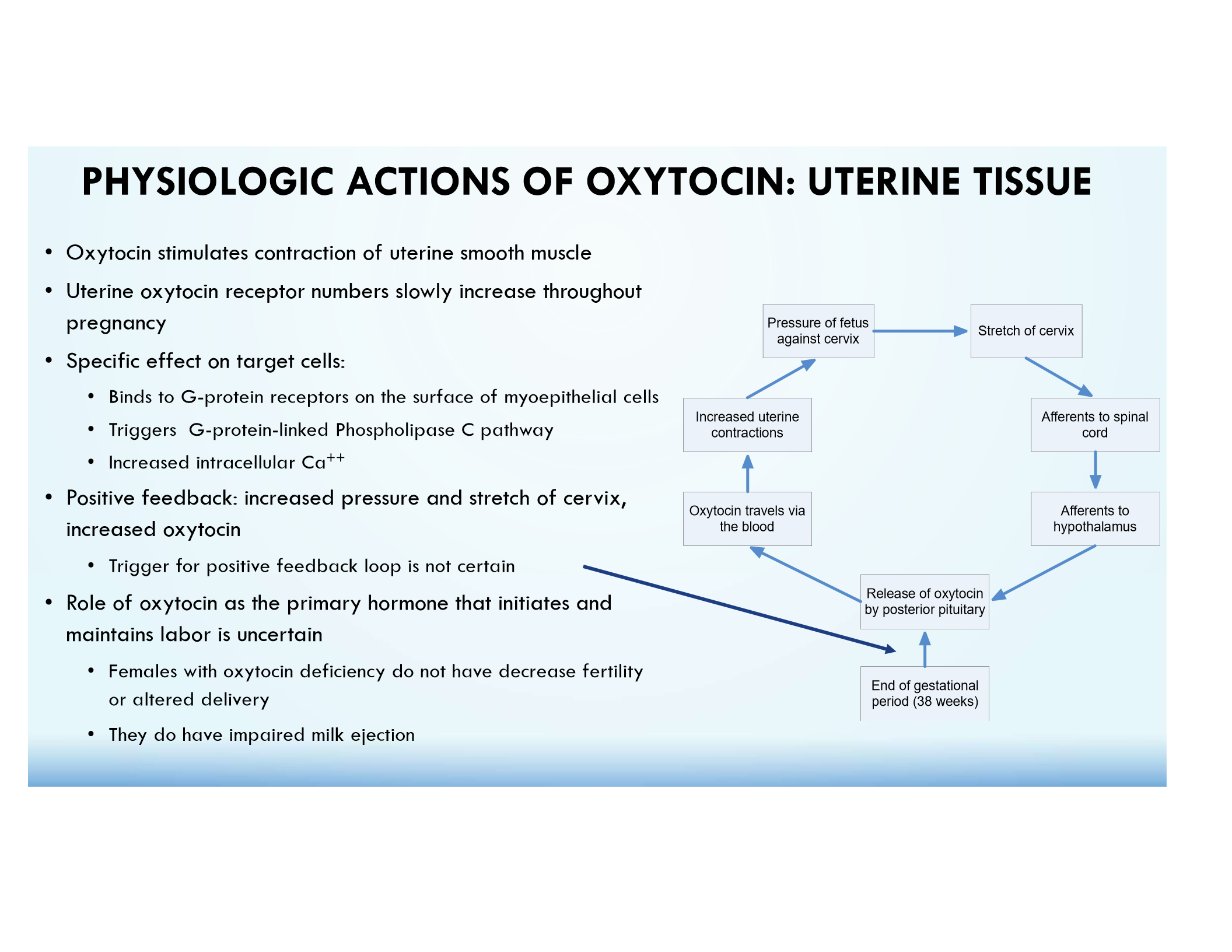
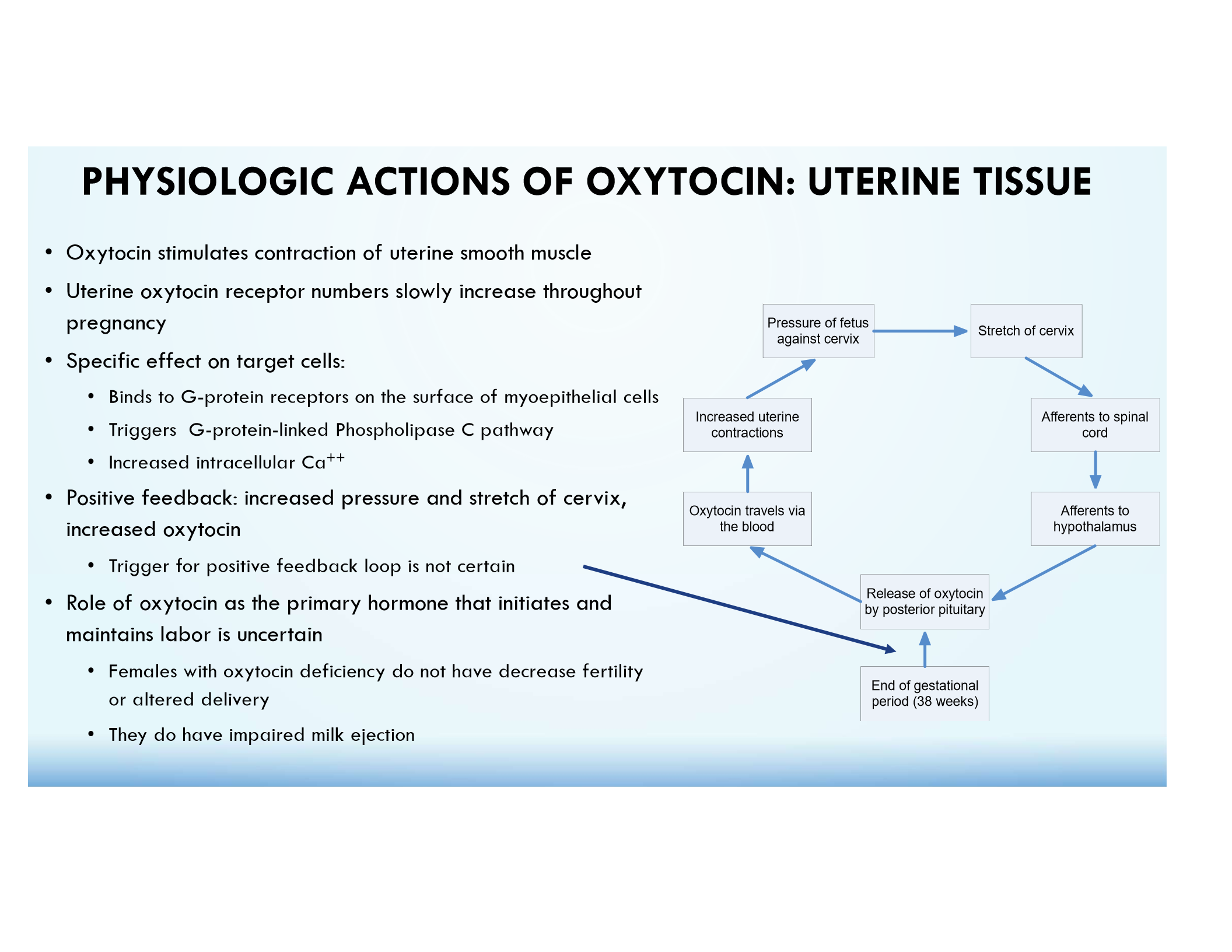
Oxytocin (OT)
Stimulates uterine contractions, milk ejection, and bonding behaviors; regulated by positive feedback.
Oxytocin Milk Ejection
Stimulates myoepithelial cell contraction in breast tissue.
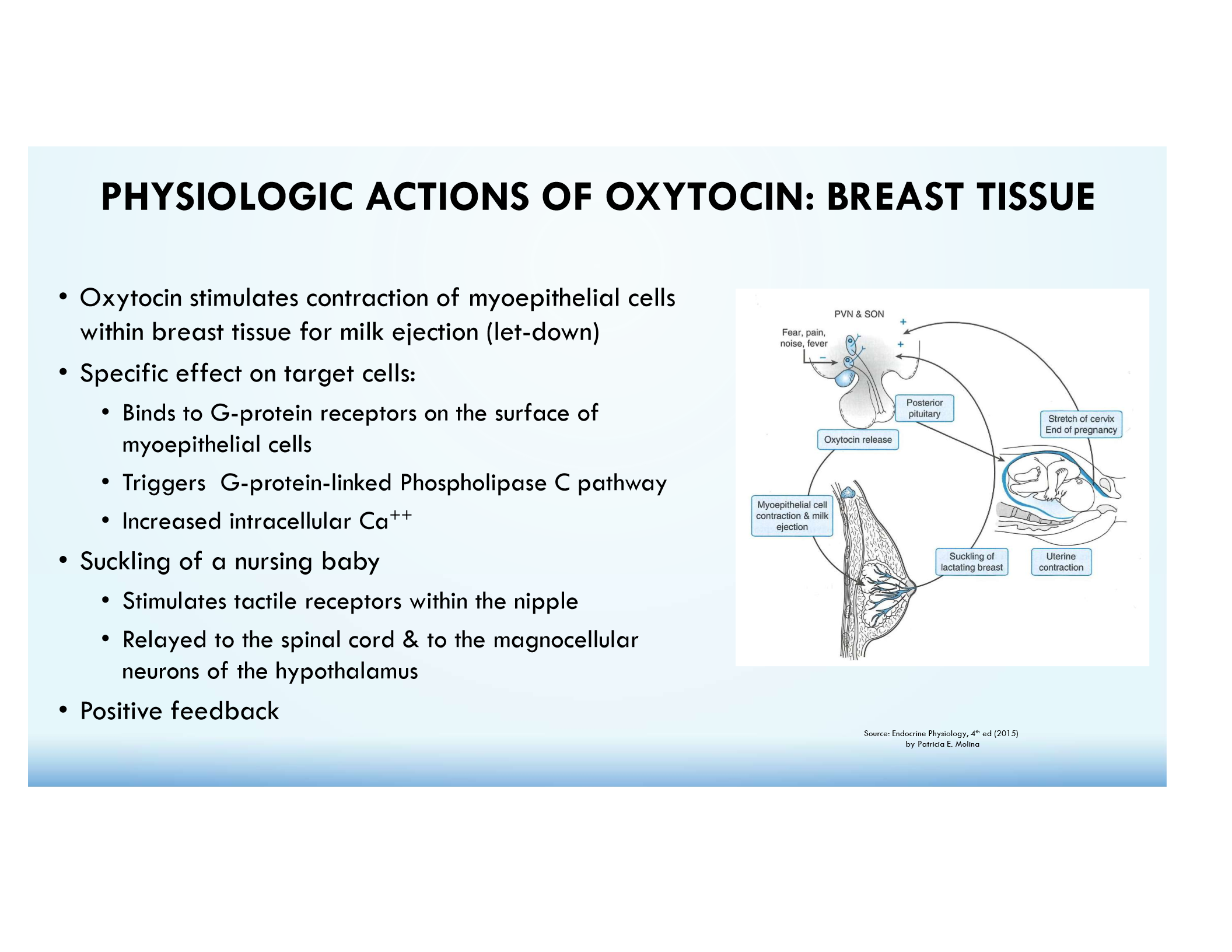
Oxytocin Uterine Contractions
Increases intracellular Ca²⁺ via G-protein receptors.
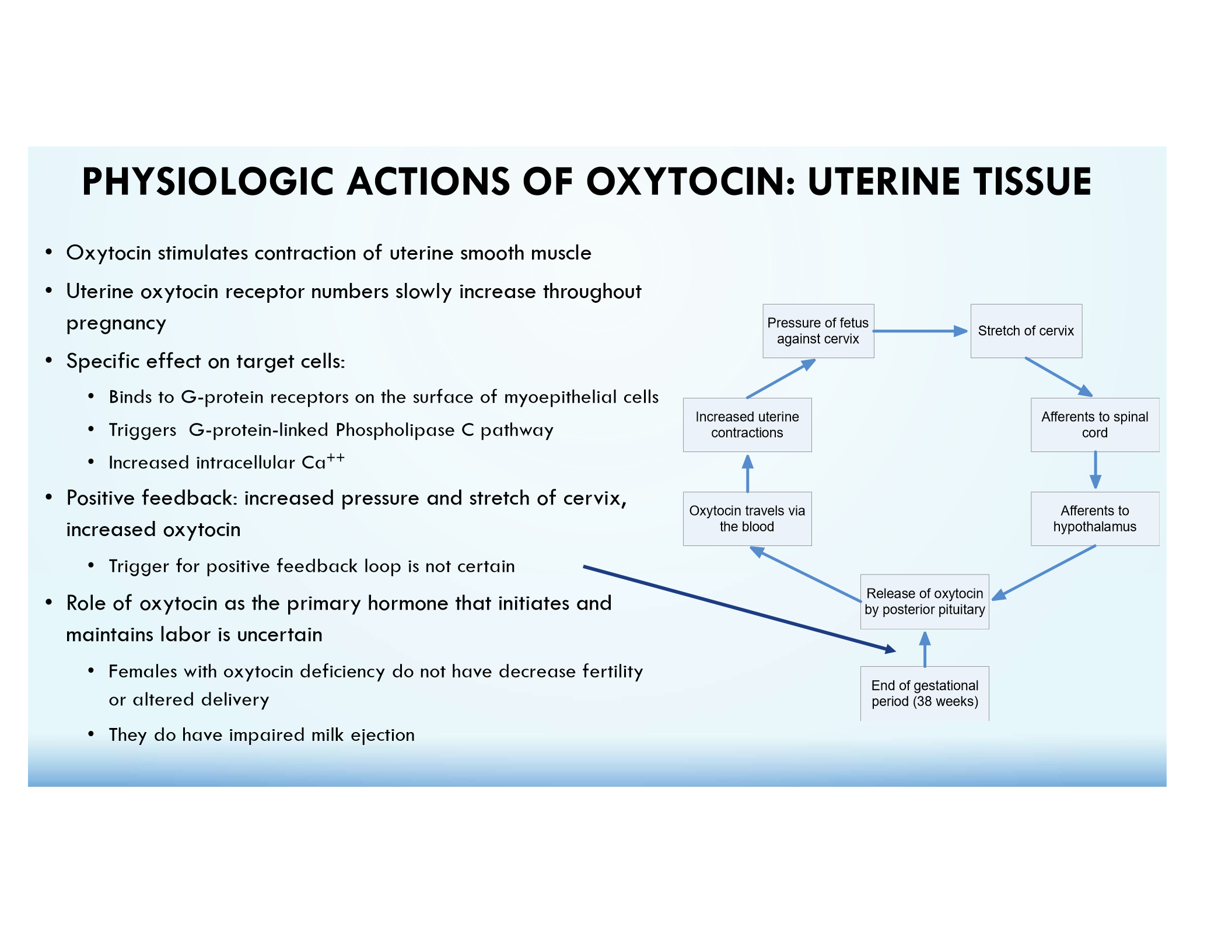
Oxytocin Positive Feedback
Increased stretch of cervix → more oxytocin → stronger contractions.
