Postural Control Development and Aging: Neuroscience, Milestones, and Fall Prevention
1/151
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
152 Terms
What are the initial positions in the development of postural control?
Supine, prone, prone on elbows, quadruped, tall kneeling, half kneeling, standing.
What sensory systems contribute to movement in postural control?
Somatosensory, Visual System, Auditory System, Vestibular System.
How does poor postural control affect distal skills in infants?
Poor postural control can mask more mature distal skills such as reaching, eye-head control, and leg movement.
What is the role of proximal stability in infant mobility?
If an infant lacks proximal stability, they will have impaired distal mobility; therefore, proximal stability must be provided for distal mobility to occur.
What is the relationship between postural, locomotor, and manipulative systems in development?
The simultaneous development of postural, locomotor, and manipulative systems is essential for the emergence and refinement of skills.
What are the motor milestones associated with emerging postural control?
Head control, sitting, creeping/crawling, pull to stand, independent stance, walking.
What functional skills require postural control?
Sitting, standing, walking unsupported, reaching forward, moving from sitting to standing.
How does the immature postural system affect behavior in infants?
An immature postural system is a limiting factor or constraint on the emergence of other behaviors such as coordinated arm and hand movements and inhibition of reflexes.
What is the significance of taking infants through the development sequence?
Taking infants through the development sequence helps improve gait.
What is the impact of postural control on coordinated movements?
Postural control is essential for the development of coordinated movements, as poor control can hinder the ability to perform tasks requiring coordination.
What is the role of physical therapists in relation to postural control?
Physical therapists contribute knowledge as movement specialists in areas of neuroscience related to postural control.
What is the effect of postural control on functional skills?
Postural control is crucial for performing functional skills such as sitting, standing, and walking.
Why is head stability important in postural development?
Head stability is important for maintaining balance and facilitating further motor development.
What does 'prone on elbows' help develop in infants?
'Prone on elbows' helps with extension and head stability.
How does postural control relate to the development of gait?
Proper postural control is necessary for the development of gait, as it supports the transition through various developmental stages.
What are the consequences of lacking proximal stability in infants?
Lacking proximal stability can lead to difficulties in achieving distal mobility and overall motor development.
How do sensory systems interact in the context of postural control?
Sensory systems such as somatosensory, visual, auditory, and vestibular work together to facilitate movement and maintain balance.
What is the importance of motor milestones in infant development?
Motor milestones indicate the progression of postural control and overall motor development in infants.
What is the relationship between postural control and reflex inhibition?
Effective postural control is necessary for the inhibition of reflexes, allowing for more coordinated movements.
What is the significance of the sequence of motor behaviors in development?
The predictable sequence of motor behaviors reflects the developmental progression of postural control and related skills.
What is the Reflex/Hierarchical Theory of postural control development?
It posits that the emergence of posture and movement control depends on the appearance and subsequent integration of reflexes, with their appearance and disappearance reflecting the increasing maturity of cortical structures.
