Clin med- cardiac physiology
1/84
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
85 Terms
Where do the coronary arteries arise from and what is their function?
originate from the base of the aorta
function: provide the heart with blood supply (oxygen and nutrients)
When does the heart receive blood?
during diastole when it is relaxing
What are the three types of cardiac cells and their functions?
myocardial (99%)- contraction
specialized conducting cells- allow cells to contract in unison
pacemaker cells (1%)- can initiate depolarization and are autorhythmic
What two arteries supply the SA and AV nodes, and where do they branch from?
SA node artery and AV node artery
Branch off the RCA
What are some properties of cardiac muscle?
single nucleus, semi-spindle in shape, interconnected via gap junctions or intercalated discs, involuntarily controlled
Which wall of the heart is most concerning for an MI?
anterior wall because it is the thinnest and there is the greatest potential for rupture
What is the measurement that tells you how much pressure the LV needs to pump blood into the aorta?
diastolic BP
What is the electrical conduction pathway in the heart?
SA node (primary pacemaker) →
inter-atrial pathway (brings impulse from R atrium to L atrium) & internodal pathway (SA to AV) →
AV node (secondary pacemaker) →
Bundle of His (brings impulse into ventricles) →
R and L bundle branches →
Purkinje fibers (supplies myocardium)
Is conduction velocity faster in the LBB or the RBB?
left b/c left ventricle is much thicker
Which side of the heart pumps more blood?
trick question- both ventricles pump same amount of blood
Why is the left ventricle much thicker than the right ventricle?
left ventricle pumps blood to the whole body while the right ventricle only pumps blood to the lungs
In the heart's conduction pathway, where does the greatest delay occur and why?
From the AV node to the Bundle of His (0.1 sec)
This delay allows the atria to contract and the ventricles to fill, prevents atria and ventricles from contracting at the same time
What are some characteristics of pacemaker cells?
autorhythmic (can initiate AP on their own), coupled to myocytes via gap junctions, no resting membrane potential
What are the typical paces set by the SA node, AV node, and Purkinje fibers?
SA node: 60-100 bpm
AV node: 40-60 bpm (nodal rhythm)
Purkinje: <40 bpm (idioventricular rhythm)
Why is the SA node the primary pacemaker of the heart?
it is the fastest to depolarize and has the highest (least negative) resting membrane potential
Describe SA and AV action potential
Phase 4 (spontaneous depolarization): -60 mV: slow influx of Na+ in via funny channels
-50mV: slow influx of Ca++ in via T channels
-40mV: greater influx of Ca++ via L channels- allows cell to reach threshold (between -40 and -30 mV)
Phase 0 (depolarization): large influx of Ca++ into cell via L channels
Phase 3 (repolarization): outward flux of K+, Ca++ channels inactivated
What are the differences between the action potentials of SA/AV node cells and Purkinje fiber cells?
Na+ vs Ca++ for depolarization
slower rate to reach threshold and lead to an AP (Purkinje fibers start more negative)
Plateau phase in Purkinje fibers
Describe myocyte and Purkinje fiber action potential
Phase 4 (resting potential ~90 mV): influx of K+ exiting
Phase 0 (depolarization): rapid influx of Na+ while K+ channels close
Phase 1: Na+ influx deactivated and slow K+ exiting
Phase 2 (plateau): slow Ca++ entry with K+ exiting
Phase 3 (repolarization): rapid K+ exit and Ca++ inactivated
What is the difference between an absolute and relative refractory period?
absolute- no stimulus no matter how strong will depolarize the myocardial cells
refractory- a sufficiently strong stimulus will depolarize myocardial cells
What are some characteristics of myocytes?
fast response action potentials, NOT autorhythmic, have true resting membrane potential
How much faster is skeletal muscle AP than cardiac muscle AP?
100x faster- 3ms vs 300ms
long AP in cardiac muscle allows heart to relax and refill before it contracts again
What are the effects of sympathetic innervation on the myocardium?
Epinephrine/norepinephrine, adrenergic receptors: increase HR, conduction velocity, and force of contraction
What are the effects of parasympathetic innervation on the myocardium?
