Circulatory System: Blood Vessels, Blood Pressure, and Hemodynamics
1/77
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
78 Terms
What is the primary function of the circulatory system?
To transport blood, nutrients, gases, and waste products throughout the body.
What are the main components of the circulatory system?
The heart, blood vessels (arteries, veins, and capillaries), and blood.
What type of blood vessels carry blood away from the heart?
Arteries.
What type of blood vessels return blood to the heart?
Veins.
What are capillaries and their role in the circulatory system?
Capillaries are small blood vessels where the exchange of gases, nutrients, and waste occurs between blood and tissues.
Who was the first to correctly understand that blood circulates around the body?
Chinese emperor Huang Ti (2697 to 2597 BC)
What did William Harvey demonstrate about blood circulation?
He showed that the heart pumps blood in a circuit.
What are the three principal categories of blood vessels?
Arteries, veins, and capillaries.
What is the function of arteries?
They carry blood away from the heart.
What is the function of veins?
They carry blood back to the heart.
What connects the smallest arteries to the smallest veins?
Capillaries.
What are the three layers of blood vessel walls?
Tunica interna, tunica media, and tunica externa.
What is the role of the tunica interna?
It lines the blood vessel and is exposed to blood, serving as a selectively permeable barrier.
What is the function of the tunica media?
It consists of smooth muscle that controls blood vessel diameter and strengthens the vessel.
What does the tunica externa do?
It anchors the vessel and provides passage for small nerves and lymphatic vessels.
What are conducting arteries?
