KINESIOLOGY 484 - Exam 2
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
118 Terms
The Components of Balance
Vestibular System
Vision
Somatosensory
Vestibular System
Semicircular Canals
3 Planes of Movement
Detects change in motion
Acceleration
Deceleration
Vision
Orientation to horizon
Somatosensory
Proprioception…
Joint mechanoreceptors (ligaments, jt. capsule)
Musculotendinous: Muscles spindles, GTOs
Kinesthesia…
Tactile/touch perception of skin mechanoreceptors
Pressure, vibration, stretch
Balance
A complex feedback loop to create the ability to adapt to the ever-changing enviornment
Common Measurements of Balance
Postural Sway
Horizontal movement of the center of gravity when a person is standing still
Functional Movement Tests
Dual task challenges: adding cognitive
Prognosis with Vision Impairment
Lower level of self-efficacy
Lower level of social connection
Less overall physical activity
Vision Impairment
Even mild vision impairment increases mortality risk in adults 40+ years old
Vision loss causes…
Apprehension (scared) of Environment
Vision Maladaptations…
Poor static & dynamic balance
Forward head posture
Slower gait, wider stance
Results of Vision from Exercise
Improves balance skills, spatial orientation, and gait efficiency
Decreases chronic disease
Improved socialization abilities
Improvement in independence, confidence & self-image
Almost all individuals with visual impairment have…
Residual vision
Legal Blindness
Vision of 20/200 or less with the best correction
Blind by visual field
Less than 10 ft. of central vision or having tunnel vision
Visual field disturbances…
Halos
Ghosting
Glare
Visual Snow
Visual Impairment Effective Program Design
GOAL: Create a program that will strengthen self-efficacy, as well as physiological adaptations
SAFETY
Plan for Cues is Essential: Give environmental, verbal, and exercise instruction cues
Visual Impairment Special Considerations
Have safety precautions for balance
Environmental cues: Use good contrasting colors with equipment
Pair with a partner of similar skill level for higher demand activities (ex. special soccer team where all individuals have a sort of vision impairment)
ACSM rules for bodily safety: Extra clearance is needed for high-impact activities
Create a predictable facility environment: Give a tour of the facility then keep the facility layout consistent every time
Wandering happens and is a safety risk: use a constant sound source so they can always have an understanding of where they are
Verbal Cues and Exercise Directions: Consistent, simple, direct verbal cues established prior to exercise (do not correct every movement or self-efficacy will weaken)
Manual Guidance: Describe where and how you intend to touch individual, be gentle
Braille-Me Method (Vision Impairment)
Demonstrate an action first, while the participant feels your movements
Hands-on Method (Visual Impairment)
Guide the participant through an action by grasping the most beneficial body areas (wrists, shoulder, etc.) then moving them through the desired movements
Hearing Loss…
Umbrella term that applies to people who are hard of hearing or deaf
Hard of Hearing…
Mild to severe level of loss
Some range of useful hearing and intentional use for the purpose of communication
Usually has assistance of auditory device
Deaf…
Severe to profound level of hearing loss
Unable to use residual hearing for processing information or communication
May or may not use sign language as a primary mode of communication
Not viewed as a disability/limitation
Distinct cultural community
Sensorineural Hearing also commonly has…
Commonly also have vestibular disorder (issues with semicircular canals)
Most common risk factor for hearing loss
Aging and excessive noise
4 Types of hearing loss
Conductive
Sensorineural
Mixed
Central
Conductive Hearing Loss…
Sound cannot effectively pass through the outer or middle ear
Preventing proper transfer of vibration
Sensorineural Hearing Loss…
The inner ear structures and associated nerves have deteriorated
MOST COMMON type of hearing loss
Region where sensory receptors (stereocilia) convert sound vibration waves to neural signals transmitted to brain for interpretation
Mixed Hearing Loss…
Combined conductive and sensorineural
Common with aging
Central Hearing Loss…
Central nervous system damage
NOT COMMON
Hearing aids do not…
Correct or restore hearing
They provide amplification so the person can make most of their abilities
Sound Amplifiers, Auditory Cue Converters
Can help combat background noise, echos
Visual light alarms
Tactile clocks
Cochlear Implants
Directly stimulates auditory nerve
Could possibly restore some useable hearing
Special Considerations for Hearing Loss…
Be aware of balance and spatial awareness with sensorineural hearing loss
Content of message must be recieved
Make sure there is not misinterpretation
Concise, Consistent Cues
How to train with someone with hearing loss?
