12 lead interpretation
1/82
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
83 Terms
Sodium
Flows into the cell to initiate depolarization
Potassium
Flows out of the cell to initiate repolarization
decreased or increased levels of potassium result in the following:
hypokalemia- increased myocardial irritability
hyperkalemia- decreased automaticity/ conduction
Calcium
Has a critical role in depolarization of the pacemaker cells (maintains depolarization) and in myocardial tractility (involved in the contraction of heart muscle tissue)
decreased or increased levels of calcium result in the following:
hypocalcemia: decreased contractility and increased myocardial irritability
hypercalcemia: increased contractility
Magnesium
Stabilizes the cell membrane; acts in concert with potassium and opposes the actions of calcium
decreased or increased levels of magnesium result in the following:
hypomagnesemia: decreased conduction
hypermagnesemia: increased myocardial irritability
P wave
Depolarization of the atria
P-R interval
Depolarization of the atria and the delay at the AV junction
QRS Complex
Depolarization of the ventricles and repolarization of the atria
ST segment
Period between ventricular depolarization and beginning of repolarization
T wave
Ventricular repolarization
R-R interval
Time between two successive ventricular depolarizations
Autonomic nervous system

§The parasympathetic nervous system
§Concerned primarily with vegetative functions
§Sends messages primarily through the vagus nerve
§Rest and digest nervous system
§Vagus stimulation
§Acetylcholine (ACh) signals SA node, slowing heart
§Atropine opposes ACh effect
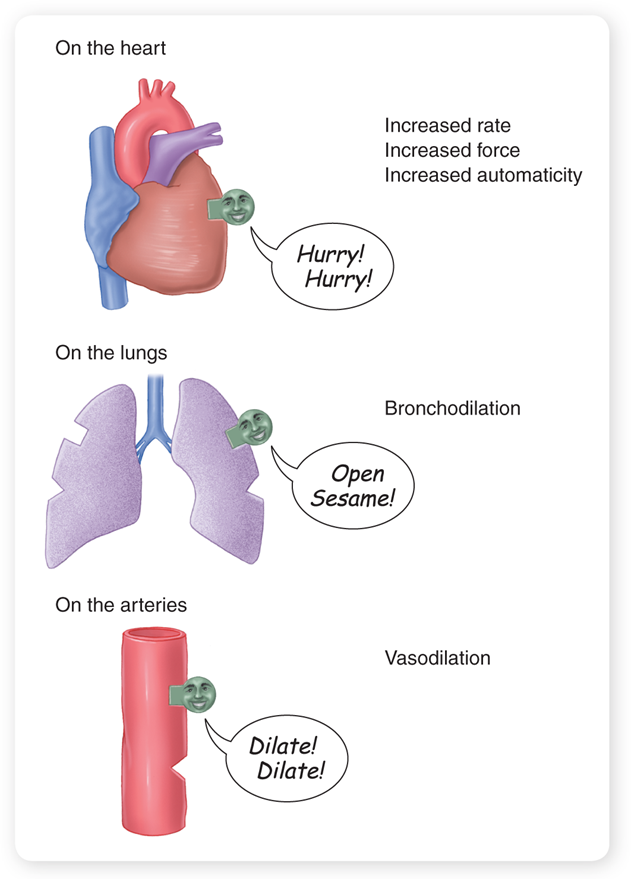
§The sympathetic nervous system
§Prepares the body to respond to various stresses
§Fight or flight
§Increases heart rate
§Strengthens the force of cardiac muscle contractions
§Provides other adaptive responses
§Norepinephrine
§Epinephrine
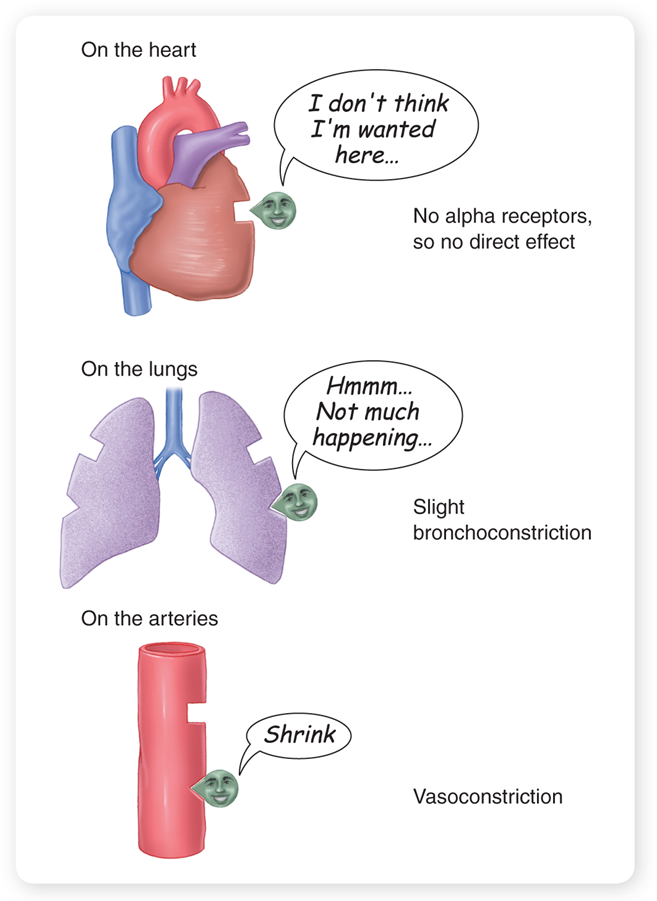
receptors
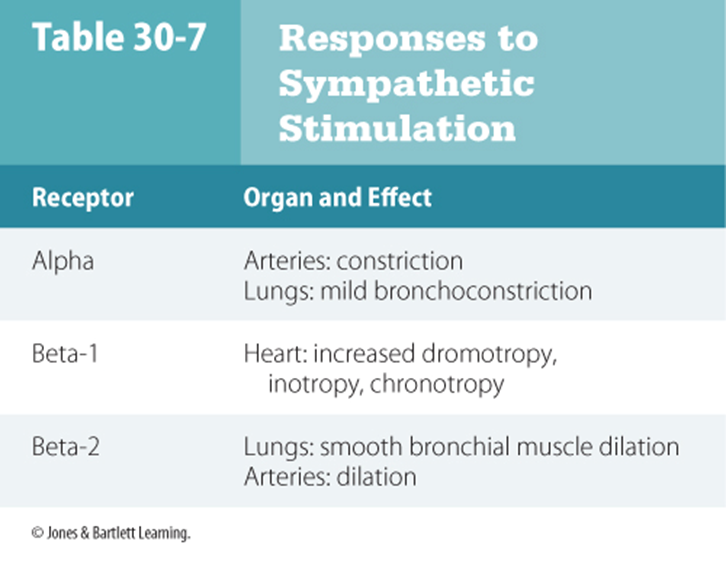
Beta Agents
Alpha Agents
Normal Sinus rhythm

Sinus bradycardia
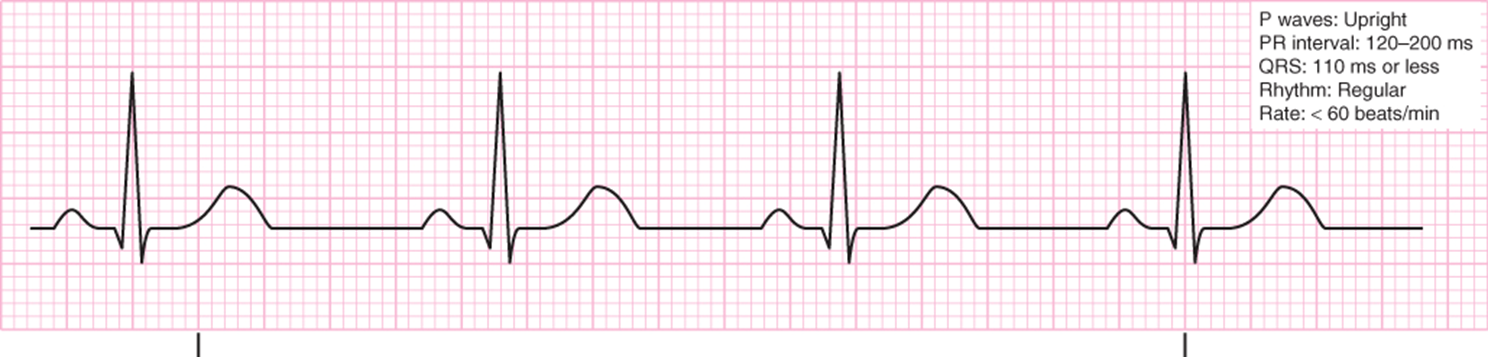
Treatment focuses on patients tolerance to
§Sinus tachycardia

§Sinus dysrhythmia

§Sinus arrest
§Sick sinus syndrome
§Encompasses a variety of rhythms that involve a poorly functioning SA node and is common in older patients
§Announces itself in many ways
§Patients may remain asymptomatic or they may experience a syncopal or near-syncopal episode, dizziness, and palpitations.
§Atrial rhythms
§Any area of the atria may originate an impulse.
§Some rhythms originating from the atria produce upright P waves that precede each QRS complex, but they are not as well rounded as those generated by the SA node.
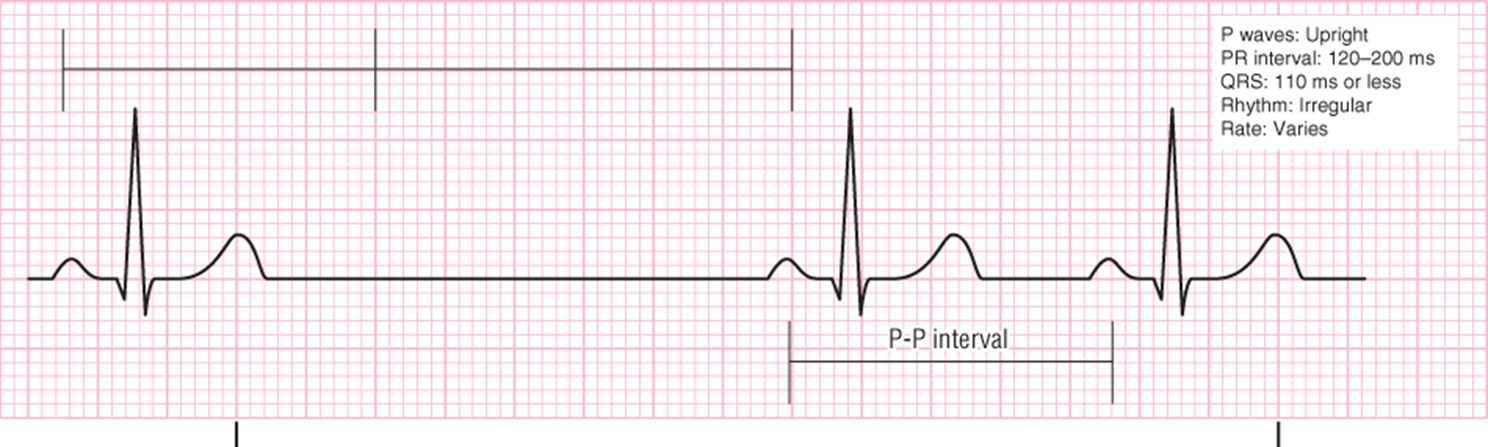
§Wandering atrial pacemaker
§Treatment is usually not indicated in the prehospital setting.

