Benign leukocytoses 19 study document
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
24 Terms
Benign leukocytoses
Benign leukocytoses are non-malignant increases in white blood cell (WBC) count. They are typically
reactive and occur in response to physiological or pathological stimuli such as infections, stress,
inflammation, or other systemic conditions.
The main types of benign leukocytoses include:
• Neutrophilia
• Lymphocytosis
• Eosinophilia
• Basophilia
• Monocytosis
1. Neutrophilia
Definition:
Neutrophilia is defined as an increased number of neutrophils in the blood, typically above 7,500/μL
in adults.
Function of Neutrophils:
• First responders to bacterial infections.
• Major contributors to acute inflammation.
• Kill pathogens via phagocytosis, oxidative burst, and degranulation.
Neutrophil Distribution:
• Bone Marrow: Contains most neutrophils at all stages of development.
• Peripheral Blood: Only ~5% of neutrophils are in circulation.
o Of these, ~50% are in the circulating pool.
o The other 50% are marginated (adhered to vessel walls).
Types of Neutrophilia:
1. Mature Neutrophilia
• Increased segmented neutrophils (fully developed).
• Seen in:
o Bacterial infections
o Tissue necrosis
o Inflammatory disorders
o Stress response
o Glucocorticoid therapy
o Post-surgery, trauma
2. Immature Neutrophilia (Left Shift)
• Presence of band cells, metamyelocytes, myelocytes, or earlier forms in blood.
• Indicates increased bone marrow activity or marrow stress.
Causes of Immature Neutrophilia:
• Severe infections (especially bacterial)
• Severe anemia (marrow compensation)
• Bone marrow infiltration (e.g., fibrosis, metastases)
• Myeloproliferative disorders
Key Concepts:
Left Shift
• Increased presence of immature neutrophils.
• Indicator of acute infection or marrow stimulation.
Leukemoid Reaction
• Extreme leukocytosis (>50,000 WBC/μL).
• Resembles leukemia but is reactive (not malignant).
• Seen in severe infections or stress.
Leukoerythroblastic Reaction
• Presence of immature myeloid and erythroid cells in blood.
• Suggests bone marrow infiltration (e.g., metastatic cancer, fibrosis).
Toxic Changes in Neutrophils:
Seen in response to severe infection or inflammation:
• Toxic Granulation: Coarse, dark granules.
• Döhle Bodies: Pale blue inclusions, aggregates of rough ER.
• Cytoplasmic Vacuolization: Indicates phagocytic activity, may suggest sepsis.
o Most concerning finding.
2. Lymphocytosis
Definition:
Increase in lymphocyte count above:
• Adults: >4,000/μL
• Children: Normal range higher (up to 9,000/μL in infants).
Functions of Lymphocytes:
• T cells (80%): Cellular immunity.
• B cells (15%): Humoral immunity.
• NK cells (5%): Natural cytotoxicity.
Types of Lymphocytosis:
1. Mature Lymphocytosis
• Increased number of small, mature-appearing lymphocytes.
• Causes:
o Infectious lymphocytosis
o Bordetella pertussis (whooping cough)
o Stress (e.g., post-exercise)
2. Reactive (Atypical) Lymphocytosis
• Large, irregular lymphocytes (often activated T cells).
• "Downey cells" or plasmacytoid appearance.
• Seen in:
o Infectious mononucleosis (EBV)
o CMV
o Viral hepatitis
o Pediatric viral infections
o Autoimmune diseases
3. Eosinophilia
Definition:
Eosinophil count > 500/μL.
Functions:
• Important in parasite defense and allergic reactions.
Causes:
• Parasitic infections (esp. helminths)
• Allergic conditions (asthma, hay fever)
• Drug hypersensitivity
• Skin diseases (eczema, pemphigus)
• Hodgkin lymphoma, other malignancies
• Autoimmune diseases
Eosinophils are characteristically found in which of the following conditions?
Parasitic infections
Basophilia
Definition:
Basophil count > 100/μL (rarely seen in benign conditions).
Causes:
• Chronic myeloid leukemia (CML): most common association.
• Myeloproliferative neoplasms
• Rarely in:
o Hypersensitivity reactions
o Endocrine disorders (e.g., hypothyroidism)
Monocytosis
Definition:
Monocyte count > 1,000/μL.