Plan together on what communication strategies work best for them
Generally no altered responses to exercise
How to communicate effectively with an individual with hearing loss?
USE: Preferred method of communication AND prepare before an exercise session
FACE: Square up to the person to utilize as much non-verbal AND visual communication as possible, avoid focusing on the interpreter
LIP READING: Nothing should hinder the view of your mouth
VOLUME: Do not try to talk louder, it makes it harder to read lips
Make sure there is no misinterpretation (SC Hearing Loss)
Individuals with hearing loss are often visual learners
Demonstrations are essential
Be careful of sarcasm and non-verbal communication
If the individuals speech is hard to understand, ask for clarification
Concise, Consistent Cues (SC Hearing Loss)
Facial, body language, gestures
Have them choose how to get their attention in the gym during activity
Correctional cues: Make together based upon their communication preference
What to avoid with hearing loss individuals?
Avoid loud, constant, background noise
Always use sound for a purpose (ex. sound vibration)
Avoid “visual noise”
AKA a busy environment, they will focus on what is moving around them
Make sure they remove their assisted hearing device if they are doing contact sports
Tympanic Membrane Tubes
Prevent water entry into the ear canal with ear plugs
Communication in a busy gym… How do you keep them focused on you?
Have them face a wall if possible so that the visual noise is behind them and they can focus on you if you need to communicate something quickly
Nevermind rule
Never say “nevermind” to your patient because it lowers their self-efficacy
Multiple Sclerosis is…
Inflammatory neuromuscular disease that damages the myelin sheath of the Central Nervous System
“Immune-Mediated”
MS Facts…
Average age of diagnosis is 30 years
2/3 more common in women than men
Severity and progression is unpredictable from very aggressive to mild
Risk Factors for MS…
Genetics (not considered a hereditary disease)
Environmental Factors (more common in those living farther from the equator)
Lifestyle (smoking, high BMI)
Infectious Disease (linked with mono)
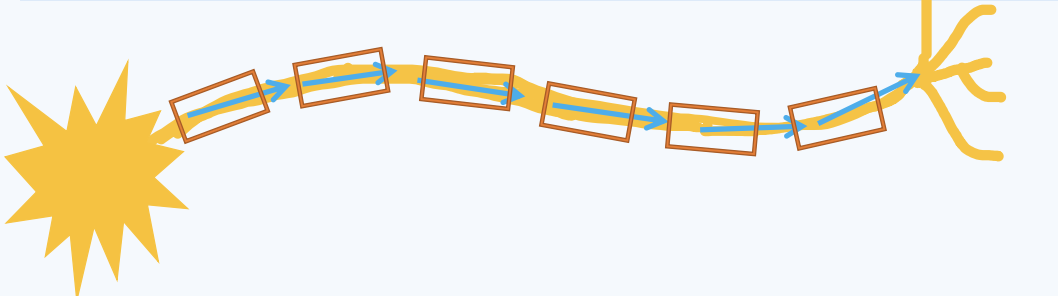