§Premature atrial complex

§When frequent, treatment is focused on correcting underlying cause.
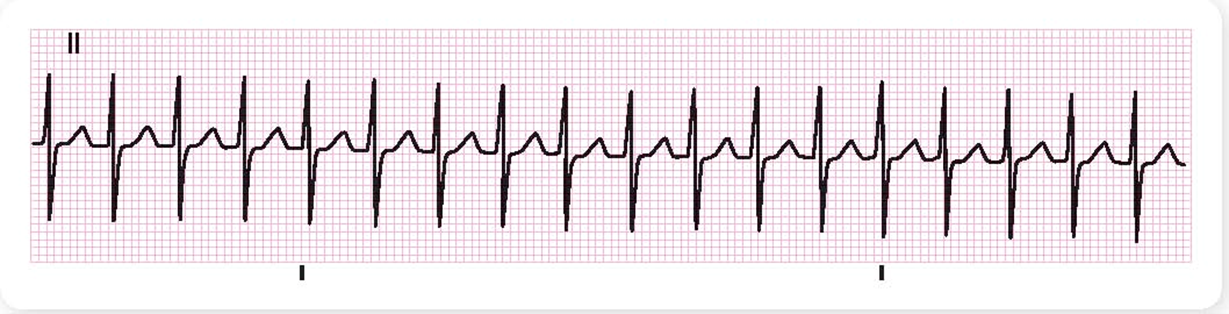
§Supraventricular tachycardia
§Atrial flutter
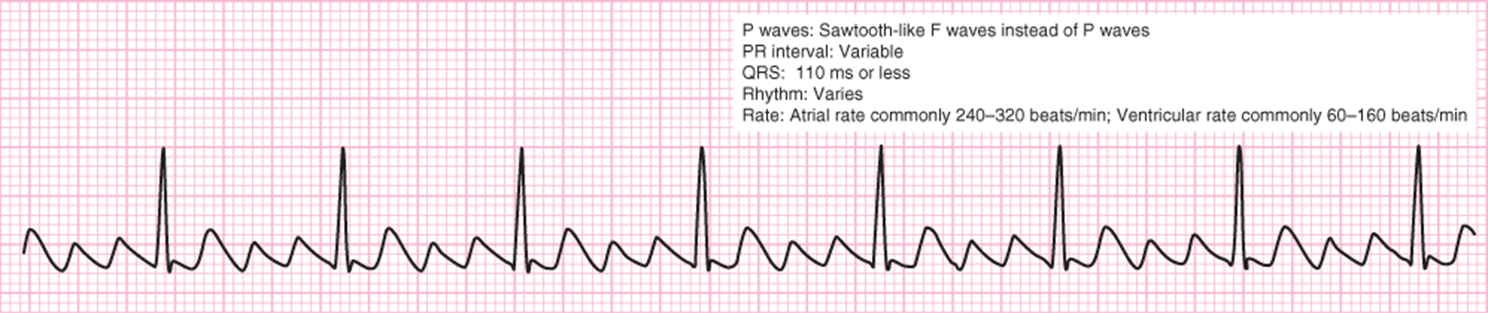
§Medication or electrical cardioversion
§Atrial fibrillation

§Prehospital treatment is usually limited to supportive care.
§Multifocal atrial tachycardia

§Treatment is usually deferred until arrival at the ED.
AV-nodal reentrant tachycardia and AV reciprocating tachycardia
Regular, narrow, complex tachycardias without obvious P waves preceding every complex
Often termed PSVT (paroxysmal)
AVNRT is the most common
AVRT is a similar-appearing tachycardia that results from an accessory pathway.
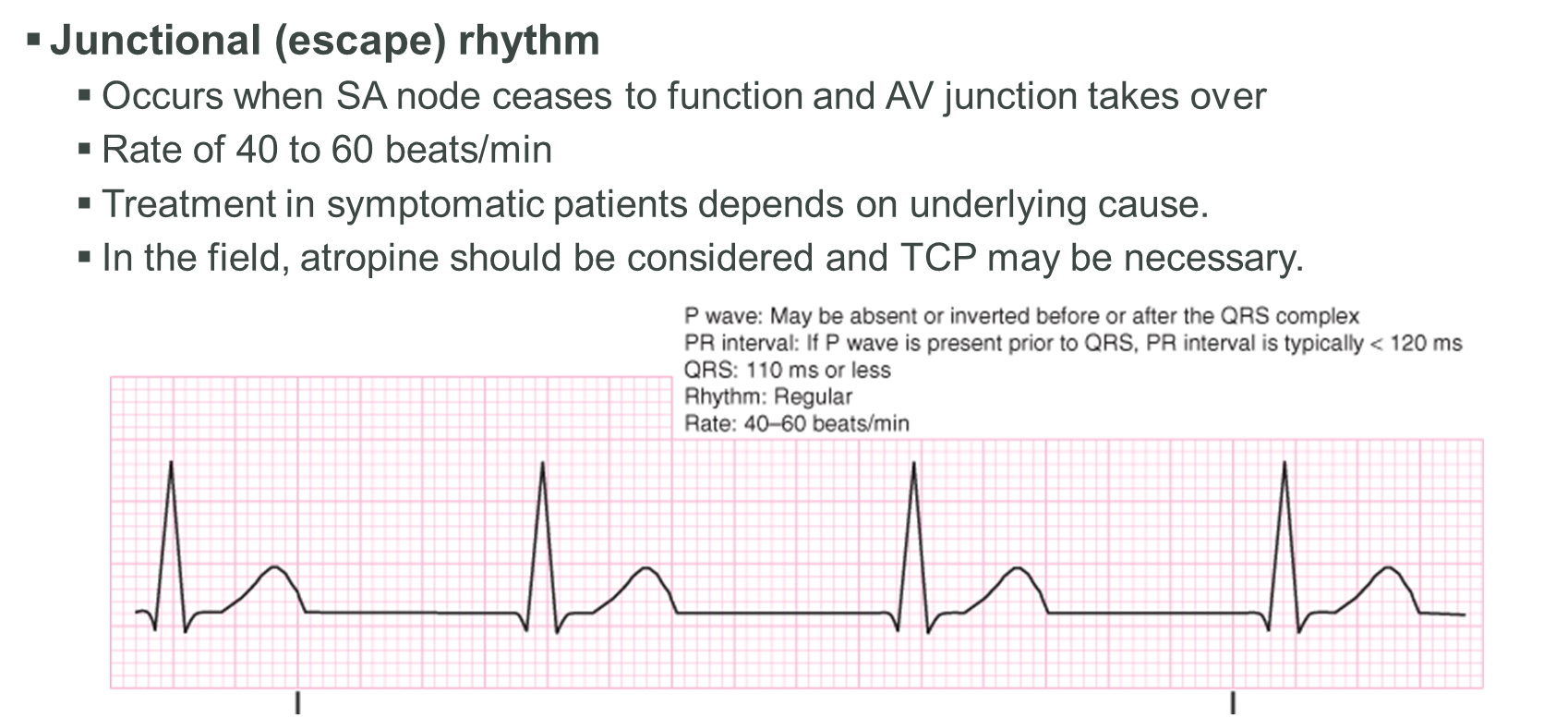
Junctional (escape) rhythm
In the field, atropine should be considered and TCP may be necessary.
Accelerated junctional rhythm

Seldom requires treatment in the prehospital setting (but should be monitored)
Junctional tachycardia
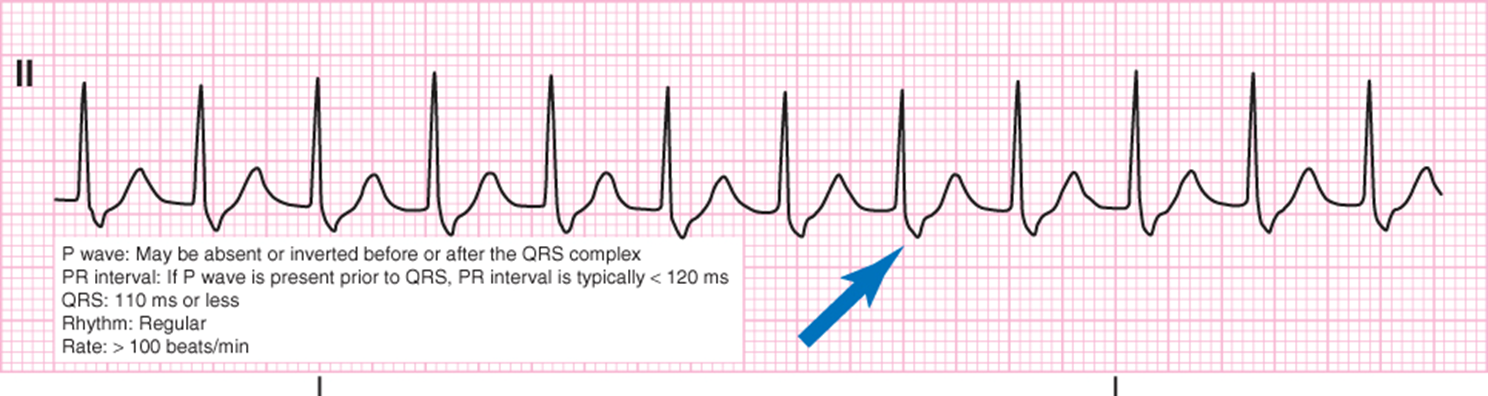
Premature junctional complex

Rarely treated in the prehospital setting
§First-degree AV block

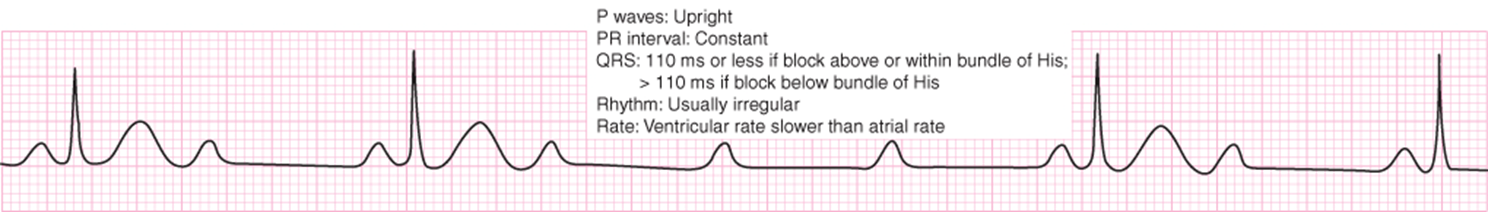
§Second-degree AV block: Mobitz type 1 (Wenckebach)

Second-degree AV block: Mobitz type II (Classical
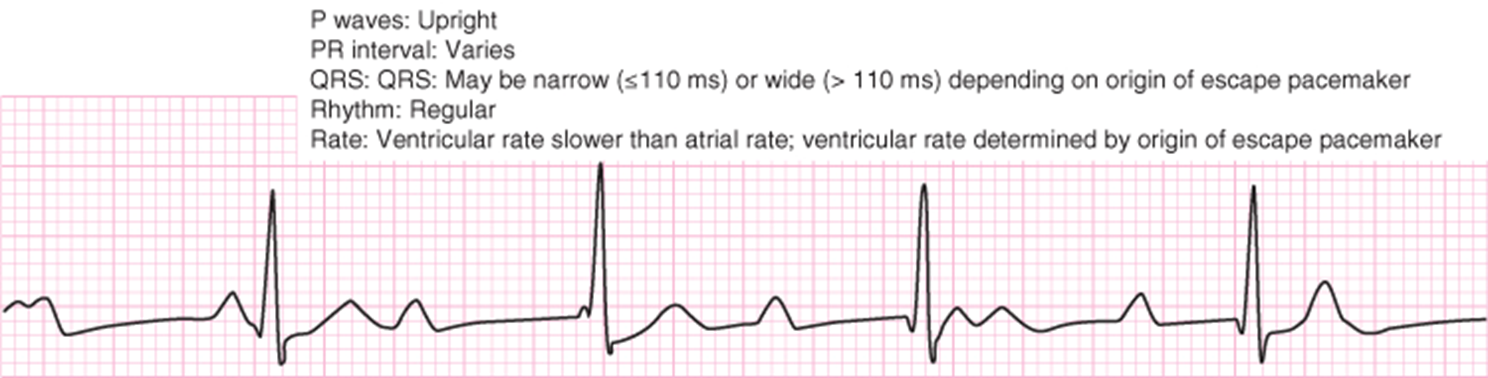
§Third-degree AV block (complete AV block)
§Idioventricular rhythm
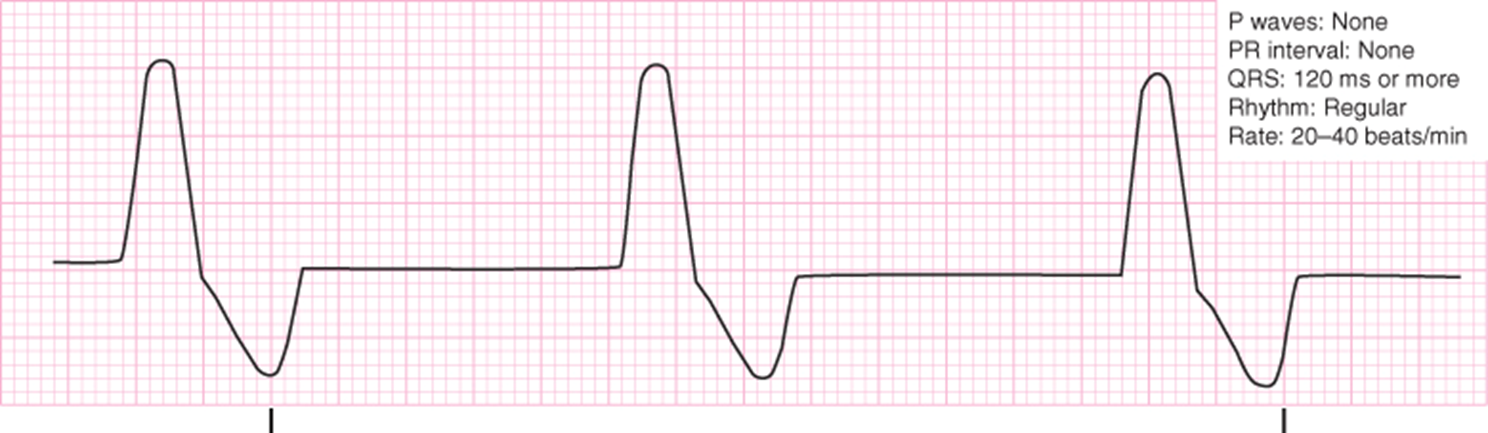
§Accelerated idioventricular rhythm