The largest arteries, such as the aorta, that expand during systole and recoil during diastole.
What are distributing arteries?
Medium-sized arteries that distribute blood to specific organs.
What are resistance arteries?
Small arteries with a thicker tunica media in proportion to their lumen.
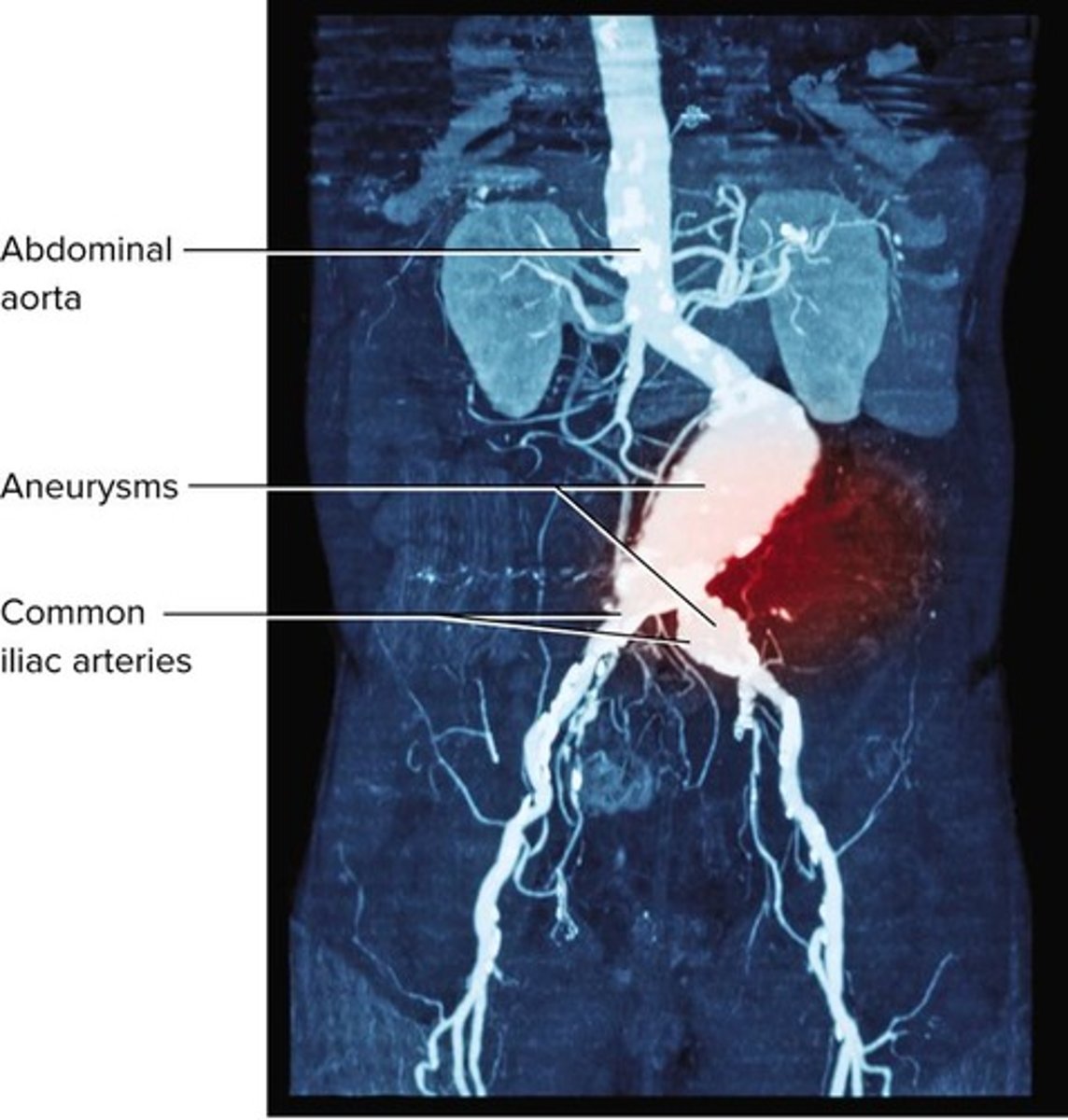
What is an aneurysm?
A weak point in an artery or heart wall that forms a bulging sac that may rupture.
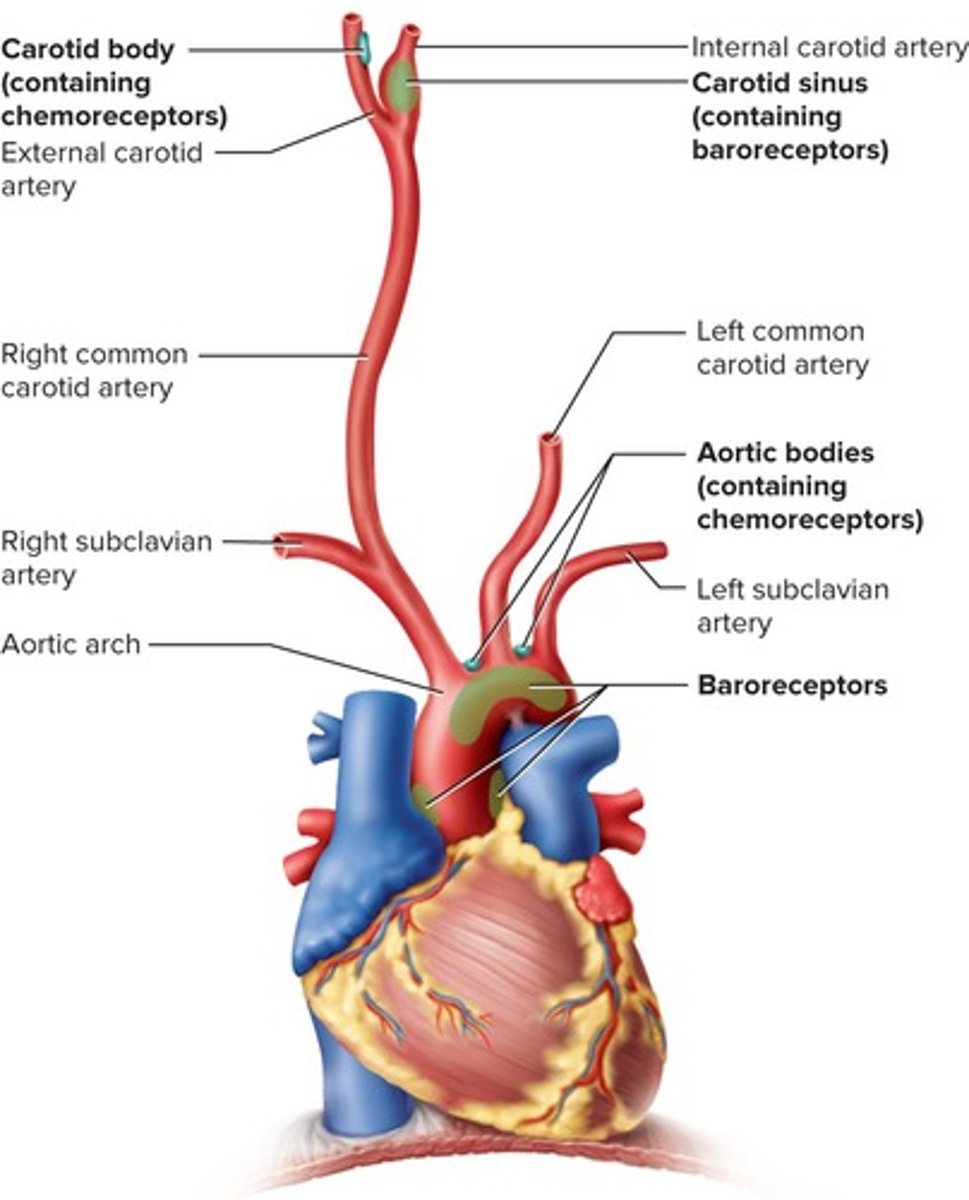
What are carotid sinuses?
Baroreceptors in the walls of the internal carotid artery that monitor blood pressure.
What are capillaries primarily used for?
They are exchange vessels where gases, nutrients, wastes, and hormones pass between blood and tissue fluid.
What are continuous capillaries?
Capillaries with tight junctions that allow passage of solutes like glucose.
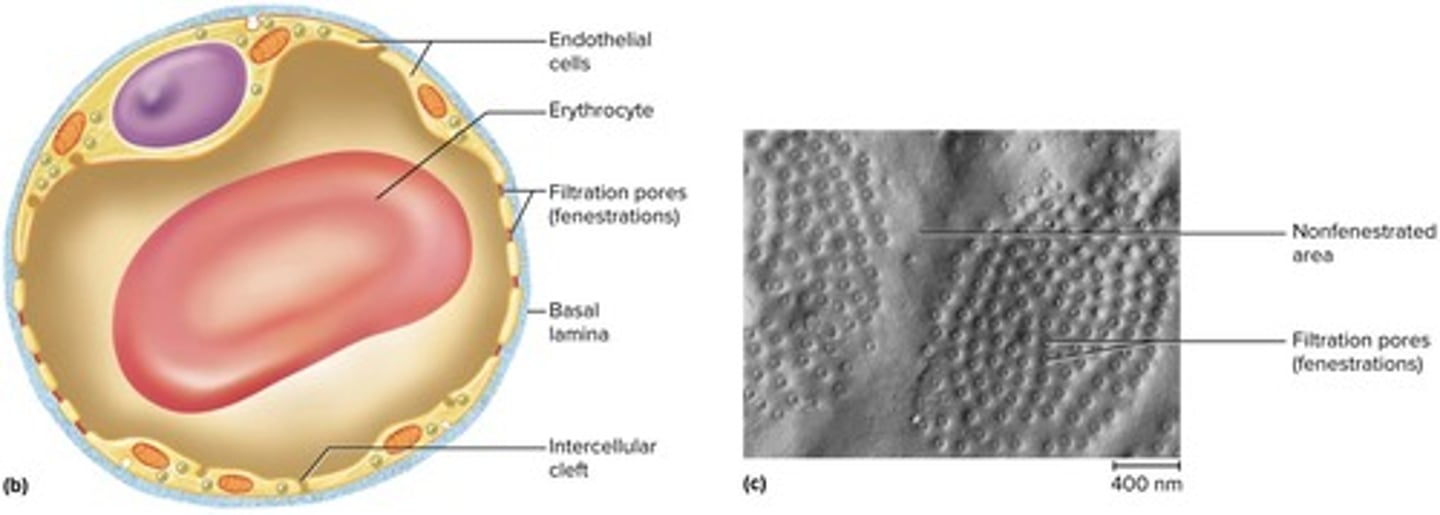
What are fenestrated capillaries?