MS Physiology is a…
Disease of communication leak
What is Insulation? (MS)
Insulation is the material that resists electrical signal flowing through itself
What is the function of insulation? (MS)
It enhances the ability of the electrical signal to stay within the conductive wires and efficiently travel down the wire path
It keeps signals separate within individual wires that are close to each other
What do nerves send electrical signals for?…
Communication
Myelin is…
An insulating sheath surrounding the nerve axon
Increases both the velocity and strength of electrical signal traveling down the length of the axon
Velocity is…
The speed of electrical impulse (MORE communication sent)
How MUCH message is sent to the muscles
Repeating message = more force
Strength is…
Amplitude of message (EFFECTIVE message sent)
Complex Movement is…
The precise ability to immeasurable vary these two properties of communication
Slower Signals =
Less strength in communication of message
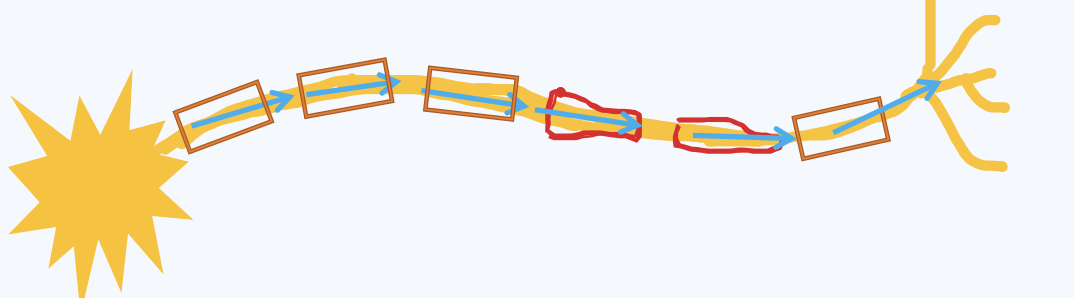
Oligodendrocytes
Cells that create and maintain myelin the the CNS only!
What are the 2 structures attacked and destroyed by inflammation in MS?
Oligodendrocytes and myelin
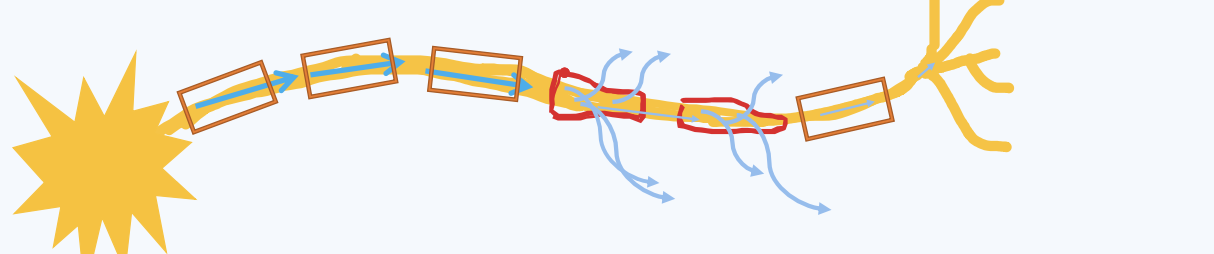
What are the 2 unique symptoms found in MS?
Uhthoff’s phenomenon
Lhermitte’s sign
Uhthoffs Phenomenon is…
An increase in neurological symptoms with elevated body temperatures
Healthy Electrical Signals…
The electrical signal travels down the axon and myelin insulates the axon to keep the electrical signal travelling down the axon path
MS Electrical Signals…
Myelin has been damaged, but often some are still present. In some places, thin myelin will be enough to insulate an electrical signal at normal body temperature
MS Electrical Signals (at elevated core temperature)…
Electricity travels faster/easier at higher temperatures, therefore it needs more insulation, but the damaged myelin insulation is insufficient to keep electrical signals going down the axon
Therefore less signal reaches dendrites to send the impulse to the next neuron = A weaker, slower, signal and more symptoms like weakness, fatigue, and less coordination (Uhthoffs phenomenon)
Why is it called Multiple Sclerosis?