§Ventricular tachycardia

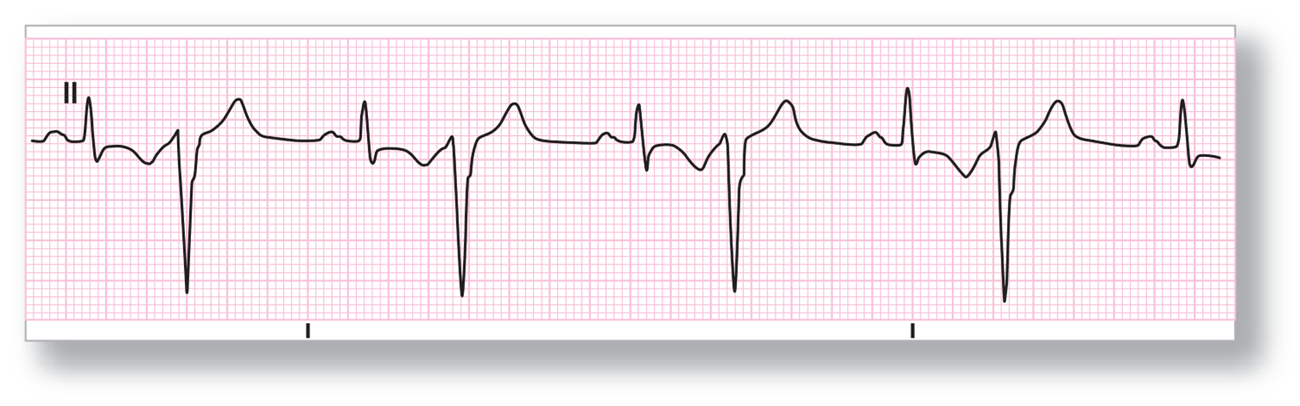
Premature ventricular complex (PVC)
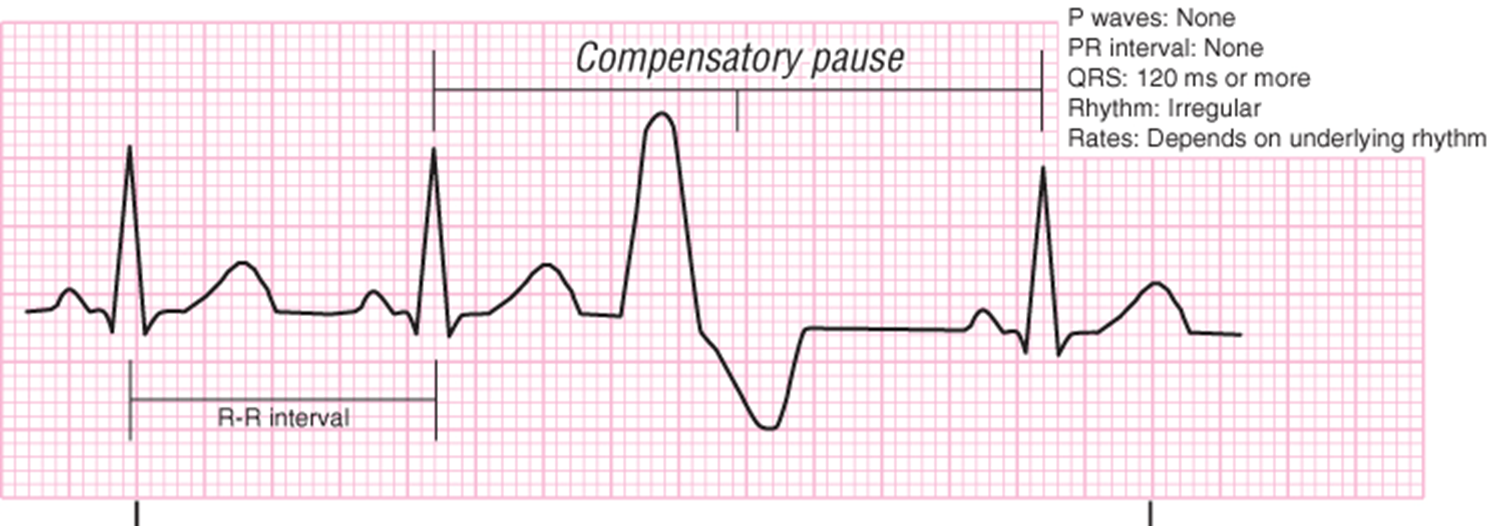
§Unifocal premature ventricular complexes
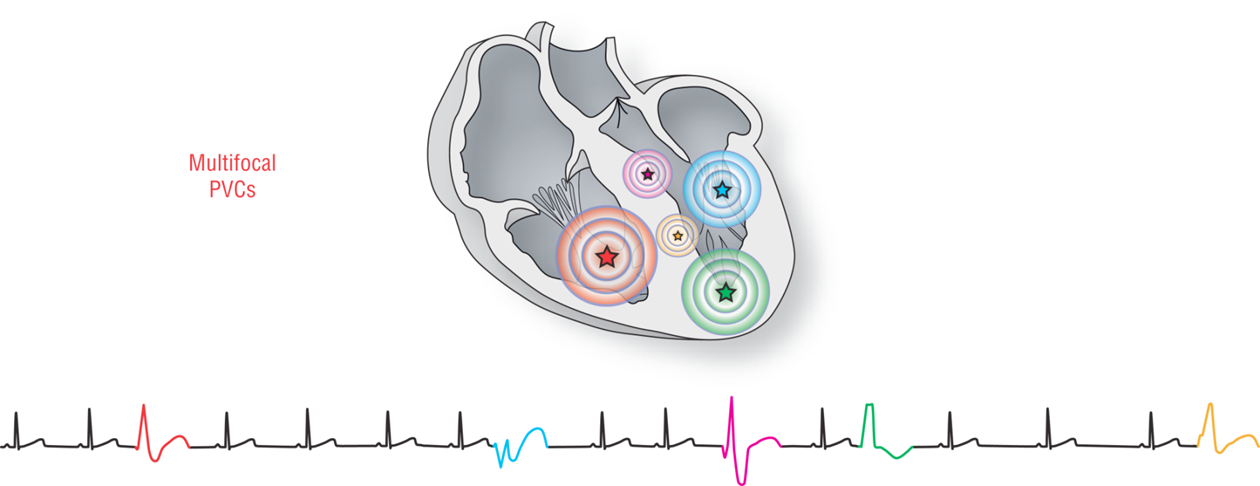
Premature ventricular complex- Multifocal
Premature ventricular complex
Couplet
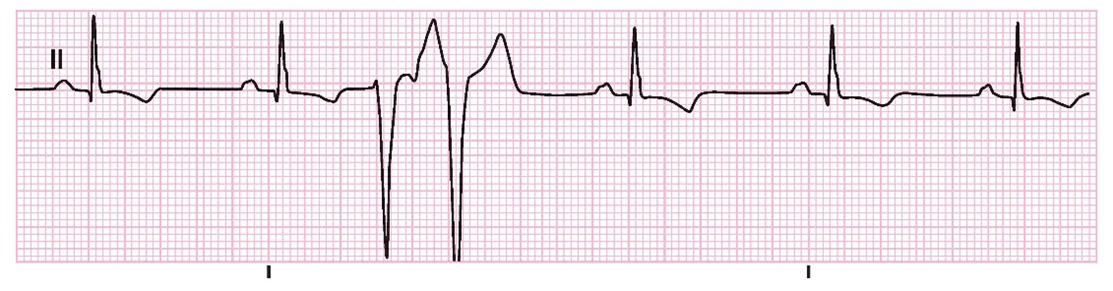
Premature ventricular complex
Bigeminy, Trigemini
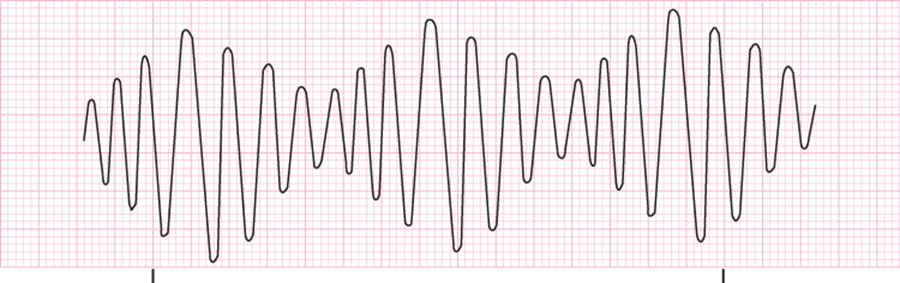
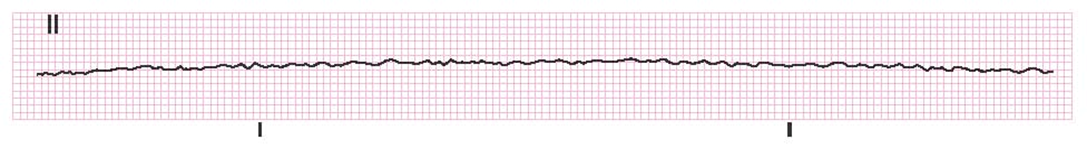
§Ventricular fibrillation (VF)
Rhythm in which the entire heart is no longer contracting