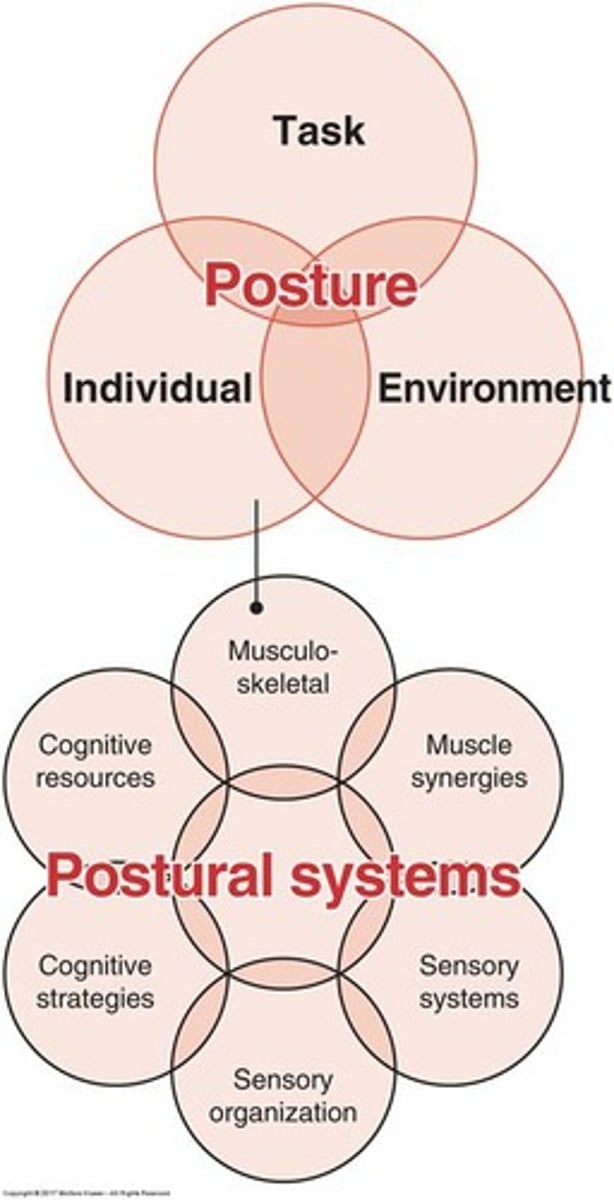
What does the Systems Theory of postural control emphasize?
It emphasizes the complex interaction between neural and musculoskeletal systems, including changes in the musculoskeletal system, development of motor coordination strategies, individual sensory systems, sensory strategies for organizing, and cognitive resources.
At what age do infants begin to show directionally specific postural responses in neck muscles?
As young as 1 month of age.
What role does vision play in the development of postural control?
Vision is important in calibrating vestibular and proprioceptive systems and is critical for calibrating somatosensory inputs for head posture control.
When does the emergence of independent sitting typically occur in infants?
Between 6 to 8 months of age.
What are the stages of control an infant goes through when learning to sit independently?
1. No control; 2. Attempts to initiate upright sitting; 3. Partial control with a large range of body sway; 4. Functional control with minimal sway.
What is reactive balance control and when does it become available in infants?
Reactive balance control in the trunk is available to a limited extent in infants before they develop independent sitting.
How does trunk control improve in infants learning to sit?
Trunk control improves and is associated with improved reach trajectories.
What is the relationship between reactive balance control and anticipatory control in newly sitting infants?
Reactive balance control emerges prior to anticipatory control.
What happens to an infant's reliance on visual inputs when controlling sway as they gain experience in independent sitting?
Dependence on visual inputs decreases with increasing experience in independent sitting.
What must infants learn to do to transition to independent stance?
They must learn to balance within reduced stability limits, control additional degrees of freedom, and recalibrate sensorimotor representations for postural control.
What are the two strategies infants explore to control postural sway when learning to stand and walk?
The specific strategies are not provided in the notes, but they involve balancing and controlling sway.
What is exploratory postural sway used for?
To investigate and explore the sensorimotor workspace for posture control.
What is performatory postural sway?
It uses sensory information to control posture.
What occurs before the emergence of independent stance in infants?
The ability to support weight against the force of gravity in a standing position.
Which sensory system elicits organized postural responses in standing infants at an earlier age?
The visual system.
What adaptive ability regarding balance is not mastered by infants during their first year of walking?
The ability to use hips in balance.
How long do hip-dominated responses last in walkers with limited experience?
They are present in walkers with only 3 to 6 months of walking experience.
What challenges do children face in postural control due to their body structure?
Children are shorter and top-heavy, making balance more difficult.
At what level is the center of mass (COM) located in a child?
Approximately at T12.
How do compensatory postural responses of young children compare to those of adults?
They are more variable and slower.
At what age do postural responses in children become similar to those of adults?
By 7 to 10 years of age.
What components do skilled movements consist of?
Both postural and voluntary components.
