Dosage form and compounding final
1/293
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
294 Terms
Requirements for dosage forms (5)
- chemical & physical stability
- suitable preservation needed
- uniformity of drug across entire dosage form
- acceptability-patient compliance
- suitable packaging and labeling
Need for dosage forms: Which dosage form is used to protect a drug from oxygen or humidity?
coated tablets
Need for dosage forms: Which dosage form is used to protect a drug from gastric acid after oral administration?
enteric coated tablets
Need for dosage forms: Which dosage form is used to conceal bitter, salty, or offensive taste/odors of drugs?
sugar coated tablets
Need for dosage forms: Which dosage form is used to provide unstable or insoluble drugs in the desired liquid preparations?
syrups and suspensions
Need for dosage forms: Which dosage form is used for rate-controlled drug action/controlled release drug delivery systems?
gels and patches
Need for dosage forms: Which dosage form is used for optimal drug action from topical administration?
creams and ointments
Need for dosage forms: Which dosage form is used to provide for insertions of a drug into one of the body's orifices?
suppository
Need for dosage forms: Which dosage form is used to provide for placement of drugs directly into circulation or tissues
IV, SC, and IM
Need for dosage forms: Which dosage form is used to provide optimal drug action through inhalation therapy?
DPIs, nasal spray
Hepatic metabolism
when a drug is absorbed from the gut and delivered to liver via the portal circulation
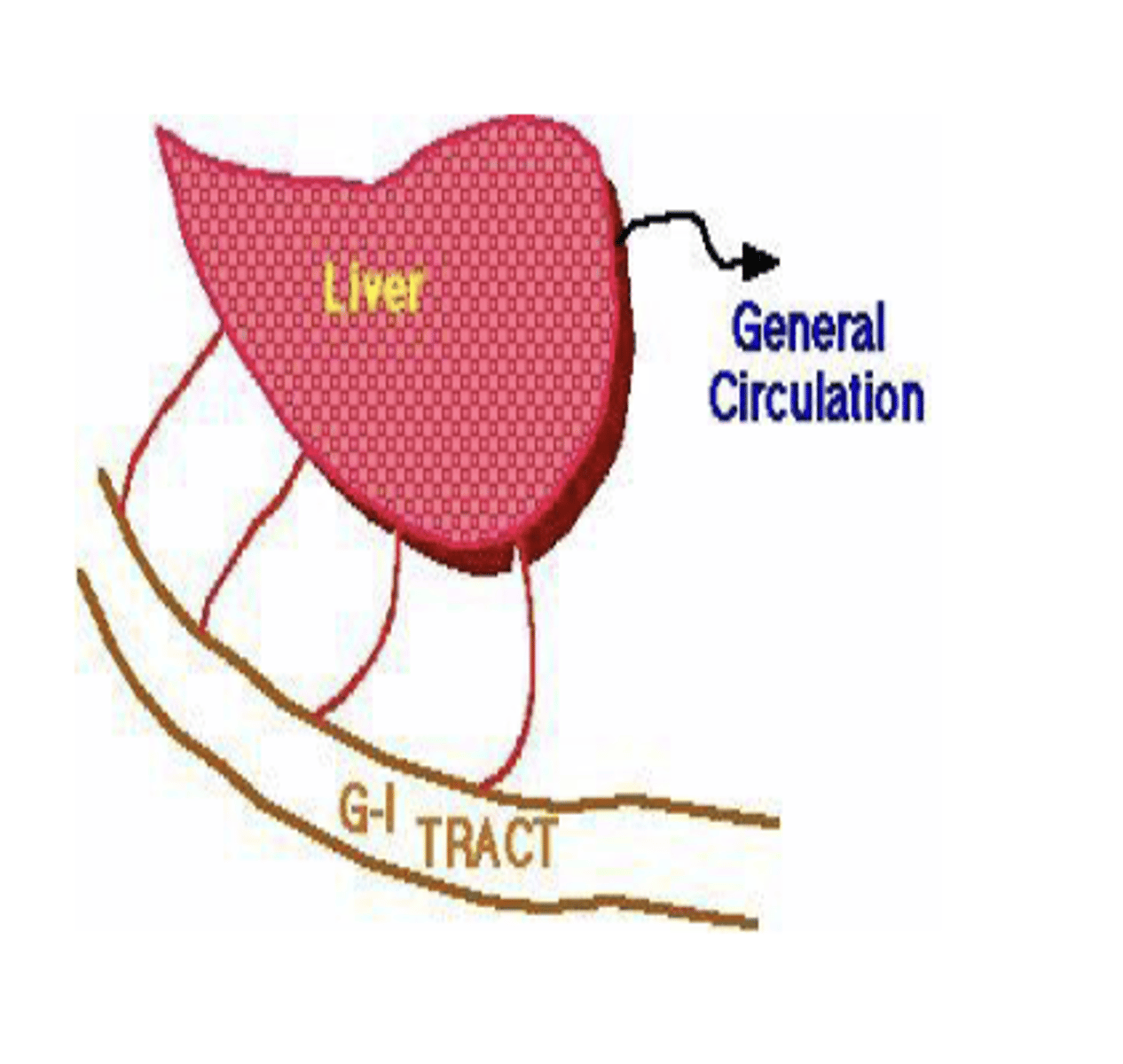
First-pass effect
when a drug's concentration is significantly reduced prior to reaching circulation
- occurs during its initial passage through the liver after absorption from the GI tract
A drug administered parenterally is injected....
Examples? (6)
through the hollow of a fine needle into the body at various sites and to various depth
- IV
- IM
- SC
- Intradermal
- Epidural
- Intrathecal
What is the most important requirement for an injectable preparation?
must be sterile and pyrogen free
Choose the correct statement: When using injectable medications...
A. No drug is lost
B. Sometimes small amounts of drug are lost
B. Sometimes small amounts of drug are lost (air bubbles, liquid may stay in vial)
Advantages of parenteral routes (3)
▪ Enables use of drugs that are destroyed, inactivated, or poorly absorbed when taken orally
▪ Bypasses liver, avoiding first-pass effect
▪ Ideal for patients who are:
•Unconscious
•Unable to take oral medications
Intramuscular route
- its less rapid than what?
- more rapid than what?
- where is the injection site?
- what is the volume of injection?
- less rapid but longer lasting than IV- second only to IV route in rapidity of onset of action
- more rapid than PO
- injection site is deep in skeletal muscle
- 0.5-2 mL
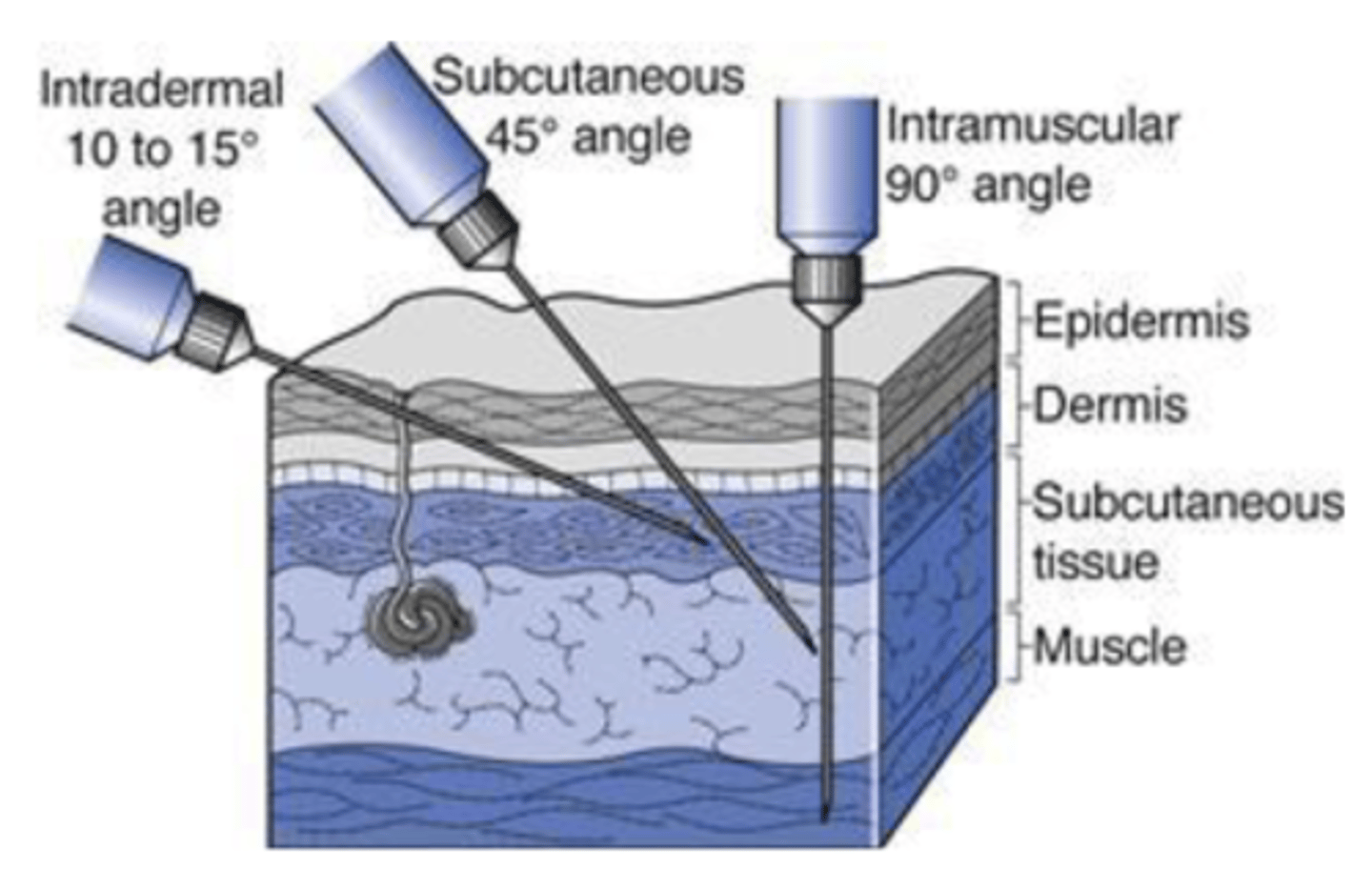
Subcutaneous route
- where is the injection site?
- onset of action is slower than what? faster than what?
- is it suitable for self administration?
- limited to volume _______.