Quivering without organized contraction
Random depolarization of many cells
Rhythm most commonly seen
Responds well to defibrillation
Chest compressions help make the heart more susceptible to defibrillation.
§Ventricular fibrillation (VF)
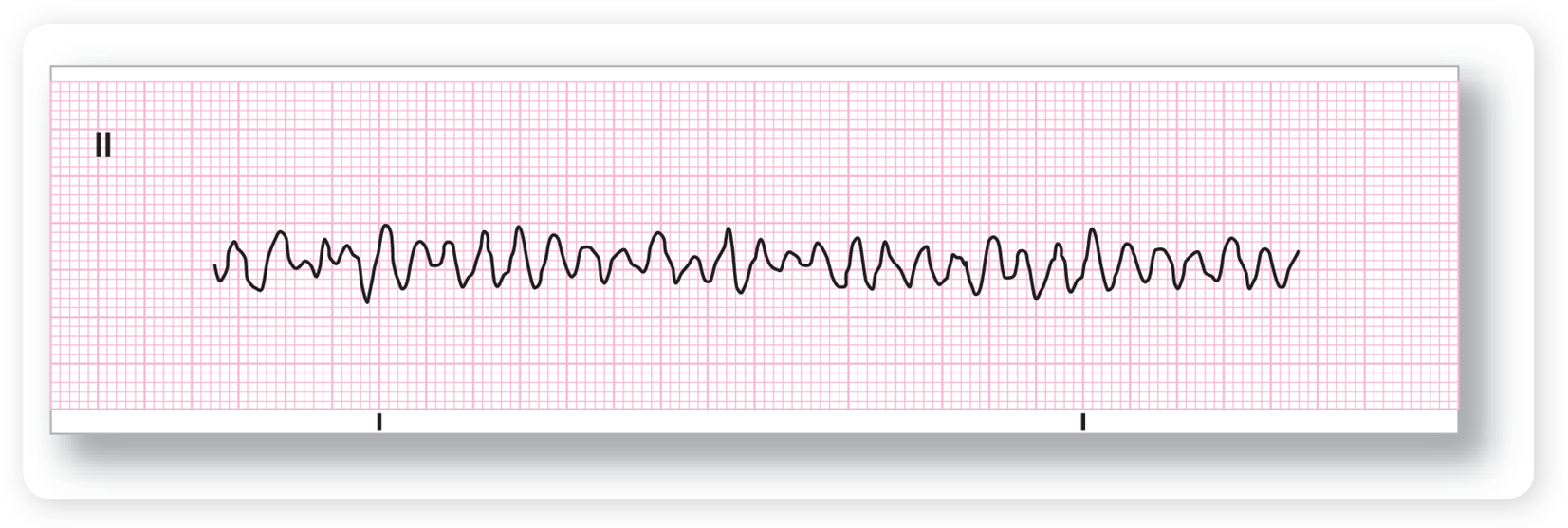
§Ventricular fibrillation (VF)
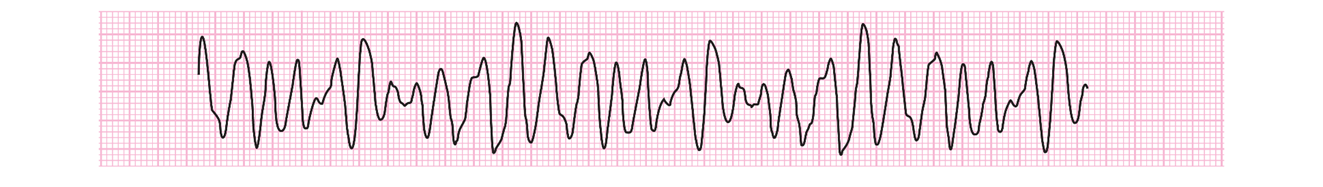
§Ventricular fibrillation (VF)
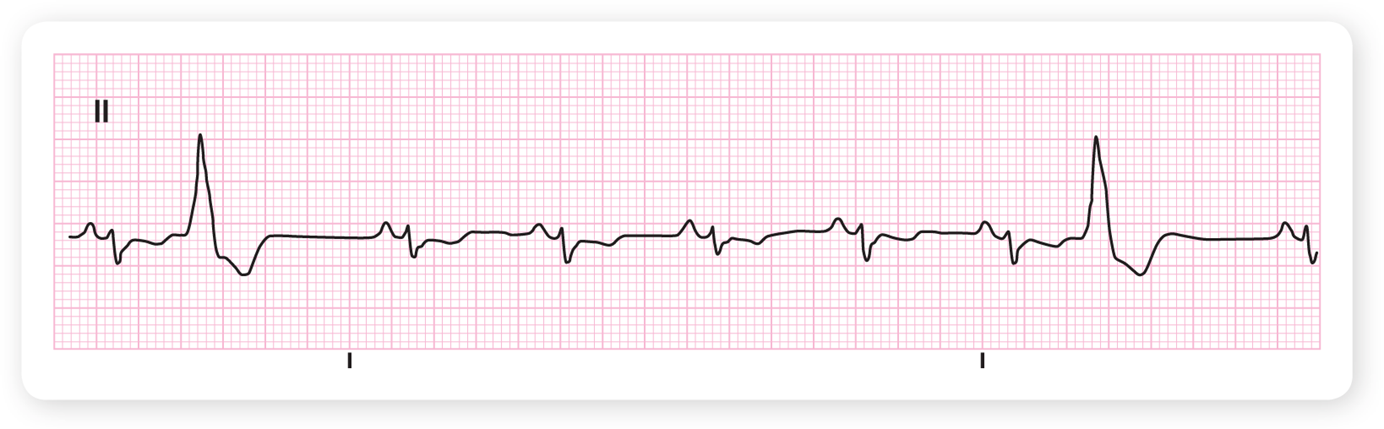
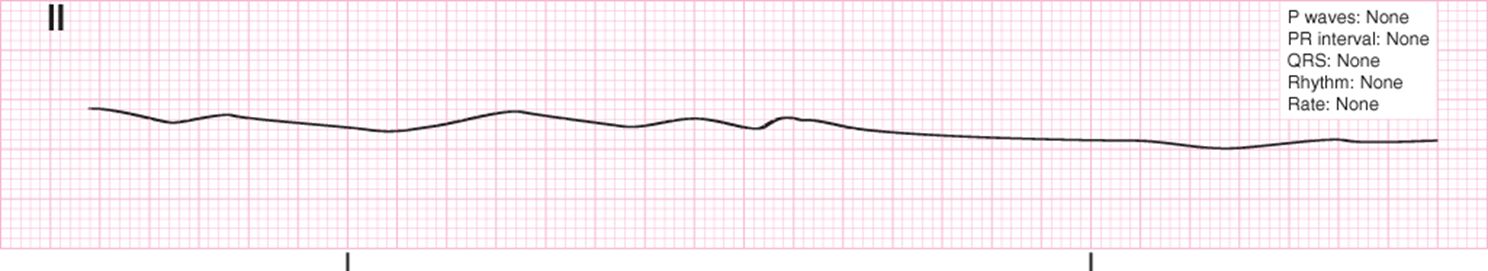
§Asystole
Paced Rhythms
Many types exist.
Ventricular pacemakers are attached to the ventricles only.
Demand pacemakers
