Biology - Chapter 16: Homeostasis
1/99
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
100 Terms
Homeostasis
The maintenance of a constant internal environment within restricted limits.
What does it mean if the medulla becomes thicker?
The loop of Henle is longer
2 reasons why homeostasis is important
1. To maintain a stable blood pH and core temperature
2. To maintain a stable blood glucose concentration
Why is it important that homeostasis is used to maintain a stable blood pH and core temperature?
Enzymes are sensitive to changes in pH and temperature and any change may affect the rate of reaction or denature them - if pH and temperature are kept constant, it ensures that reactions take place at a stable rate
Why is it important that homeostasis is used to maintain a stable blood glucose concentration?
Changes to BGC affect blood water potential so may cause cells to shrink / expand + if need constant BGC to ensure a reliable source of glucose for respiration in cells
5 stages of a control mechanism
1. The optimum point
2. Receptor
3. Coordinator
4. Effector
5. Feedback mechanism
Repeat!!
2 types of control mechanisms
Positive feedback and negative feedback
Negative feedback
When the change triggers a response which reduces the effect of a change (back to the optimum level)
Positive feedback
When a deviation from the optimum causes changes that result in an even greater deviation from the normal
Why do control centres have many receptors and effectors?
It allows them to have separate mechanisms that each produce a positive movement towards the optimum so there is a greater degree of control of the particular factor being regulated
4 features of hormones
1. Produced in glands, which secrete it directly into the blood
2. Carried in the blood plasma to the cells they act on (the target cells) which have specific receptors on their CSM complementary to them
3. Effective in low concentrations
4. Often have widespread and long-lasting effects
Example of a use of the second messenger model
The regulation of BGC by adrenaline and glucagon
Describe the second messenger model mechanism involving adrenaline (7)
1. Adrenaline binds to a transmembrane protein receptor in the CSM of a cell
2. This causes the protein to change shape on the inside of the membrane
3. This causes the enzyme adenyl cyclase to be activated
4. Adenyl cyclase converts ATP to cAMP
5. cAMP acts as a second messenger that binds to a protein kinase enzyme
6. This changes the shape of protein kinase, activating it
7. The protein kinase enzyme catalyses the conversion of glycogen to glucose
cAMP
Cyclic AMP
What is the role of the pancreas in controlling blood glucose?
Has islets of Langerhans that detect changes in the BGC and produce insulin or glucagon in order to regulate BGC
2 types of islets of Langerhans cells
α-cells and β-cells
Which one's bigger - α-cells or β-cells?
α-cells
What is the function of α-cells?
Produce glucagon
What is the function of β-cells?
Produce insulin
3 processes that take place in the liver to regulate BGC
Glycogenesis, glycogenolysis and gluconeogenesis
Glycogenesis
The conversion of glucose into glycogen
Glycogenolysis
The breakdown of glycogen to glucose
Gluconeogenesis
The production of glucose from sources other than carbohydrates
3 sources of blood glucose
1. Directly from the diet (hydrolysis of carbohydrates)
2. Glycogenolysis in the small intestine
3. Gluconeogenesis
3 main hormones that control blood glucose concentration
Insulin, glucagon and adrenaline
What do β-cells detect?
A rise in BGC
How do β-cells and insulin affect the BGC? (4)
1. β-cells detect the increase in BGC so secrete insulin into the blood
2. Insulin binds to the glycoprotein receptors on the CSM of body cells
3. This causes cells to take up more glucose
4. Overall, it causes BGC to decrease to the optimum level
What happens to body cells after insulin binds to the glycoprotein receptors? (3)
1. It causes the tertiary structure of the glucose transport carrier protein to change shape and open so more glucose moves into cells by facilitated diffusion
2. It causes an increase in the number of carrier proteins responsible for glucose transport in the CSM
3. It activates enzymes that convert glucose into glycogen or fat
After it binds to body cells, how does insulin lower BGC? (4)
1. It increases the rate of absorption of glucose into cells
2. It increases the respiratory rate of cells, so they use more glucose and more is taken up
3. It increases the rate of conversion of glucose into glycogen in the cells of the liver and muscles
4. It increases the rate of conversion of glucose into fat
What do α-cells detect?
A fall in BGC
How do α-cells and glucagon affect the BGC? (5)
1. α-cells detect a fall in BGC and secrete glucagon
2. Glucagon attaches to specific protein receptors on the CSM of liver cells
3. It activates the enzymes that convert glycogen to glucose
4. It also activates enzymes that convert amino acids and glycerol into glucose
5. This increases BGC to the optimum
How does adrenaline affect BGC? (2)
1. It attaches to protein receptors on the CSM of target cells
2. It activates enzymes that catalyse the breakdown of glycogen into glucose in the liver
Why are insulin and glucagon said to work antagonistically?
