Physiology- Hematology
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
components of blood
Plasma (55%)- noncellular component
Buffy coat (<1%)
Erythrocytes (45%)
total blood volume for humans
women = 5L
men= 5.5L
plasma
non cellular
PLASMA PROTEINS
antibodies
coagulation factors
ALBUMIN
drives oncotic pressure/gradient
carrier protein
90% water + dissolved substances
vitamins and nutrients
electrolytes (ex. Na+, K+, etc)
hormones
functions of plasma proteins
EST ONCOTIC GRADIENT
help maintain pH (act as buffer)
transport poorly soluble substances (by binding to transport proteins)
aid in immunity (immunoglobulins)
promote blood clotting
what organ is primarily responsible for the production of plasma proteins?
liver
osmosis
move down concentration gradient
high concentrate of H2O→ low concentration of H2O
albumin
primary driver of oncotic pressure
most abundant plasma protein
how does the presence of albumin in blood prevent edema?
the high concentration of albumin in blood pulls water/fluid into vessels instead of into tissues (osmosis)
intravascualr space/vasculature
plasma
intersistial space/fluid
fluid btwn cells
intracellular fluid
fluid inside cells
flow of blood
heart→ arteries (nutrient and oxygen rich)→ capillary beds (exchange for nutrient and oxygen poor blood)→ veins→ heart→ lungs
capillaries
specialized vessels
sites of exchange btwn plasma and tissue cells
oxygen and nutrient rich blood diffuses into tissue via FILTRATION (exits arterial end) and diffuses out of the tissue via REABSORPTION (venous end- now oxygen poor)
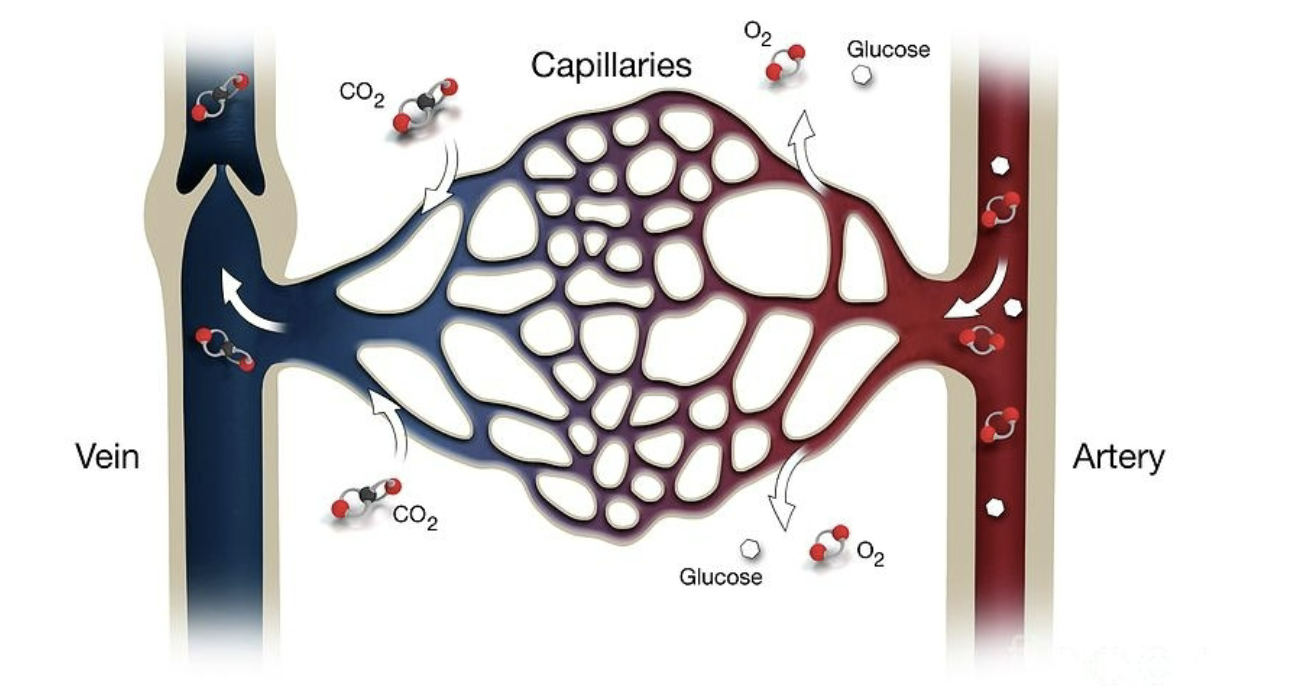
characteristics of capillaries
thin walls (1 endothelial cell)
easier for filtration and reabsorption
extensive branching = large surface area for exchange
velocity of travel is slow
walls range in “porosity” depending on the target organ
fenestrations= pores (larger → easier filt/reab)
capillary filtration
mvmt of fluid OUT of the capillary and into interstitial space
capillary reabsorption
mvmt of lfuid back INTO capillary
what are the forces that drive mvmt of fluid in/out of capillaries
pressure gradients
hydrostatic pressure: mechanical force (blood pressure)
oncotic pressure: force drawing water to area of HIGHER particle conc (albumin greater in vasculature)
arterial end of capillary bed
hydrostatic pressure (blood pressure) > osmotic pressure
closer the heart, therefore greater pressure
fluid moves out of the capillary into interstitial space (filtration)