Functions:
• Phagocytosis
• Antigen presentation
• Differentiate into macrophages in tissues.
Causes:
• Chronic infections (e.g., tuberculosis, endocarditis)
• Autoimmune diseases (e.g., lupus, rheumatoid arthritis)
• Malignancies (e.g., Hodgkin lymphoma)
Diagnostic Approach to Leukocytosis
When leukocytosis is found on a complete blood count (CBC), a systematic approach is important to
determine whether it's reactive (benign) or malignant.
Step 1: Confirm the Type of Leukocytosis
• Neutrophils ↑ → Neutrophilia
• Lymphocytes ↑ → Lymphocytosis
• Eosinophils ↑ → Eosinophilia
• Basophils ↑ → Basophilia
• Monocytes ↑ → Monocytosis
Check the absolute counts, not just percentages.
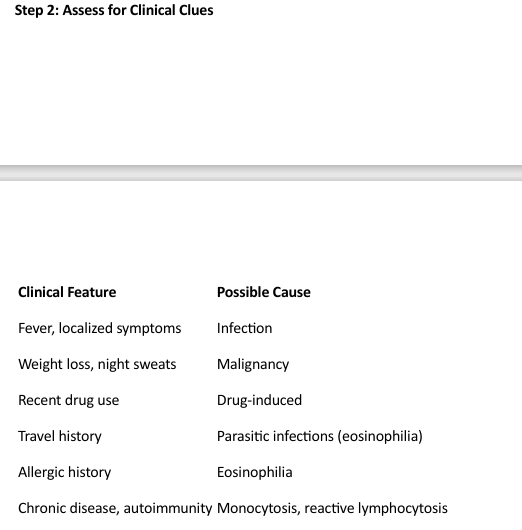
Step 2: Assess for Clinical Clues
Step 3: Peripheral Blood Smear
Examine for:
• Left shift: Bands, metamyelocytes → infection or stress
• Blasts: Suggest leukemia
• Toxic granulation, Döhle bodies, vacuolization: Infection
• Atypical lymphocytes: Viral infections (e.g., EBV)
• Basophilia + eosinophilia + myelocytes → think CML
Step 4: Additional Tests
• Infection markers: CRP, procalcitonin
• Serologies: EBV, CMV, HIV
• Bone marrow biopsy: If malignancy suspected
• Flow cytometry: Immunophenotyping (e.g., for lymphoproliferative disorders)
Differential Diagnosis: Leukemoid Reaction vs. CML

Physiological Leukocytosis
Occurs without disease:
• Exercise
• Pregnancy
• Smoking
• Postpartum
• Emotional stress
• Seizures
• Exposure to heat or cold
Usually transient, and no treatment needed.
Drug-Induced Leukocytosis
Several drugs can stimulate WBC production or release:
• Glucocorticoids: Demargination of neutrophils
• Lithium: Stimulates granulopoiesis
• Epinephrine: Mobilizes marginated pool
• Colony-stimulating factors (e.g., G-CSF): Used therapeutically
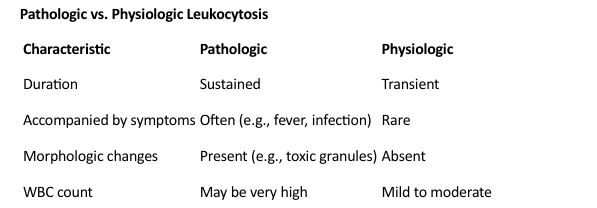
Pathologic vs. Physiologic Leukocytosis
Clinical Relevance
• Recognition of benign leukocytosis prevents unnecessary bone marrow biopsy or concern for
leukemia.
• Persistent or unexplained leukocytosis, especially with blasts, basophilia, or splenomegaly,
should raise suspicion for hematologic malignancies.
• Understanding reactive patterns helps differentiate infections and autoimmune disorders
from neoplastic conditions.
A 10-year-old child has a WBC count of 15,000/μL, with 70% lymphocytes and atypical lymphocytes on smear. What’s the most likely cause?
Infectious mononucleosis
Which condition is most likely associated with eosinophilia?
Parasitic infection
What distinguishes a leukemoid reaction from CML?
High LAP score in leukemoid, low in CML; Philadelphia chromosome absent in leukemoid