Oxytocin Psychosocial Effects
Involved in bonding, trust, and social behavior.
ADH (Vasopressin)
Increases water reabsorption in the kidneys by inserting aquaporins into collecting duct cells.
SIADH (Syndrome of Inappropriate ADH Secretion)
Excess ADH causes water retention, leading to hyponatremia.
Disorder of impaired water excretion due to inappropriate ADH secretion
Hyponatremia-occurs if water intake exceeds reduced urine output (hyponatremia with concentrated urine)
Symptoms can include nausea and vomiting, headache, confusion, weakness and fatigue, restlessness, muscle weakness, and seizures
Etiology is varied and can include CNS disturbances, malignancies, surgery, hormone deficiencies, infection, and side effects of medication use
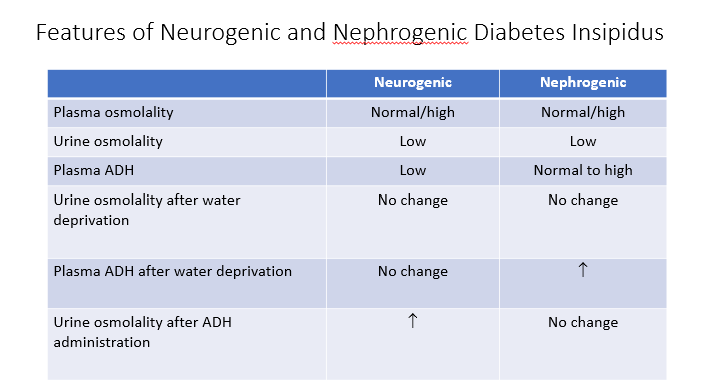
Diabetes Insipidus
Inability to concentrate urine; results in polyuria and hypernatremia (large volume of urine)!
2 Types:
Neurogenic (hypothalamic or central)- unregulated ADH
Nephrogenic- unresponsiveness to ADH
Distinguish if polyuria is due to an increase in an osmotic agent (i.e. glucose) or due to renal disease
Diagnosis is confirmed by dehydration stimulus followed by the inability to concentrate urine
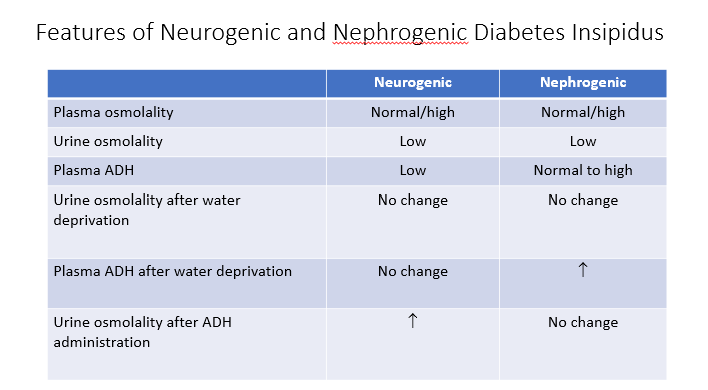
Neurogenic Diabetes Insipidus
ADH is not produced (hypothalamic or pituitary dysfunction).
AKA unregulated ADH.
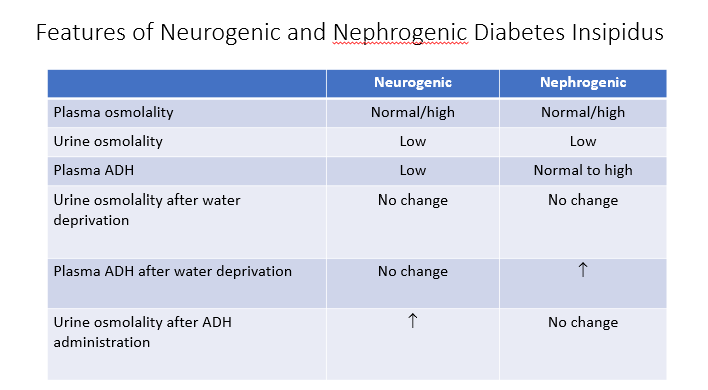
Nephrogenic Diabetes Insipidus
Kidneys are unresponsive to ADH.
AKA unresponsive to ADH.
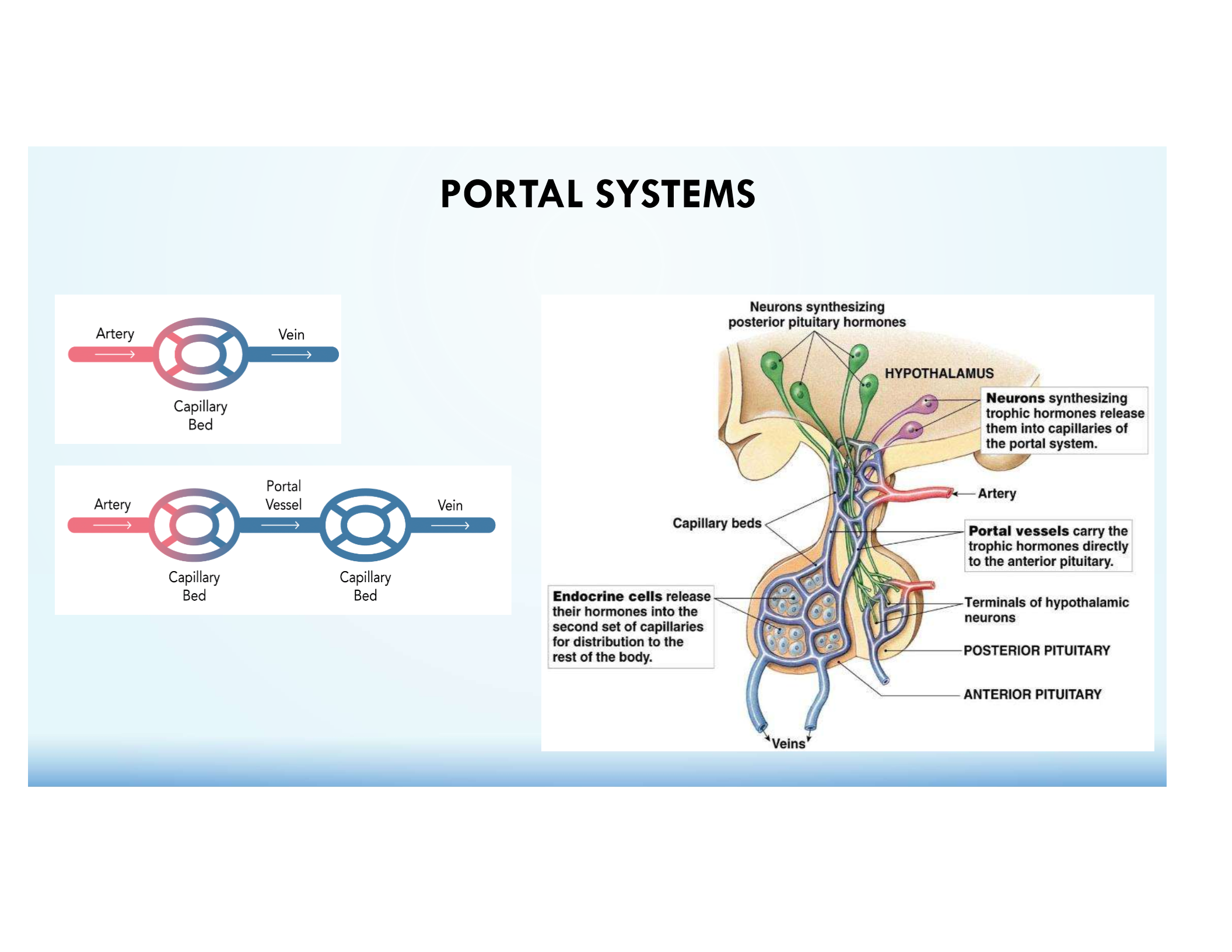
Hypophyseal Portal System
Transports hypothalamic hormones directly from the hypothalamus to the anterior pituitary via two capillary beds in series.
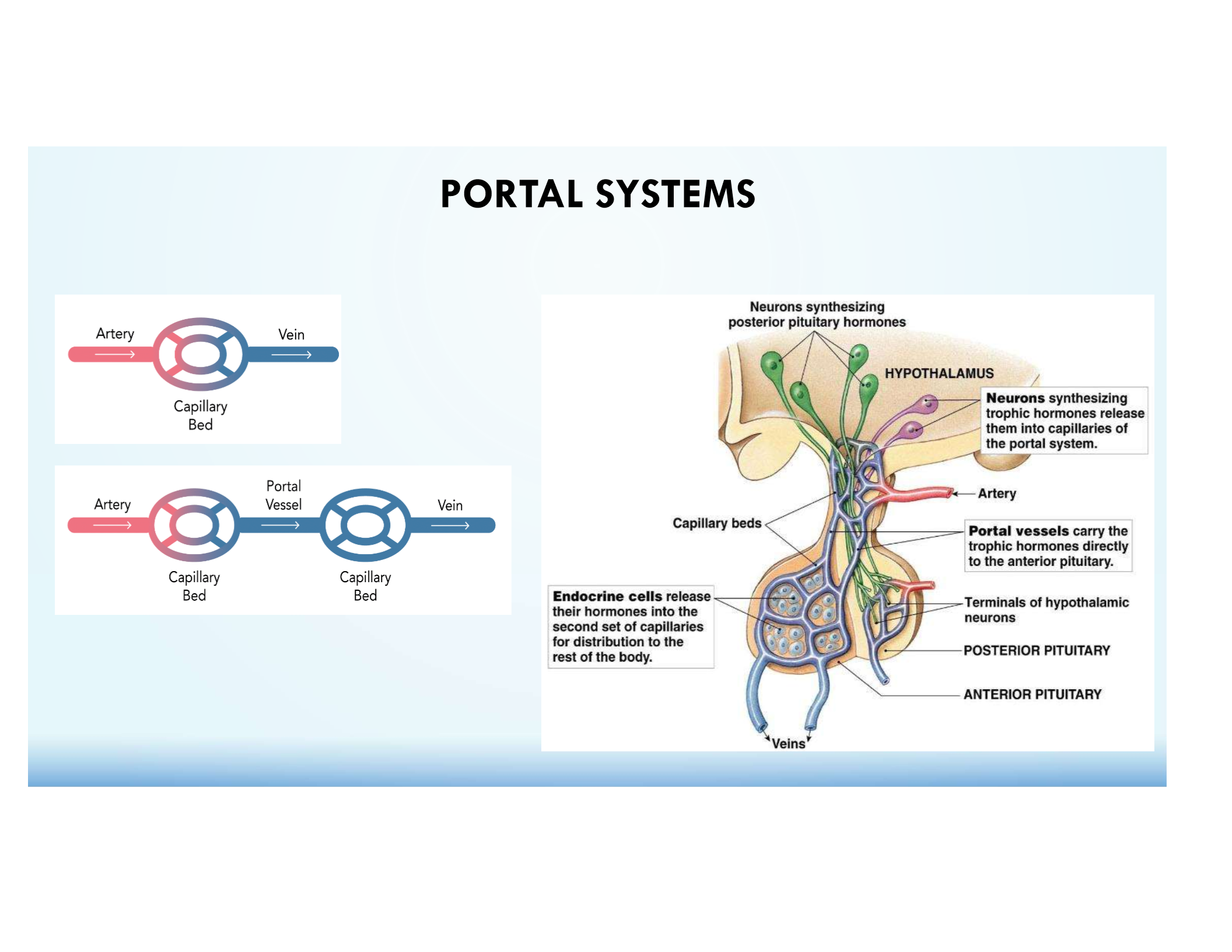
Function of the Hypophyseal Portal System
Allows rapid, direct hormone delivery for precise endocrine regulation.