Ach, muscarinic receptors: decrease HR, conduction velocity (don't affect force of contraction)
How does a heart transplant affect the innervation of the heart?
lose neural innervations so heart becomes completely reliant on circulating catecholamines to regulate HR, contractility and conduction velocity
Patients with heart transplants need to ease into exercise more slowly and cool down more slowly b/c hormonal influences are slower than neural
In addition to neural innervation, what else affects the heart?
circulating catecholamines- slower than neural input
How does the parasympathetic nervous system influence action potentials?
increases K+ exiting, decreases Ca++ entry, makes resting membrane potential more negative, decreases rate of rise to threshold
HR slows because it takes longer to reach threshold
How does the sympathetic nervous system influence action potentials?
increases Ca++ entry, increase rate of rise to threshold, increases HR because cell can reach threshold faster
When do we get vectors? Which direction do they run?
vectors are created by a difference in charge
they run negative to positive
What does a biphasic wave on an EKG mean?
it means the vector is going 90 degrees from the lead
How do the waves of depolarization or repolarization travel from cell to cell?
via gap junctions
When the vector runs towards a positive electrode you get a ____________ deflection (depolarization)
positive
When the vector runs towards a negative electrode you get a ___________ deflection (repolarization)
negative
How is cardiac muscle different from skeletal muscle? How is it similar?
Different- single nucleus, interconnected (intercalated discs, gap junctions), all or none principle, autorhythmic cells (excites itself), involuntary contraction
Similar- both striated, both contract
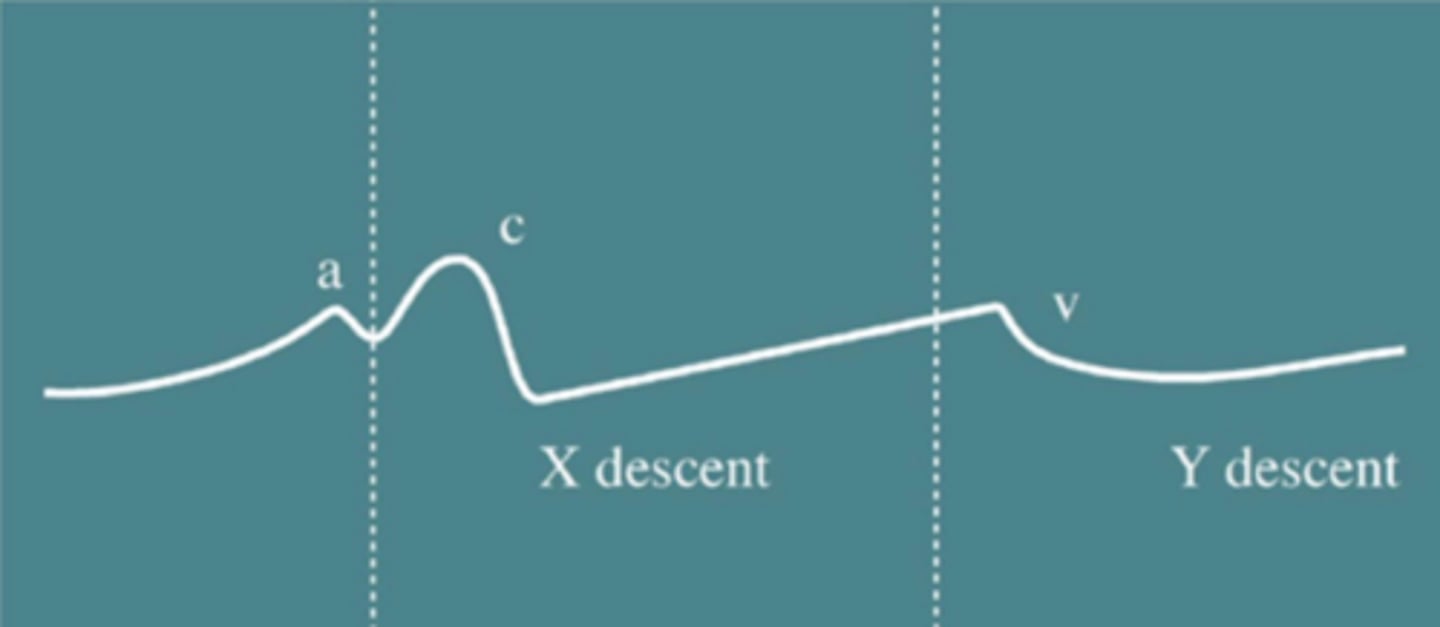
What are the three waves of the atrial pressure curve and what do they mean?