What is the role of the postural component in skilled movements?
It establishes a stabilizing framework that supports the primary movement.
How is postural control defined?
The ability to adapt sensory information about position and movement of the body in space to changing task and environmental conditions.
What cognitive resources are required for postural control?
Attentional resources.
How does task complexity affect postural control?
Additional attentional resources are required with increasing postural task complexity.
What effect do postural demands have on younger children's performance?
They tax their attentional resources, affecting both postural and cognitive performance in dual-task situations.
What changes occur in motor components as children develop postural control?
Changes in body morphology and refinement of muscular response synergies.
What refinements occur in postural motor behavior as children grow?
Decrease in sway velocity and reduction of oscillatory sway behavior.
What shift occurs in the sensory aspects of postural control by age three?
A shift from predominance of visual control of balance to somatosensory control.
How does the automaticity of postural control change with age?
It increases, requiring less attentional resources.
What are the objectives of the 604BG Clinical Neuroscience II course?
Discuss the development of balance and postural control, areas of neuroscience relevant to physical therapists, postnatal development of the nervous system, factors contributing to aging, and age-related changes in systems important to postural control.
What factors contribute to aging according to the notes?
External factors (lifestyle and environment) and internal factors (genetic factors, health-related behaviors, efficiency of DNA repair).
What percentage of longevity is attributed to genetic factors and health-related behaviors?
Genetic factors contribute to 20% of longevity, while health-related behaviors contribute to 80%.
What lifestyle factors can influence aging?
Lifestyle, diet, levels of exercise, stress, and self-efficacy.
What is the significance of psychosocial factors in aging?
Psychosocial factors play a significant role in aging and can influence health outcomes.
What does the term 'heterogeneity of aging' refer to?
It refers to the variability in physical capabilities among older adults and the importance of not assuming decline in all.
What is the continuum of physical function among older adults?
A classification system that categorizes older adults based on age and skill performance, developed by Spriduso et al.
What are IADLs and BADLs?
IADLs (Instrumental Activities of Daily Living) involve managing oneself financially and other tasks for independence; BADLs (Basic Activities of Daily Living) include bathing and taking care of physical needs.
How is a fall defined clinically for older adults?
A fall is defined as an older adult falling to the ground or being found lying on the ground, or unintended contact with a supporting surface resulting in injury.
What is the research definition of a fall?
The inability to recover stability, requiring assistance to prevent a fall, which can come from another person or a harness.
What is the clinical significance of falls in older adults?
Falls can lead to serious injuries and are a major concern in the rehabilitation of older adults.
What age-related changes occur in the systems important to postural control?
Changes occur in both the musculoskeletal and neural systems.
What is the impact of aging on functional capabilities?
Aging does not necessarily correlate with a decline in function; individual capabilities can vary significantly.
What is the importance of self-efficacy in relation to aging?
Self-efficacy can influence health-related behaviors and overall longevity.
What are the implications of the continuum of physical function for researchers?
It assists researchers in categorizing older adults not just by age but also by their performance abilities.
What does the term 'postural control' encompass?
It encompasses the capacity of an individual, the demands of a task, and the strategies used to accomplish tasks in different environments.
What is the significance of understanding alterations in postural control?
Understanding alterations helps in the rehabilitation of older adults and in addressing balance issues.
How does aging affect the efficiency of DNA repair?
Aging can lead to decreased efficiency of DNA repair, contributing to various health issues.
What is the role of lifestyle in longevity?
Lifestyle choices significantly influence longevity and can be modified to improve health outcomes.
What does the literature suggest about classifying older adults?
There is difficulty in reading literature regarding how subjects are classified as older or elderly, indicating a need for clearer criteria.
What is the relationship between aging and functional decline?
Not all older adults experience functional decline; many maintain their physical capabilities.
What are the leading causes of death in the elderly related to unintentional injuries?
Unintentional injuries, including cardiovascular disease, cancer, cerebrovascular accidents (CVA), and pulmonary disorders, are the 5th leading cause of death in the elderly, with falls accounting for 2/3 of these deaths.