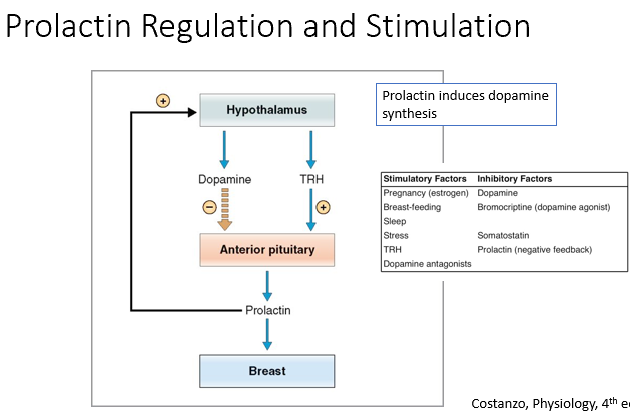
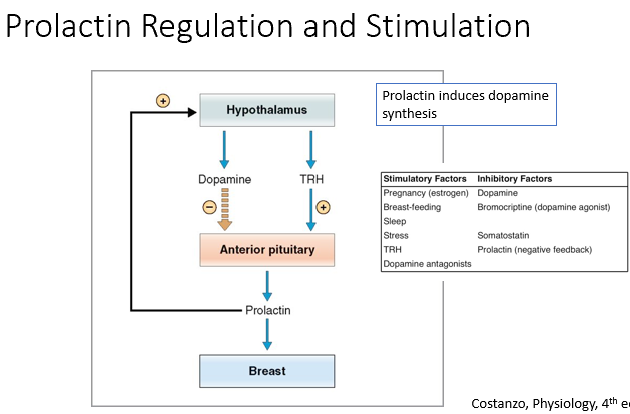
Prolactin (PRL)
Stimulated by TRH (hypothetical)
Inhibited by dopamine (negative inhibition)
Stimulates mammary gland development and milk production
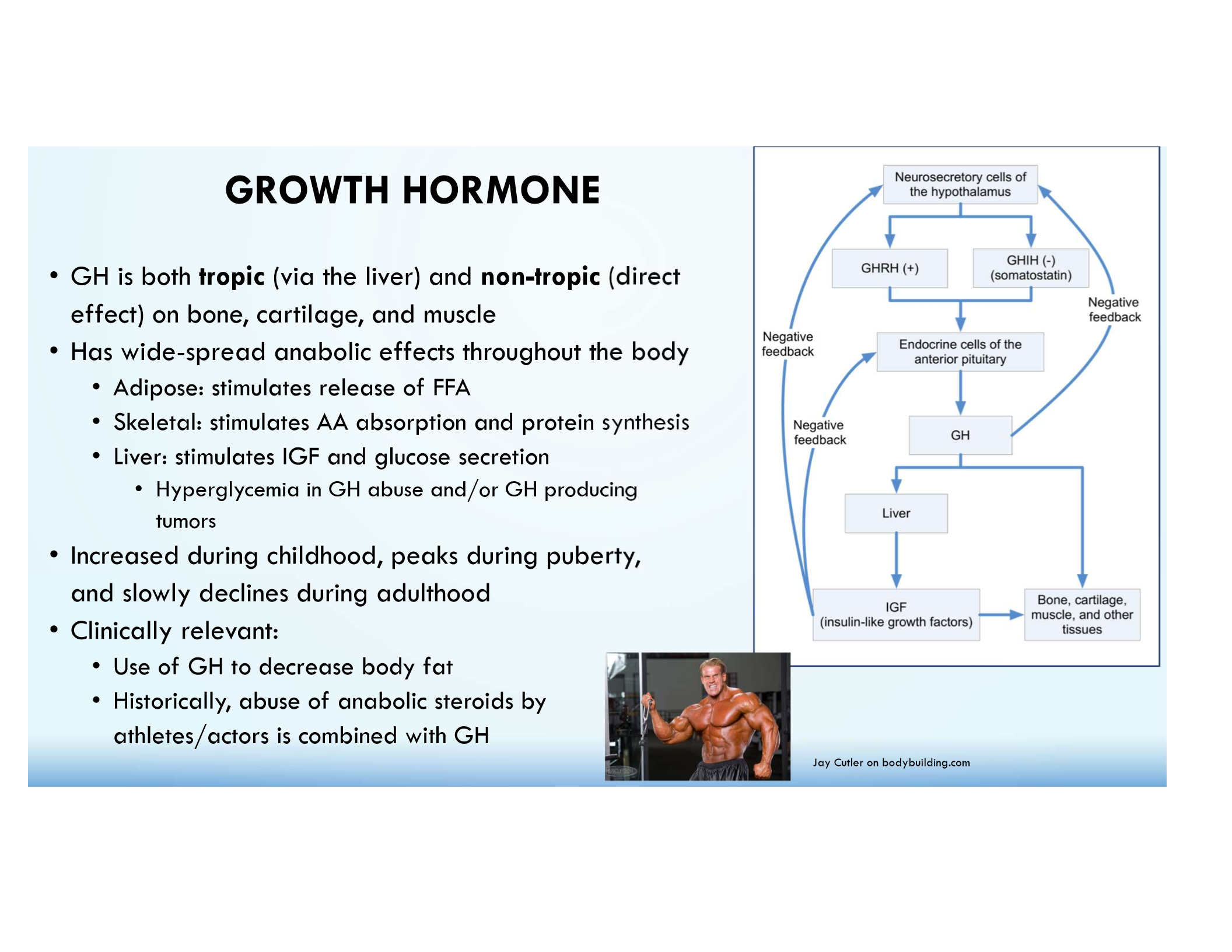
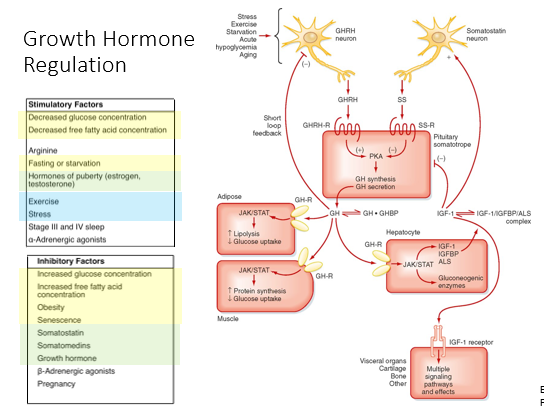
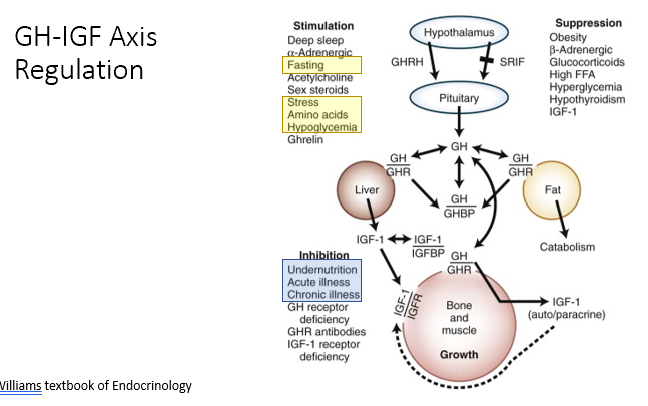
Growth Hormone (GH)
Stimulated by GHRH, inhibited by somatostatin; promotes growth, protein synthesis, and metabolism.
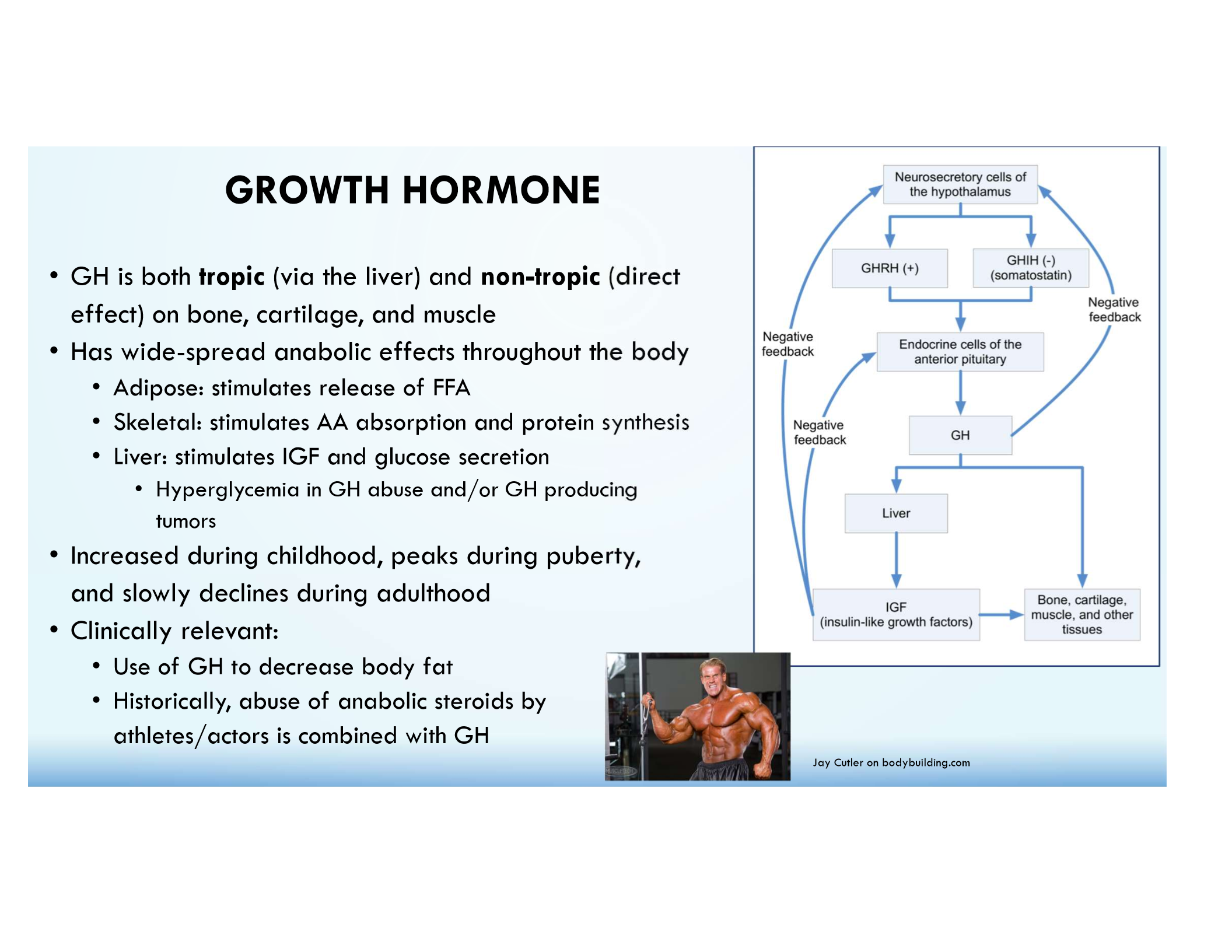
Growth Hormone Direct Effects
Lipolysis, protein synthesis, glucose metabolism.
Growth Hormone Indirect Effects
IGF-1 secretion from the liver promotes growth effects.
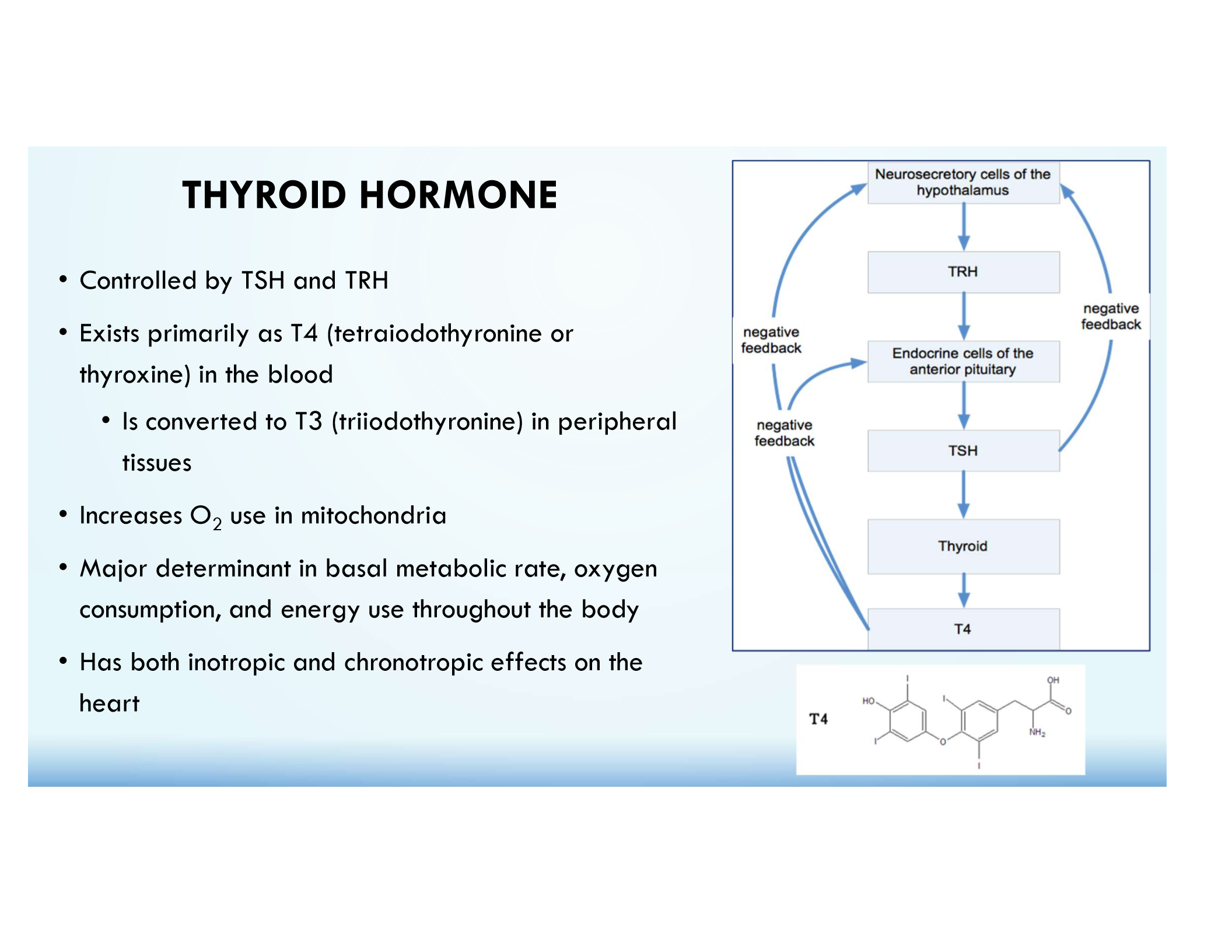
Thyroid Hormone (T3/T4)
Regulated by TRH → TSH; increases metabolism, heart rate, and O₂ consumption.
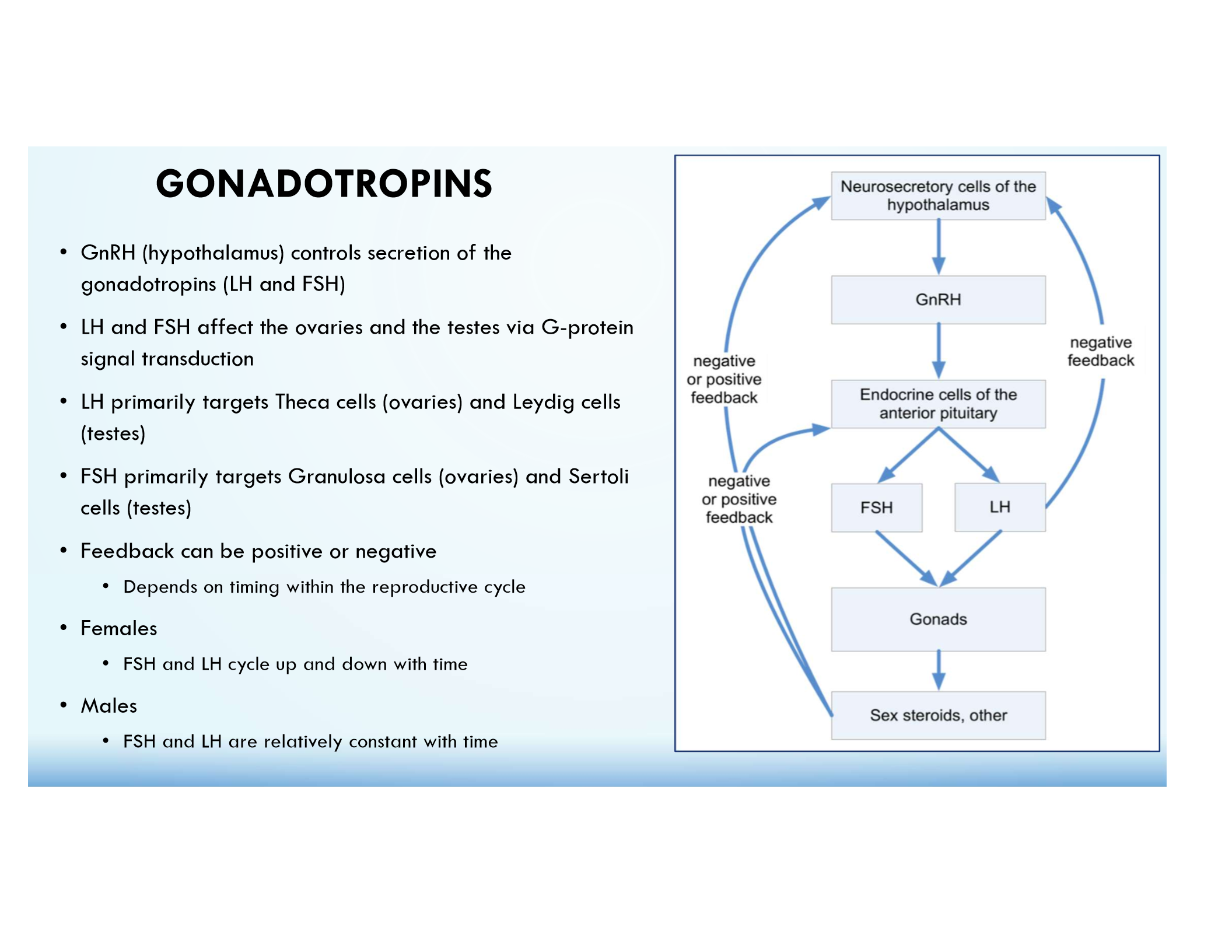
Sex Steroids (Estrogen/Testosterone)
Regulated by GnRH → FSH/LH; involved in reproductive function and gametogenesis.