- connective tissue below the skin, between dermis and muscle
- slower than IM, faster than PO
- suitable for self admin
- ≤ 1.3 mL
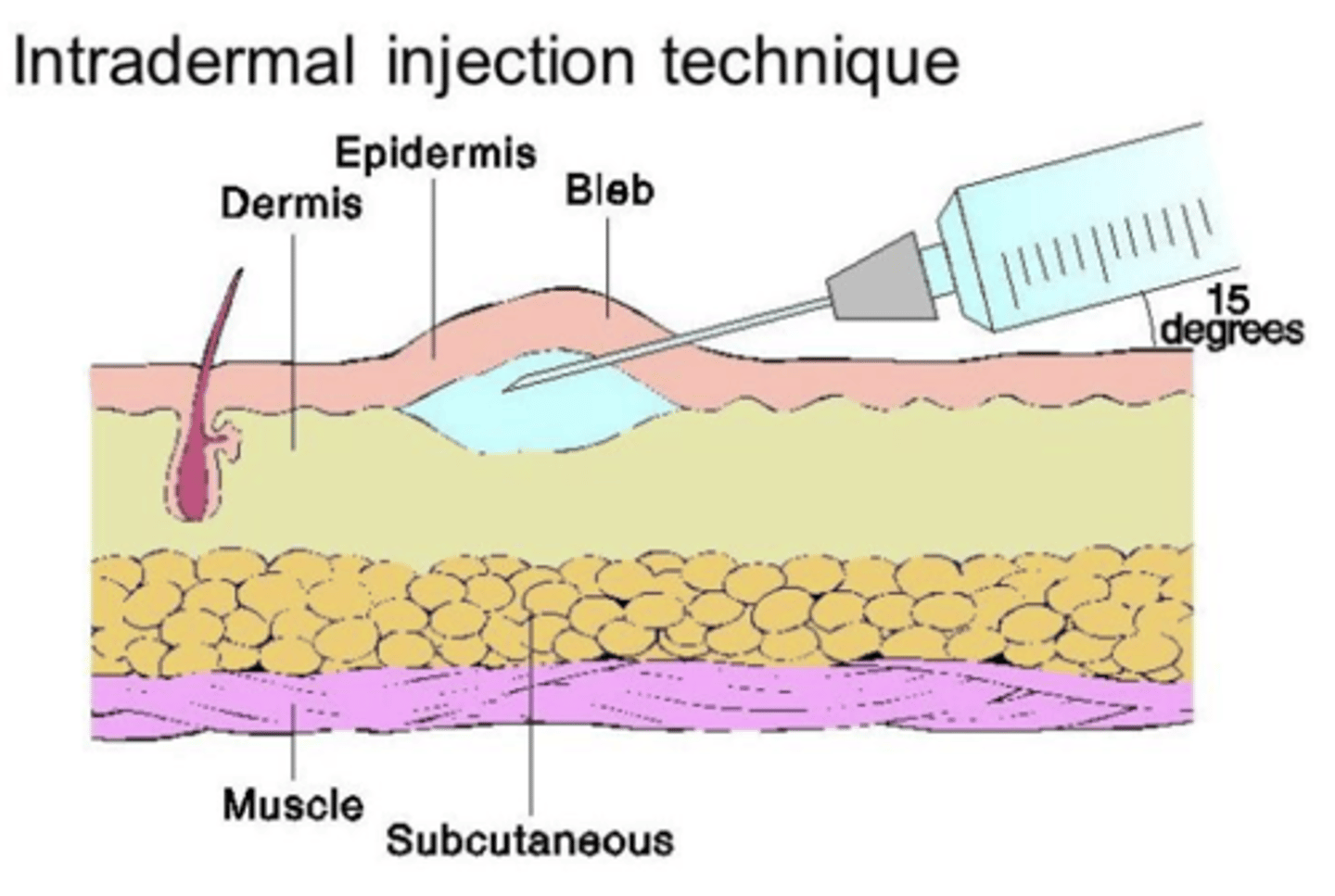
Intradermal route
- where is the injection site?
- typically used for small volume ____-____
- what diagnostic measures is it used for?
- into the dermis rather than beneath
- 0.05-0.1 mL
- allergy test or tuberculin skin test
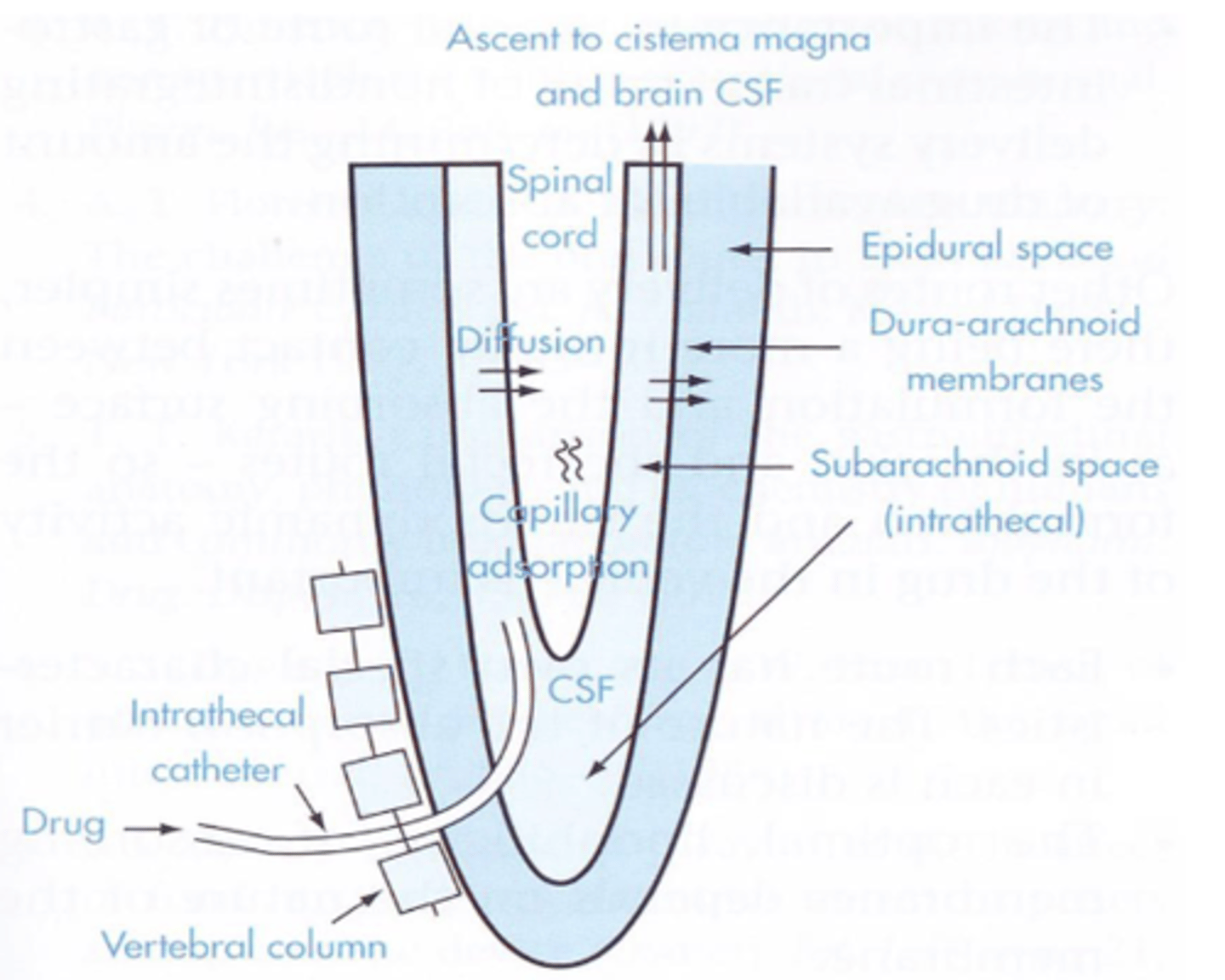
Epidural route
- where is the drug delivered to?
- where are clinical effects localized to?
- examples? (3)
- outside of the dura and not into the cerebrospinal fluid
- localized to spinal cord
(morphine sulfate extended, steroids, anesthetics)
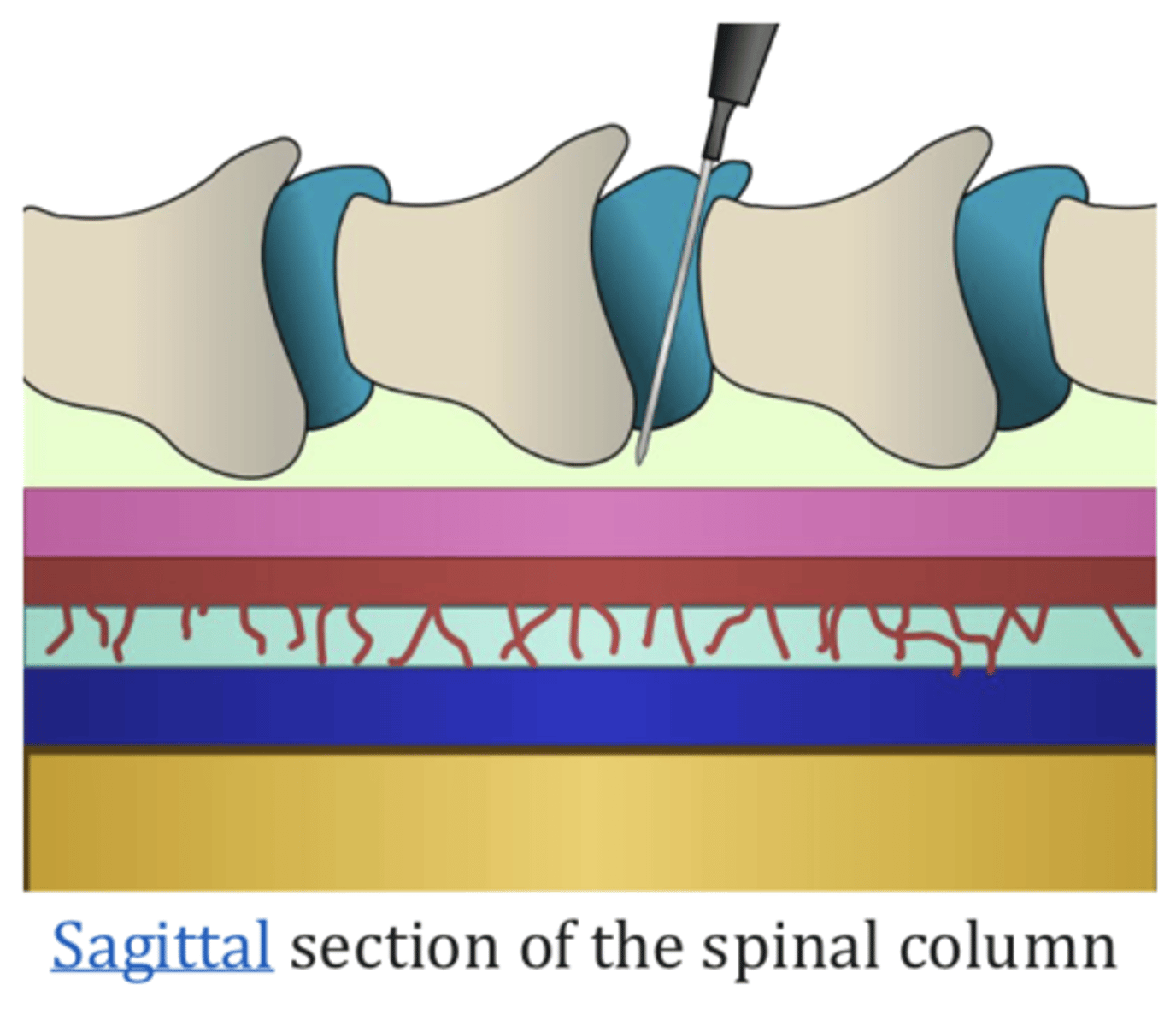
Intrathecal route
- delivers drug to where?