They act in opposite directions - insulin lowers BGC, while glucagon increases it
Is the concentration of glucose constant?
No - it fluctuates about an optimum point
Diabetes
A disease in which a person is unable to metabolise carbohydrate, especially glucose
2 types of diabetes
Type 1 (insulin dependent) and Type 2 (insulin independent)
When does Type 1 diabetes start?
Normally in childhood
How is Type 1 diabetes caused?
The body is unable to produce insulin e.g. due to an autoimmune response where the body's immune system attacks its own β-cells
When does Type 2 diabetes start?
Usually in people over 40
How is Type 2 diabetes caused? (2)
1. Glycoprotein receptors on body cells being lost or losing their responsiveness to insulin
2. An inadequate supply of insulin from the pancreas
How is Type 1 diabetes treated?
Insulin injections (biosensors used to monitor BGC to determine dose of insulin to be given) along with managing the carbohydrate intake
How is Type 2 diabetes treated?
Regulating the intake of carbohydrate in the diet and matching this to the amount of exercise taken, potentially along with insulin injections or drugs that stimulate insulin production or that slow down the rate of glucose absorption
Osmoregulation
The homeostatic control of the water potential of the blood
Nephron
The functional unit of the kidney
7 parts of the kidney
- Fibrous capsule
- Cortex
- Medulla
- Renal pelvis
- Ureter
- Renal artery
- Renal vein
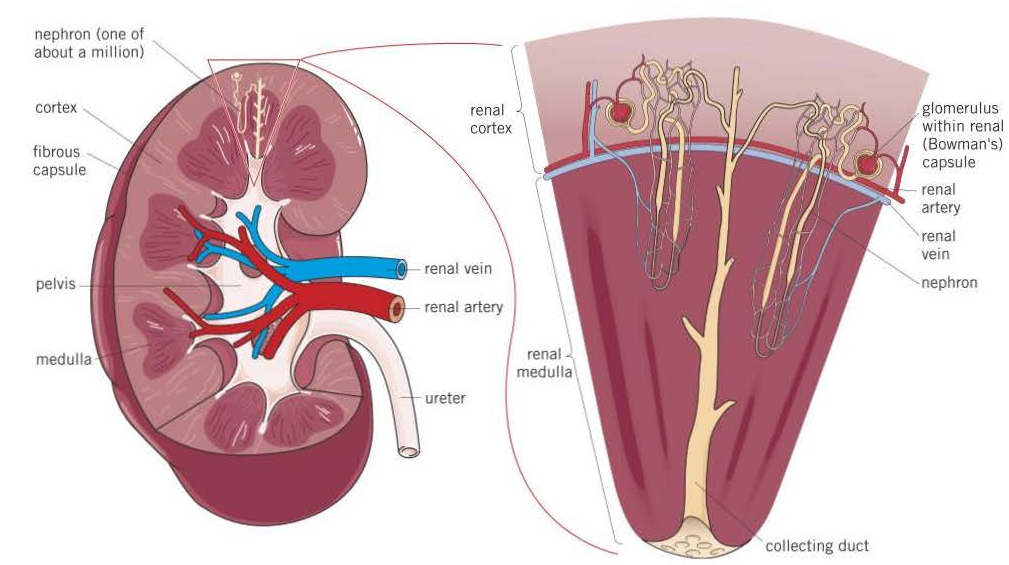
Fibrous capsule
Outer membrane that protects the kidney
Cortex
A lighter coloured region made up of renal (Bowman's) capsules, convoluted tubules and blood vessels
Medulla
A darker coloured inner region made up of loops of Henle, collecting ducts and blood vessels
Renal pelvis
Funnel-shaped cavity that collects urine into the ureter
Ureter
A tube that carries urine into the bladder
Renal artery
Supplies the kidney with blood from the heart via the aorta
Renal vein
Returns blood to the heart via the vena cava
5 parts of the nephron + 4 blood vessels
5 parts:
- Renal (Bowman's) capsule
- Proximal convoluted tubule
- Loop of Henle
- Distal convoluted tubule
- Collecting duct
4 blood vessels:
- Afferent arteriole
- Glomerulus
- Efferent arteriole
- Blood capillaries
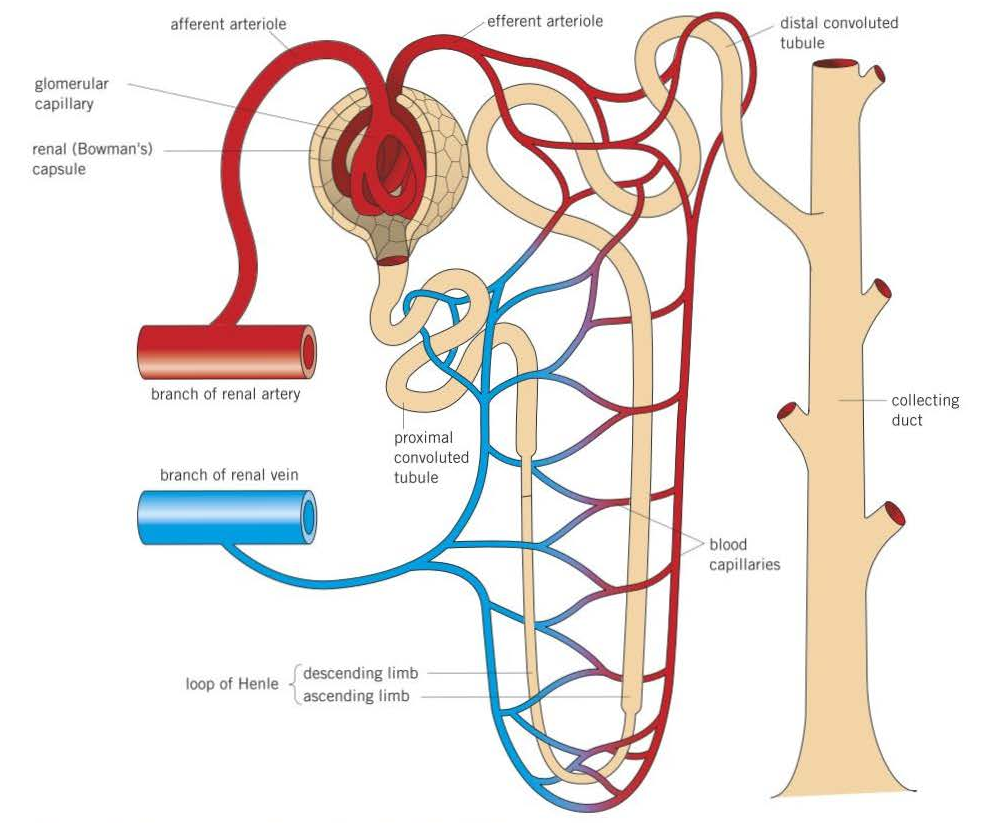
Bowman's capsule
The cup-shaped portion at the start of the nephron that encloses the glomerulus
Proximal convoluted tubule
Series of loops surrounded by blood capillaries - has walls made of epithelial cells with microvilli
Loop of Henle
Long, hairpin loop that extends from the cortex into the medulla and back again (it is also surrounded by blood capillaries)
Distal convoluted tubule