A wave: atrial contraction (occurs during diastole- AV valves are open)
C wave: ventricular contraction, pushes AV valves up into the atrium (occurs during systole- AV valves are closed)
V wave: atrial pressure > ventricular pressure due to passive filling during the diastole phase (AV valves are about to open)
Blood fills into atria during systole when ventricles are contracting (between C and V waves)
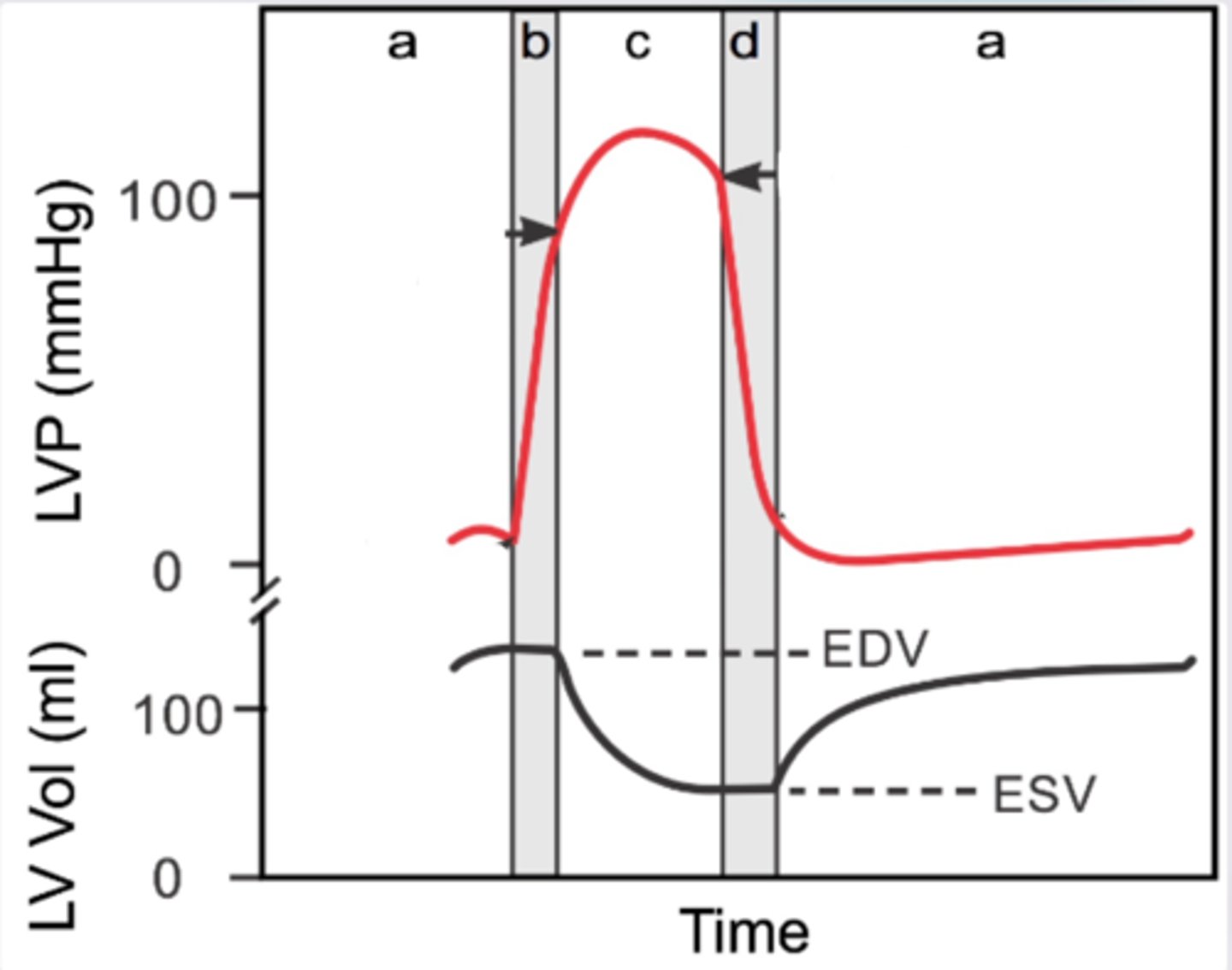
What are the waves of the ventricular pressure curve and what do they mean?