- what is it used in the treatment of?
- spinal cord and brain
- cancer pain
Ocular administration
application of drug into the eye
- conjunctival, topical, intra-ocular
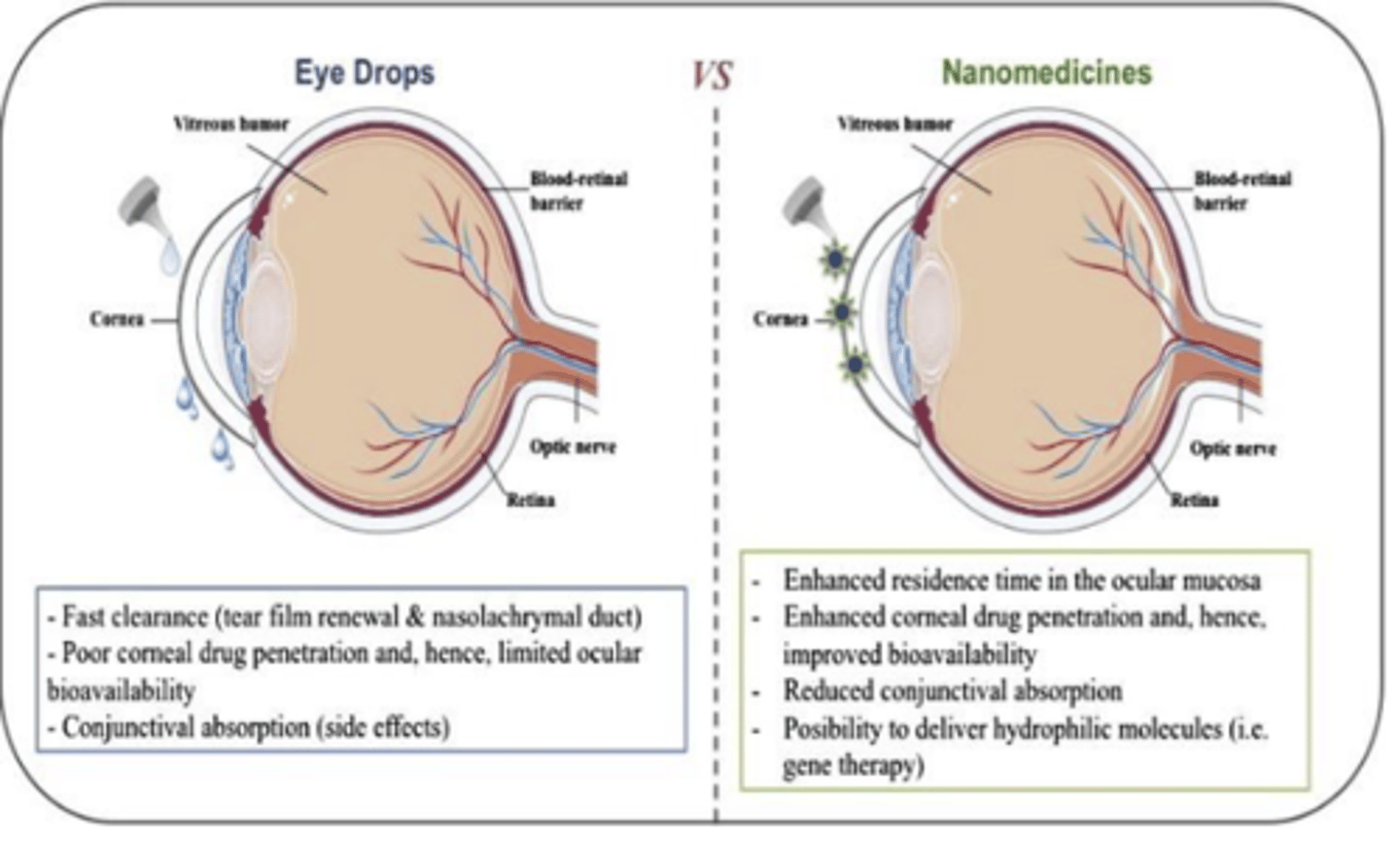
(ocular) Conjunctival
application of a drug to the conjunctival mucosa or lining of the inside of the eyelid
(ocular) Topical
To treat anterior segment diseases
(bimatoprost, tobramycin)
Intra-ocular
VEGF used to treat age related macular degeneration
VEGF (vascular endothelial growth factor-protein that stimulates formation of new blood vessels)
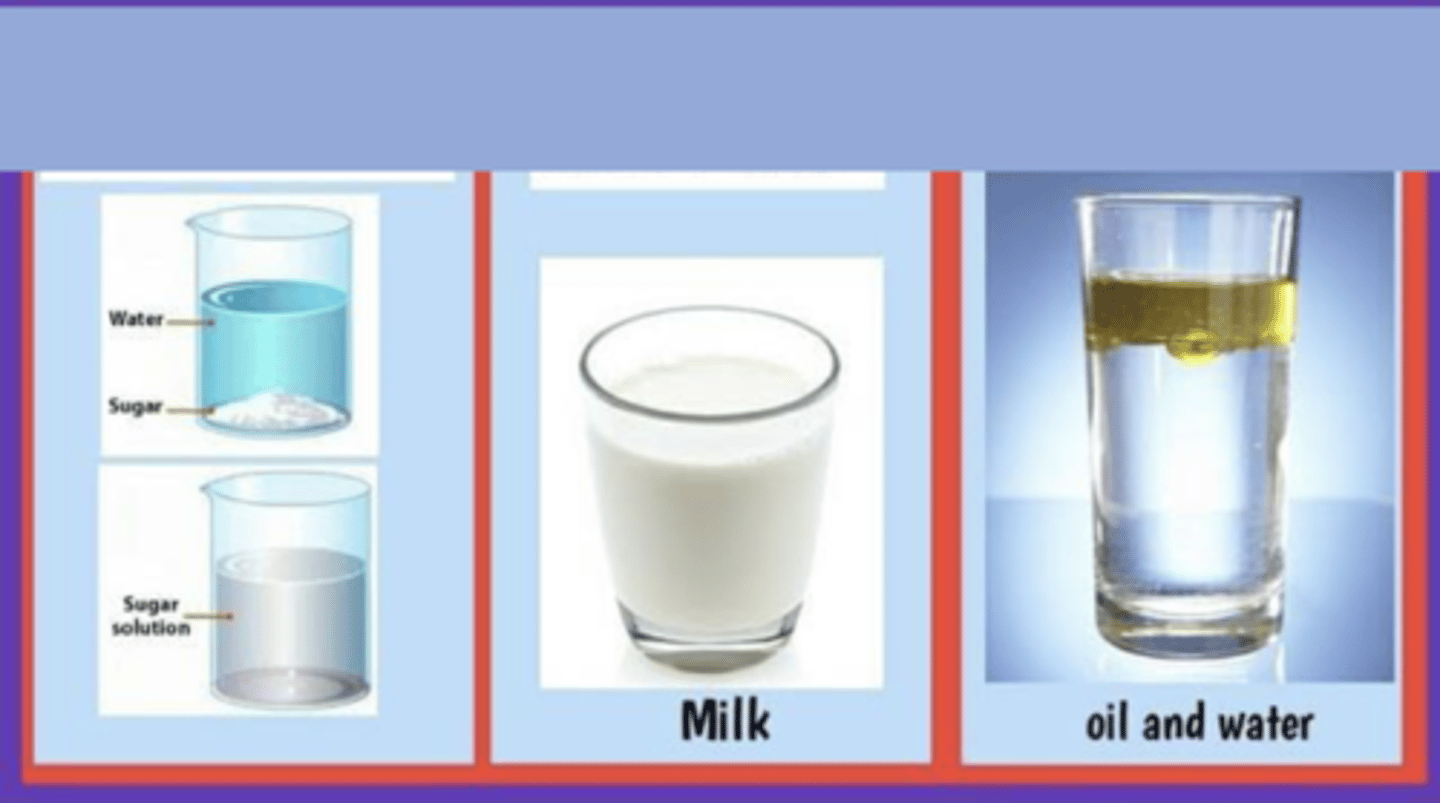
Characteristics of a true Solution: (6)
▪ homogeneous mixture of two or more substances
▪ particles cannot be seen by naked eye
▪ Does not cause beams of light to scatter
▪ A solution is stable
▪ solute from a solution cannot be separated by filtration (or mechanically)
▪ only one phase
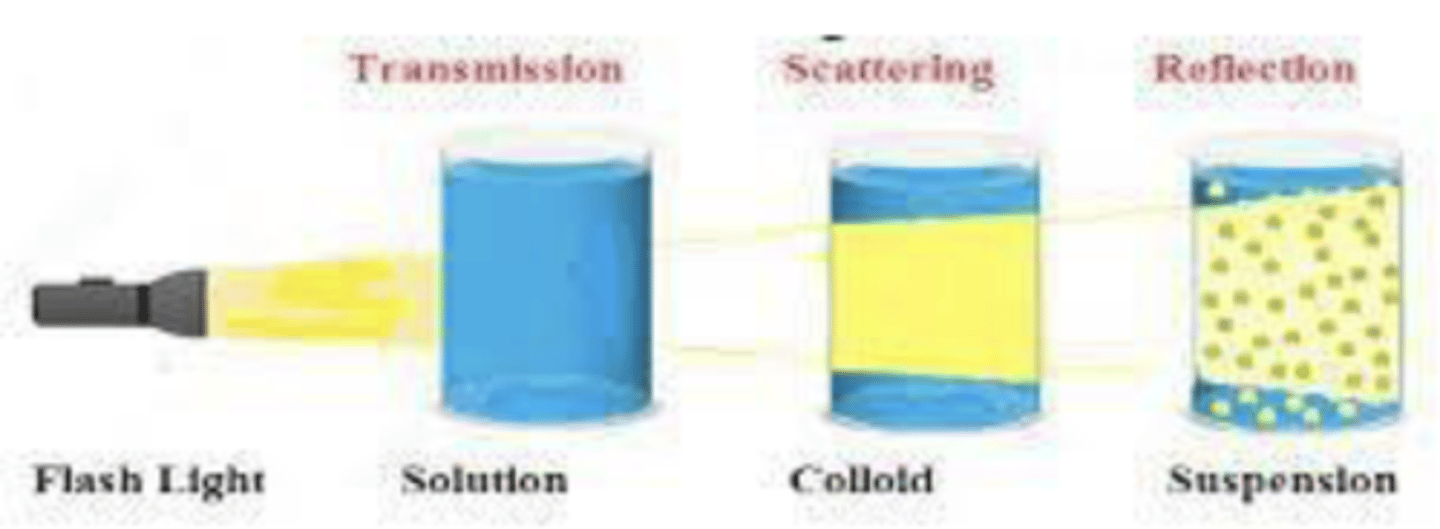
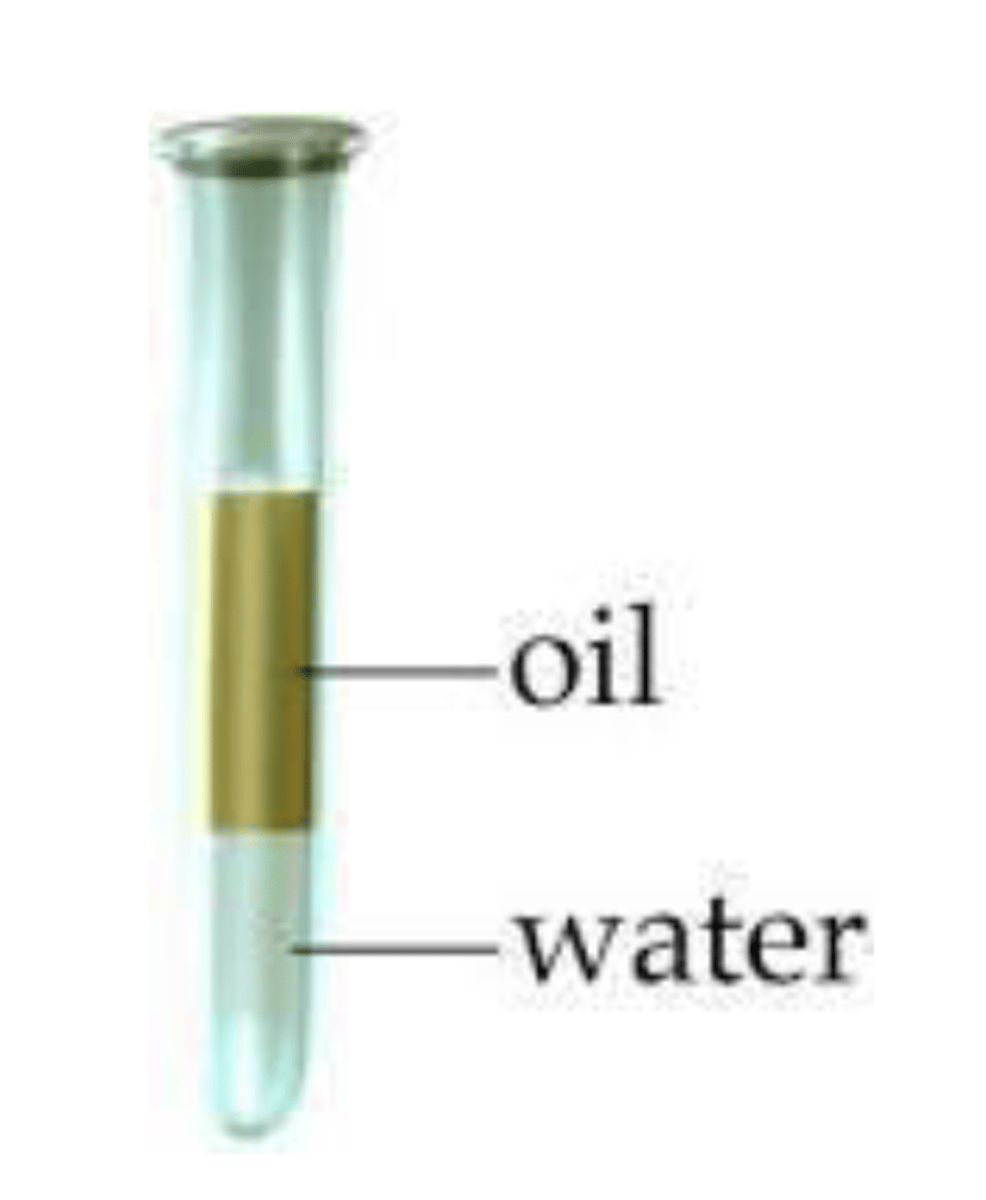
Suspensions are obtained when....
insoluble solid particles are dispersed in a liquid medium
Characteristics of colloids: (5)
▪ homogeneous mixture (under a microscope, are hetero)
▪ solute does not settle out on standing
▪ particles are too small to be seen by naked eyes
▪ Colloids can be distinguished from solutions as they exhibit light scattering