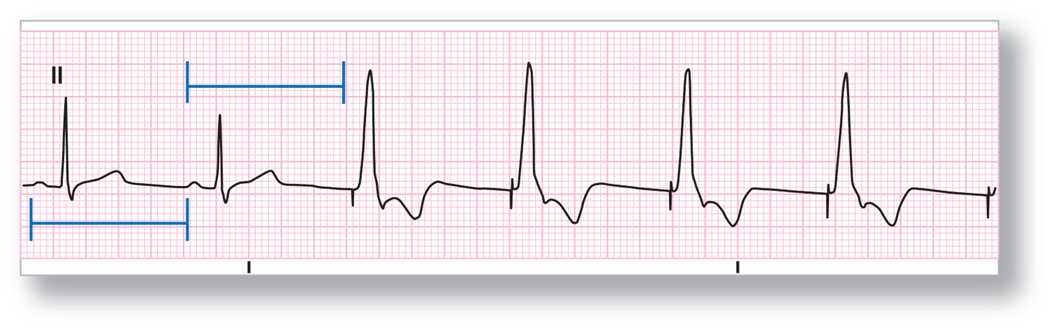
§Artificial pacemaker rhythms
§Artificial pacemaker rhythms
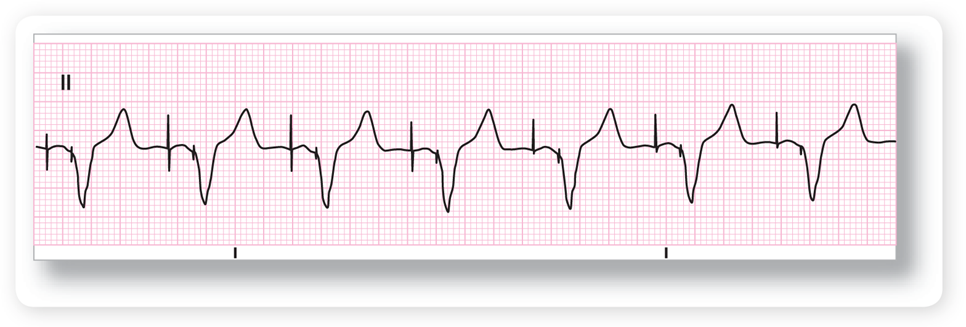
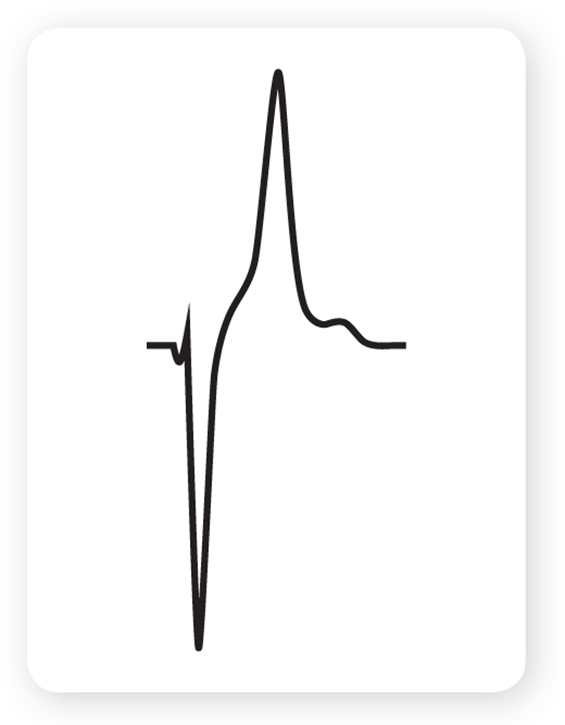
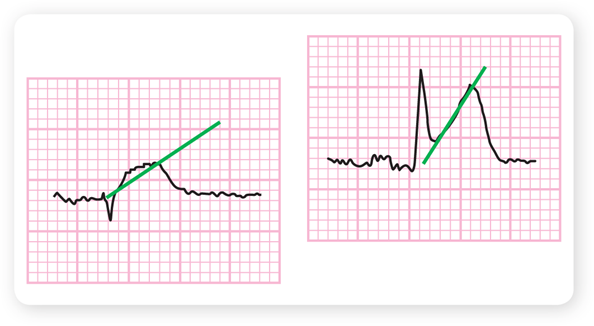
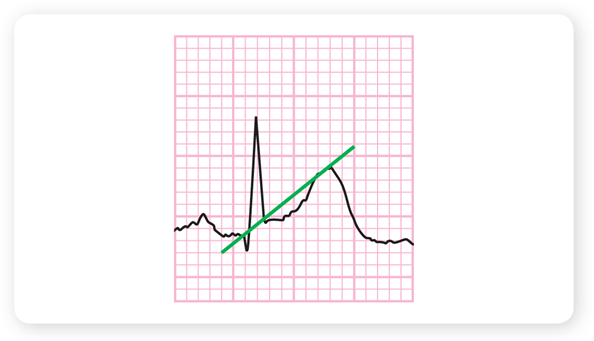
§Delta wave
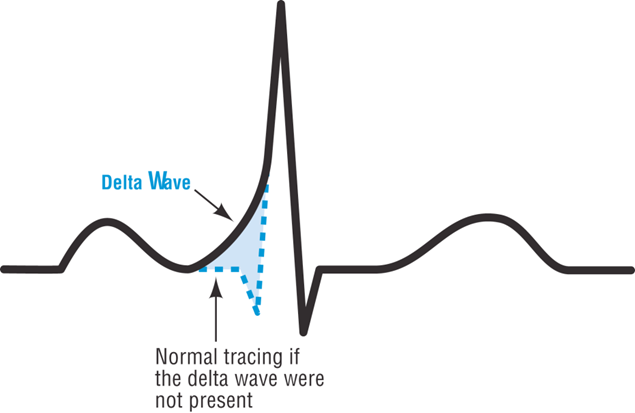
atrial fibrillation with Wolff-Parkinson-White syndrome
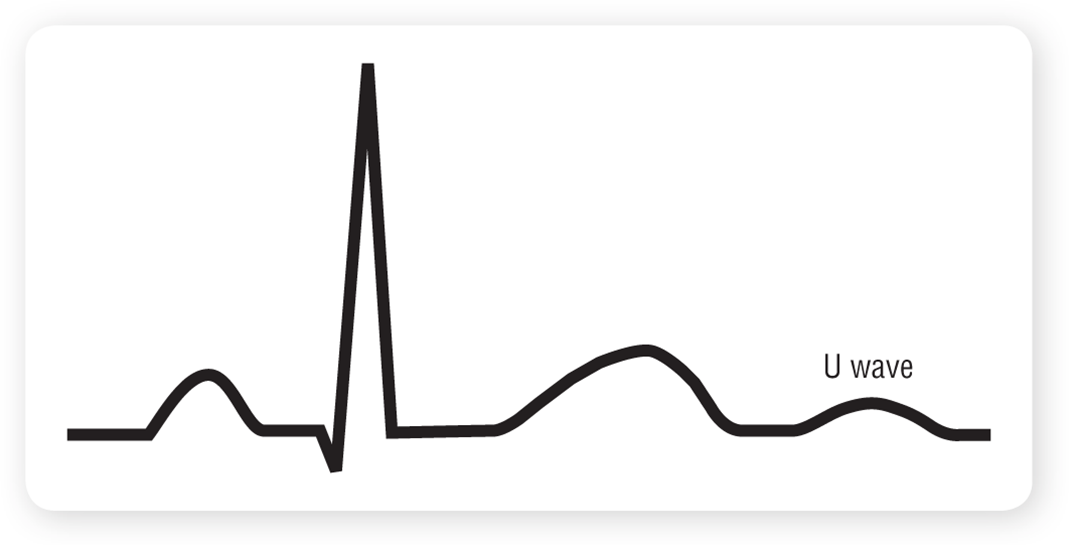
§Osborne (J) wave
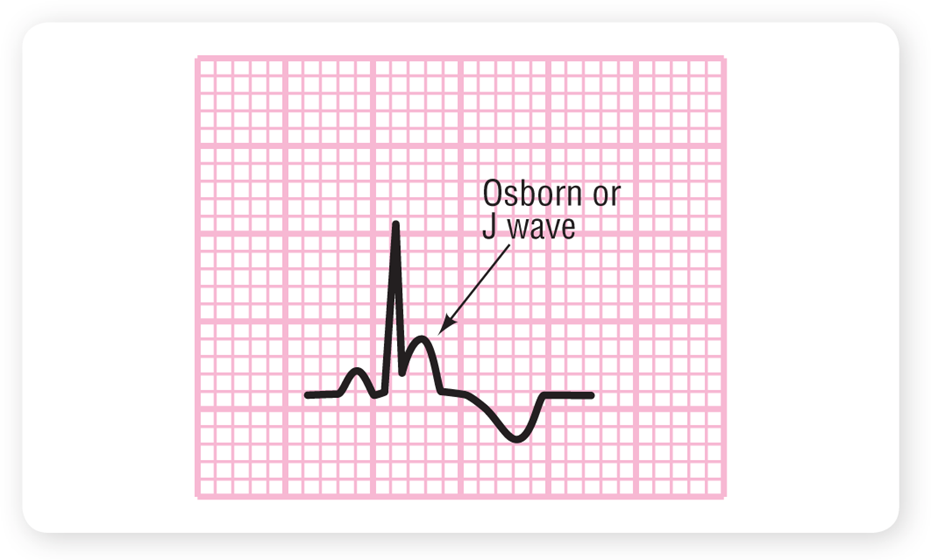
primarily caused by hypothermia
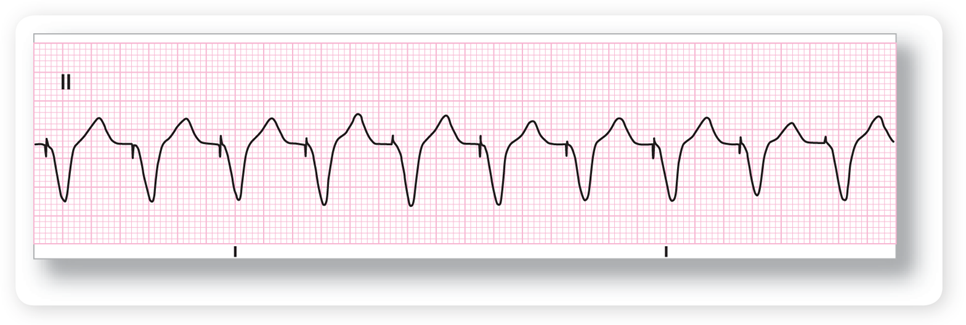
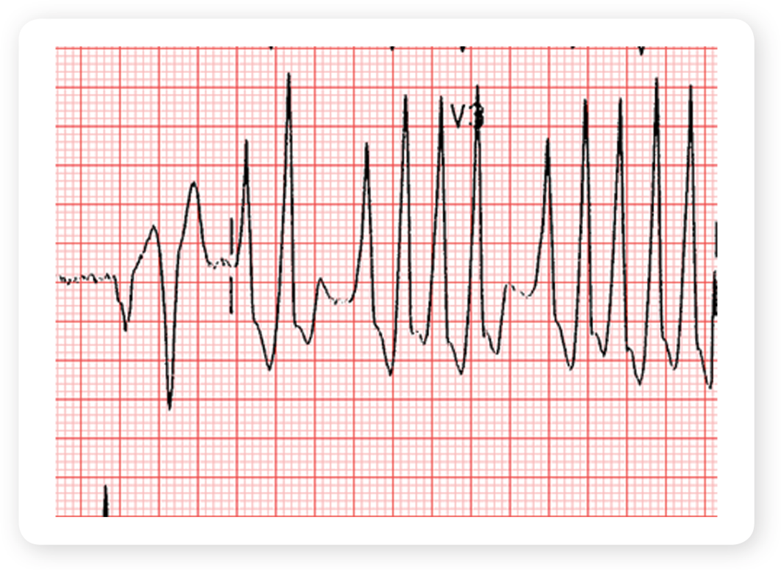