a: diastole- passive ventricular filling, followed by atrial contraction
b: onset of systole- isovolumetric contraction (all valves are closed, heart is squeezing)
c: systole- ventricular contraction (blood ejection)
d: diastole- isovolumetric relaxation (all valves are closed)
What pressure opens the aortic valve?
Systolic pressure (peak pressure about 120 mmHg)
What does the dicrotic notch represent?
when the aortic pressure is greeater than the ventricular pressure- pressure in aorta jumps slightly because blood is trying to come back to the heart → closes aortic valve
How does aortic stenosis affect aortic pressure?
tight valve= difficult to get blood out= pressure will be much lower
What is a consequence of aortic regurgitation?
leaky valve= blood going back into L ventricle= develop L ventricle hypertrophy= puts strain on heart muscle
What is normal end diastolic volume (blood stored in LV normally)?
120 mL
What are the waves of the LEFT ventricular pressure curve and what do they mean?
a: diastole (peak end diastolic volume)
b: systole (isovolumetric contraction; no change in ventricular volume)
c: ventricular contraction (ventricular volume reduced- end systolic volume ~50mL)
d: diastole (isovolumetric relaxation; no change in ventricular volume)
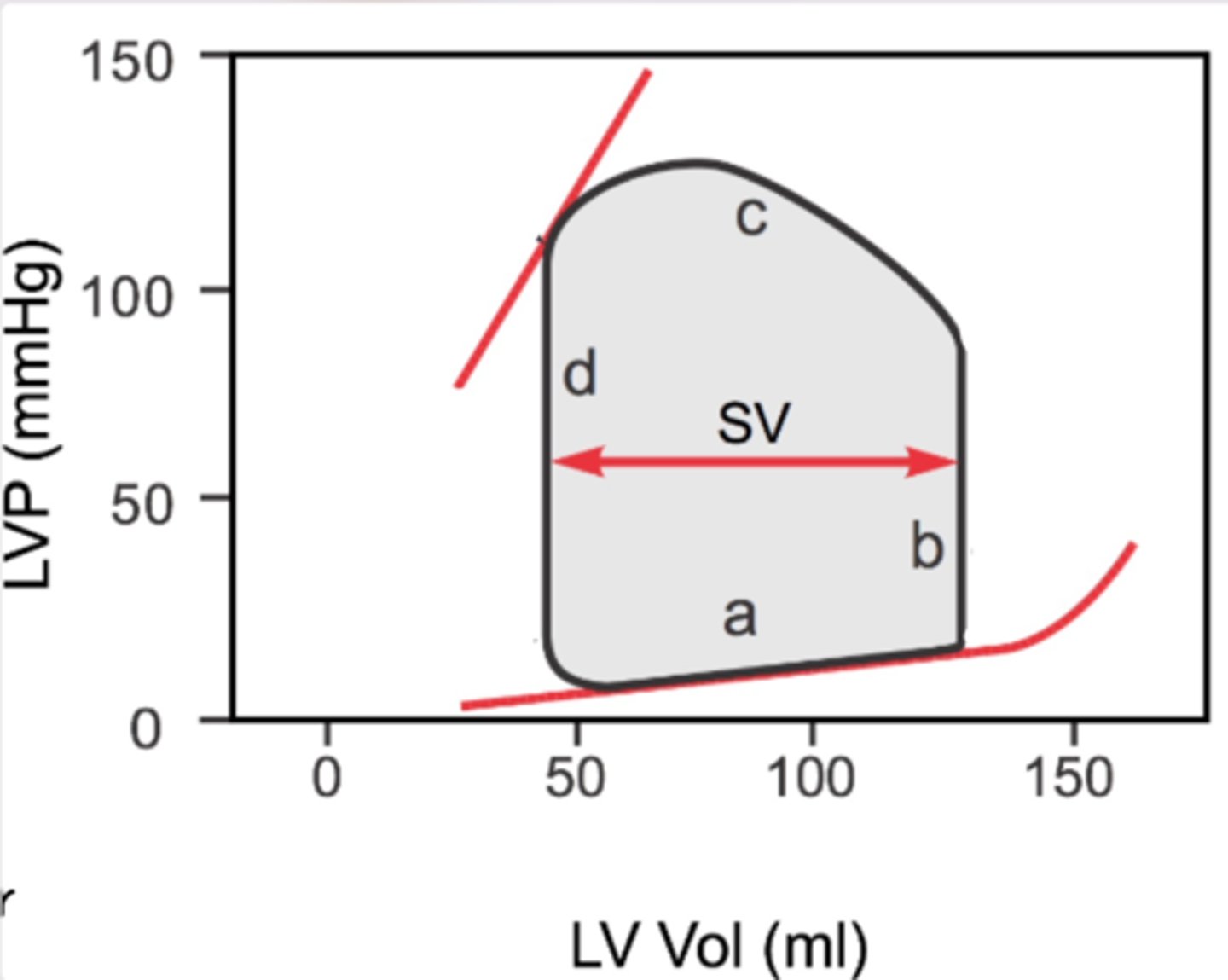
What is stroke volume? How is it calculated?
the volume of blood pumped out of the L ventricle during each systolic cardiac contraction
SV= end diastolic volume - end systolic volume
What happens if you decrease heart compliance?
increase LV pressure and LV volume
If LV volume increases, what happens to pressure?
Pressure also increases
What do S1 and S2 represent?
S1- closure of AV valves (onset of ventricular contraction)
S2- closure of semilunar valves (onset of ventricular relaxation)
What is S4?
