25: Fractures
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
First thing to do when a patient comes in for a fracture
Treat the patient first! It is likely from trauma, and the fracture can wait
Radiographs to take if a patient presents for a traumatic event and you suspect a fracture
2 views where you suspect the fracture
Check the thorax!!
Why do we need oblique views of the distal limb when evaluating fractures
You will only see the fracture if you are in the plane of view, and they can easily hide in the distal limb
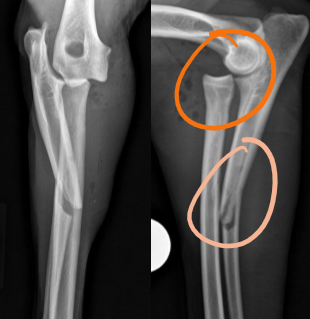
Normal anatomic variations that may mimic a fracture line
Superimposed ST
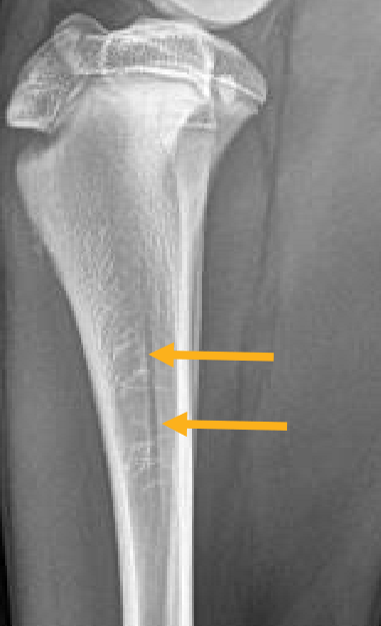
Nutrient foramen
Heel crack (ungulates)
Location of the nutrient foramen
In the cortex of the proximal diaphysis in long bones
List the 7 descriptors for bone fractures
ST changes: open or closed, swelling
Complete or incomplete
Simple or comminuted
Traumatic or pathologic
Configuration
Displacement
Acute or chronic
Why do we care if a fracture is open or closed
Open fractures are or were open to the outside world, and there is an increased risk of infection
Radiographic findings associated with an open fracture
Gas in ST or penetrating debris
Typical cause of diffuse ST swelling
Fluid (edema, hemorrhage, etc.)
Incomplete fracture
Fracture line does not cross from cortex to cortex
Complete fracture
Fracture line crosses from one cortex to the other cortex
Common signalment for an incomplete fracture
Young animals; immature bones are flexible → greenstick fracture
Fissure line
Smaller fracture line extending from the main fracture line
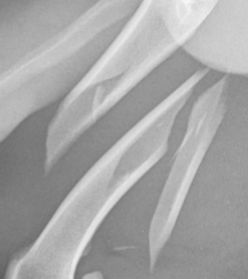
Simple fracture
One line is splitting a bone into two pieces
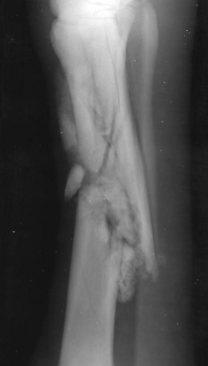
Comminuted fracture
Lots of lines, lots of bone pieces
Pathologic fracture
The bone was not normal prior to the fracture, and broke in response to what might have been a normal amount of stress to the bone
Why do we care to differentiate between traumatic and pathologic fractures
Informs whether and how to treat
List the fracture configurations
Transverse
Oblique
Spiral
Segmental (>1 piece)
Common location for a spiral fracture
Tibia
How is displacement described
How the distal segment of the fracture moved from normal
Radiographic indicators of an acute fracture
Sharp edges with no new bone
Radiographic indicators of a chronic fracture
Rounded edges with periosteal new bone (callus), fracture gap may be increased due to healing processes
Common type of fracture involving the flat bones of the skull
Depression fracture
Common type of fracture involving the spine
Compression fracture
Avulsion fracture
Fracture at the site of soft tissue attachment (enthesis)
Enthesophyte
Periarticular new bone at site of ST attachment
Common site of avulsion fracture
Apophyses
Common types of fractures in the carpal and tarsal bones
Chip fractures and slab fractures
Alternate name for physeal fractures
Salter-Harris fracture
Patient demographic for physeal fractures
Juvenile patients with open physes
Type 1 physeal fracture
Physeal fracture separating metaphysis and epiphysis
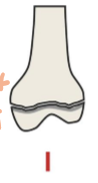
Type 2 physeal fracture
Fracture running through physis and metaphysis

Type 3 physeal fracture
Fracture running through the physis and epiphysis

Type 4 physeal fracture
Combo of 2 and 3, runs from metaphysis through the physis and out the epiphysis

Type 5 physeal fracture
Crushing fracture, prematurely closing the physis

Most common type of Salter-Harris fracture in vet med
Type 2
Hardest physeal fracture to diagnose
Type 5
Most common physeal fracture at the distal humerus
Type 4
Most common site of type 5 fracture and why
Distal ulna because the physis is V shaped
Consequence of a Type 5 physeal fracture at the ulna
Stunted ulnar growth with continued radial growth → cranial bowing of radius
Consequence of a cranially bowed radius
Increased risk of elbow dysplasia
Montagia fracture
Fracture with accompanying luxation