▪ Can be solid, liquid or gas.
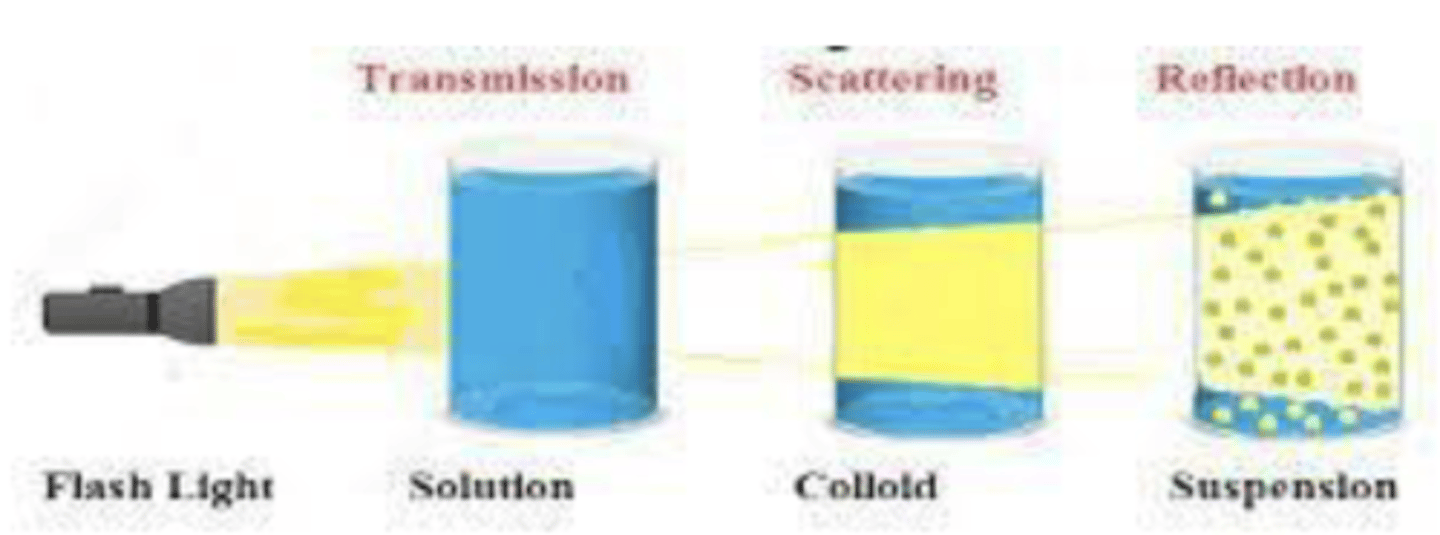
Solution, colloid, suspension comparison
Factors affecting the emulsion type
- Nature of emulsifying agent
- Phase-volume ratio (amounts of oil & water)
- Order of mixing
*****The phase in which the emulsifier is more soluble will be the....
external (continuous) phase- Bancroft’s rule (1913)
******Water-soluble surfactants tend to give what type of emulsions?
o/w emulsions
*****Oil-soluble surfactants tend to give what type of emulsions?
w/o emulsions
A hydrophilic (water-soluble) emulsifying agent will promote the formation of:
A. O/W emulsion
B. W/O emulsion
A. O/W emulsion
Phase-volume ratio
determines the relative number of droplets formed initially
The greater the number of droplets, the greater the chance of.....
collision
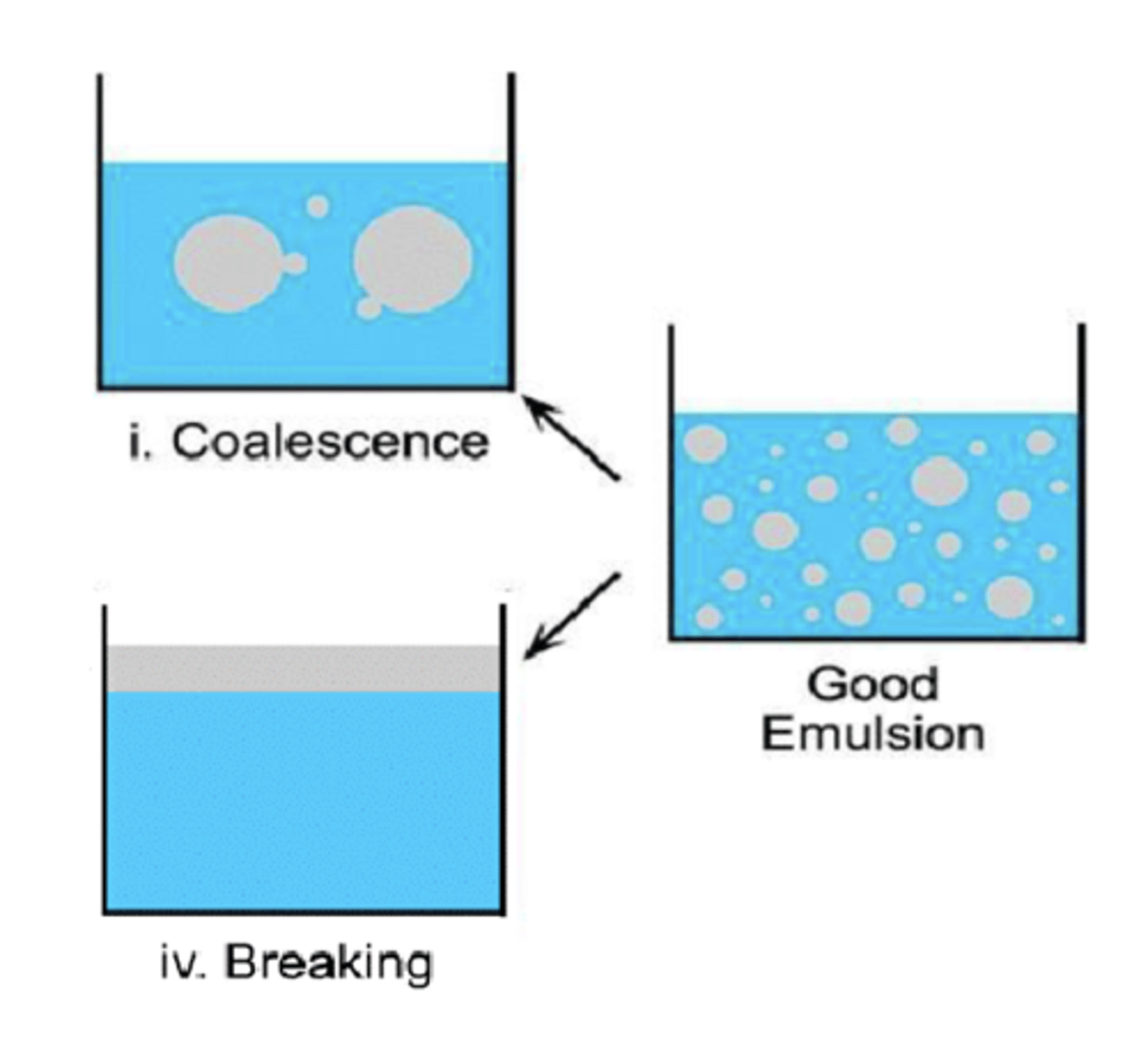
More collisions increase the risk of coalescence (droplets merging), which can lead to _______________ and _________________
phase separation and emulsion instability
Usually, the phase present in greater amount becomes the ___________ phase
external phase
Order of mixing
by altering the sequence of addition and the mixing conditions, it's possible to create either o/w emulsions or w/o emulsions
Flavorants
- substances added to provide flavor to the emulsion.