§Hyperkalemia on an ECG
Profound, severe hyperkalemia
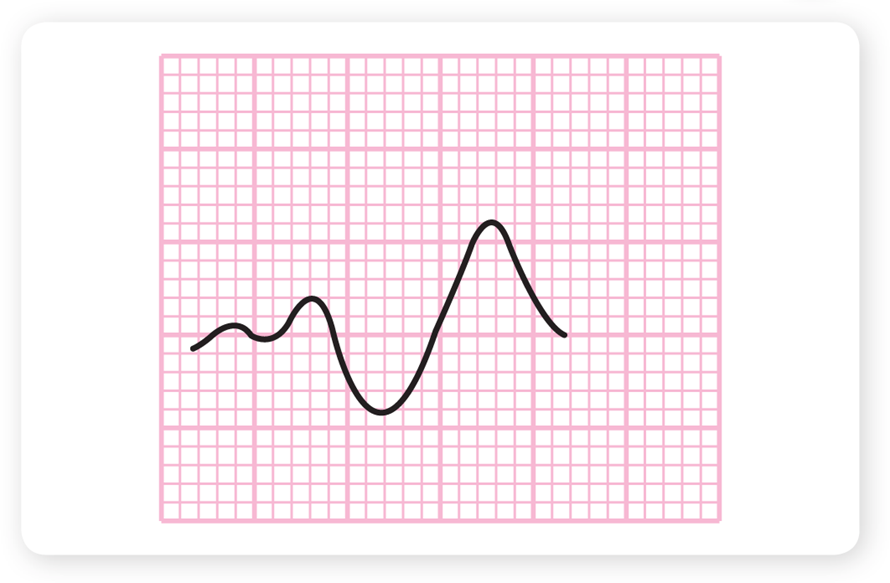
Hypokalemia
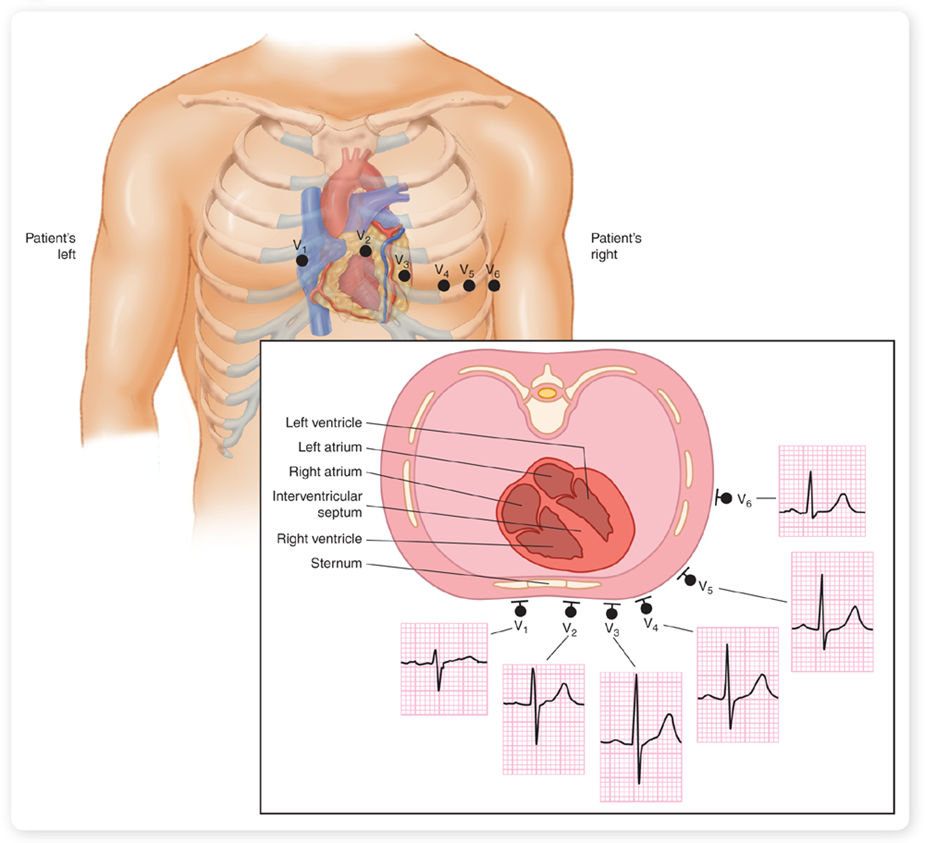
ECG Leads record
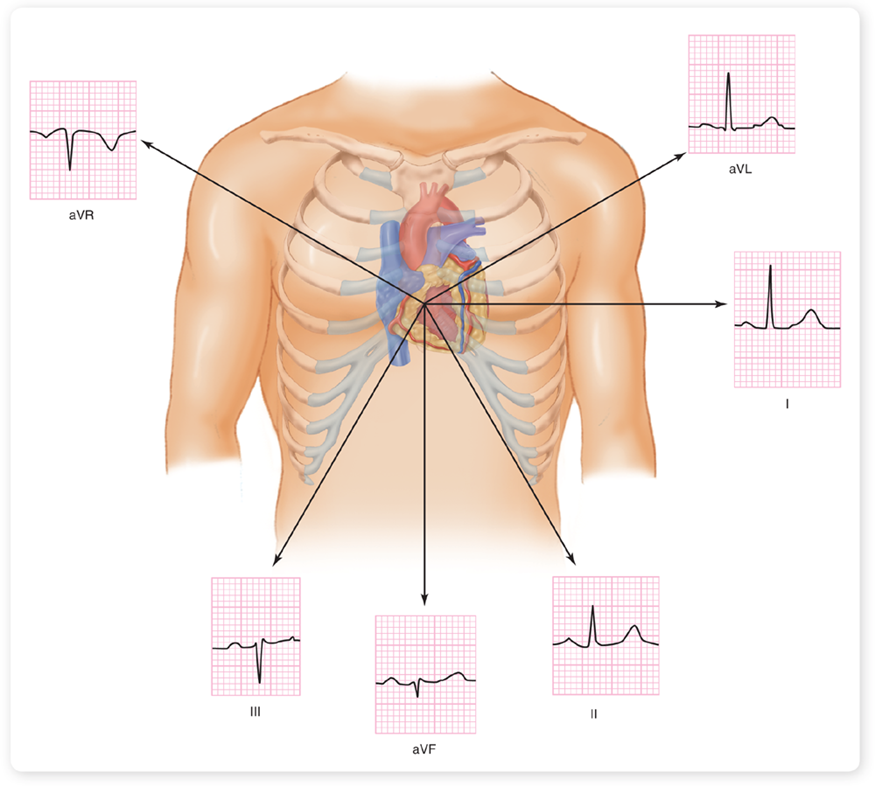
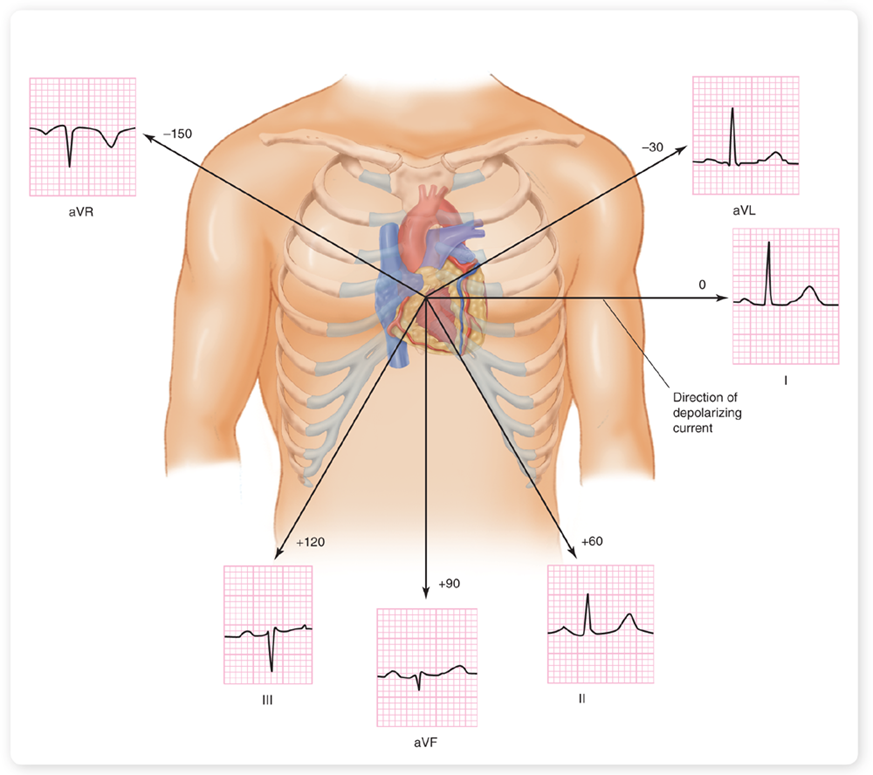
Leads look at
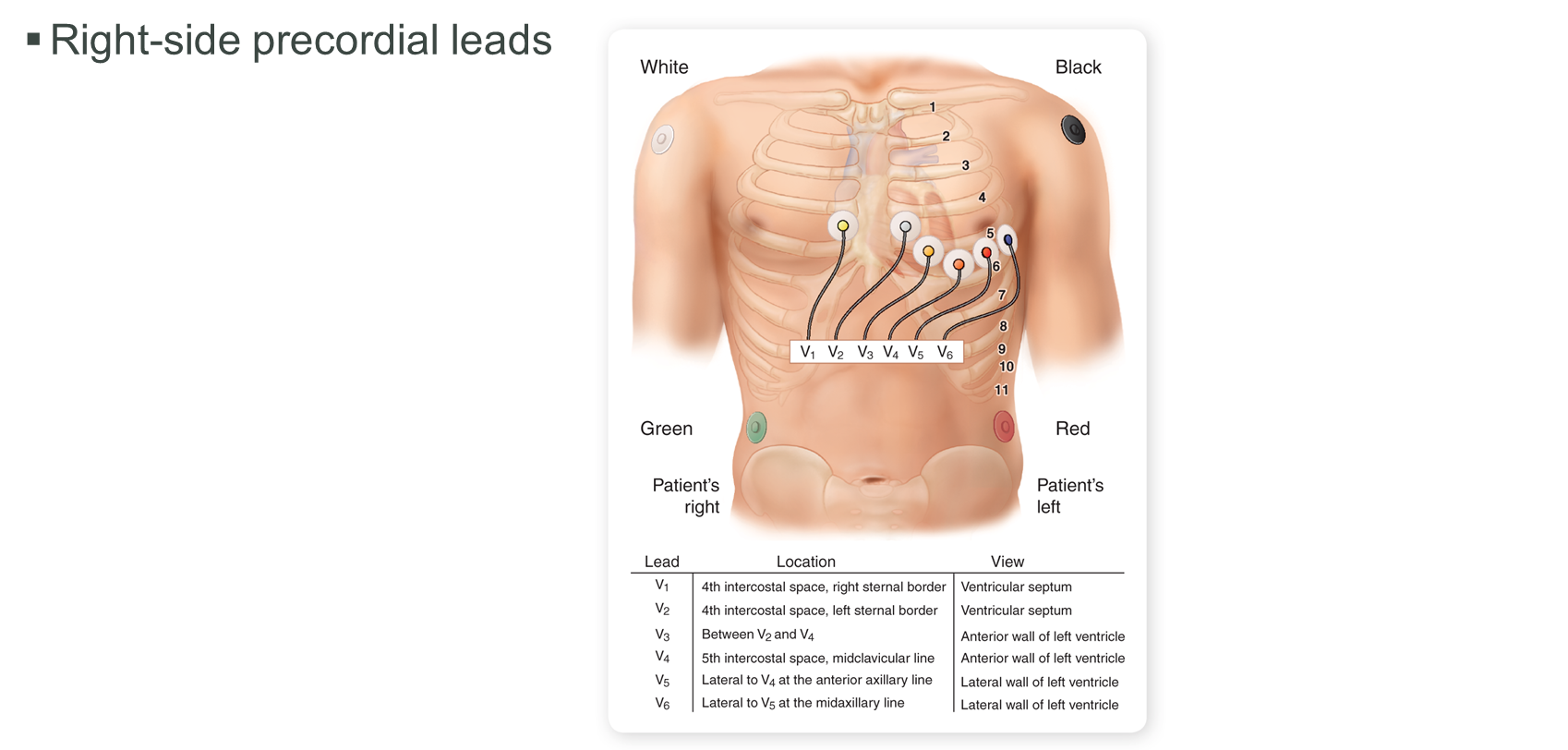
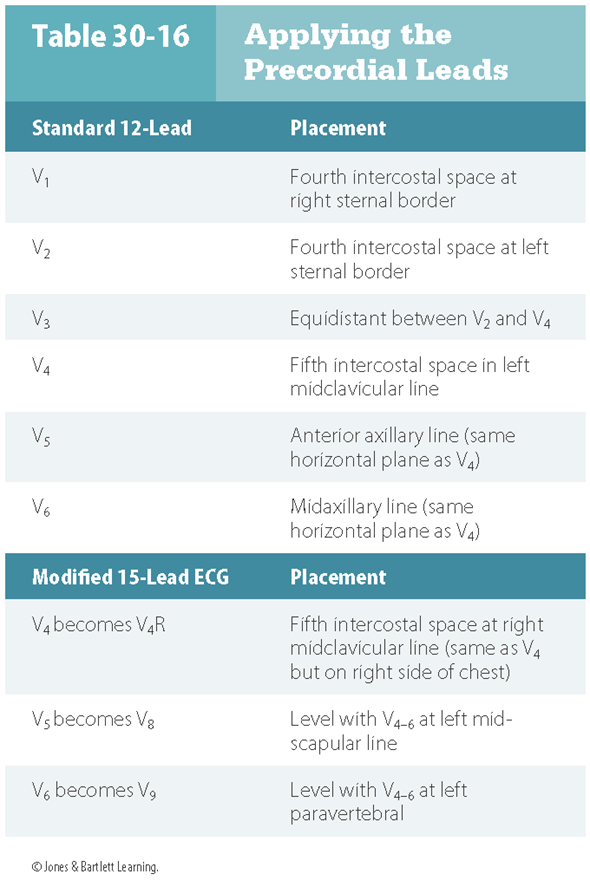
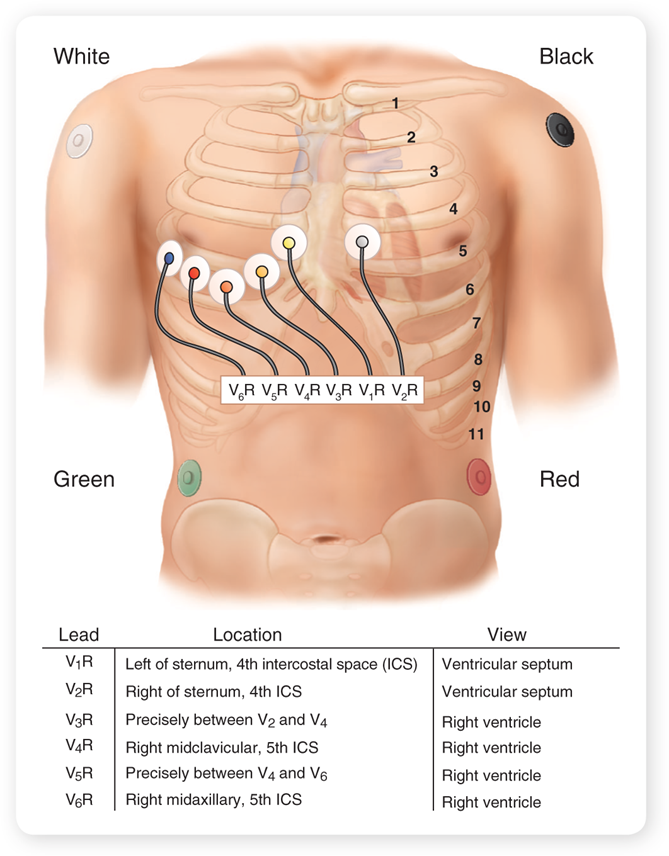
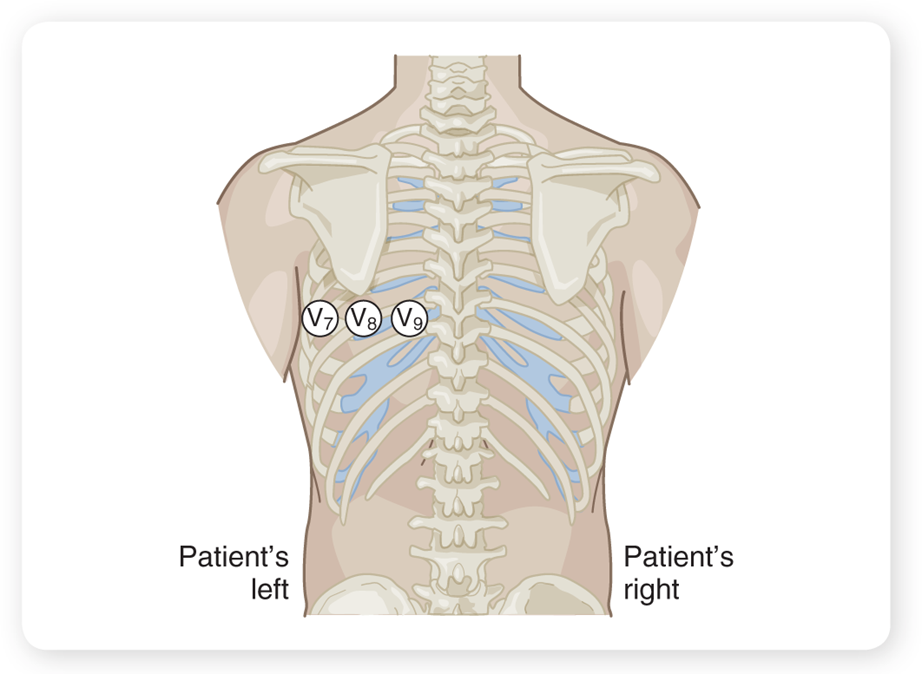
§Right-side precordial leads
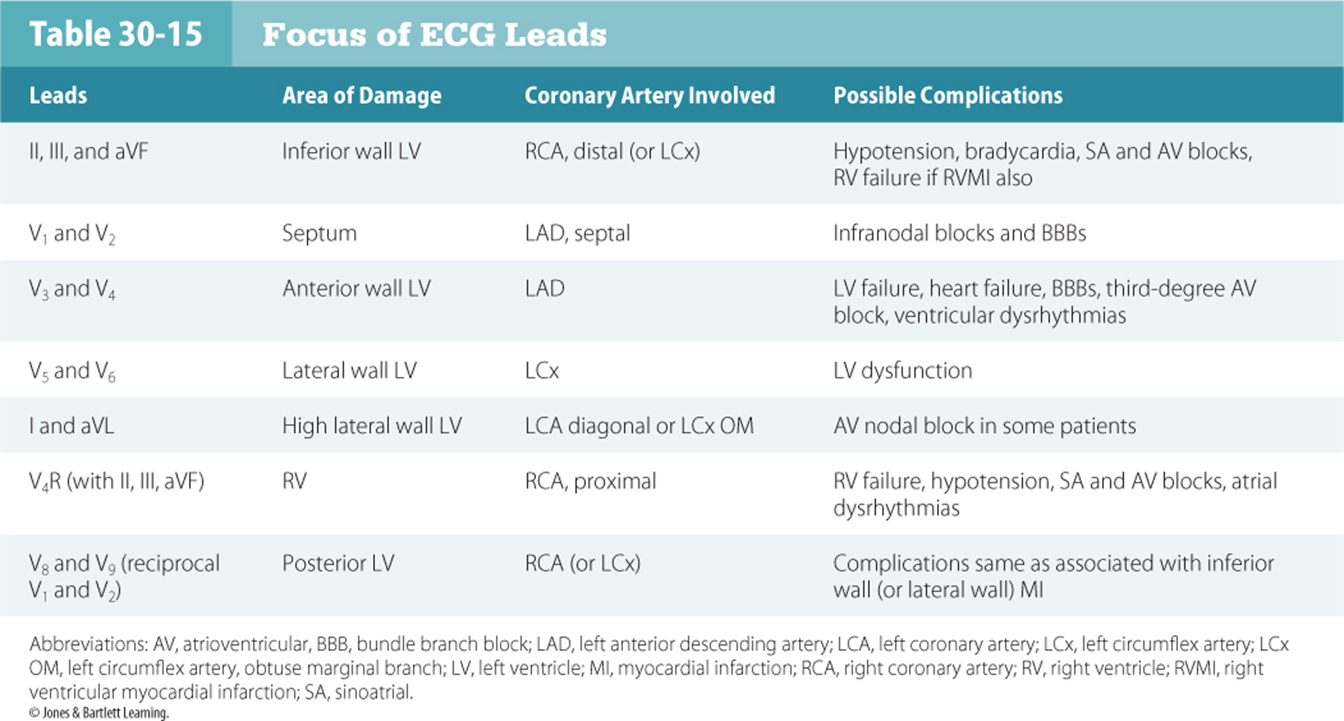
Focus of ECG leads
15 lead placement
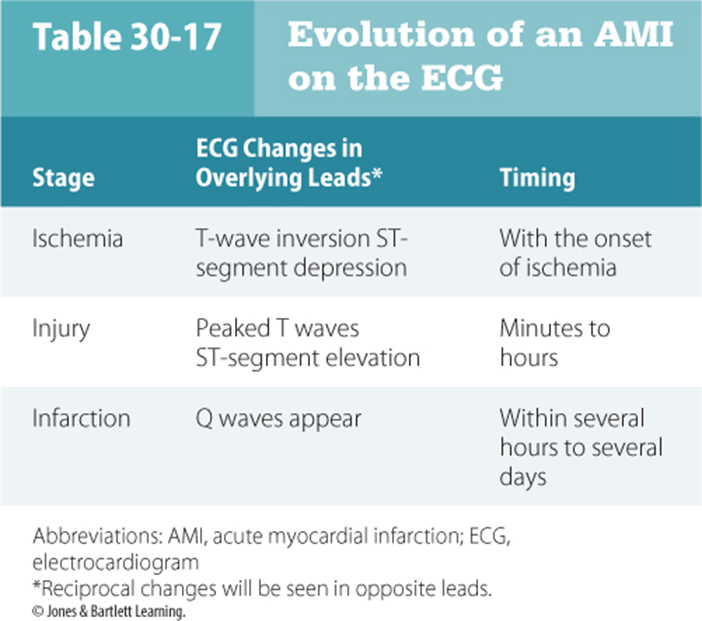