venous end of capillary bed
osmotic/ oncotic pressure > hydrostatic pressure
fluid moves back into capillary (reabsorption)
what happens with an increase in hydrostatic pressure
more filtration occurs → edema
what happens with a decrease in albumin?
decrease in osmotic pressure→ edema (water no longer wanting to go into vasculature/ no longer low concentration of H2O)
why is there an excess amount of fluid in the belly for Kwashiorkor
malnutrition
there is a loss of albumin production in the liver due to lack of nutrients/proteins
not enough solute (albumin) in vasculature→ fluid comes out due to concentration gradient
what is hematopoiesis
production of blood cells
characteristics of hematopoiesis
ALL blood cells develop from the same HEMATOPOIETIC STEM CELL in bone marrow
differentiation is driven by different cytokines, hormones, and growth factors
what types of cells can stem cells differentiate into
leukocytes (WBCs)
erythrocytes (RBCs)
thrombocytes (platelets)
differentiation of hematopoietic stem cells into RBCs
erythropoiesis → erythropoietin
differentiation of hematopoietic stem cells into WBCs
leukopoiesis→ growth factors and cytokines
differentiation of hematopoietic stem cells into platelets
thrombopoiesis→ thrombopoietin
characteristics of erythrocytes (RBCs)
looses most of it’s organelles
no nucleus
no mitochondria (conserve oxygen it carries)
flexible surface membrane
move through small capillaries
bioconcave
maximize surface area
contains hemoglobin
oxygen carrying molecule
contains iron
structure of hemoglobin
GLOBIN
structural protein with 4 subunits (2 alpha and 2 beta)
HEME
iron groups found in globin subunits
carry 1 molecule of oxygen each
how many molecules of oxygen can 1 RBC carry?
250 hemoglobin (in 1 RBC) x4 oxygens= 1 billion
why is hemoglobin needed?
oxygen is poorly soluble in the blood→ needs transport protein
what is a possibility of going wrong with binding to hemoglobin?
other molecules can bind to heme
binding affinity of CO>O2—> carbon monoxide poisoning
variations of Hemoglobin
HbA
HbA1c
HbF
HbA
2 alpha chains
2 beta chains
92% of adult Hgb
HbA1c
avg glucose number over ~3 months
spontaneously binds glucose over time
2 alpha chains
beta-NH glucose
increased in diabetes
HbF
2 alpha chains
2 gamma chains
major fetal Hgb
promotes oxygen transfer across placenta as it more tightly binds to O2
what drives erythropoiesis (creation of more RBCs)?