What are intrinsic factors that contribute to fall risk in the elderly?
Intrinsic factors include muscle weakness, history of falls, gait and/or balance deficits, use of assistive devices, visual deficits, arthritis, impaired activities of daily living (ADLs), depression, cognitive impairment, and age greater than 80 years.
What are extrinsic factors that contribute to fall risk in the elderly?
Extrinsic factors relate to the environment, such as presence of stairs, throw rugs, slippery surfaces, and poor lighting.
When is the fall risk highest for elderly patients post-hospital discharge?
The fall risk is at its highest 1-6 months post-discharge from the hospital.
How does muscle strength change with age?
Muscle strength declines with age, with lower extremity manual muscle testing (MMT) potentially declining as much as 40% between ages 30-80.
What is the impact of falls on knee and ankle strength in skilled nursing facility residents?
In skilled nursing facility residents with a history of falls, knee strength can be reduced by 2 times and ankle strength by 4 times compared to residents without a history of falls.
What happens to muscle endurance as people age?
Muscle endurance decreases with age, leading to a loss of Type I and II muscle fiber types, decline in motor units, and changes at the neuromuscular junction.
What are the clinical implications of age-related changes in postural control?
Clinicians should evaluate primary neuromuscular and secondary musculoskeletal contributions to instability, including sensory evaluation, manual muscle testing, range of motion (ROM), and balance assessment.
What age-related changes occur in the skeletal system affecting postural control?
There is a decrease in range of motion (ROM) and loss of spinal flexibility, particularly in extension, leading to an increased forward posture in older adults.
How does the center of mass change in older adults?
The center of mass shifts forward in older adults due to age-related changes in the musculoskeletal system.
What is the effect of aging on ankle joint flexibility?
Older adults experience a loss of ankle joint flexibility.
What changes occur in steady-state balance as people age?
There is an increase in sway noted with an increase in age.
What test can clinicians use to assess steady-state balance?
The Rhomberg Test can be used to assess sway, and clinicians can also observe sway while the patient sits at the edge of the bed.
What factors should clinicians assess to evaluate balance in elderly patients?
Clinicians should assess sensory function, manual muscle strength, range of motion, and inquire about living conditions.
What are the implications of decreased muscle force production in older adults?
Decreased muscle force production leads to faster fatigue and slower rates of tension development.
What happens to the functional capacity of muscles as people age?
Changes in skeletal muscle affect functional capacity, resulting in a decrease in maximum isometric force and increased fatigue.
What is the significance of evaluating living conditions in elderly patients?
Understanding living conditions helps identify environmental fall risk factors that may contribute to instability and falls.
What are the primary systems involved in postural control that decline with age?
The primary systems involved in postural control include the motor systems and musculoskeletal systems.
How do age-related changes affect reactive and proactive balance control?
Aging affects the ability to maintain steady-state posture, reactive balance control, and proactive balance control.
What is the relationship between cognitive impairment and fall risk in the elderly?
Cognitive impairment is an intrinsic risk factor that can increase the likelihood of falls in the elderly.
What role does depression play in fall risk among elderly individuals?
Depression is an intrinsic factor that can contribute to increased fall risk in elderly individuals.
Why is it important for clinicians to assess both neuromuscular and musculoskeletal factors in elderly patients?
Assessing both factors is crucial for understanding the comprehensive causes of instability and developing effective interventions.
What is the significance of assessing spontaneous sway during quiet stance?
It serves as an indicator of balance control.
What are the Romberg and Sharpened Romberg tests used for?
To assess balance, particularly in individuals with neurological diseases.
What is a notable limitation of the Romberg test?
It may not be the best assessment for individuals with neurological diseases.
How do age-related changes affect functional stability limits?
Functional stability limits are reduced with age.
What is the purpose of the 'Sit and Reach' and 'Stand and Reach' tests?
To assess flexibility and balance in older adults.