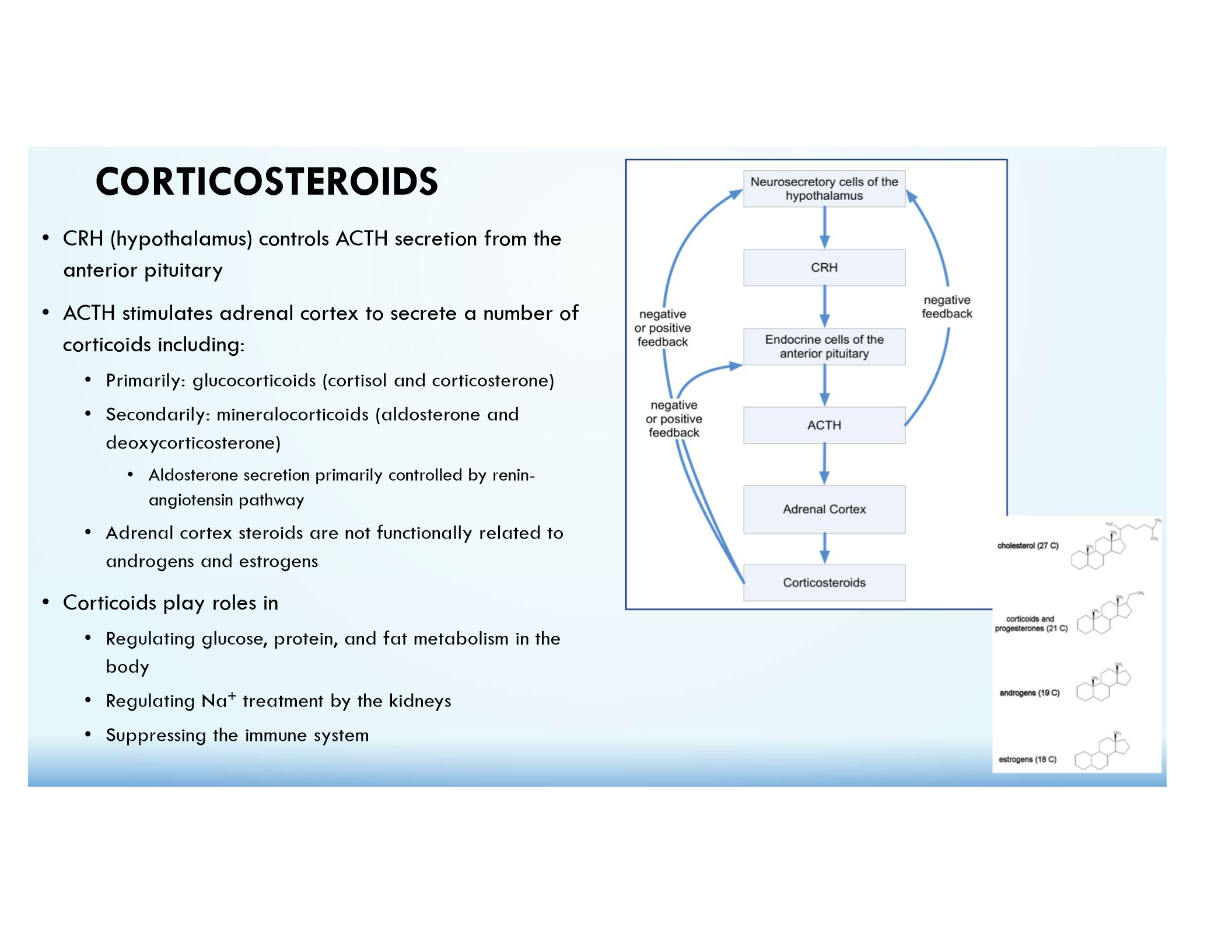
Corticosteroids (Cortisol)
Regulated by CRH → ACTH; involved in stress response, metabolism, and immune suppression.
Hypopituitarism
Deficiency of pituitary hormones; causes include trauma, tumors, or congenital defects.
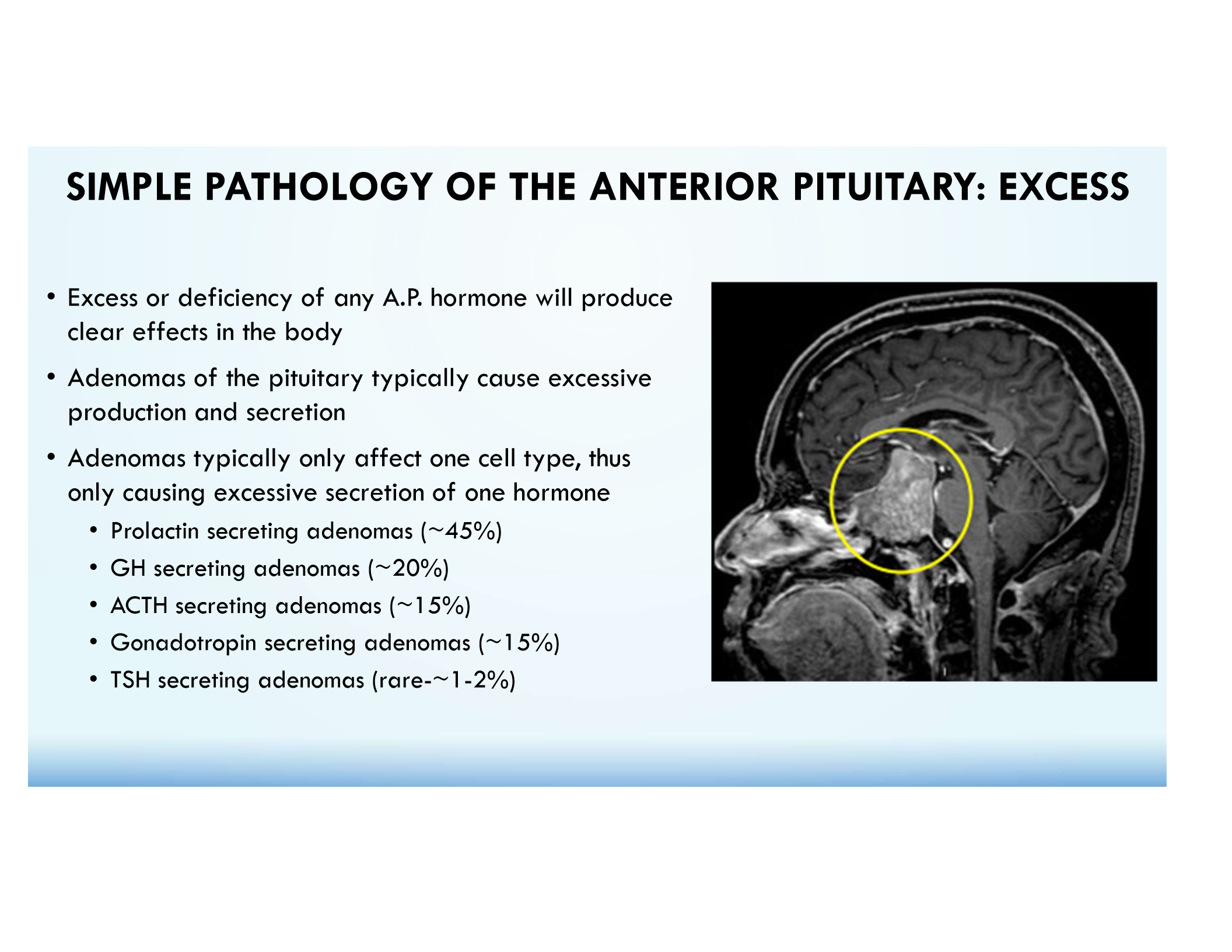
Hyperpituitarism
Excess hormone secretion, often due to adenomas.
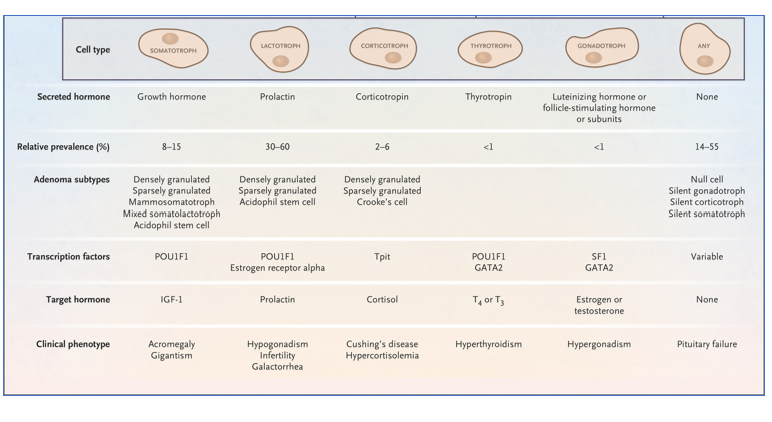
Prolactinoma (45%)
Most common pituitary adenoma; causes ↑ PRL, galactorrhea, and infertility.
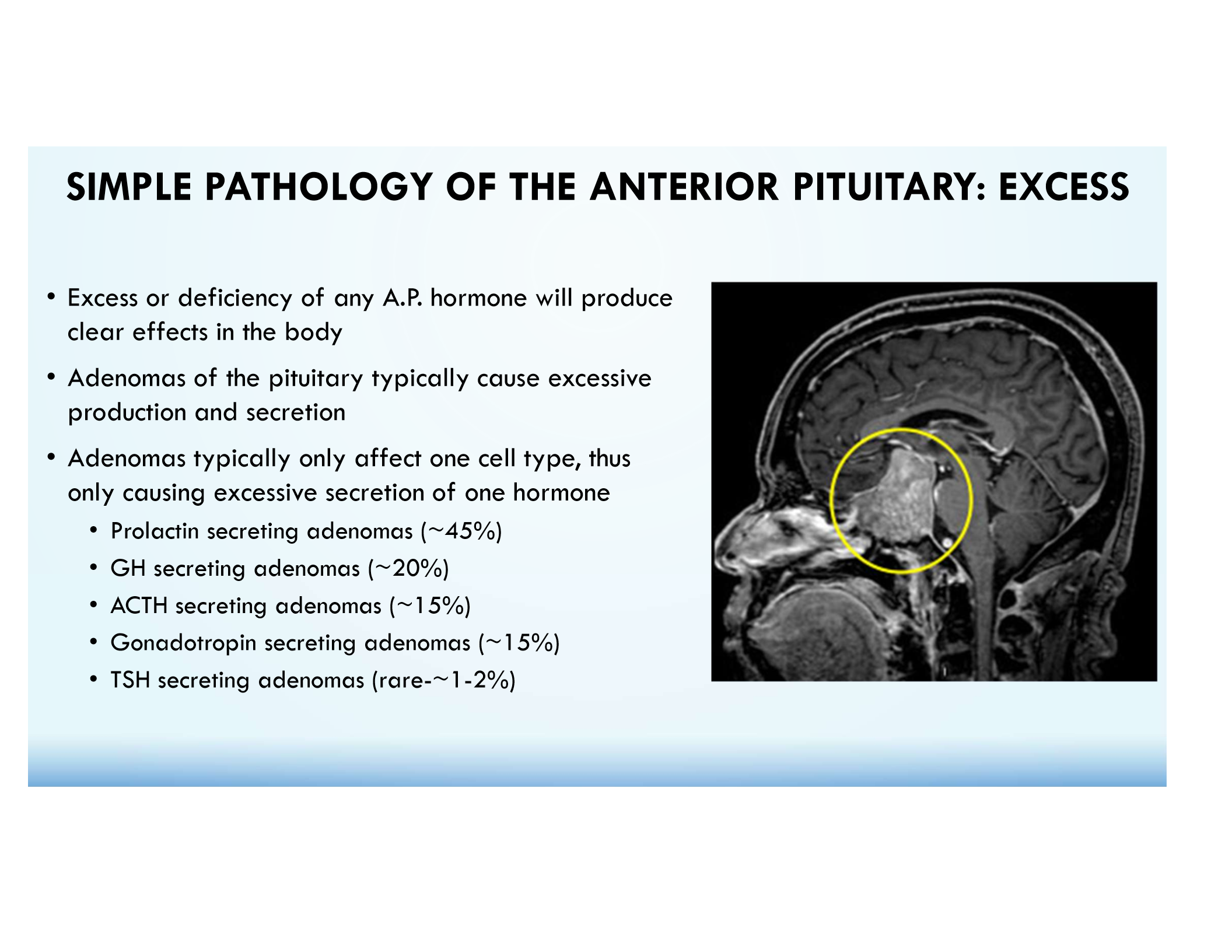
GH Adenoma (20%)
Causes acromegaly (adults) or gigantism (children).