- can include natural or artificial flavors, herbs, spices, or other aromatic compounds
Flavorants are only used in what type of emulsions?
oral emulsions
Should a flavorant reside in the internal phase or external phase?
A. Internal phase
B. External phase
C. It depends on the drug
B. External phase
- strength of flavor in the internal phase will be reduced
What is the most important requirement from a well-formulated emulsion?
adequate physical stability
(otherwise, it will revert to 2 separate bulk phases)
What are major phenomena associated with physical instability? (3)
- creaming
- coalescence (= cracking = breaking)
- inversion
Emulsion instability: Creaming
- upward movement of dispersed droplets
- reversible; moderate amount of shaking will redisperse the droplets uniformly
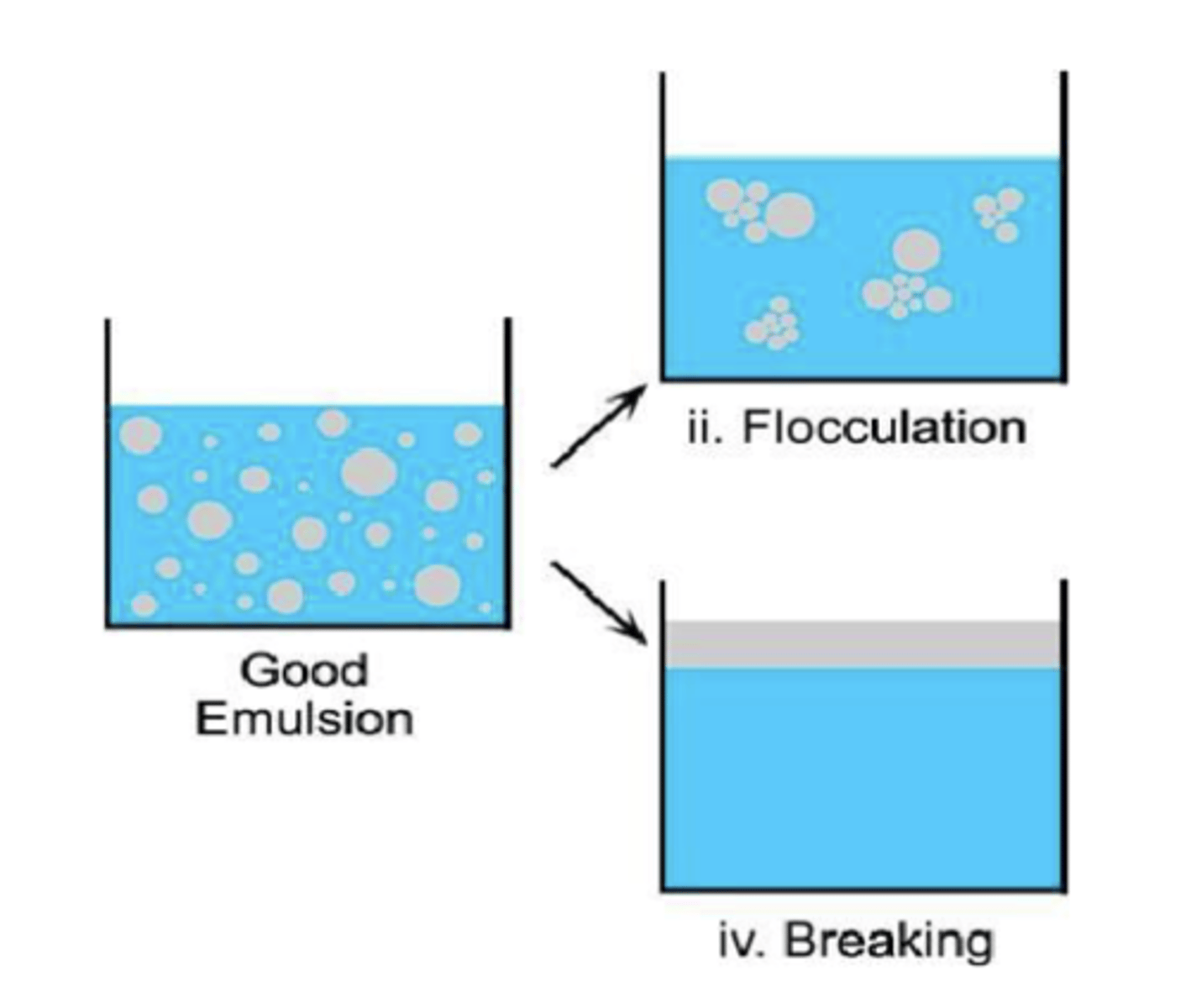
Why do oil droplets go up and not sediment?
due to density differences between the dispersed phase (oil) and the continuous phase (water)
What are problems with creaming? (3)
- not aesthetically acceptable
- poor content of uniformity
- may facilitate issue of coalescence
How can creaming be prevented?
Increasing the viscosity of the continuous phase by the use of thickening agents- most frequent approach
Emulsion instability: Coalescence
- complete fusion of droplets (film of EA surrounding droplets of internal phase is broken)
- decreased number of droplets and separation of the 2 immiscible phases
- irreversible
Reasons for coalescence
- bacterial growth
- adverse storage conditions (freezing: ice disrupts the interfacial film, elevated temperatures: increased motion of the EA results in a expanded film)
Emulsion instability: Phase inversion
emulsion inverting by changing from O/W to a W/O emulsion (or vice versa)
T/F: Wherever possible, the volume of the dispersed phase should not exceed 50% of the total volume of the emulsion
TRUE
Ointments
- homogenous, highly viscous semi-solid preparation
- oil-based (higher conc. of oil, 80%)
- greasy
- effective for dry or thickened skin
General uses of ointments (3)
1. Acts as protective/protectant - serve as physical barrier to environment
2. Acts as emollient - softens skin, makes it pliable
3. Carrier of medicament - vehicle
Creams (4)
- water-based, lower oil concentration
- lighter, less greasy than ointments
- easily absorbed
- good for moisturizing and treating mild skin conditions
How do ointments differ from creams?
ointment differs from a cream in that it has an oil base, as opposed to being water-soluble
Creams are solid emulsions containing...
suspensions or solutions of medicinal agents for external application
Examples of creams of the o/w type
foundation creams, hand creams, shaving creams, vanishing creams
Examples of creams of the w/o type
cold creams, emollient creams
Components of parenterals (4)
1. Active ingredient
2. Vehicle(s)
3. Excipients
4. Primary container & closure
Vehicles can be: (3)
- Aqueous (vehicle of greatest importance)
- Hydroalcoholic
- Oil
Aqueous vehicles (6)
1. Water for injection, USP
2. Sterile water for injection, USP
3. Bacteriostatic water for injection, USP
4. Sodium chloride injection, USP
5. Bacteriostatic sodium chloride injection, USP
6. Ringer's solution/Ringer's lactate solution
Water for injection, USP (6)
- how frequently used is it?
- what does it meet the same standards as?
- what kind of preparations is it used in?
- can it contain added substances?
- when is its intended use within?
- what must it be free of?
- most frequently used solvent in the large-scale manufacture of injections
- meets same standards for presence of solids as purified water USP (≤ 1 mg/100 mL)
- used in preparations that will be terminally sterilized during or after the manufacture process
- should not contain added substances
- intended used within 24 hours
- pyrogen free, tight containers
Sterile water for injection, USP (5)
- What should it not contain?
- What is it intended to be used as?
- What is it packaged in?
- sterile & pyrogen free
- should NOT contain antimicrobial agent
- intended to use as solvent, vehicle, or diluent
- packaged in single-dose containers (≤ 1 liter)
Bacteriostatic water for injection, USP (6)
- what does it contain?
- what kind of container is it supplied in?
- it is used as a sterile vehicle in the preparation of what?
- in what volume is the formulation only administered?
- sterile & pyrogen free
- contains one or more appropriate antimicrobial agents
- supplied in a multiple-dose container ≤ 30 mL
- prefilled syringe
- vial
- sterile vehicle in the preparation of small volumes of injectable preparations
- only used when the volume of formulation is ≤ 5 mL
What does the USP require on the label for bacteriostatic water for injection
"Not for use in newborns"
- benzyl alcohol exposure in newborns leads to gasping syndrome
- 11 ml/kg/day may be lethal
The container label for bacteriostatic water for injection must state the....
names and proportions of the agents or antimicrobial agents (antimicrobial agent should not interact with API)
Sodium chloride injection, USP (3)
- it is a sterile....
- does it have a bacteriostatic agent?
- it is a sterile vehicle in...
- sterile isotonic solution of sodium chloride in water for injection
- no bacteriostatic agent
- sterile vehicle in solutions or suspensions of drugs for parenteral administration
Bacteriostatic sodium chloride injection, USP (3)
- sterile isotonic solution of....
- what does it contain?
- Its 2 uses?
- sterile isotonic solution of 0.9% sodium chloride in water for injection
- contains one or more appropriate antimicrobial agents
- used as a vehicle and to flush a catheter or IV line to maintain patency
Ringer's Injection, USP, and Ringer's Lactate Solution, USP (7)
- What 3 salts does it consist of?
- it is considered...
- It is commonly used for...
- what is it sometimes used as?
- What is it extensively used in?