Capillaries with filtration pores that allow rapid absorption or filtration, found in organs like kidneys.
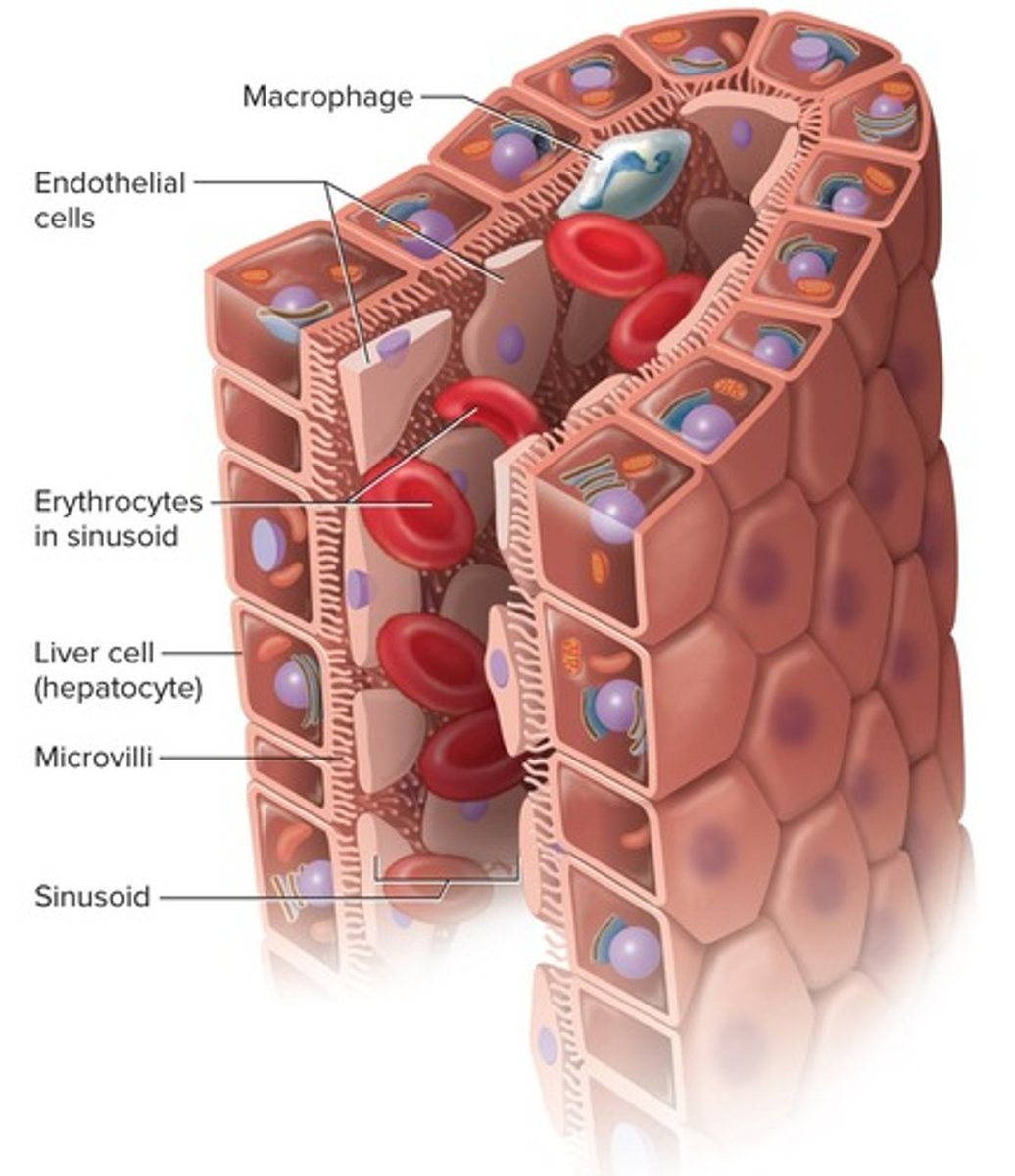
What are sinusoids?