- More than one area that has the scaring of myelin
- Random per person
- Multiple different symptoms due to many different areas affected
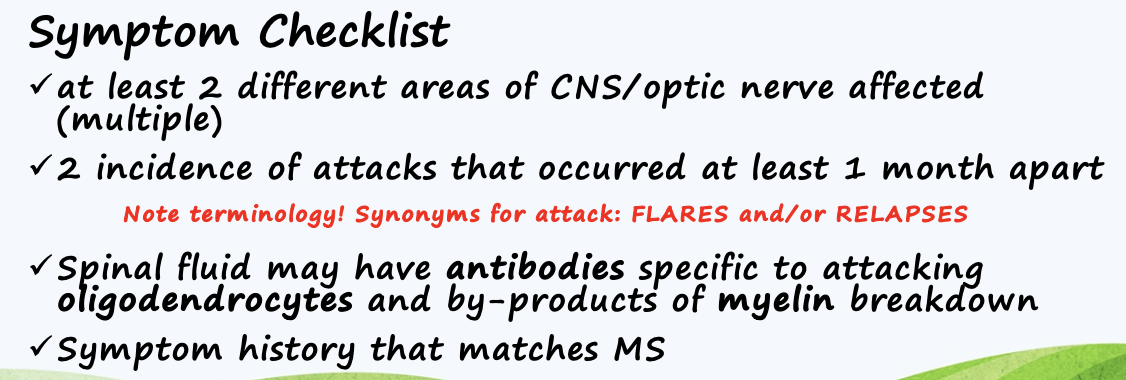
What qualifies individuals for MS?
Having more than one legion within the entire CNS
Have to have a full body MRI every 6 months to see if you have more legions
2 incidences of attacks that occurred at least 1 month apart
Spinal fluid may have antibodies specific to attacking oligodendrocytes and by-products of myelin breakdown
Symptom history that matches MS
Synonyms for “attack” (MS)
Flares and/or Relapses
Areas of Symptomology (MS)
VERY individualized, which leads to the difficult nature of the diagnosis
People with the diagnosis can present with very different symptoms
Why are there so many different ways that MS can manifest as symptoms for an individual?
Because MS can happen at multiple different locations in the CNS, therefore it depends on the location to determine symptoms. It also depends on the severity of the condition, ranging from mild to severe, some individuals may not experience symptoms and some may be very affected by them.
(Broad) Signs and Symptoms of MS
The most commonly reported symptom is FATIGUE
Pain/Perception…
Neuropathy
Visual changes
Heat/cold insensitivity
Bladder and bowel difficulties
Movement
Muscle weakness
SPASTICITY: Increased excitability in muscles due to CNS damage
ATAXIA: Lack of muscle control during voluntary movements
Balance issues, vertigo/dizziness
Intellectual
Cognitive impairment
Emotional imbalances
Why does MS happen?
Starts with a dysfunction of the inflammatory/immune system
Lhermitte’s Sign is…
Electrical sensation down the back or limbs when bending the neck
Commonly located right on the brainstem
Only an issue with neck flexion
Lesions are hyperexcitable, stretching them triggers an electrical impulse
How to avoid Lhermittes Sign? (MS)
Avoid having individuals do exercises resulting in neck flexion
How to resolve Lhermitte’s if it occurs
You do not have to completely cease exercise, try a different position where they do not have to do neck flexion
How is MS diagnosed?
Through the process of elimination
Rule out everything else that might be the cause, the evaluate if symptoms match the checklist
The most common type of MS is…
Relapsing-Remitting: Unpredictable flares which may or may not leave permanent deficits followed by periods of remission. Decline is not constant
What are the other types of MS?
Progressive Relapsing
Primary Progressive
Secondary Progressive
All of these conditions continue to get worse no matter the treatment
What to do during Flares? (MS)
Do not exercise
Use steroid-anti inflammatories to completely eliminate inflammatory response
The older the age of initial onset…
The faster the rate of decline
The older you are when you get diagnosed, the faster the rate of decline (ages 50+)
MS is considered a….