- it is a systemic ________ to treat ____________
- it replaces __________ and ___________ in patients with low _________ or low __________
- NaCl (860 mg), KCl (30 mg), and CaCl2 (33 mg) in 100 mL solution. Ringer's lactate solution contains sodium lactate in addition to 3 salts
- considered physiologically balanced (closely resembles body's extracellular fluid)
- commonly used for fluid resuscitation after blood loss
- sometimes used as a vehicle for other drugs
- extensively used in aggressive volume resuscitation
- a systemic alkalizer to treat metabolic acidosis
- replaces water and electrolyte loss in patients with low blood volume or low blood pressure
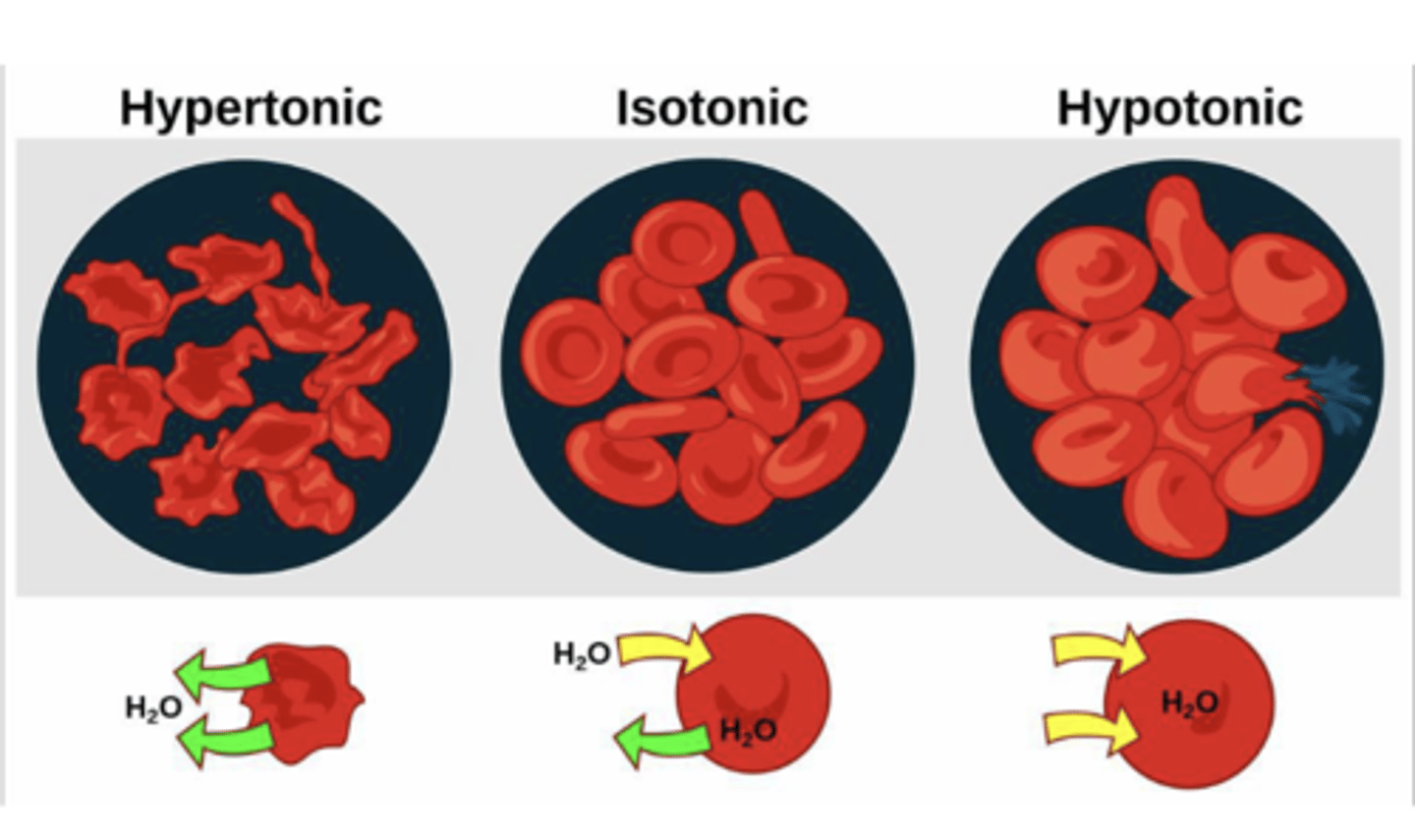
Tonicity agents
hypotonic or hypertonic will lead to hemolysis or crenation (shrinkage)
(ex: dextrose, sodium chloride, potassium chloride)
(hypertonic- high conc. of solute in body fluid , leads to shrinkage hypotonic- cells swell isotonic- osmotic pressure within cell and body fluid are similar)
Freeze-drying/lypophilization
- sublimation phenomenon
- vials are filled
- vials are placed in a lyophilizer
- freezing stage (~(-40) degrees C
- drying stage (secondary)
- removal of bound water/unfrozen water
- can be stored and shipped (proteins < 30 degrees C, small molecules, 40 degrees C)
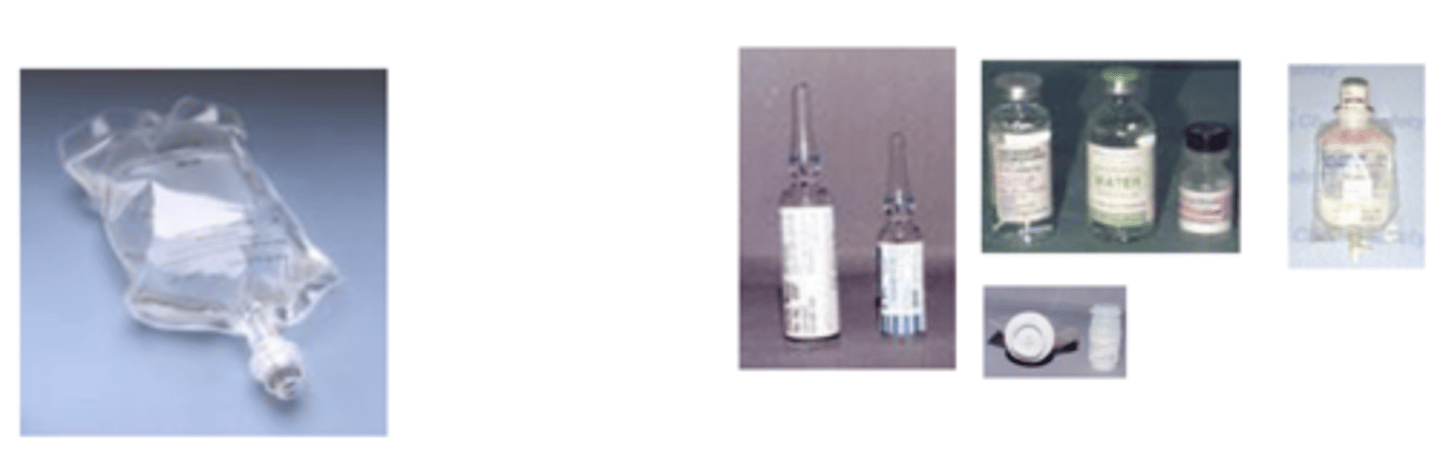
LVP vs. SVP solutions
LVP
- injections given in hospital
- >100 mL
- plastic bags & glass bottle
- electrolyte and fluid balance- parenteral nutrition, vehicles
SVP
- ≤ 100 mL
- primarily to deliver medications
- ampules, vials, and prefilled syringes
Roles of pharmacist in LVP solutions: What do complex preparations involve? (4)
• Accurate calculations
• Compounding
• Aseptic technique
• Familiarity with all aspects of parenteral combinations
Pulmonary dosage forms (3)
1. pressurized metered-dose inhalers (pMDIs)
2. dry powder inhalers (DPIs)
3. Nebulizers
Pressurized metered-dose inhalers (pMDIs) AKA metered-dose inhalers (6)
- multi-dose system that delivers a certain dose as an aerosol
- most common inhalation device
- simplest of all aerosols
- accurate metering of small doses of drug
- predetermined dose is released as a spray on actuation of metered valve
- drug is dissolved or suspended in liquid propellant(s)
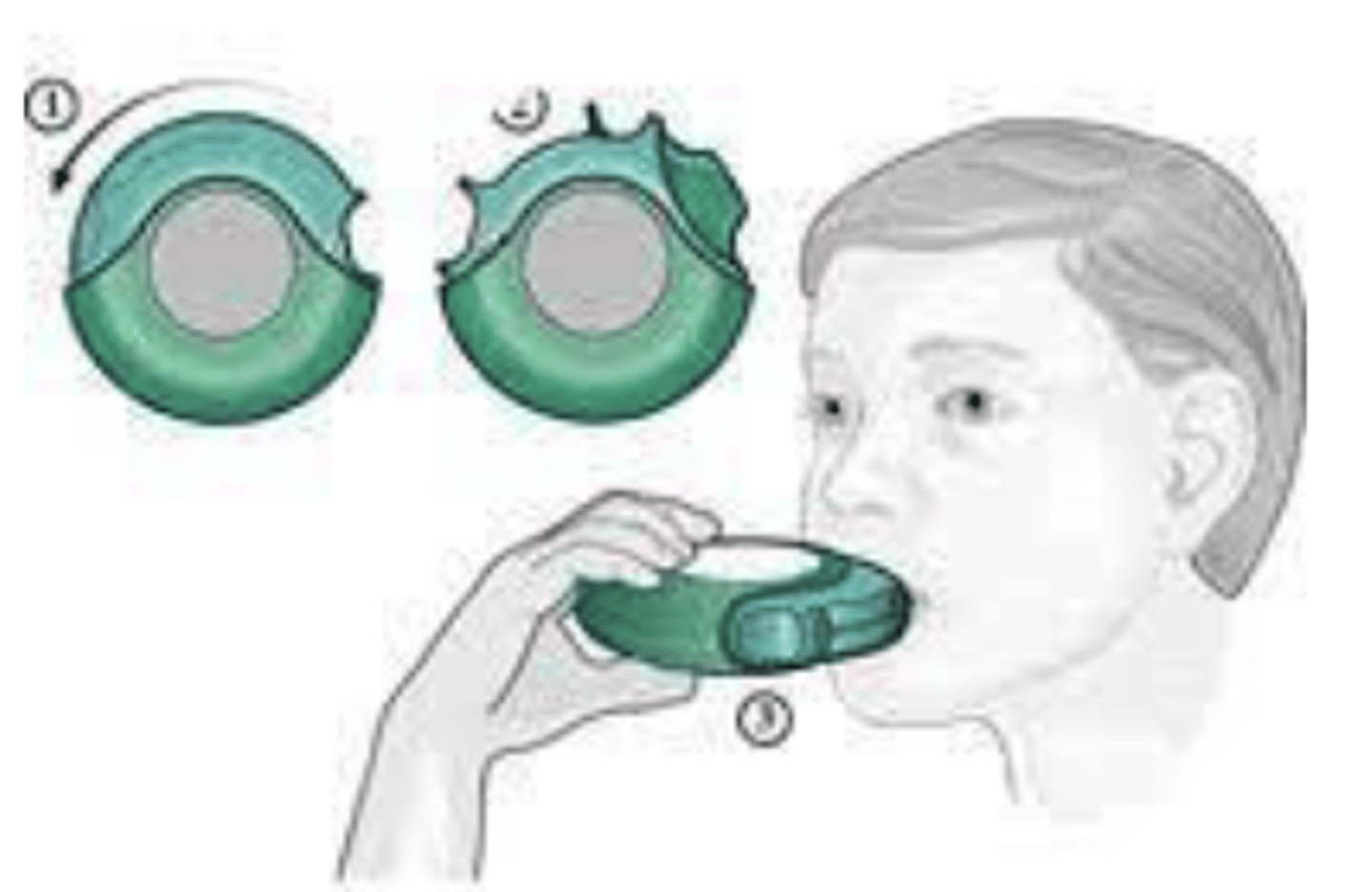
Dry powder inhalers (DPIs) (5)
- delivers drug as a ____________________
- inhaled as a ___________________________________
- passive or __________________
- what does it rely on?