Series of loops surrounded by blood capillaries - has walls made of epithelial cells but is surrounded by fewer capillaries than the proximal tubule
Collecting duct
A tube into which a number of distal convoluted tubules from a number of nephrons empty - lined by epithelial cells and becomes increasingly wide as it empties into the pelvis of the kidney
Afferent arteriole
A tiny vessel that ultimately arises from the renal artery and supplies the nephron with blood.
Glomerulus
A many-branched knot of capillaries from which fluid is forced out of the blood
Efferent arteriole
A tiny vessel that leaves the renal capsule and carries blood away. It has a smaller diameter than the afferent arteriole so causes an increase in blood pressure within the glomerulus.
Blood capillaries
A connected network of capillaries that surrounds the proximal convoluted tubule, the loop of Henle and the distal convoluted tubule from where they reabsorb mineral salts, glucose and water.
What happens to the blood capillaries in the kidney?
They merge together to form venules that then merge together to form the renal vein
4 stages of osmoregulation
1. The formation of glomerular filtrate by ultrafiltration
2. The reabsorption of glucose and water by the proximal convoluted tubule
3. The maintenance of a gradient of Na+ ions in the medulla by the loop of Henle
4. The reabsorption of water by the distal convoluted tubule and collecting ducts
Describe the process of the formation of glomerular filtrate by ultrafiltration (4)
High hydrostatic pressure forces water, glucose, ions and urea out
They are forced out through fenestrations in the capillary endothelium
And through the capillary basement membrane
Meanwhile, proteins remain as they are too large to move through the filter
What resists the movement of the glomerular filtrate out of the glomerulus? (5)
- Capillary epithelial cells
- Connective tissue and the epithelial cells of the blood capillary
- Epithelial cells of the renal capsule
- The hydrostatic pressure of the fluid in the renal capsule
- The low water potential of the blood in the glomerulus
What features are there to reduce the resistance against the movement of glomerular filtrate out of the glomerulus? How does this reduce the resistance against the filtrate's movement? (2 + 1)
1. Podocytes, which make up the inner layer of the renal capsule: they have spaces beneath them through gaps between their branches rather than through them
2. Fenestrations in the glomerular capillaries: fluid passes between, rather than through, these cells
These increase the hydrostatic pressure of the blood in the glomerulus so it can overcome the resistance
What does ultrafiltration operate on the basis of?