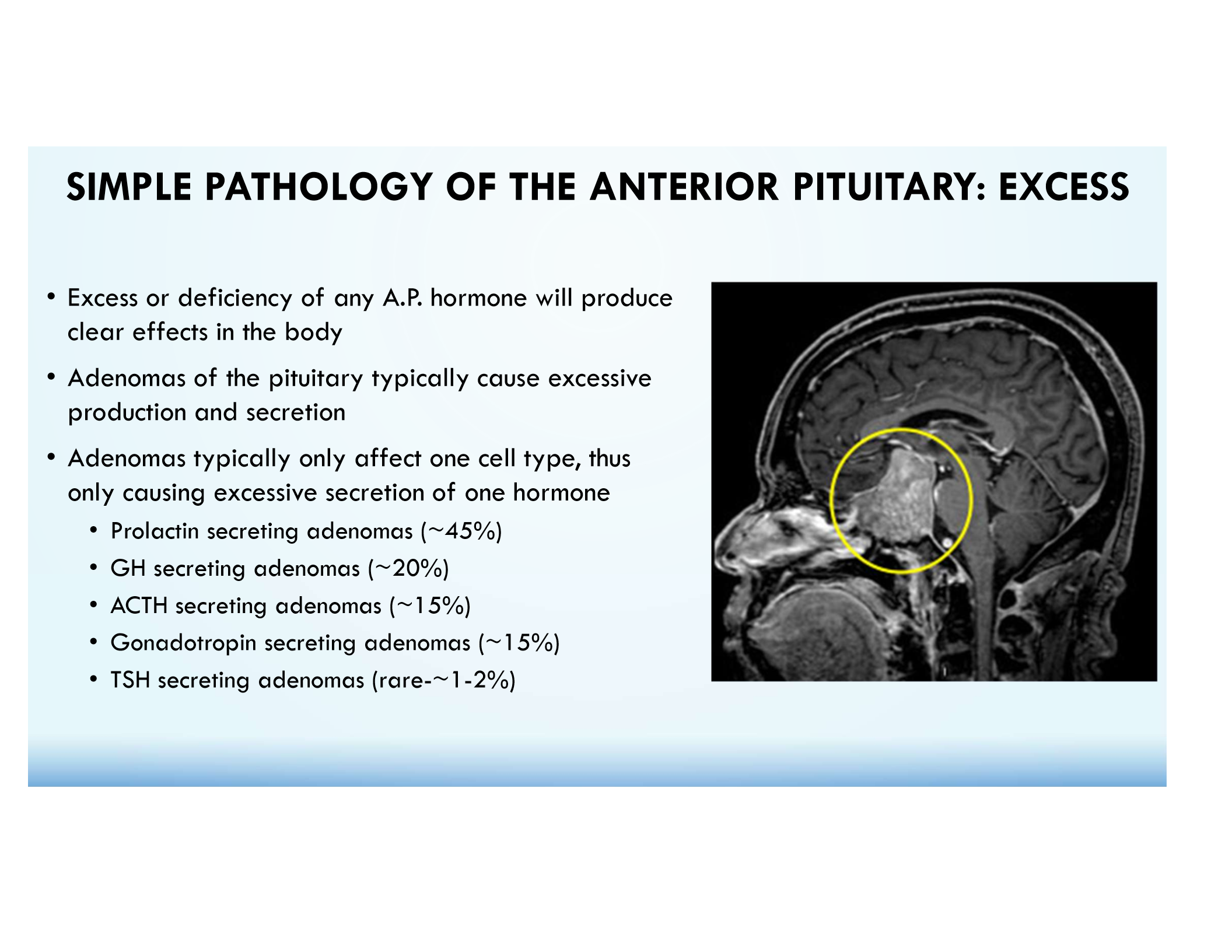
ACTH Adenoma (15%)
Causes Cushing’s Disease due to excess cortisol.
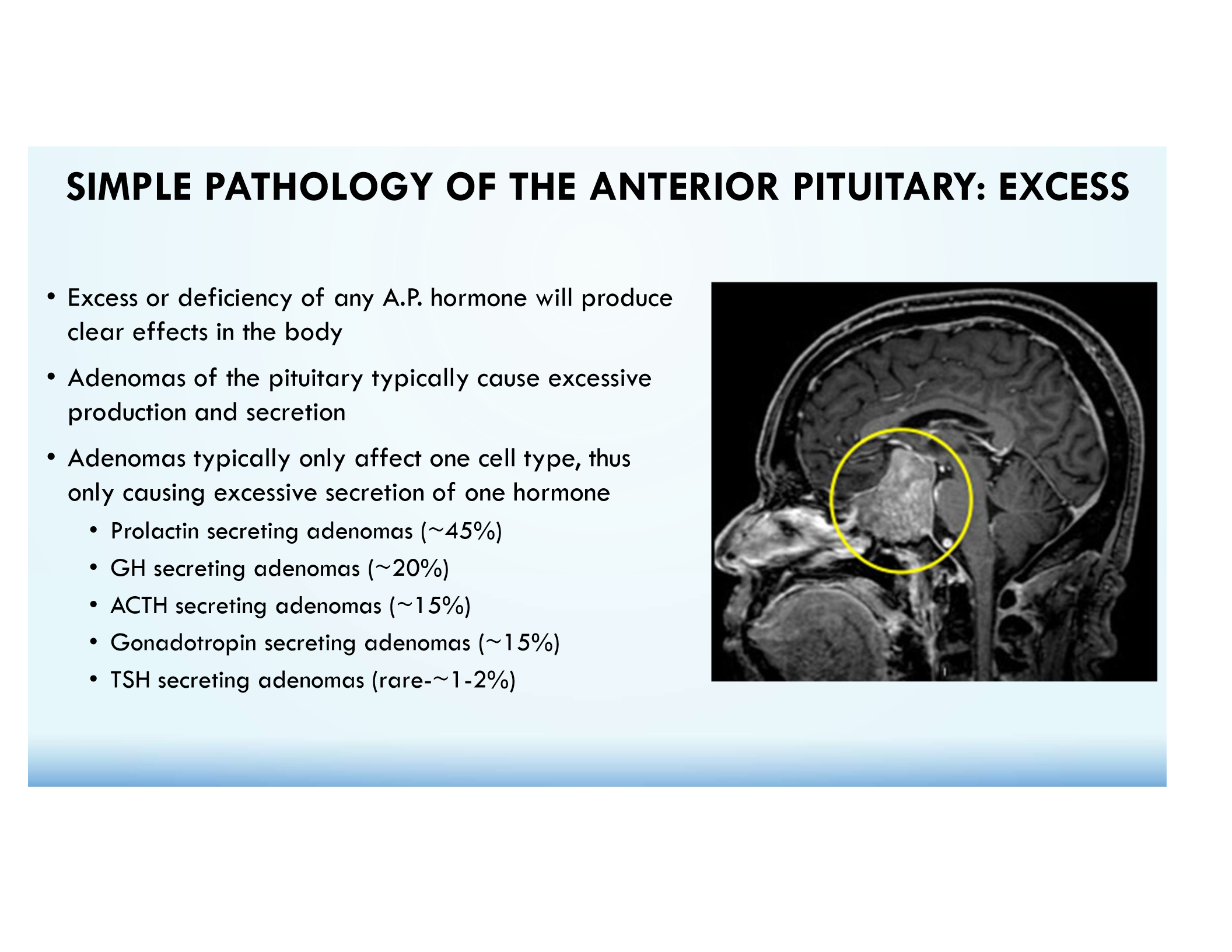
FSH/LH Adenomas (15%)
Often clinically silent.
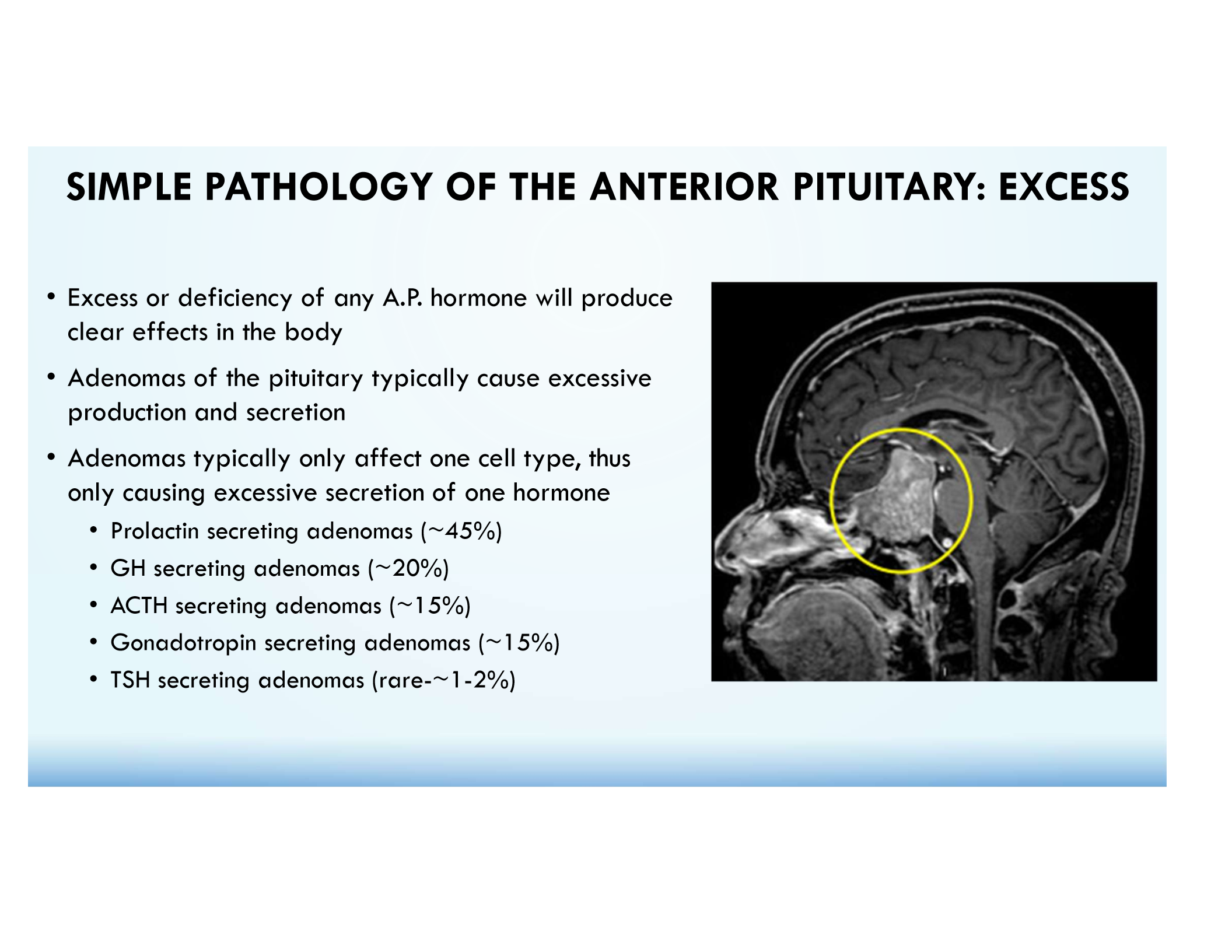
TSH Adenoma (1-2%)
Rare adenoma that causes hyperthyroidism.
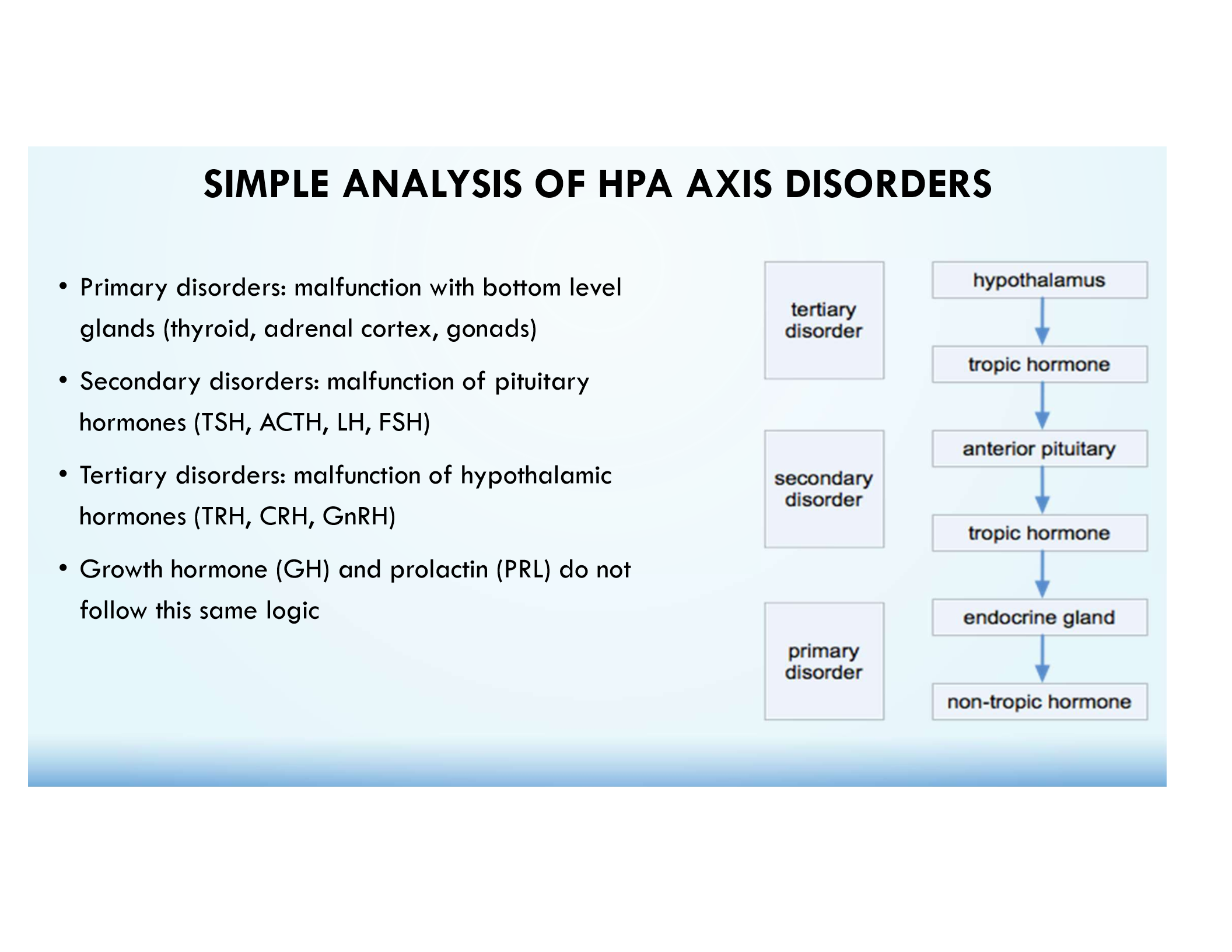
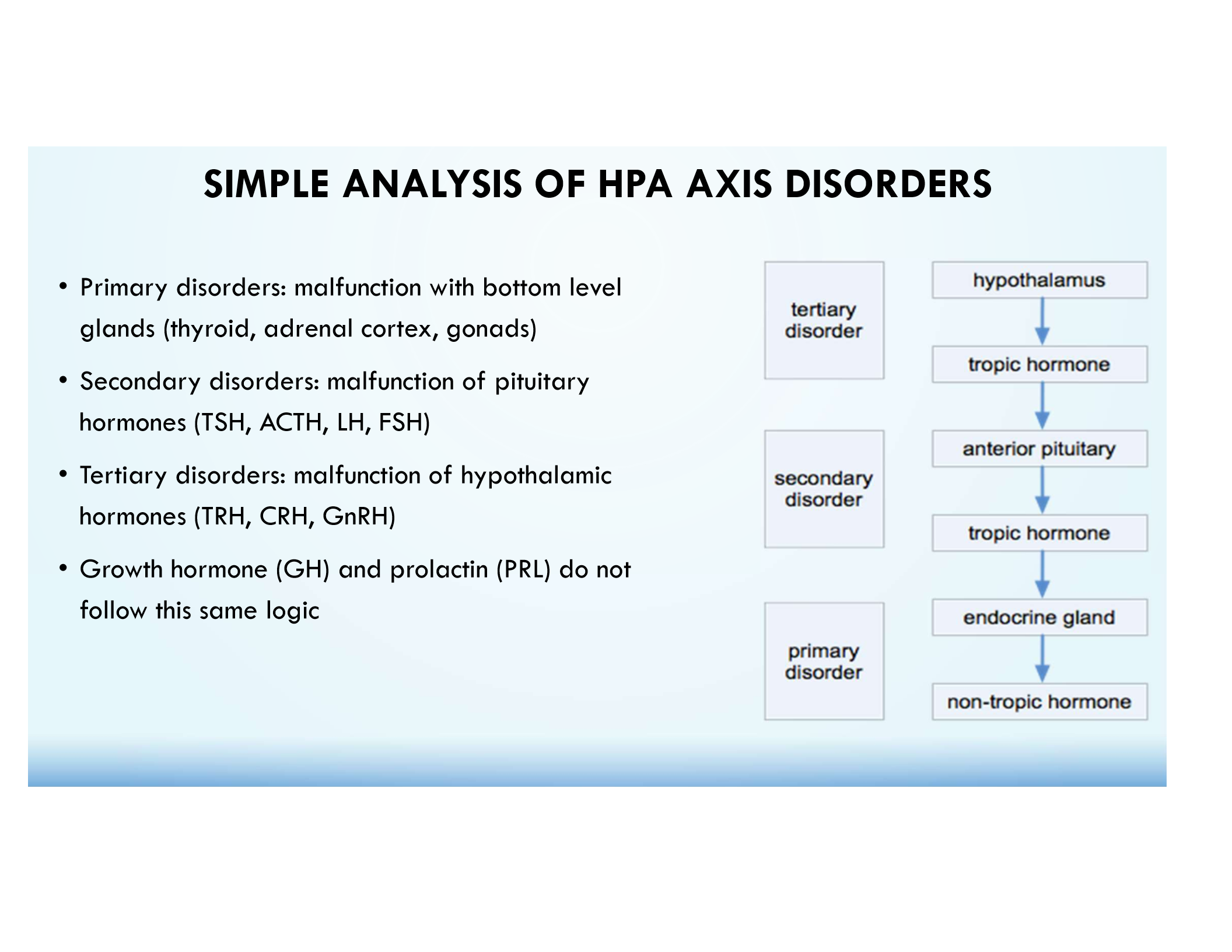
Primary Endocrine Disorder
Malfunction of the target gland (e.g., adrenal cortex in Addison’s disease).