hypoxia drives erythropoietin (EPO) production in kidney→ EPO travels to bone marrow→ erythropoiesis
why is EPO produced by the kidney
the organ receives extreme high blood flow for filtration adn reabsorption, therefore is sensitive to changes in O2
clinical correlation: lance armstrong
use of synthetic EPO→ increase of erythrocyte production→ increased amount of O2 to tissues
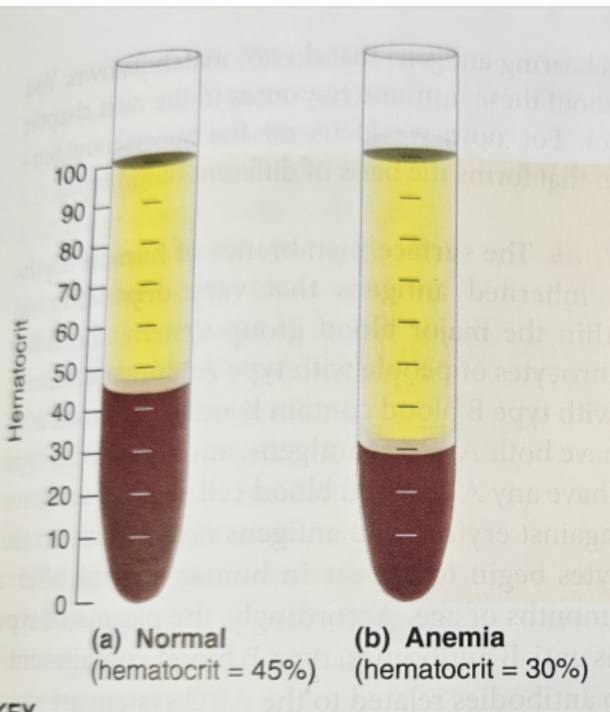
anemia
decreased hematocrit
normal erythrocyte count (hematocrit) is 45%
CAUSE DECREASE IN O2 and PERFUSION
causes of anemia
destruction/loss of RBCs
hemorrhage
hemolysis
decreased production
nutritional deficiencies (iron, B12, folate)
renal anemia (kidneys cannot produce EPO)
ex. pt with chronic kidney disease or renal failure
aplastic anemia (bone marrow dysfunction)
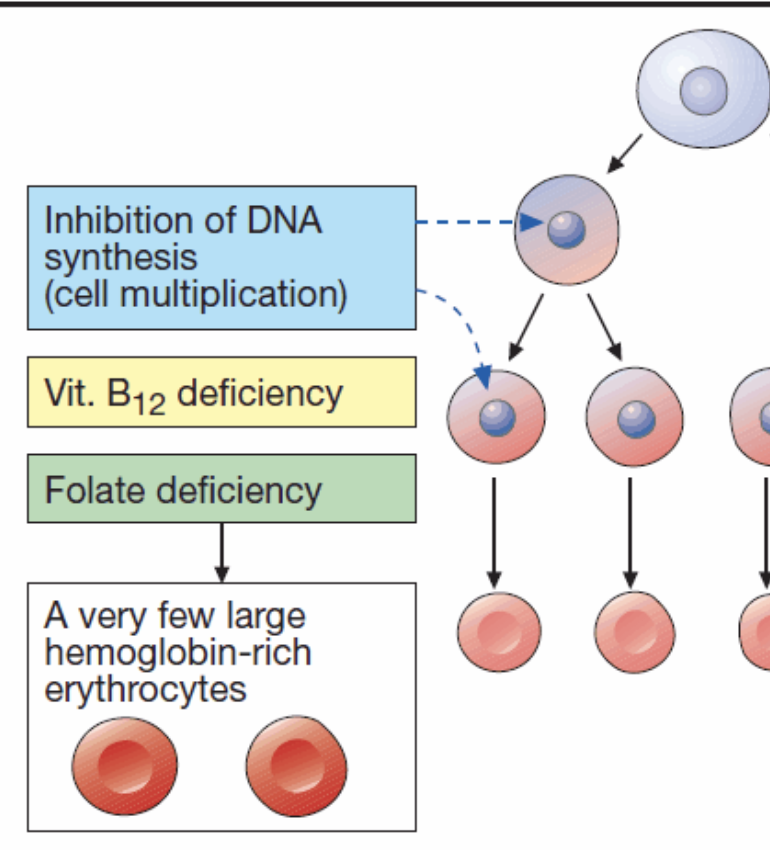
Vitamin B12 or folate deficiency
macrocytic anemia
B12 and folate needed to promote DNA synthesis and cell division, therefore low levels → inhibition of DNA synthesis (cell. multiplication)
very few, large hemoglobin rich RBCs