Irregular blood-filled spaces in the liver and spleen that allow larger molecules to enter circulation.
What is a capillary bed?
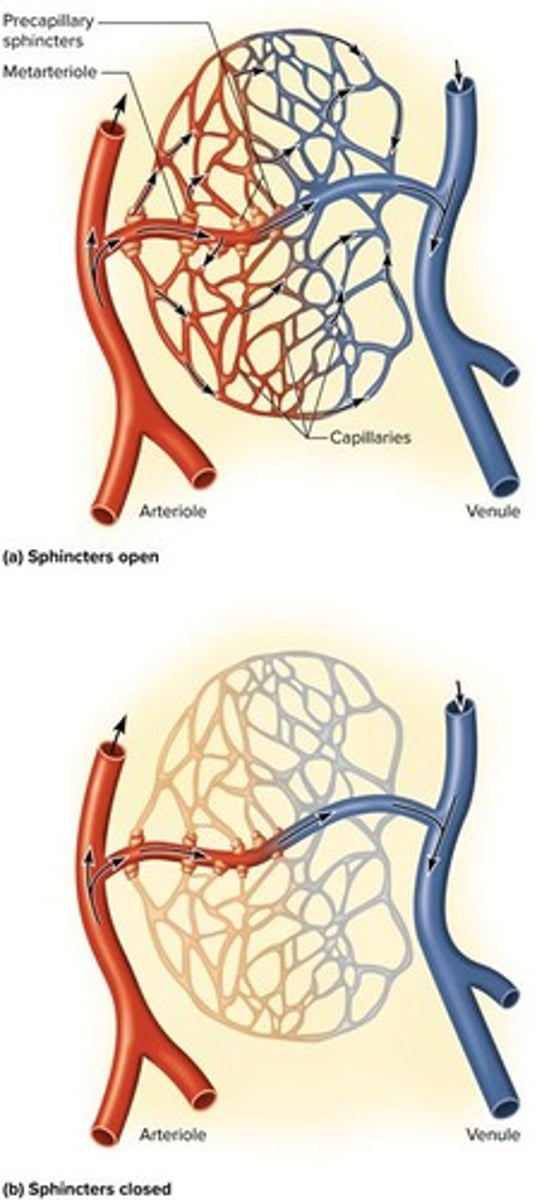
A network of 10 to 100 capillaries supplied by a single arteriole or metarteriole.
What is the role of precapillary sphincters?
They control blood flow in capillary beds by constricting or relaxing.
What characterizes veins compared to arteries?
Veins are thin-walled, flaccid, and have a greater capacity for blood containment.
What are varicose veins?
Enlarged veins that occur when blood pools and valves fail, often seen in the lower legs.
What is the simplest route for blood circulation?
Heart → arteries → arterioles → capillaries → venules → veins.
What is a portal system in circulation?
A pathway where blood flows through two consecutive capillary networks before returning to the heart.