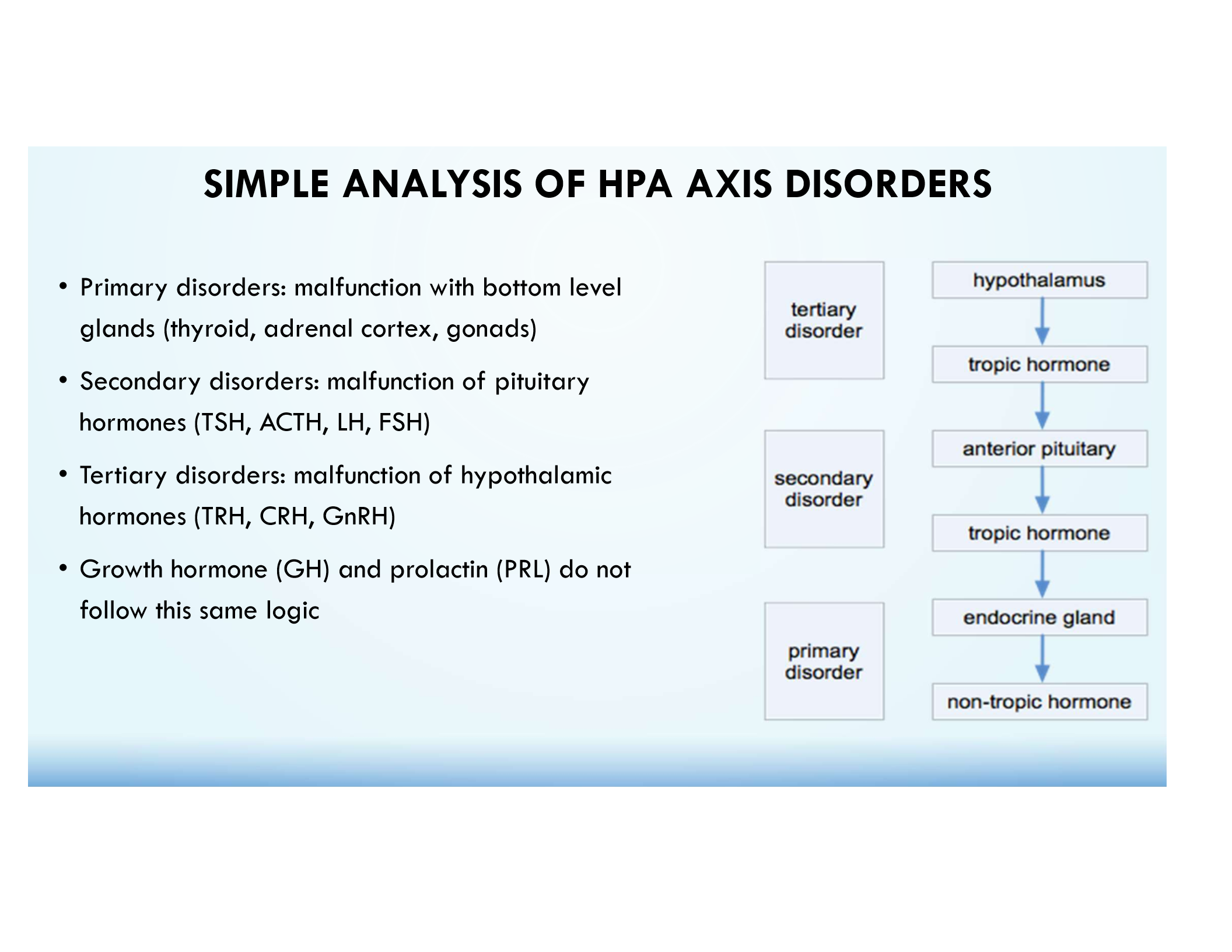
Secondary Endocrine Disorder
Malfunction of the pituitary (e.g., low ACTH causing adrenal insufficiency).
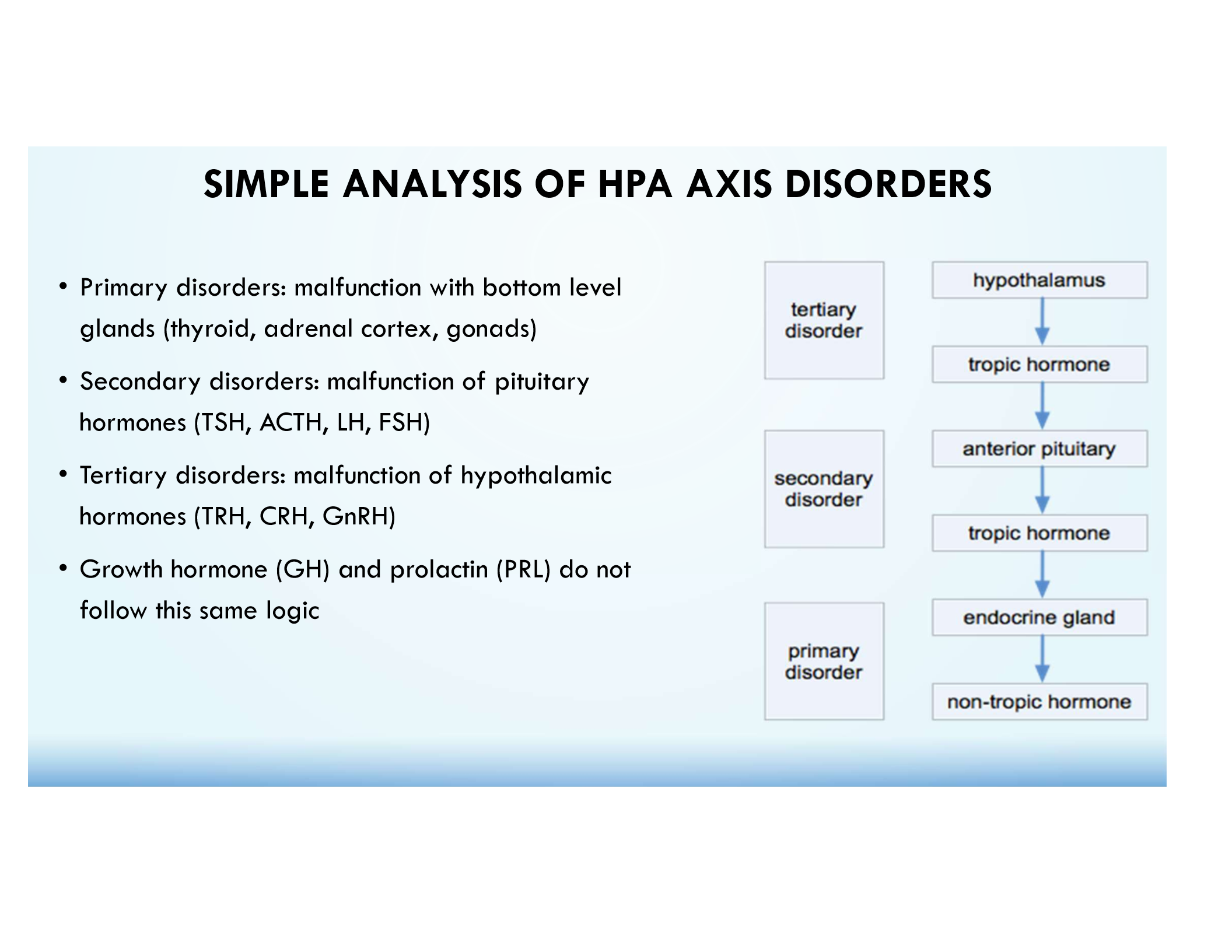
Tertiary Endocrine Disorder
Malfunction of the hypothalamus (e.g., low CRH causing adrenal insufficiency).
Primary Adrenal Insufficiency (Addison’s Disease)
Low cortisol, high ACTH.
Secondary Adrenal Insufficiency
Low cortisol, low ACTH, high CRH.
Tertiary Adrenal Insufficiency
Low cortisol, low ACTH, low CRH.
ACTH Stimulation Test in Primary Adrenal Insufficiency
No increase in cortisol.
SIADH Symptom
Hyponatremia.
Hormone Least Affected by Pituitary Trauma
Insulin (not HPA-regulated).
Hormone Controlled by Osmoreceptors
ADH.
Hormones Synthesized in Hypothalamus
ADH & Oxytocin.
Hormone Controlled by Positive Feedback
Oxytocin.
Example of Two Tropic Hormones
CRH & TRH.
Key Feature of a Portal System
Two capillary beds in series.
Primary Cortisol Disorder Affects Which Organ?
Adrenal Cortex.
Low Estrogen, Low FSH, Low GnRH Indicates
Tertiary disorder.
GH and PRL
Do NOT follow the HPA Axis of Disorders
A 36 y/o male has suspected adrenal insufficiency, as evidenced by low blood pressure, darkening of the skin, and low blood [na+]. An ACTH stimulation test is ordered to confirm the diagnosis. This test involves injecting a small amount of synthetic ACTH and then monitoring changes in blood cortisol. If this is primary adrenal insufficiency, we will expect what of the following to occur as a result of this test?
A. Blood cortisol to increase a small amount
B. Blood cortisol to increase a large amount
C. Blood cortisol to decrease as small amount
D. Blood cortisol to decrease a large amount
E. Blood cortisol to stay about the same
E. Blood cortisol to stay about the same
(primary adrenal insufficiency means that adrenal cortex is malfunctioning. Thus, additional synthetic ACTH will not produce any effect to blood cortisol).
SIADH (syndrome of inappropriate antidiuretic hormone secretion) results in excessive production of ADH. Which symptom are you most likely to see with SIADH?
A. Hypercortisolism
B. Hyponatremia
D. Spontaneous lactation
E. Acromegaly
B. Hyponatremia
XS ADH leads to water retention → dilution of blood and decreased Na+ levels
A 17 y/o male is in a high speed motor vehicle accident which results in severe facial trauma. The secretion of what hormone is the least likely to be effected as a result of this accident?
A. Insulin
B. T4
C. Cortisol
D. GH
E. LH
A. Insulin
(this is the one hormone in this list that is not directly controlled by the hypothalamic-pituitary axis); damage to the hypothalamus and especially to the pituitary can affect the secretion of any of the other hormones
In hypothalamus, osmoreceptors are involved in
A. Aldosterone secretion
B. ACTH secretion
C. ADH secretion
D. GH secretion
C. ADH secretion – ADH is involved in urine concentration as well as amount of urine produced
Which set of hormones is synthesized in the hypothalamus
A. TSH and oxytocin
B. ADH and oxytocin
C. FSH and ADH
D. FSH and TSH
B. ADH and oxytocin – TSH & FSH are synthesized in the anterior pituitary
Which hormone is controlled by positive feedback mechanism?
A. GH
B. TSH
C. ACTH
D. Oxytocin
D. Oxytocin
Which set of hormones are both tropic hormones
A. CRH and TRH
B. ACTH and ADH
C. Oxytoxin and LH
D. Estrogen and cortisol
A. CRH and TRH – Estrogen, ADH, oxytocin, & cortisol are non-tropic
A portal system differs from systemic circulation because portal systems
A. go directly from arterioles to venules
B. have two capillary beds in series
C. are only found between the hypothalamus and posterior pituitary
D. are used only for release of neurohormones
B. have two capillary beds in series
Note:
A. One capillary bed exists between arterioles and venules in systemic circulation
C. Liver and kidneys have portal systems
D. Neurohormones are released directly into systemic circulation via exocytosis
Which organ would be abnormal in a primary cortisol disorder?
A. Hypothalamus
B. Anterior pituitary
C. Posterior pituitary
D. Adrenal cortex
D. Adrenal cortex
A patient presents with low estrogen, low FSH, and low GnRH. This pattern of results is most characteristic of a _____ disorder
A. Primary
B. Secondary
C. Tertiary
C. Tertiary (all 3 are low)
Note:
(Primary – low estrogen, high FSH, high GnRH)
(Secondary – low estrogen, low FSH, high GnRH)
Posterior Pituitary Hormones
Oxytocin
Anti-diuretic hormone (ADH) also vasopressin or arginine vasopressin (AVP)
Anterior Pituitary Hormones (& cells that produce them)
GH (somatotrophs)
Prolactin (lactotrophs)
LH/FSH (gonadotrophs)
TSH (thyrotrophs)
ACTH (corticotrophs)
ADH or AVP
Maintains normal osmolality of body fluids and normal blood volume
Released when serum osmolality is increased
Works on principle cells of the distal tubule (increases water resorption)
Induces contraction of vascular smooth muscle to protect against severe volume depletion
Oxytocin
Milk letdown
Uterine contraction
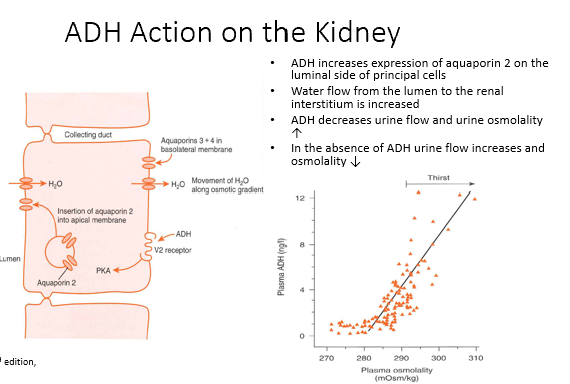
Mechanism of ADH
ADH increases expression of aquaporin 2 on the luminal side of principal cells
Water flow from the lumen to the renal interstitium is increased
ADH decreases urine flow and urine osmolality ↑
In the absence of ADH urine flow increases and osmolality ↓
Stimulus for secretion = Increased Plasma Osmolarity
How to tell the difference between Neurogenic and Nephrogenic DI?