Evolution of an AMI
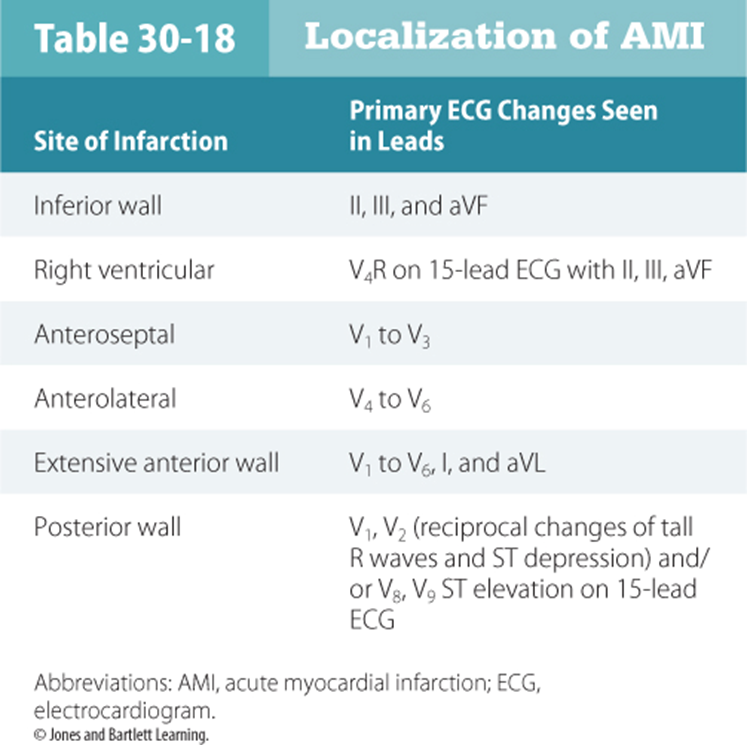
localization of AMI
§Evolutionary pattern of acute myocardial infarction
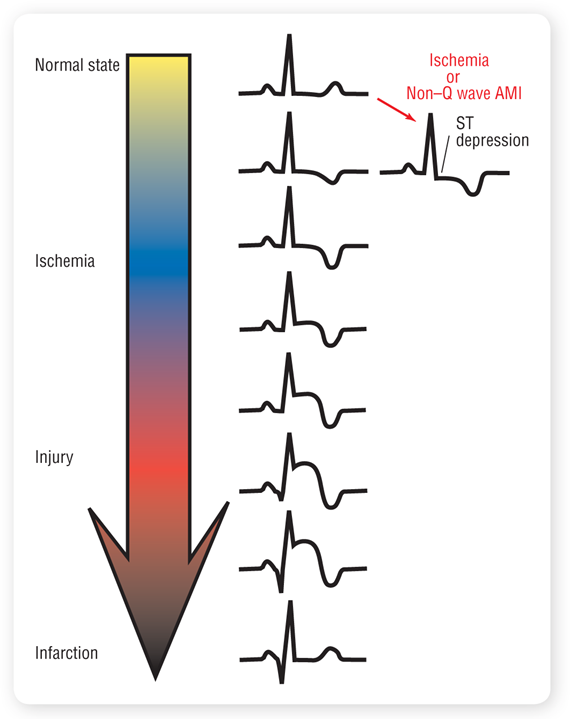
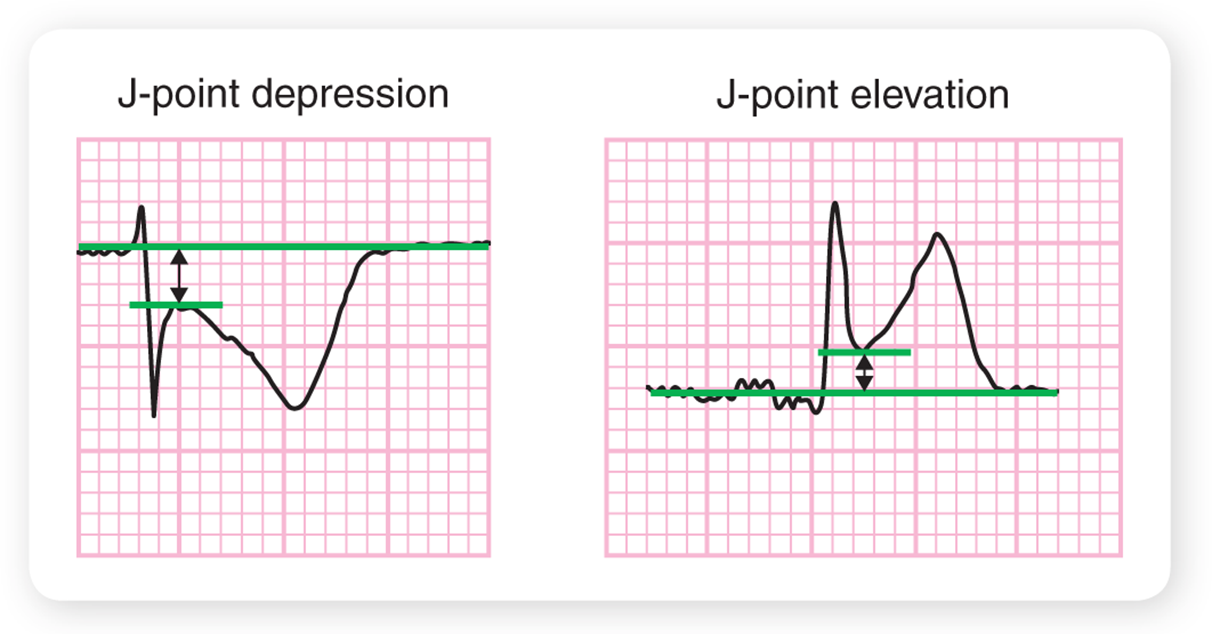
J point Depression and Elevation
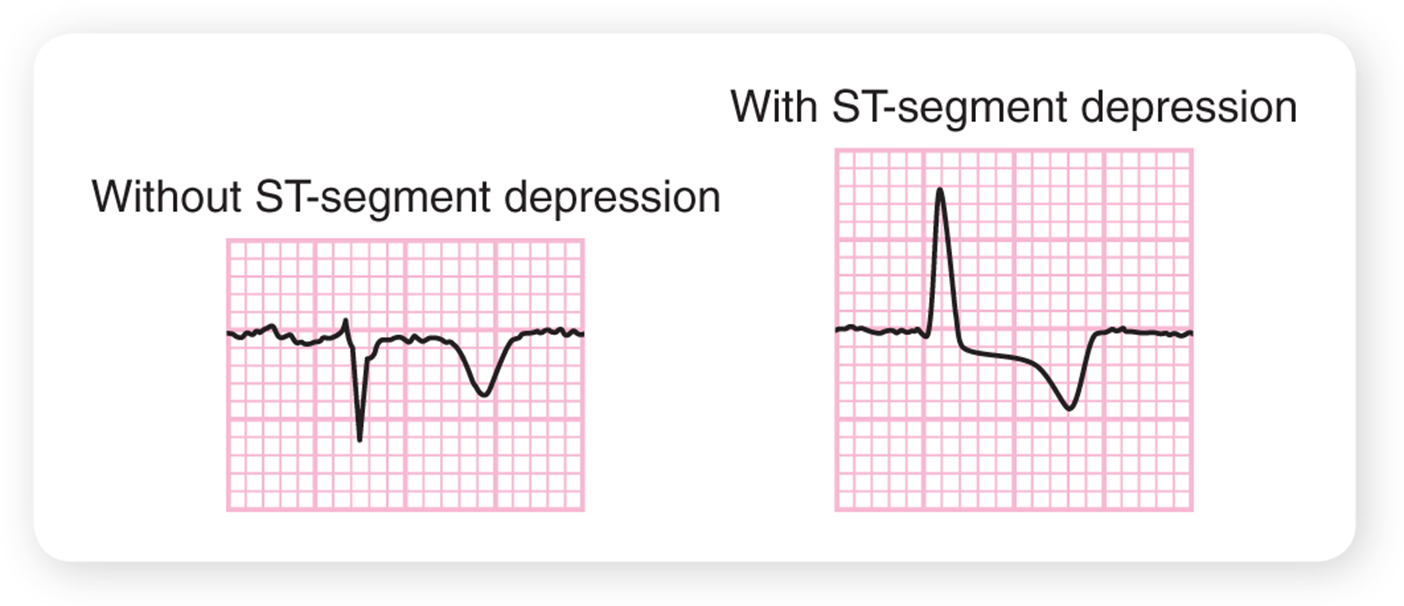
§T-wave inversion
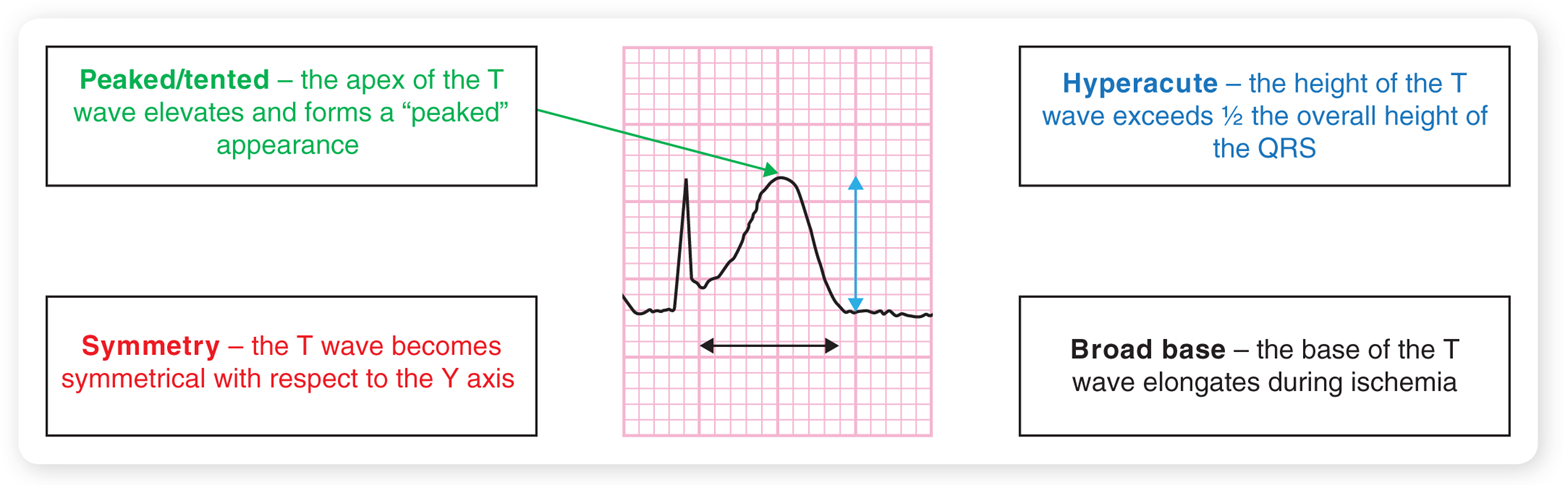
T-wave morphology
Right Side Leads
Posterior Leads
§Convex versus concave ST segment
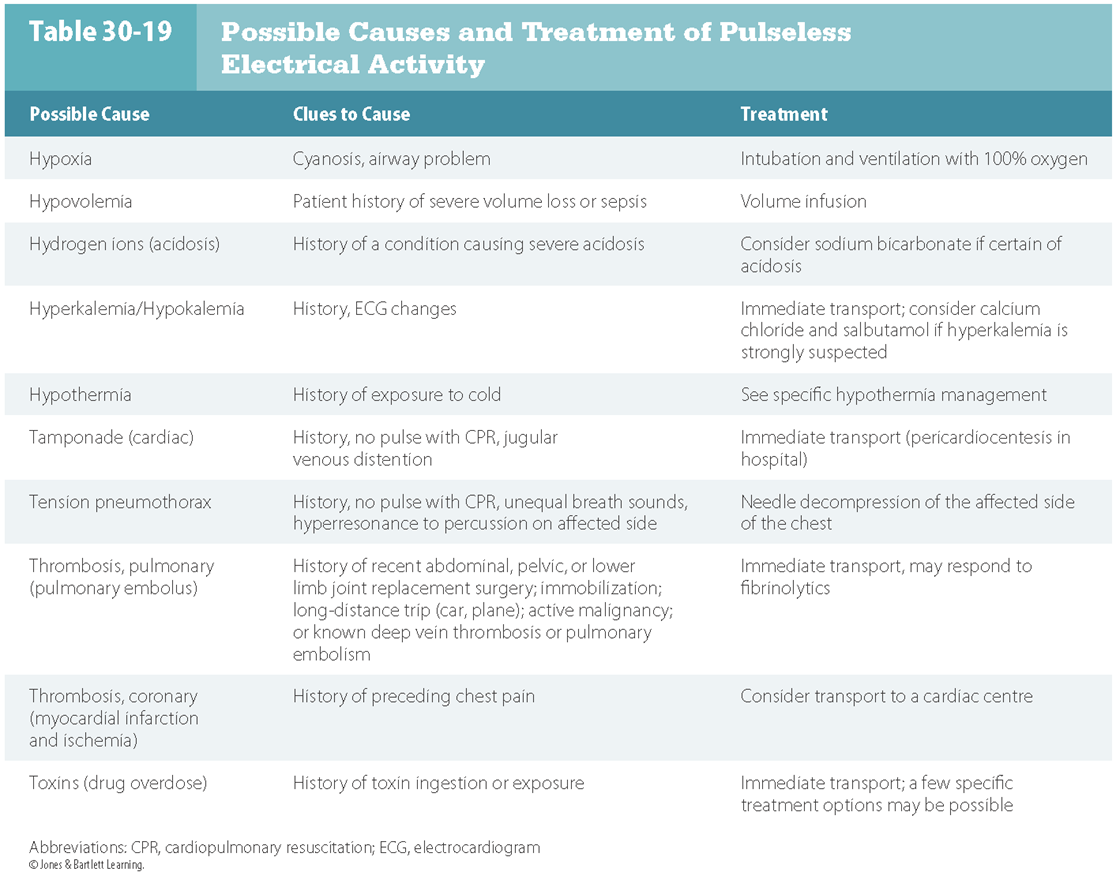
H’s and T’s
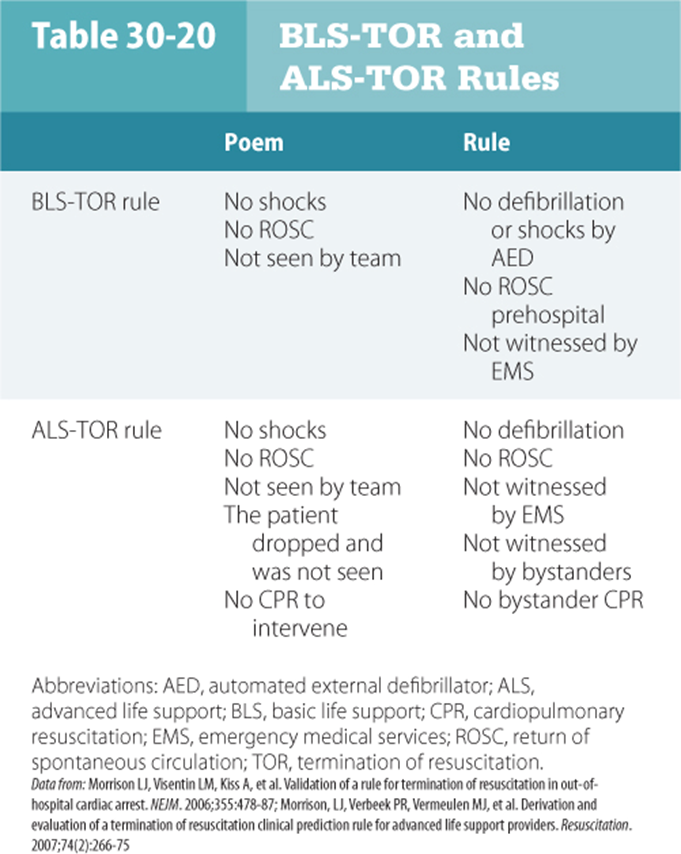
BLS-TOR and ALS-TOR rules
OLOL