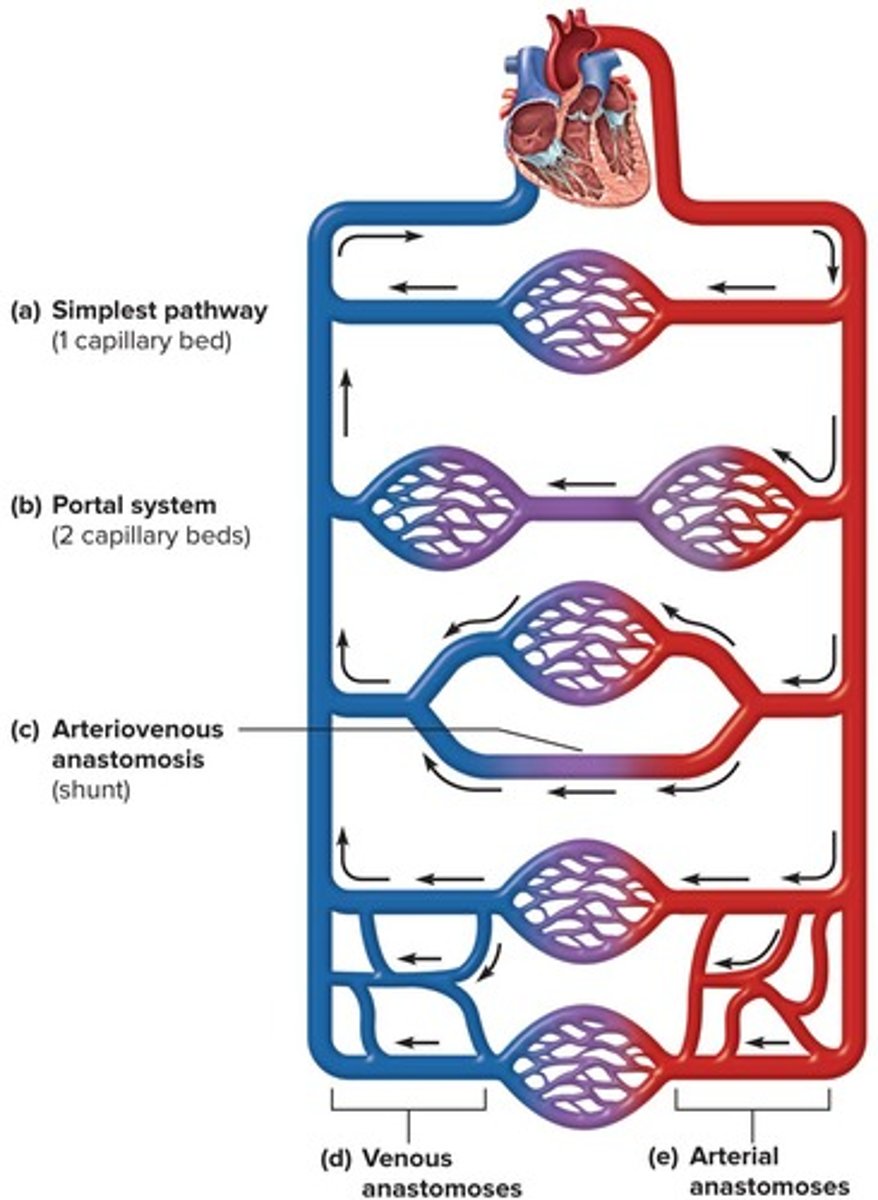
What is an anastomosis in the circulatory system?
Convergence between two vessels other than capillaries.
What is an arteriovenous anastomosis?
A shunt where an artery flows directly into a vein.
What is a venous anastomosis?
The most common type of anastomosis where one vein empties directly into another.
What is an arterial anastomosis?
A connection where two arteries merge, providing collateral routes of blood supply.
What does blood flow refer to?
The amount of blood flowing through an organ, tissue, or blood vessel in a given time (mL/min).
What is perfusion?
Flow per given volume or mass of tissue in a given time (mL/min/g).
What is hemodynamics?
The physical principles of blood flow based on pressure and resistance.
How is blood pressure (BP) defined?
The force that blood exerts against a vessel wall.
Where is blood pressure typically measured?
At the brachial artery using a sphygmomanometer.
What are the two pressures recorded in blood pressure measurements?
Systolic pressure (peak arterial BP during ventricular contraction) and diastolic pressure (minimum arterial BP during ventricular relaxation).