heard at end of diastole, due to forceful atrial contraction in a stiff or hypertrophic ventricle (atrial gallop)
What is S3?
heard at beginning of diastole - associated with heart failure (ventricular gallop)
When are extra heart sounds heard in the following conditions:
aortic stenosis
mitral regurgitation
aortic regurgitation
mitral stenosis
aortic stenosis- systole (S1 and S2 blend together)
mitral regurgitation- systole
aortic regurgitation- diastole
mitral stenosis- diastole
How is cardiac output calculated? What is resting CO and how can it change with exercise?
HR x SV. Resting= ~5L/min
During exercise, cardiac output can increase up to ~20-25 L/min
How do you calculate max HR?
220-age
Why does stroke volume reach its maximum at ~50% of maximum exertion and drop off at higher heart rates?
filling time decreases
What are some variables that increase heart rate?
decreased parasympathetic tone
increased sympathetic tone
Bainbridge reflex (atrial reflex - baroreceptors detect pressure in atrium and respond to increased pressure (vol) by increasing HR)
What are some variables that increase stroke volume?
increased sympathetic tone (increases contractility)
increased circulating catecholamines
increased preload (venous return) leads to increase in contractility
decreased afterload (resistance for heart to overcome) due to decrease in arterial resistance - heart doesn't have to work as hard
What is preload?
also known as the left ventricular end-diastolic pressure (LVEDP), it is the amount of ventricular stretch at the end of diastole
What is afterload?
also known as the systemic vascular resistance (SVR), it is the amount of resistance the heart must overcome to open the aortic valve and push the blood volume out into the systemic circulation
What are things that can increase venous return?