The size of the molecule - small ones are removed
5 adaptations of the proximal convoluted tubules
1. Microvilli: provide a large surface area to reabsorb substances from the filtrate
2. Many mitochondria: provide ATP for active transport
3. Many channel/carrier proteins for active transport
4. Many channel/carrier proteins for co-transport
5. Many ribosomes to produce carrier/channel proteins
Describe how the proximal convoluted tubule reabsorbs glucose and water (4)
1. Na+ ions actively transported out of cells lining the PCT into the blood capillaries
2. This lowers the Na+ concentration of these cells
3. Na+ ions diffuse down the diffusion gradient from the lumen of the PCT into the epithelial lining cells by facilitated diffusion via carrier proteins
4. The carrier proteins carry another type of molecule (e.g. glucose, amino acids, ions) with the sodium ions - co-transport
5. These molecules then diffuse into the blood
How does the proximal convoluted tubule reabsorb glucose, amino acids and ions?
By active transport and co-transport
Describe how the loop of Henle maintain a gradients of Na+ ions absorbs water from the filtrate. (7)
Ascending limb walls impermeable to water
At ascending limb, Na+ ions actively transported out
Ions move into medulla, lowering the water potential
Some ions also diffuse into the descending limb
(more ions in medulla, so lower water potential there than in descending limb)
Descending limb walls permeable to water, so water moves out by osmosis
Deeper into medulla, the lower the water potential in the medulla - tip of the hairpin has lowest medulla water potential
This process is known as the countercurrent mechanism
2 regions of the loop of Henle
The descending limb and the ascending limb
Describe the descending limb of the loop of Henle
Narrow with thin walls highly permeable to water
Describe the ascending limb of the loop of Henle
Wider with thick walls impermeable to water
Interstitial region
The region of the medulla between the two limbs of the loop of Henle
What part of the loop of Henle has the lowest water potential?
The tip of the hairpin
What does the countercurrent multiplier do? (3)
The filtrate in the descending limb and ascending limb of the Loop of Henle move in opposite directions
The water potential of the descending limb decreases as you go down while the water potential of the ascending limb increases as you go up
Ensures that there is always a water potential gradient in the medulla drawing water out of the Loop of Henle into the blood.
How does the distal convoluted tubule and collecting ducts reabsorb water? (2)
The cells that make up the distal convoluted tubule have microvilli and mitochondria so can reabsorb mineral ions from the filtrate by active transport, adjusting the water and salts reabsorbed and controlling the pH of the blood
What might cause a decrease in the water potential of the blood? (3)
1. Too little water being consumed
2. Too much sweating occurring
3. Large amount of ions being taken in
What happens when there is a fall in water potential of the blood? (12)
1. Osmoreceptors detect the fall in water potential of the blood
2. They send more nerve impulses to the thirst centre of the brain to encourage the individual to drink more water
3. Water moves out of the osmoreceptors by osmosis and they shrink
4. This causes the hypothalamus to produce ADH, which is then secreted by the pituitary gland into the capillaries
5 ADH passes in the blood to the kidney
6. Specific protein receptors on the CSM of the cells of the DCT and collecting duct bind to ADH, causing the enzyme phosphorylase to be activated
7. This causes vesicles containing aquaporins in the cells to move to and fuse with the CSM
8. This increases the number of water channels, increasing the permeability of the DCT and collecting duct to water
9. This means more water moves into the DCT and collecting duct, increasing the water potential
10. ADH also increases the permeability of the collecting duct to urea, so urea moves out, lowing the water potential of fluid around the duct
11. This causes more water to move out of the collecting duct by osmosis down the water potential gradient - the water then re-enters the blood
12. Osmoreceptors detect the increase in the water potential and send fewer impulses to the pituitary gland so less ADH is secreted
What detects changes in the water potential of the blood?