What is the normal blood pressure value for a young adult?
120/75 mm Hg.
What is pulse pressure?
The difference between systolic and diastolic pressure.
What is mean arterial pressure (MAP)?
Diastolic pressure plus one-third of pulse pressure.
What is arteriosclerosis?
The stiffening of arteries due to deterioration of elastic tissues of artery walls.
What is atherosclerosis?
The buildup of lipid deposits that become plaques in the arteries.
What is hypertension?
High blood pressure defined as chronic resting BP greater than 130/80 mm Hg.
What are the consequences of hypertension?
Can weaken arteries, cause aneurysms, and promote atherosclerosis.
What is hypotension?
Low blood pressure, often caused by blood loss, dehydration, or anemia.
What three variables determine blood pressure?
Cardiac output, blood volume, and resistance to flow.
What is peripheral resistance?
The opposition to flow that blood encounters in vessels away from the heart.
What factors influence peripheral resistance?
Blood viscosity, vessel length, and vessel radius.
What are vasoreflexes?
Changes in vessel radius, including vasoconstriction and vasodilation.
What happens to blood velocity from the aorta to capillaries?
Blood velocity decreases due to greater distance traveled, smaller radii of arterioles and capillaries, and increased friction.
What happens to the number of vessels and their total cross-sectional area as you move farther from the heart?
The number of vessels and their total cross-sectional area increases.
How does blood velocity change from capillaries to the vena cava?
Blood velocity increases again as it moves from capillaries to the vena cava.
Why do veins create less resistance than capillaries?
Veins are larger, allowing a larger amount of blood to be forced into smaller channels.
What is autoregulation in the context of blood supply?
Autoregulation is the ability of tissues to regulate their own blood supply.
What triggers vasodilation according to the metabolic theory of autoregulation?
Inadequate perfusion leads to waste accumulation, which stimulates vasodilation to increase perfusion.
What are vasoactive chemicals?
Substances secreted by platelets, endothelial cells, and perivascular tissue that stimulate vasomotor responses.
Name two vasodilators.
Histamine and prostaglandins.
What role does the vasomotor center of the medulla play?
It exerts sympathetic control over blood vessels, stimulating most to constrict while dilating vessels in cardiac muscle.
How does angiotensin II affect blood pressure?
It raises blood pressure as a potent vasoconstrictor.
What is the function of aldosterone in blood pressure regulation?
Aldosterone promotes sodium retention by the kidneys, supporting blood pressure.
What effect do natriuretic peptides have on blood pressure?
They lower blood pressure by antagonizing aldosterone and promoting vasodilation.
What is the primary mechanism of capillary exchange?
Diffusion is the most important form of capillary exchange.
What are the three routes chemicals can take to pass through capillary walls?
Through endothelial cell cytoplasm, intercellular clefts, and filtration pores of fenestrated capillaries.
What causes edema?
Edema is caused by the accumulation of excess fluid in a tissue due to increased capillary filtration, reduced reabsorption, or obstructed lymphatic drainage.
What are the three principal forms of low venous return (LVR) shock?
Hypovolemic shock, obstructed venous return shock, and venous pooling shock.
What is compensated shock?
A state where homeostatic mechanisms bring about spontaneous recovery.
What happens to the brain after seconds of blood deprivation?
Loss of consciousness occurs after seconds of deprivation.
What are the major branches of the aorta?
The right and left coronary arteries, brachiocephalic artery, right and left common carotid arteries, and right and left subclavian arteries.
What is portal hypertension?
A condition caused by obstruction of hepatic circulation leading to increased pressure in the portal vein.