1. skeletal muscle pump
2. respiratory and abdominal pump (engaging these muscles increases preload)
3. venoconstriction (sympathetic tone)
What are things that inhibit venous return?
1. hydrostatic pressure due to gravity
2. incompetent venous valves- decreased pressure gradient
What is the Frank Starling mechanism?
ability of the heart to change its force of contraction and therefore stroke volume in response to changes in venous return
How does increased venous return lead to increased stroke volume?
Increased venous return= increased ventricular filling (end-diastolic volume)= increased preload
Myocyte stretching increases the sarcomere length= increase in force generation/contractility and enables the heart to eject the additional venous return= increased stroke volume
After a point, why is it that increased volume results in decreased force/contractility?
Overstretching of muscle fibers means less cross bridges can form
What are extrinsic controls of stroke volume?
sympathetic/parasympathetic neural innervation
How is ejection fraction calculated?
EF%= (EDV - ESV/EDV) x 100
What is a normal ejection fraction measurement? What levels are concerning?
Normal range: 55-70%
Less than 40%: may confirm diagnosis of heart failure
<35%: patient may be at risk of life-threatening irregular heartbeats
How does the myocardium increase oxygen supply to meet metabolic needs?
Increased adenosine
Endothelial derived releasing factor (smooth muscle relaxes)- ↑NE, ↓O2 and ↑sheer stress → ↑NO, ↑vasodilation
Sympathetic tone → vasodilation
How does atherosclerosis compromise blood flow?
artery loses ability to vasodilate, also blocks blood flow throughout artery
When does atherosclerosis usually cause symptoms?
when blockage is ≥70%
What happens if a plaque ruptures?
acute thrombic event → immediate occlusion
Which is longer- systole or diastole?
Diastole- 2/3 the time of systole
What happens if resting cardiac output cannot be attained?
excessive increase of sympathetic tone
increased vasoconstriction
increased venous return
decreased kidney filtration
increased fluid retention
increased RA pressure
How do we calculate MAP? What is its significance?
MAP= diastolic pressure + 1/3 pulse pressure
this is the driving force of blood flow through the capillaries
What are the variables that contribute to resistance to blood flow?
1. viscosity of the blood (thicccccness)
2. length of the blood vessel
3. diameter of the blood vessel
What wall is opposite the inferior wall?
Lateral wall
Is the pressure in the atrium low or high?
low
What is cardiac output?
amount of blood pumped from the heart in one minute
What is blood pressure?
the force that the blood exerts against the walls of the arteries as it passes through them
equals cardiac output times peripheral vascular resistance
What is ejection fraction?
% of EDV ejected from the heart per cardiac cycle
Describe the following components during mid-late ventricular diastole: atrial vs. vent pressure
arterial vs. vent pressure
AV valves
semilunar valves
atrial > ventricular pressure
arterial > ventricular pressure
AV valves: OPEN
Semilunar valves: closed
Describe the following components during isovolumetric contraction (systole):
atrial vs. vent pressure
arterial vs. vent pressure
AV valves
semilunar valves
atrial < ventricular pressure
arterial > ventricular pressure
AV valves: closed (S1)
semilunar valves: closed
Describe the following components during ventricular ejection (systole):
atrial vs. vent pressure
arterial vs. vent pressure
AV valves
semilunar valves
atrial pressure < ventricular pressure
arterial < ventricular pressure
AV valves: closed
semilunar valves: OPEN
Describe the following components during isovolumetric relaxation (early diastole):
atrial vs. vent pressure
arterial vs. vent pressure
AV valves
semilunar valves
atrial pressure < ventricular pressure
arterial > ventricular pressure
AV valves: closed
semilunar valves: closed (S2)
What fraction of deaths are associated with heart disease and stroke?
one third
How much does heart disease cost the healthcare system a year?
$214.5 billion/year
What percentage of coronary artery disease and stroke account for male and female death?
80% males, 75% female
What is the primary cause of CAD and stroke?
atherosclerosis
What percentage of CVD is preventatable?
80%- obesity, diabetes, hyperlipidemia, hypertension, smoking, sedentary, inflammation