- are propellants needed?
- delivers drug as a stream of powder
- inhaled as a cloud of fine particles
- passive or patient-driven
- relies on the patient's inspiratory effort to dispense the dose from device
- no propellants needed
Nebulizers
converts aqueous solutions (or suspensions) of a drug into an aerosol
- droplets of solution are inspired by the patient through a mouthpiece or facemask
Types of nebulizers****
• Jet
• Ultrasonic
• Vibrating-mesh
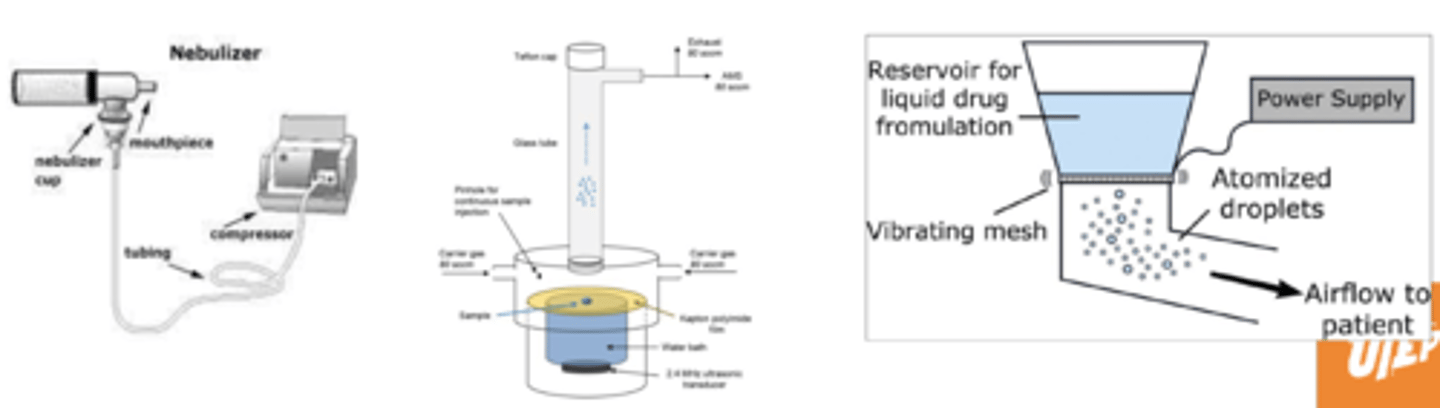
Jet
uses compressed gas to make an aerosol (tiny particles of medication in the air)
Ultrasonic
Produces aerosol at a constant rate regardless of the respiration cycle
Vibrating-mesh
Liquid passes through a very fine mesh to form the aerosol
Nasal dosage forms (4)
- drops
- sprays (squeezed bottles)
- metered dose sprays
- gels
Topical administration of the eye can treat....
diseases that affect the anterior segment of the ye
(conjunctivits, glaucoma)
Topical administration of the eye cannot provide the....
desired therapeutic concentration of the drug in the posterior segment of the eye
What is the average eye drop volume?
40 μL (25-70 μL)
Topical eye administration flow chart
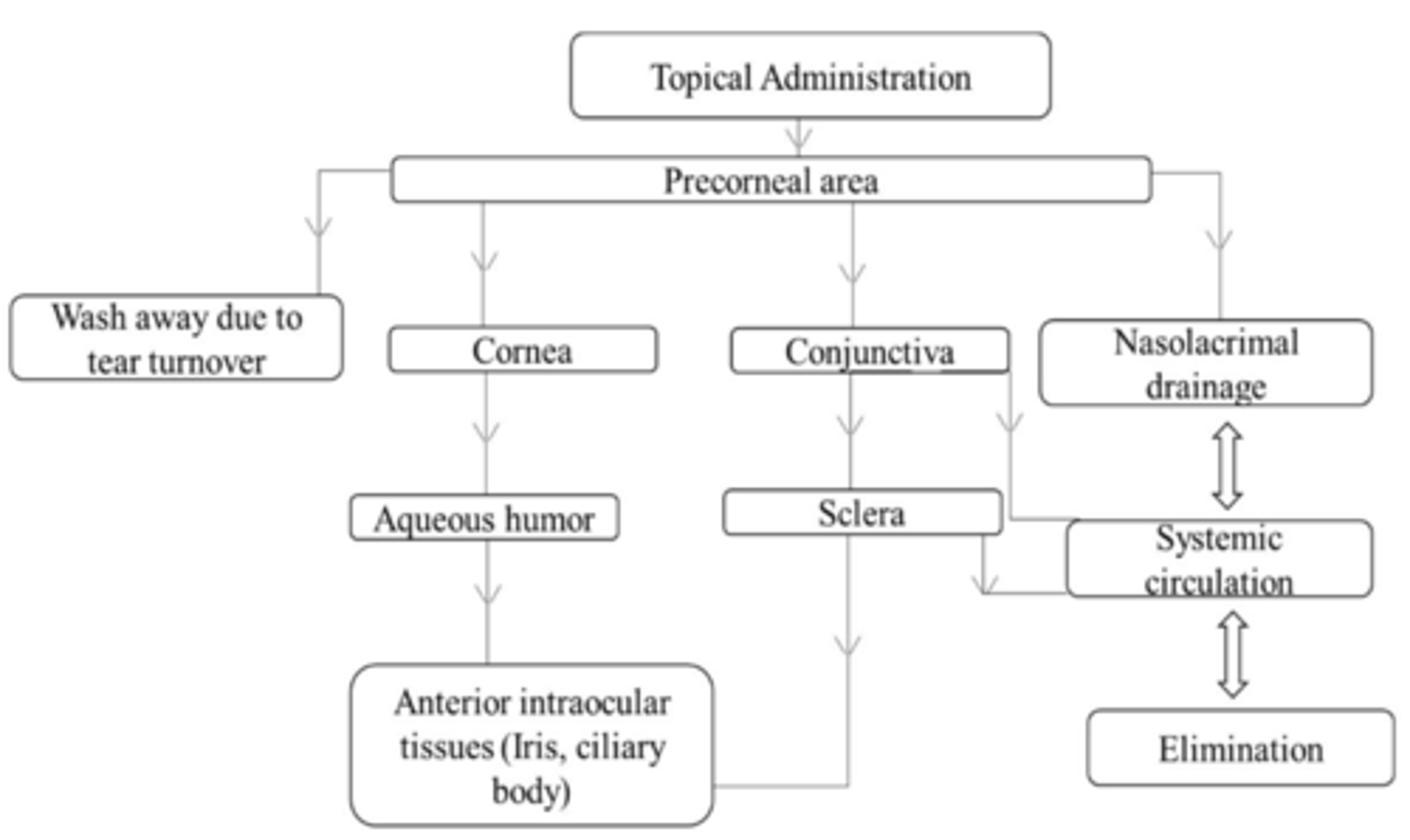
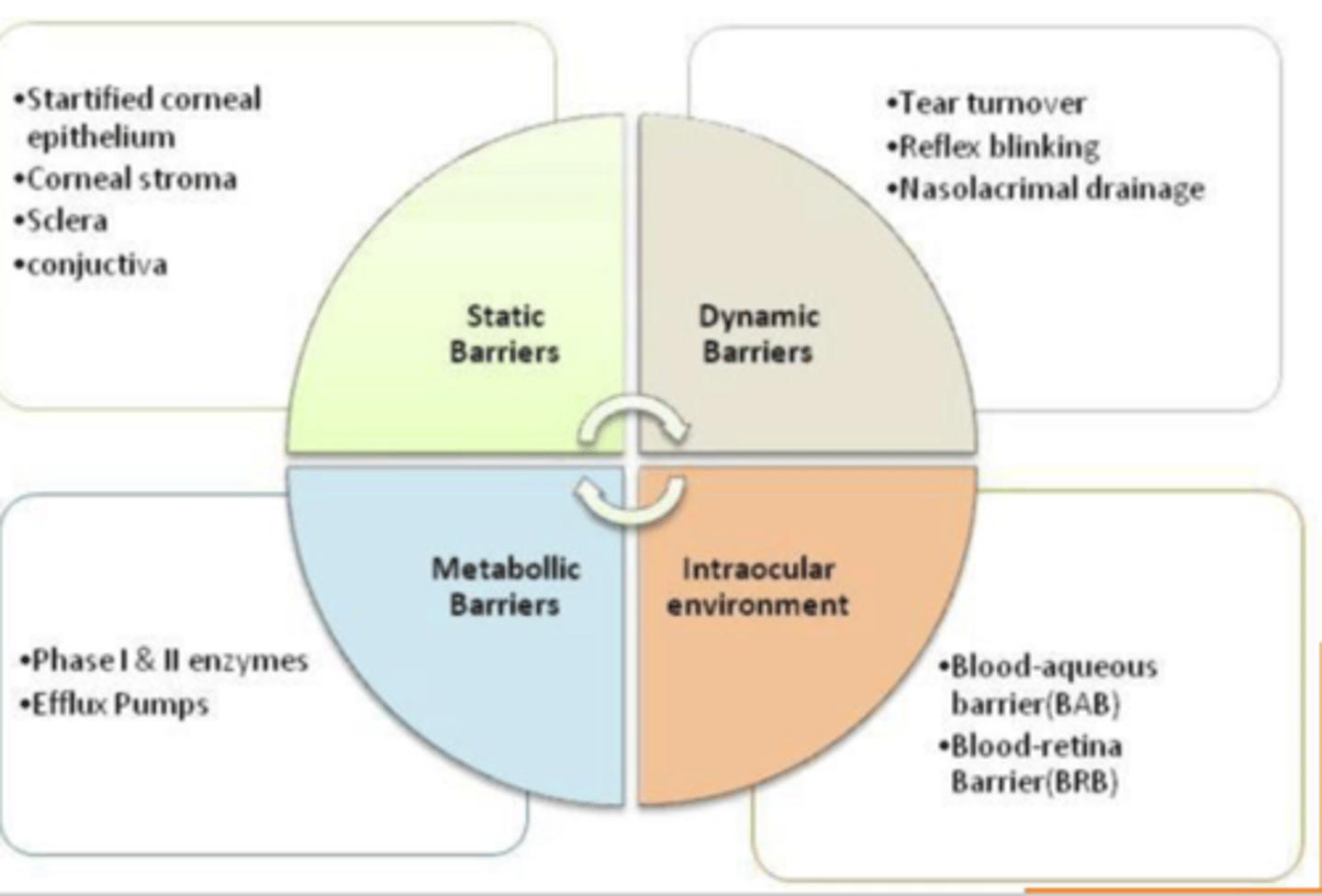
Static barriers to topical eye delivery***** (4)
- stratified corneal epithelium