Osmoreceptors in the hypothalamus of the brain
ADH
Antidiuretic hormone
Where is ADH produced?
The hypothalamus
From where is ADH secreted from?
Posterior pituitary gland
Aquaporins
Water channel proteins
When osmoreceptors detect a fall in the water potential of the blood and secrete ADH, what happens to the water potential of the blood?
It is prevented from getting any lower (rather than increasing) as the re-absorbed water originally came from the blood
What might cause an increase in the water potential of the blood? (2)
1. Large volumes of water being consumed
2. Salts used in metabolism or excreted not being replaced in the diet
What happens when there is an increase in the water potential of the blood? (6)
1. Osmoreceptors detect the increase in water potential
2. This causes them to increase the frequency of nerve impulses to the pituitary gland to reduce its release of ADH
3. As there is less ADH in the blood, the permeability of the collecting duct to water and urea decreases
4. Less water is reabsorbed into the blood from the collecting duct and the water potential of the blood falls
5. More dilute urine is produced
6. When the water potential of the blood returns to normal, the osmoreceptors cause the pituitary gland to increase its ADH release to normal levels
How does the release of ADH affect blood pressure? (2)
ADH increases the re-absorption of water, increasing the volume of blood so pressure increases
What happens to the concentration of filtrate as it moves along the loop of Henle? (2)
Concentration rises in the descending limb as Na+ ions enter by diffusion and water is lost
Concentration then falls in the ascending limb as Na+ ions are actively removed while water remains as the walls are impermeable to water
Why is glucose found in the urine of a person with untreated diabetes? (2)
There is a high concentration of glucose in their blood, and so in their filtrate
Not all the glucose is reabsorbed at the proximal convoluted tubule by facilitated diffusion/active transport as the carrier proteins are saturated
Why would no glucose be found in the urine of a person without diabetes? (2)
The glucose would leave the blood at the kidney
It would then be reabsorbed in the proximal convoluted tubule
If the glomerular filtrate of a diabetic person contains a high concentration of glucose, why would they produce a larger volume of urine? (3)
The glucose in the filtrate lowers the water potential
This causes a lower water potential gradient between the filtrate and blood plasma
As a result, less water is reabsorbed by osmosis
What happens as the length of the Loop of Henle increases? (4)
More Na+ ions actively transported out of the ascending limb
Greater Na+ concentration in the medulla
Water potential gradient is maintained for longer
More water is reabsorbed from the loop of Henle by osmosis into the blood
What would happen if the sodium or chloride ions in the filtrate produced in the nephrons could not be absorbed into the blood? (2)
Lower water potential of filtrate
Reduced water potential gradient so less water reabsorbed by osmosis in the collecting duct
What happens if a cell is more sensitive to insulin? (4)
More insulin binds to receptors
Stimulates uptake of glucose by facilitated diffusion
Activates enzymes that convert glucose to glycogen (glycogenesis)
This lowers the BGC
Why are proteins from the blood plasma not found in the urine? (3)
At the Bowman’s capsule
Proteins cannot normally pass through the filter
i.e. the basement membrane and fenestrations in the capillary endothelium
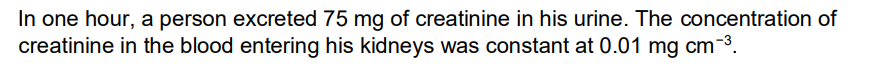
How do you calculate glomerular filtration rate (GFR)? (see example question)
Find amount of creatinine removed in the urine in one minute (e.g. 75/60 = 1.25)
Then, divide by the concentration of creatinine entering kidneys (1.25/0.01 = 125)
Original card for the reabsorption of water at the Loop of Henle.
From the textbook + internet, has more explanation than needed by a MS but can help with understanding.
Original if wanted:
1. Na+ ions are actively transported out of the ascending limb of the loop of Henle into the interstitial region and the descending limb using ATP
2. This creates a low water potential in the interstitial region
3. The thick walls of the ascending limb are impermeable to water, so no water moves out
4. However, the walls of the descending limb are permeable to water, so water moves out of the filtrate by osmosis down the water potential gradient into the interstitial region
5. The water then enters the blood capillaries by osmosis and is carried away
6. The filtrate progressively loses water in this way as it moves down the descending limb - the lowest water potential is reached at the tip of the hairpin
7. At the base of the ascending limb, Na+ ions diffuse out of the filtrate and are also actively pumped out
8. This means the filtrate develops an increasingly higher water potential
9. In the interstitial space between the ascending limb and collecting duct, there is a water potential gradient with the highest in the cortex and an increasingly lower one as you go deeper into the medulla