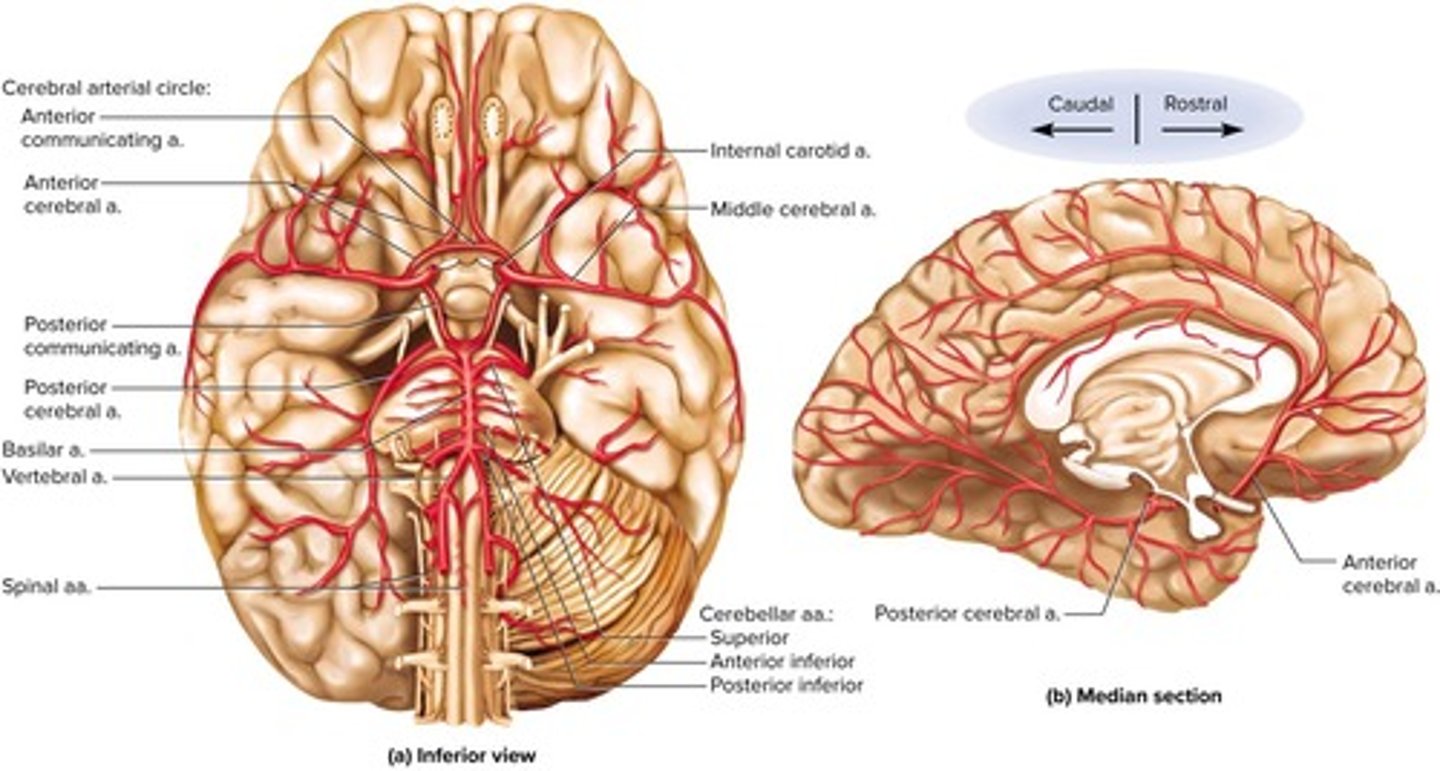
What is the significance of the Circle of Willis?
It is an arterial anastomosis at the base of the brain that receives blood from the basilar and internal carotid arteries.
What is the role of the thoracic pump in venous return?
Inhalation expands the thoracic cavity, aiding blood flow back to the heart.
What is transcytosis in capillary exchange?
Vesicle-mediated transport that moves materials across the endothelium.
What are the pathological consequences of severe edema?
Tissue necrosis, impaired oxygen delivery, pulmonary edema, and cerebral edema.
What is the effect of epinephrine and norepinephrine on blood vessels?
They cause vasoconstriction.
What is the primary purpose of vasomotion?
To control blood pressure and route blood from one body region to another.