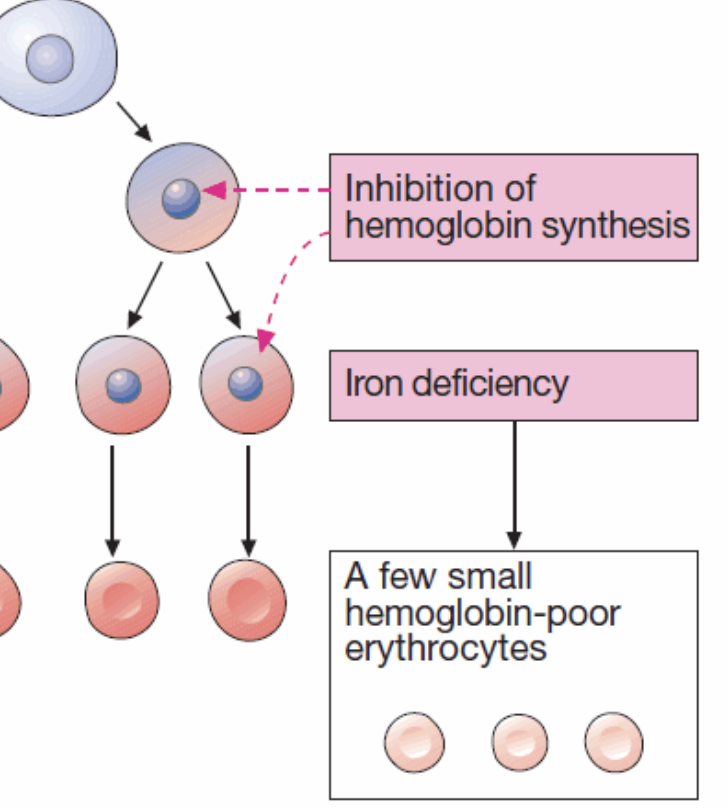
iron deficiency
microcytic anemia
low levels of iron→ lack of hemoglobin→ inhibition of hemoglobin synthesis→ small hemoglobin-poor erythrocytes (pale in color)
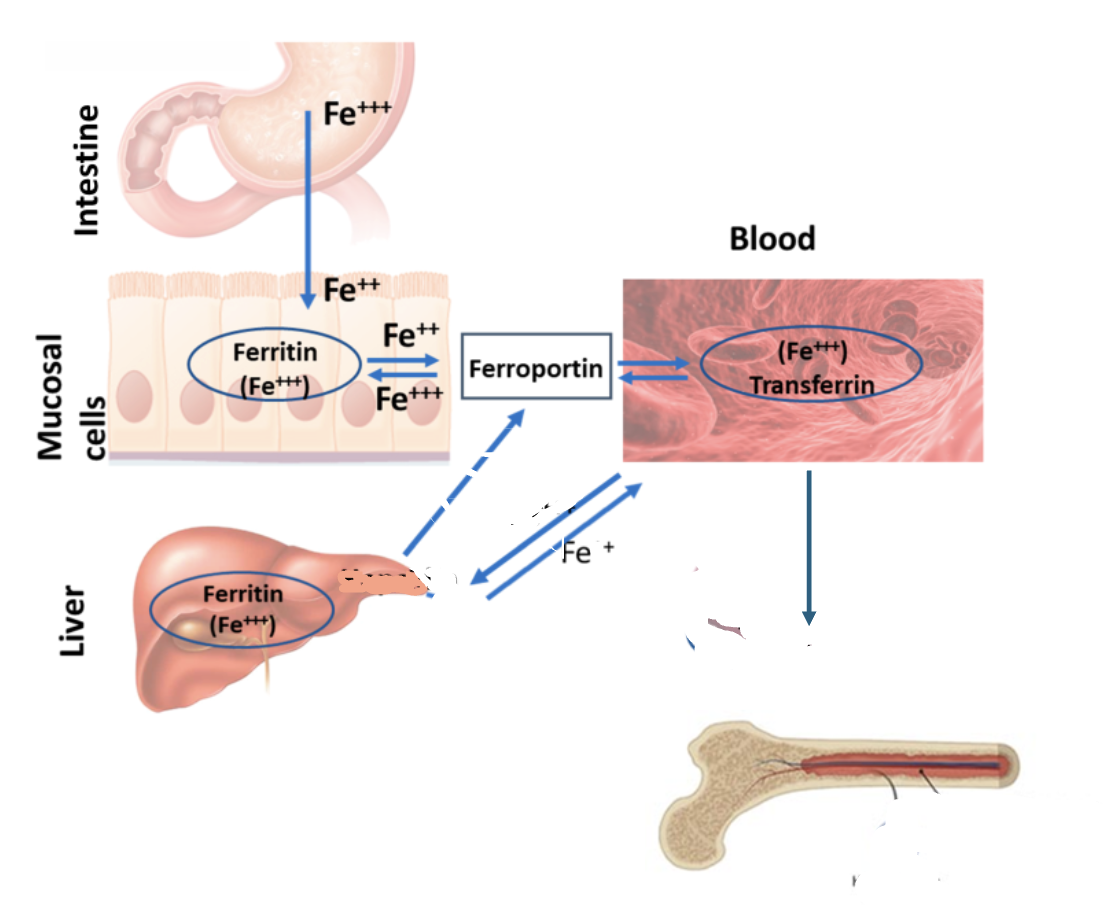
iron absorption and metabolism
iron is needed for hemoglobin synthesis
acquired through GI tract; absorbed in duodenum by enterocytes
how is iron stored
in cells within protein ferritin (in liver)
iron metabolism
iron absorbed in GI tract needs to be transferred to the liver for storage and bone marrow for erythropoiesis
transferred by transfer protein transferrin (in blood)
RBC life cycle
100-120 days
aging→ structural proteins that allow for flexibility breakdown
RBCs become stiff and get stuck in small capillaries in spleen→ RBC breakdown
macrophages ingest and breakdown Hgb
IRON is RECYCLED and stored in the liver (within ferritin)
HEME is broken down into bilirubin (conjugated in liver → make bile)
structure of arterial wall
1) tunica intima: innermost layer
composed of endothelial cells
secretes chemical substances that affect blood clotting
2) tunica media: middle layer
composed of smooth muscle
vasoconstriction/vasodilation
3) tunica externa; outermost layer
composed of collagen and elastic fibers
give vessel great flexibility
what is hemostasis
the localized stoppage of bleeding
three major steps of hemostasis
1) vascular spasm
2) formation of platelet plug
3) blood coagulation (clotting)
cellular and molecular components of hemostasis
1) thrombocytes
2) coagulation factors
thrombocytes in hemostasis
thrombopoiesis: thrombopoietin (TPO- produced by liver and kidney) stimulates myeloid stem cell to differentiate into thrombocyte
TPO producion is stimulated by inflammatory cytokines
ex. chronic inflammation leads to increased risk of blood clots; increased inflammatory cytokines→ increased production of TPO→ increased production of thrombocytes
coagulation factors in hemostasis
produced by liver→ circulate throughout serum to be ACTIVATED by other protein/enzymes
inactive in blood
what prevents blood from spontaneously clotting?