Chronic disease that affects daily life
75% of individuals are still capable of walking 15 years after diagnosis
Not a mortality disease, individuals often die of another chronic disease rather than MS
Effects of Exercise on MS
Exercise has no direct influence on prognosis or progression of the disease
There is no proof that exercise can change the course of MS
However, exercise significantly increases quality of life and improves aspects of fitness/functional movement
Expected Body Response to Exercise (MS)
80-90% age-predicted peak VO2 during exercise
Caused by lower extremity weakness and ANS dysfunction
Fatigue will hit quickly and when it does, they should stop!!
Common Maladaptations that influence gait (MS)
Balance challenges
Gait Ataxia = Lack of coordination with gait movement
Spasticity = Changes ability for ROM and ability to fire muscles in smooth manner
Muscle weakness causing foot drop (anterior tibialis very weak)
Maladaptations Result in… (MS)
Slower gait speeds
Imbalanced movements that lack efficiency
Shorter stride length
Wide base of support
Arms outstretched “tight roping”
What kind of exercises would you do to help improve MS?
Single-leg star excursion
Reverse and forward lunges
Single leg balance
Parkinson’s Disease is…
A chronic, progressive neurological disorder involving the division of the nervous system that primarily regulates coordinated muscle action
Epidemiology of Parkinson’s…
Men are about twice as likely to develop the disease than women
2nd most common neurodegenerative disease
Usually in individuals over 60 years
Etiology (causes) of Parkinson’s
It is idiopathic
Genetics (15-25%link)
Head trauma
Autoimmune
Environmental toxins (pesticides)
Higher rates with certain professions
Substantia Nigra…
Coordinates the motor control messages between the brain and spinal cord
Substantia Nigra is a….
Relay center
Afferent and Efferent messages pass through
Parkinson’s is also known as….
Disease of the regulator of the brain
Dopamine!
Neurotransmitter of the brain responsible for coordination and focus
What is the primary neurotransmitter used in substantia nigra? (PD)
DOPAMINE
You lose dopamine losing the ability to send messages= communication problem
Once diagnosed with Parkinson’s what is the first change the doctor perscribes?
A change in diet, a Mediterranean diet is best
Diagnosis of Parkinson’s….
Process of elimination
Must include all three categories
What are the three categories in diagnosis? (PD)
Bradykinesia = Slow movement(s)
ONE or MORE of the following…
Muscular rigidity
Resting tremor (unilateral)
Postural instability
Decrease in symptoms on dopamine medication
Primary signs and symptoms of Parkinson’s….
Bradykinesia
Muscle Rigidity
Tremor
Postural Instability
Bradykinesia is….
Reduced ability to initiate/coordinate movements
Freezing/start hesitation
Slowness
Incomplete motions/Decreased perception of motion
Muscle Rigidity is….
On the same side as the tremor
Stiffness can add to decreased joint ROM and cause pain
Stiffness can contribute to a lack of balance
Tremor is described as…
Pill Rolling (hand movement)
Resting tremor (tremor is not bad with movements, but resting there is a tremor)
Postural Instability (PD)
Occurs later in disease progression
Cant catch themselves when imbalance occurs
Retropulsion difficulties (when an individual starts falling backwards they cannot catch themselves)
What exercises can you do to strengthen postural instability? (PD)
Have the individual perform medicine ball throws
Signs and symptoms begin with… (PD)
60-80% of cell death - This is typically when diagnosis occurs, this is because the body survives for as long as possible until it cant anymore causing symptoms
Pathophysiology of Cell Damage (PD)
Chronic inflammation/oxidative stress causes progressive cell death of neurons in substantia nigra that produce DOPAMINE, and the dopamine RECEPTORS
Damage to Norepinephrine producing neurons (need to be ready for ANS dysfunction)