Plasma ADH is the distinguishing factor:
Neurogenic = Plasma ADH is low (unregulated ADH)
After water deprivation = no ADH change (ADH isn’t responding the way it should)
Urine osmolarity after ADH given = increases (kidneys are functioning)
Nephrogenic = Plasma ADH is normal/high (can’t respond to ADH)
After water deprivation = ADH increases as plasma osmolarity increases
Urine osmolarity after ADH given = no change (can’t respond to the ADH, issue with receptors)
Prolactin Pathway (steps, inhibited by, stimulated by)
Pathway:
Hypothalamus
Dopamine (negatively inhibits) & TRH (positively stimulates)
Anterior Pituitary
Prolactin
Breast
When prolactin is produced, it induces dopamine synthesis → negative inhibition of itself
Things that can stimulate:
Pregnancy
Breast feeding
Sleep
Stress
TRH (hypothyroidism)
Things that can inhibit:
Dopamine
Somatostatin
Prolactin
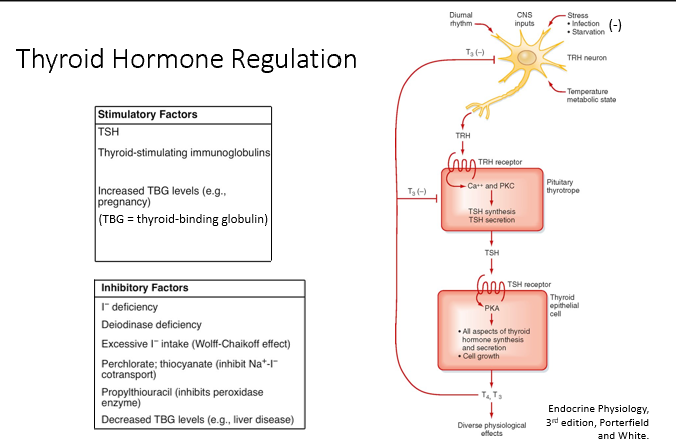
FSH/LH Pathway
Pathway:
GnRH released from median eminence/anterior pituitary (in pulses)
A continuous infusion will result in the downregulation of LH and FSH secretion.
Depending on pulses, FSH or LH will be produced more (FSH when less frequent, LH when more frequent)
FSH and LH produce sex steroids
Negative feedback on anterior pituitary & hypothalamus
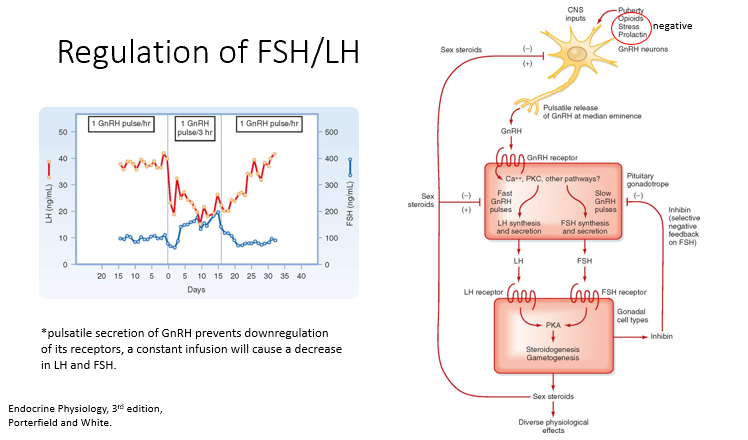
Positive and Negative GnRH regulators
Positive:
Puberty
Negative:
Opioids
Stress
Prolactin
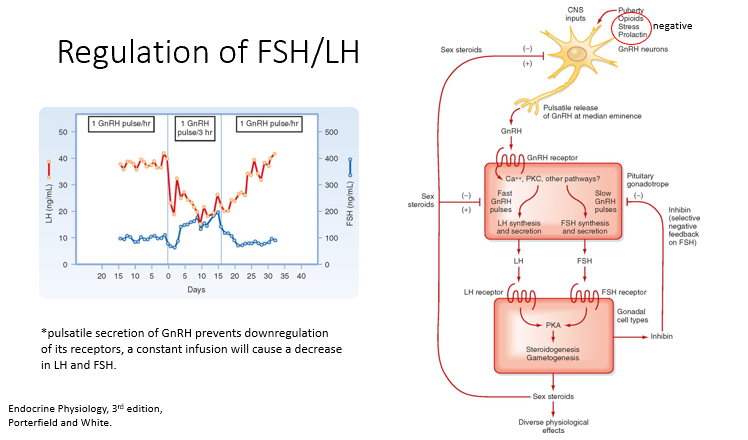
TH Pathway
Pathway:
From the hypothalamus, we have released TRH
Released to median eminence (pituitary), works on pituitary thyrotropes
Induces secretion of TSH
TSH works on thyroid epithelial cells to produce 2 hormones: T3 and T4
T3 is more active. Negatively feeds back to the pituitary and hypothalamus.
Stimulantory:
TSH
TSH Ig’s
Inhibitory:
Iodine deficiency
Excessive Iodine intake
Propylthiouracil
Stress (ICU)
Starvation (ICU)
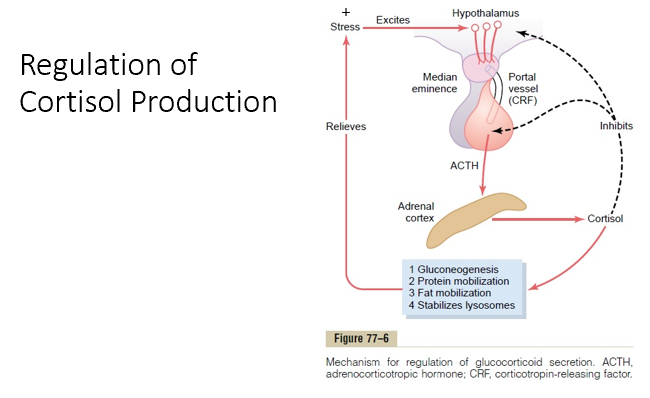
Cortisol Pathway
Pathway:
CRH is released from the median eminence of the hypothalamus
Works on corticotropes to induce expression of ACTH
ACTH upregulates the production of cortisol (via the adrenal cortex)
Cortisol increases:
Gluconeogenesis
Protein metabolism
Fat mobilization
Stabilizing lysosomes
Stimulatory:
Stress (increases cortisol)
Inhibitory:
Cortisol (feeds back to inhibits the production of CRH and ACTH @ hypothalamus and pituitary)
GH Pathway
Pathway:
GHrH secretion from hypothalamus
Acts on somatotropes to induce GH synthesis
GH acts directly on adipose, muscle, and hepatocytes to induce secretion of IGF-1 (insulin-like growth factor 1)
IGF-1 results in physical growth effects (visceral organs and bone and cartilage)
Stimulatory:
IGF-1 positively regulates Somatostatin release
Decreased Glucose & FA concentration, fasting/starvation (b/c GH counter regulates insulin!)
Exercise and stress (b/c GH protects against too much insulin)
Hormones of puberty (estrogen/testosterone)
Inhibitory:
GH negatively regulates GHrH secretion
IGF-1 negatively regulates GH secretion
Somatostatin reduces GH release
Increased Glucose & FA concentration, obesity, and senescence (lots of glucose around)
Somatostatin, Somatomedins (IGF-1), GH
IGF-1 (Inhibited by)
Inhibitory:
Undernutrition (Stress)
Acute/Chronic illness (Stress)
Note: stress increases GH but decreases IGF-1!
Thus, they don’t have to be increased at the same time.
Depends what the body is experiencing.
IGF-1
Protein intake increases THIS → Increases Insulin & GH → Increases protein synthesis & Growth → Caloric Storage is Even
Carb intake (AKA excess glucose) decreases GH but no impact on THIS → Increases Insulin → No growth because no building blocks → Caloric Storage increases
Fasting (AKA hypoglycemia and no building blocks) → Increased GH (to protect against insulin drop), Decreased THIS & Insulin → Decreased protein synthesis & growth → Increased caloric mobilization (lipids)
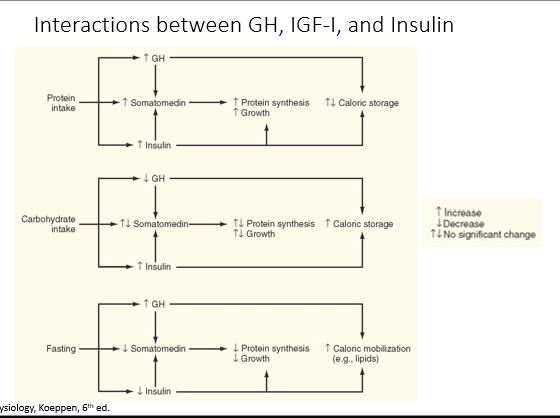
Summary of GH Actions
Diabetogenic effect- causes insulin resistance
↓ glucose uptake
↑ blood glucose levels
↑ lipolysis
↑ blood insulin levels
Increased protein synthesis and organ growth (through the actions of IGF-I)
↑ amino acid uptake
↑ DNA, RNA, protein synthesis
↑ lean body mass and organ size
Increased linear growth (through the actions of IGF-I)
Altered cartilage metabolism
Hypopituitarism
A condition where the pituitary gland, located at the base of the brain, does not produce enough hormones.
Can be caused by:
pituitary diseases
hypothalamic disease
traumatic brain injury
stroke
Hyperpituitarism
Excessive hormone production by the pituitary gland is often caused by a noncancerous tumor (adenoma) that leads to the overproduction of one or more pituitary hormones.
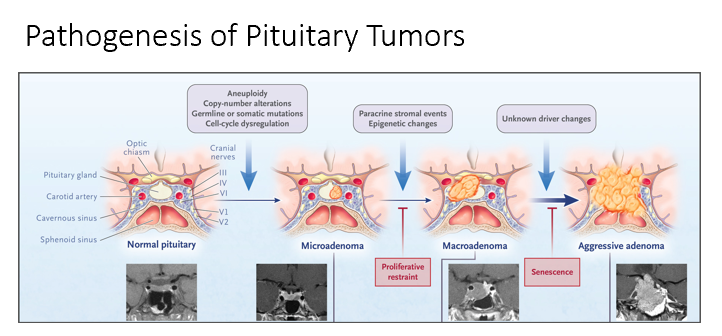
Normal → Microadenoma → Macroadenoma → Aggressive Adenoma
Can get compression of the optic chiasm! Squeezed into the sella turcia!
The 2 types we will focus on:
Adenoma of Somatotropes (overproduce GH)
Treat via targeting IGF-1
Adenoma of Lactotrophs (overproduce Prolactin)
Treat via targeting Prolactin
Cushing’s Disease
Adenoma resulting in overproduction of ACTH
Excess cortisol
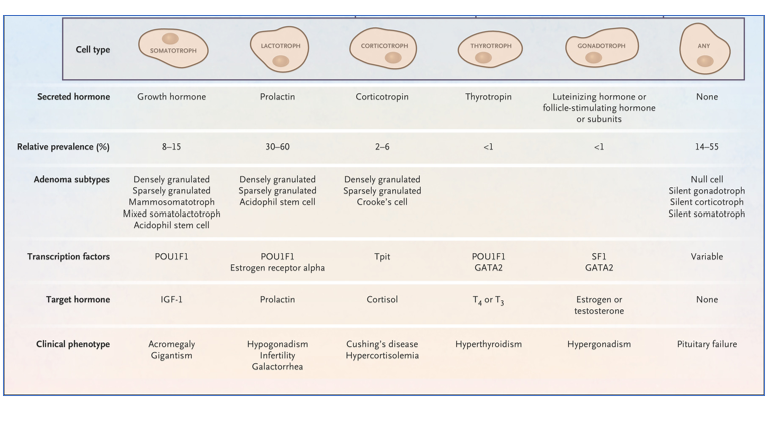
Hyperthyroidism
Adenoma resulting in overproduction of TSH
Hypergonadism
Adenoma resulting in overproduction of FSH/LH
Pituitary Failure
Adenoma resulting in overproduction of null cell
Interferes with hormone synthesis of other pituitary hormones
Damage to the pituitary stalk may result in an increase in:
a. FSH
b. GH
c. ACTH
d. PRL
e. TSH
D. PRL
During a fast, GH secretion is stimulated by:
a. Insulin
b. Glucagon
c. Ghrelin
d. Somatostatin
e. GnRH
B. Glucagon
The pituitary cell that produces two hormones is the:
a. Thyrotrope
b. Gonadotrope
c. Corticotrope
d. Somatotrope
B. Gonadotrope
A 74-year-old patient recovering from a surgical procedure complains of headache, difficulty concentrating, impaired memory, muscle cramps, and weakness of 48 hour duration. On examination, vital signs are all within normal range, and there are no signs of dehydration or of edema. Laboratory values report serum sodium of 120 mmol/L (nl, 136-145 mmol/L), Which of the following would be compatible with a differential diagnosis of syndrome of inappropriate ADH secretion?
a. Low plasma AVP levels
b. Serum osmolarity of 265 mOsm/L (nl, 285-295 mOsmol/L)
c. Plasma glucose 300 mg/dL
d. Urinary osmolarity <400 mOsm/L
B. Serum osmolarity of 265 mOsm/L (nl, 285-295 mOsmol/L)
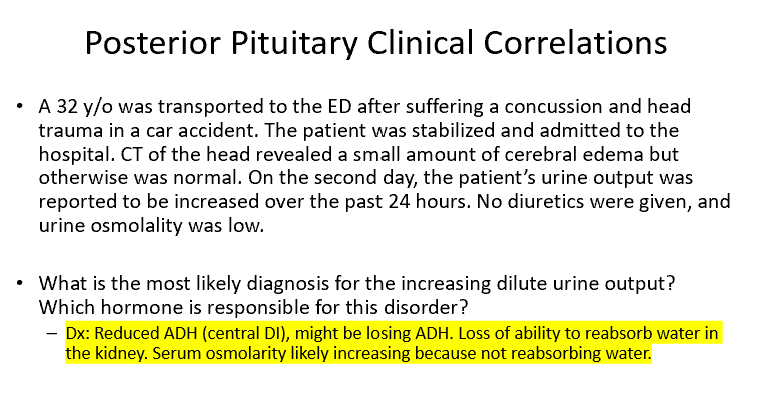
What is the most likely diagnosis for the increasing dilute urine output? Which hormone is responsible for this disorder?