- corneal stroma
- sclera
- conjunctiva
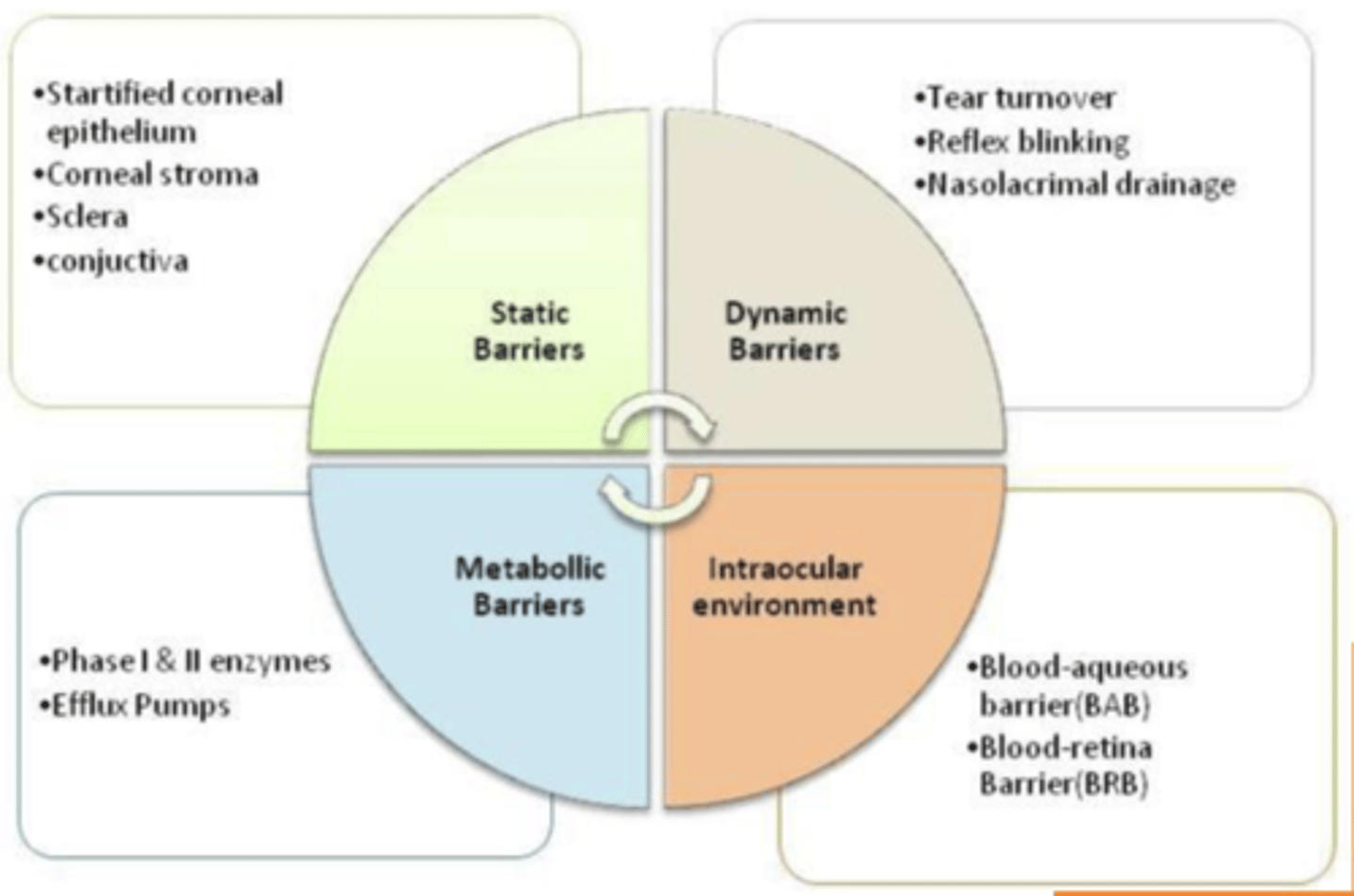
Dynamic barriers to topical eye delivery***** (3)
- tear turnover
- reflex blinking
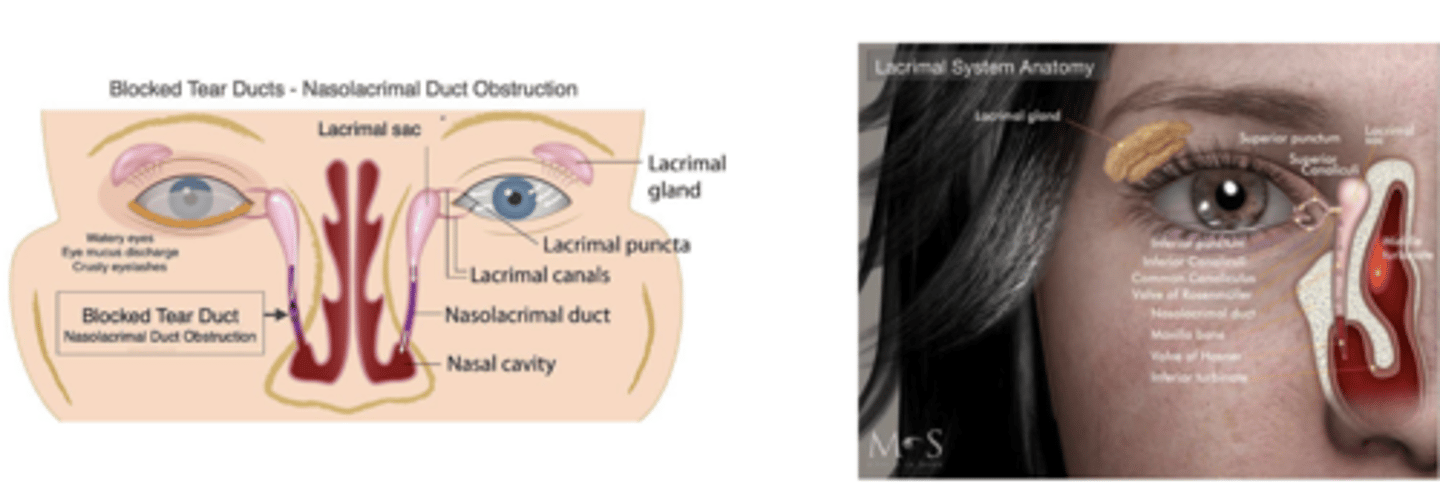
- nasolacrimal drainage
Metabolic barriers to topical eye delivery**** (2)
- Phase I & II enzymes
- efflux pumps
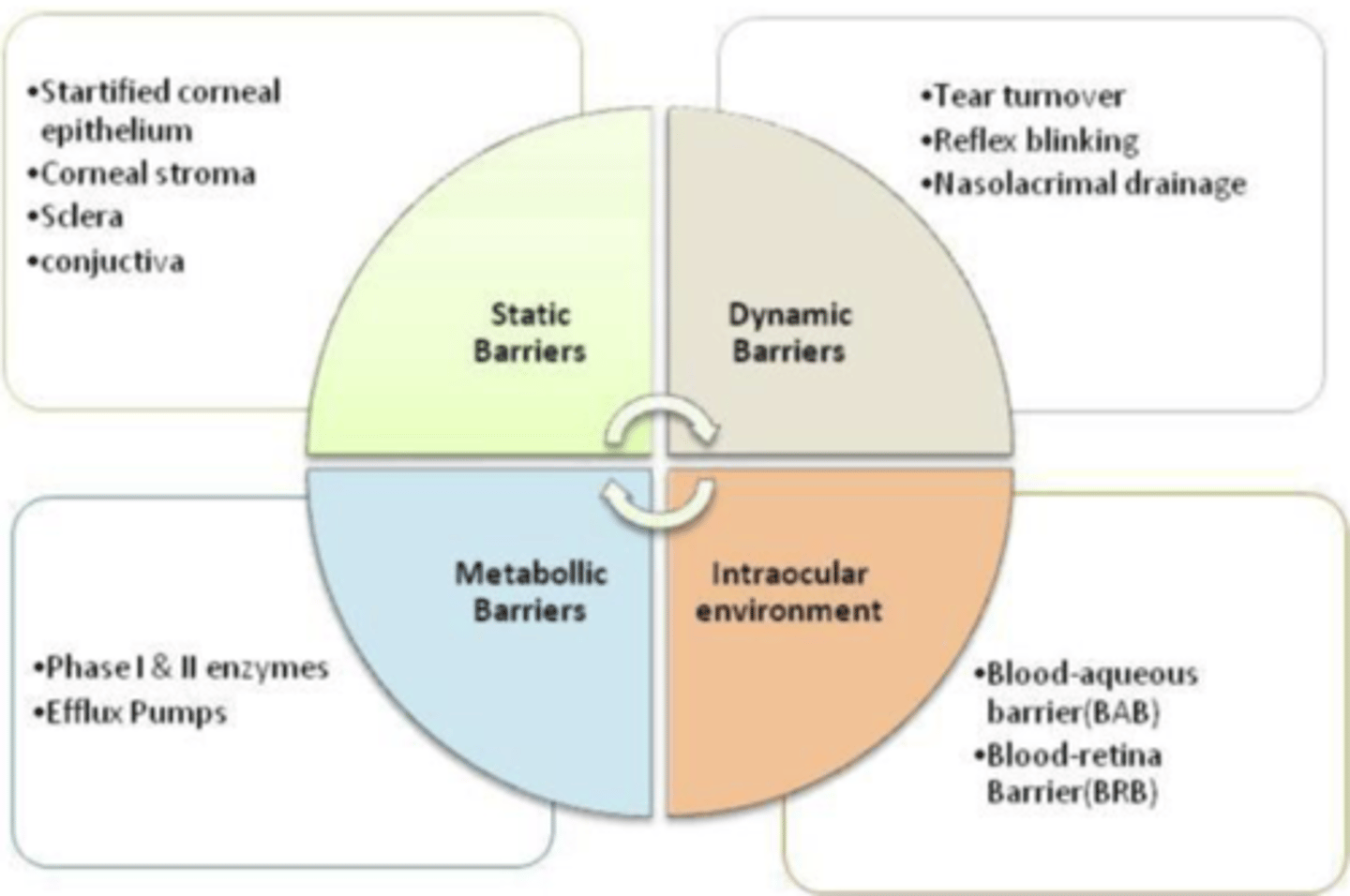
Intraocular environment
- blood-aqueous barrier (BAB)
- blood-retina barrier (BRB)
Drug losses in ocular delivery (4)
- immediate loss from spillage
- lacrimal drainage
- absorption through the conjunctiva
- corneal factors
Commercial eye dropper dispenses __________ of solution
25-70 μl
- overflow
When more than one drop is to be administered, how much time should elapse between administrations?
≥ 5 minutes
- Absorption time, Avoiding Overdose, Patient Comfort, Optimizing Therapeutic Levels
Lacrimal turnover rate is....
~1 ml/min
what accounts for loss of an ophthalmic dose in a relatively short time?
rapid washing and turnover
T/F: The conjunctive has substantial blood flow
TRUE
The drainage rate of the conjunctiva is proportional to the...
instilled drop volume
Can absorbed drug enter systemic circulation via the conjunctiva blood flow?
YES
What properties of drugs with the most effective penetration for ocular routes have?
both lipophilic and hydrophilic properties