1) endothelial cells
release N2O- inhibits platelet adhesion to endothelial wall
surface contains heparin -- inactivates clotting factors
2) forward mvmt of blood flow keeps platelets from sticking to endothelial surface
3) platelets and clotting factors are in their INACTIVE forms when circulating in the plasma
why are people more at risk of developing a blot clot when not consistently moving?
decrease in movement→ decrease in blood flow→ increased risk due to blood pooling
what is the underlying mechanism that results in hemostasis
1) injury triggers VASOSPASM to reduce size of vessel injury; “shrink the wound”/contract
injured endothelial cells secrete endothelin → triggers tunica media contraction (vasoconstriction)
direct injury to smooth muscle stimulates contraction reflex
2) platelets collect and adhere to site of injury to form platelet plug
vWF (von willenbrand factor) binds to exposed collagen from injury ( found in connective tissue underlying endothelial lining)
vWF serves as a bridge btwn fast moving platelets and injured vessel wall
binding of platelets and vWF to collagen= platelet activation
activated platelets secrete ADP and thromboxane A2 (to activate more platelets and increase ADP)
ADP causes nearby platelet surfaces to become sticky
thromboxane A2 directly promotes platelet aggregation + promotes release of more ADP from activated platelets
injured epithelial cells are no longer abel to secrete N2O
3) coagulation cascade is activated
loss of heparin - no longer inactivating clotting factors
4) damaged edges of vessel are pulled together (RETRACTION) and begin healing (REPAIR)
repair stimulates by:
platelet release of platelet-derived growth factor (PDGF)— patch up collagen, repair smooth muscle
endothelial cell release of vascular endothelial growth factor (VEGF)—renew endothelial linning
5) remove the clot through fibrinolysis
endothelial cells release tissue plasminogen activator (TPA)
converts plasminogen —> PLASMIN (active)—eats away at the clot
byproducts= FIBRINOGEN and D-DIMER
two pathways to activate coagulation
intrinsic and extrinsic
intrinsic pathway
activated by exposed collagen under vessel surface
damage INSIDE vasculature
ex. putting in a line
longer pathway; involves factors XII, XI, IX, VIII
goes to “common pathway” to factor X→ thrombin→ fibrinogen→ fibrin clot
tested by aPTT
pt ability to clot/clotting time
extrinsic pathway
activated by tissue damage
when damaged tissue releases tissue factor (III)
ex. cut
shorter pathway; factor VII
goes to “common pathway” to factor X→ thrombin→ fibrinogen→ fibrin clot
tested by PT/INR
pt ability to clot/clotting time
where does the common pathway converge
factor X
what would you expect on a PT/INR from a pt with cirrhosis
elevated PT/INR
the liver is the site of formation for most clotting factors, therefore if it is not functioning appropriately, there will be a decrease in production of clotting factors (such as factor VII), therefore increasing the time it takes to create a clot
Hemophilia is a disorder in which patients experience excessive bleeding/deficiencies in hemostasis. What might be the underlying pathophysiologic mechanism?
Hemophilia A is factor VIII deficiency
factor VIII (intrinsic pathway) deficiency will result in INCREASED aPTT, representing an issue in the intrinsic pathway clotting mech
warfarin inhibits vitamin K dependent clotting factors. What can be expected to be seen on testing for a patietn on warfarin?
elevated PT/INR
factor VII is a vitamin K dependent CF (extrinsic pathway), therefore if vitamin K is inhibited, factor VII is not created and th extrinsic pathway is “damaged” revealing an elevated read due to longer clotting time
which pathway does heparin mainly affect? what test and rest results are expected?
intrinsic pathway
elevated aPTT