Dx: Reduced ADH (central DI), might be losing ADH.
Loss of ability to reabsorb water in the kidney.
Serum osmolarity likely increasing because not reabsorbing water.
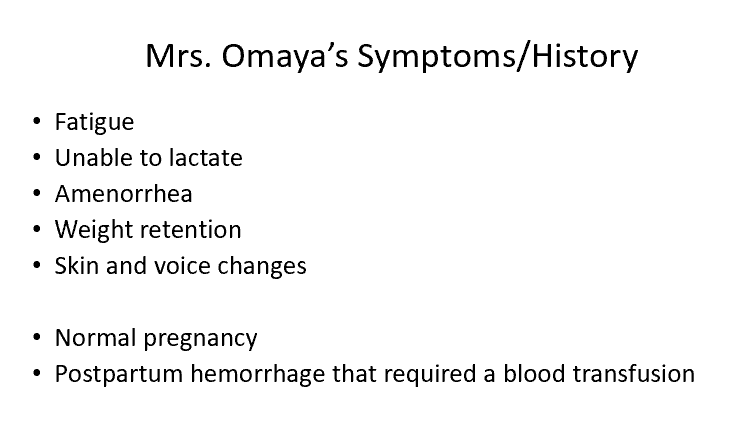
Why are pregnant women susceptible to pituitary infarction?
Body produces more hormones to maintain pregnancy (estrogen, progesterone, prolactin!). Anterior Pituitary grows in size due to this increase in prolactin (hyperplasia/hypertrophy), requiring greater blood supply.
In some cases of Sheehan’s syndrome the posterior pituitary is relatively unaffected. How can you explain this finding?
Different blood supply! Post and Ant get different blood supply. Anterior could be affected to a greater extent than the posterior pituitary.
Prolactinemia
Serum prolactin levels between 20 and 200 ng/ml can be found in patients with any cause of hyperprolactinemia
Prolactinoma >1 cm
PRL levels with typically be >200 ng/ml; <1 cm levels will typically be >100 and <200 ng/ml
Causes of Hyperprolactinemia
Pregnancy
Nipple stimulation
Stress
Decreased dopamine inhibition
Estrogen
Hypothyroidism
Chronic renal failure
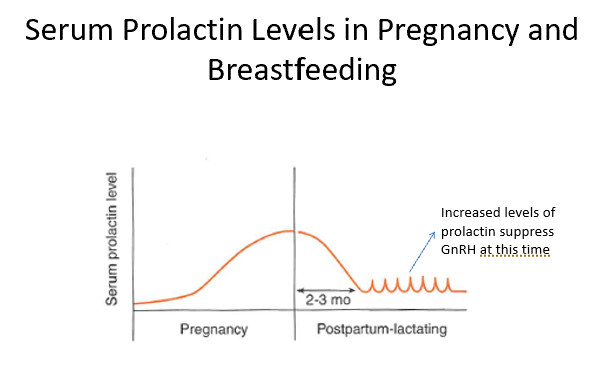
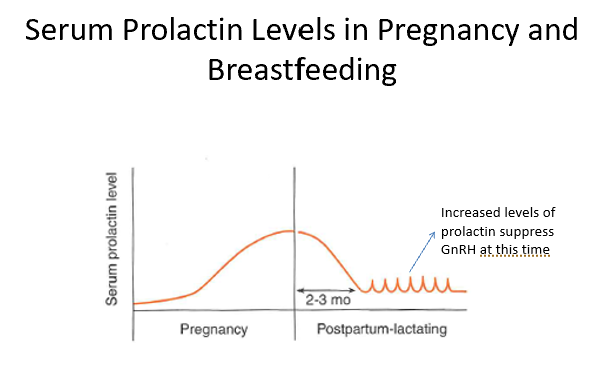
Pregnancy and Prolactin
During pregnancy, prolactin levels increase. Increasing anterior pituitary size.
Postpartum, prolactin levels fall.
If breastfeeding, prolactin levels spike!
Prolactin inhibits GnRh! (inhibiting LH/FSH)
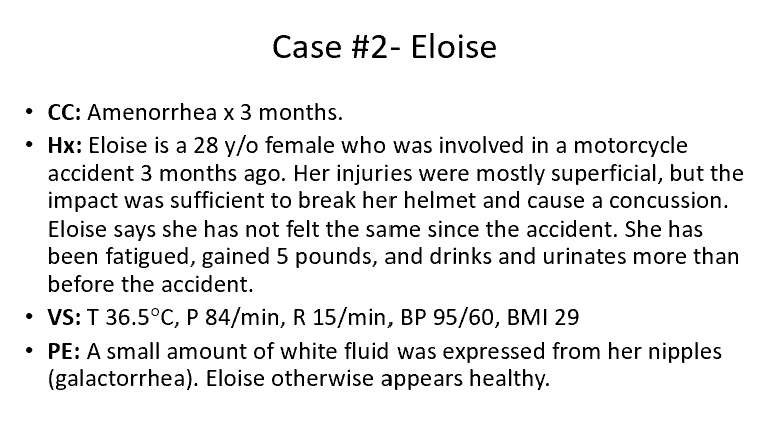
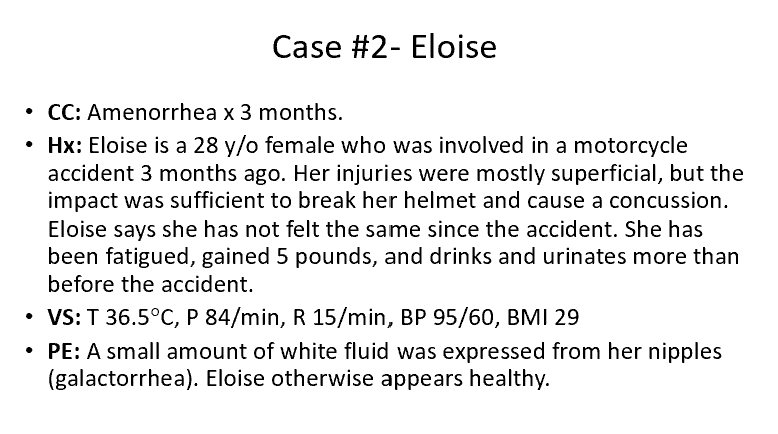
Based on Eloise’s symptoms and past medical history which condition is she most likely to have?
a. Ischemic necrosis of the pituitary
b. Traumatic damage to the pituitary stalk
c. Prolactinoma- adenoma of the lactrotropes
d. Increased prolactin secretion due to use of a dopamine antagonist
e. Hypothyroidism
B- Traumatic damage to the pituitary stalk. If there’s head trauma and hypothalamus is affected, all hormones from pituitary that rely on hypothalamus hormones will be affected!
TSH
LH
FSH
The only one that works differently is prolactin (if anterior pituitary is intact).
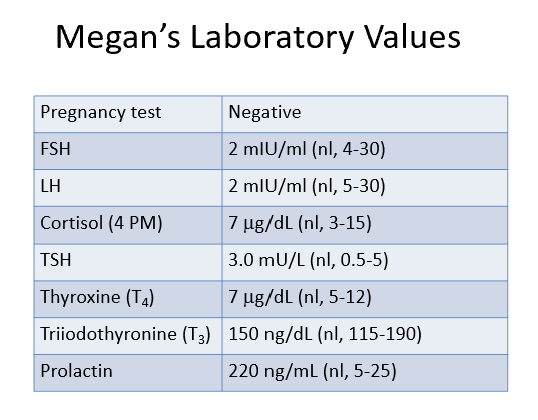
What is the most likely cause of Megan’s prolactinemia?
a. Ischemic necrosis of the pituitary
b. Hypopituitarism due to damage to the pituitary stalk
c. Prolactinoma- adenoma of the lactrotropes
d. Increased prolactin secretion due to use of a dopamine antagonist
e. Hypothyroidism
C- Prolactinoma- adenoma of the lactrotropes.
Look for high elevation of prolactin (specifically over 100 for prolactinoma)!
For D- there’s no indication that she’s on a dopamine antagonist. Also, dopamine/antagonist for dopamine would only cause an increase UP TO 100, not over.
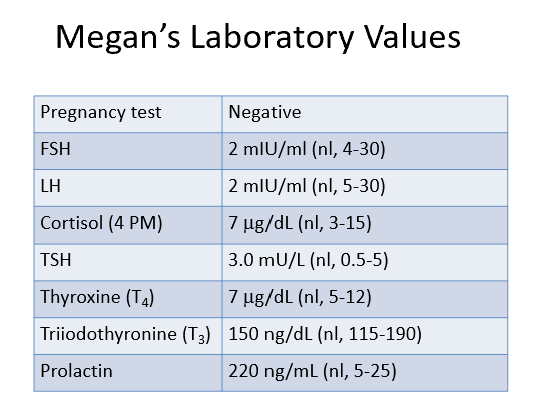
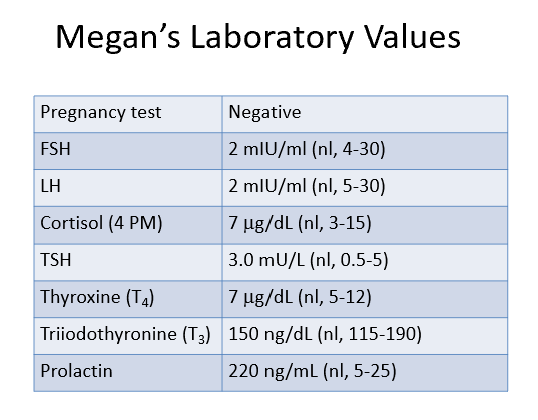
What is the likely cause of Megan’s low LH and FSH levels?
a. Negative inhibition due to high prolactin levels
b. Negative inhibition due to stress
c. Loss of LH and FSH secretion due to lactotroph hyperplasia
d. Negative inhibition due to high estrogen levels
A- Negative inhibition due to high prolactin levels.
High prolactin inhibits GnRH, causing LH and FSH to be decreased! (estrogen and progesterone will be decreased too)
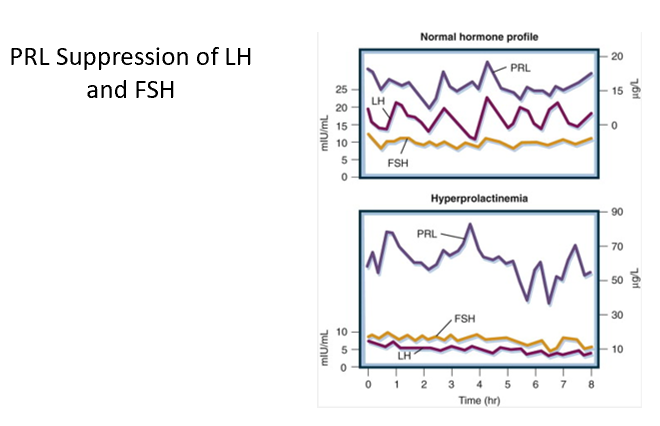
GH Levels Over Time
GH increases rapidly starting at birth, steady pre-adolescent years. Spike/peak in adolescent years (earlier for females, just slightly). Declines through adult years.
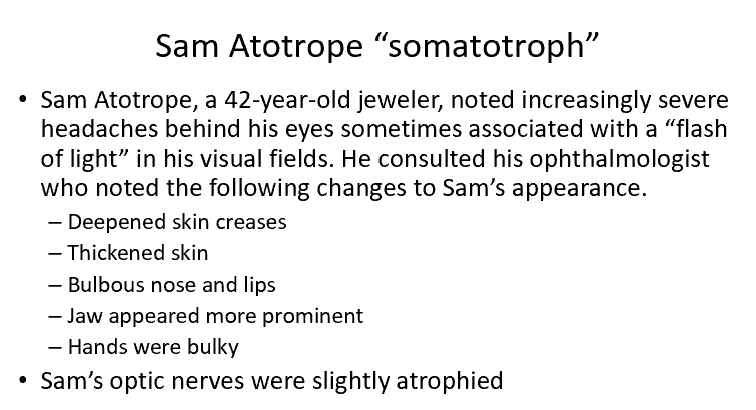
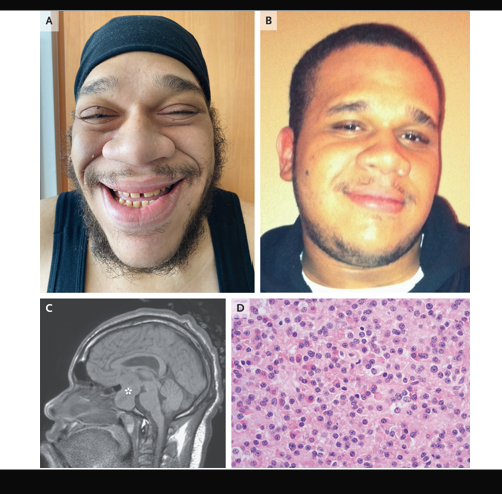
Somatotroph Adenoma Case
The physical changes and the bitemporal hemianopsia are consistent with excess growth hormone (acromegaly).
The MRI of Sam’s brain revealed a macroademona in the pituitary gland that compressed the optic nerve.
GH Levels Eating vs Fasting
When we eat, GH tends to be suppressed. Pulsatile!
Fasting days, not eating, larger and more frequent peaks in GH!
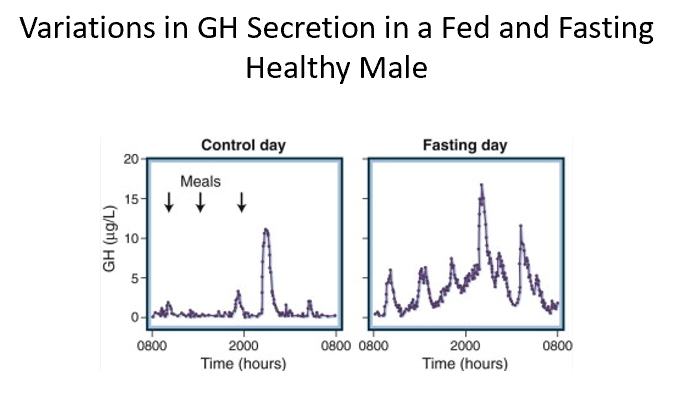
A patient was scheduled for a growth hormone suppression test. If each of the following events occurred the morning of the test, which of the events would be most likely to suppress growth hormone levels?
a. She ate four large doughnuts for breakfast.
b. While unlocking her car, she was chased by the neighbor’s vicious dog.
c. She fell asleep at the start of the test and slept soundly until it was completed 1.5 hours later.
d. She forgot to eat her breakfast before the test.
A- She ate four large doughnuts for breakfast.
Large amount of glucose, suppressing growth hormone!
Everything else is a stimulant for GH!