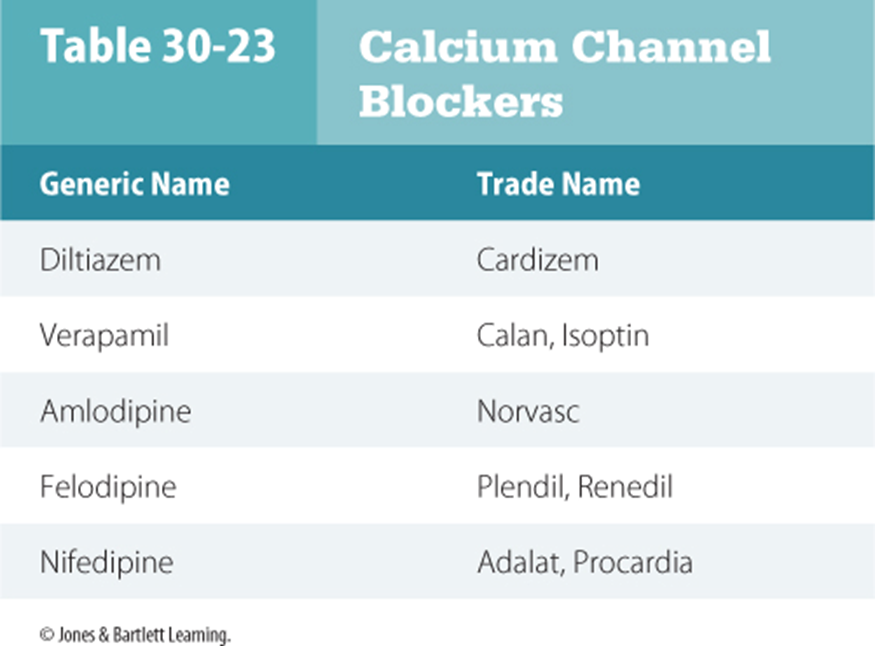
Calcium channel blockers
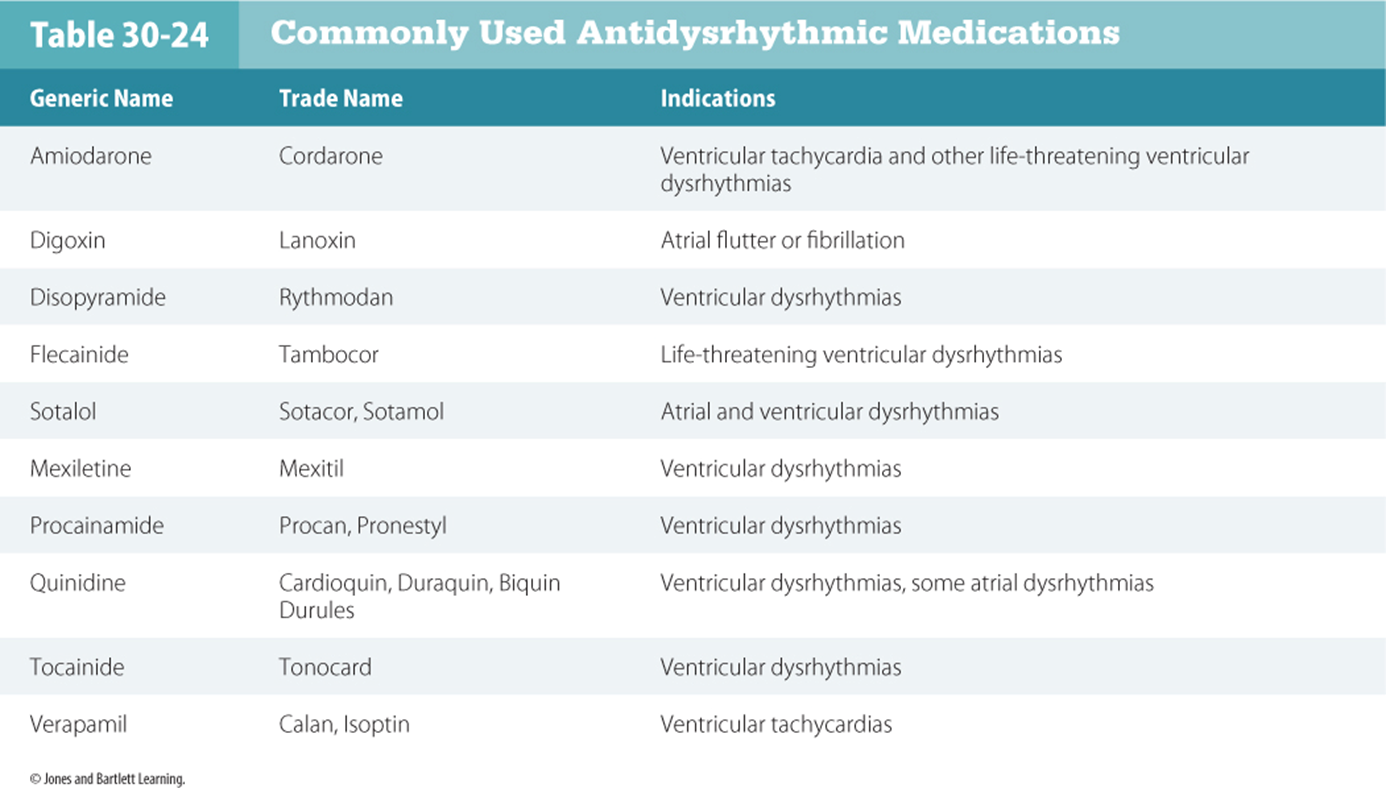
Antidysrhythmic Medications
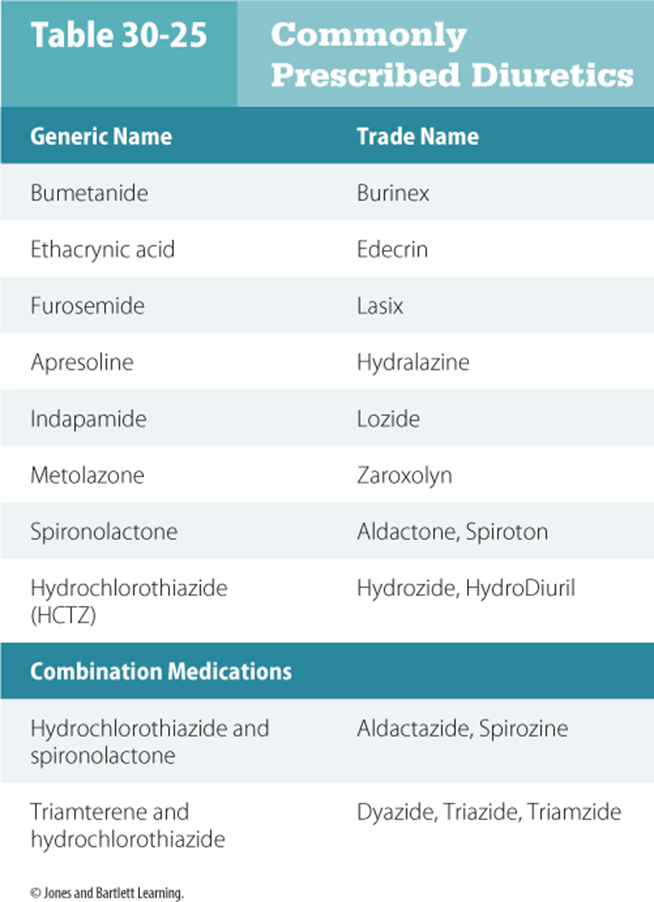
Diuretics
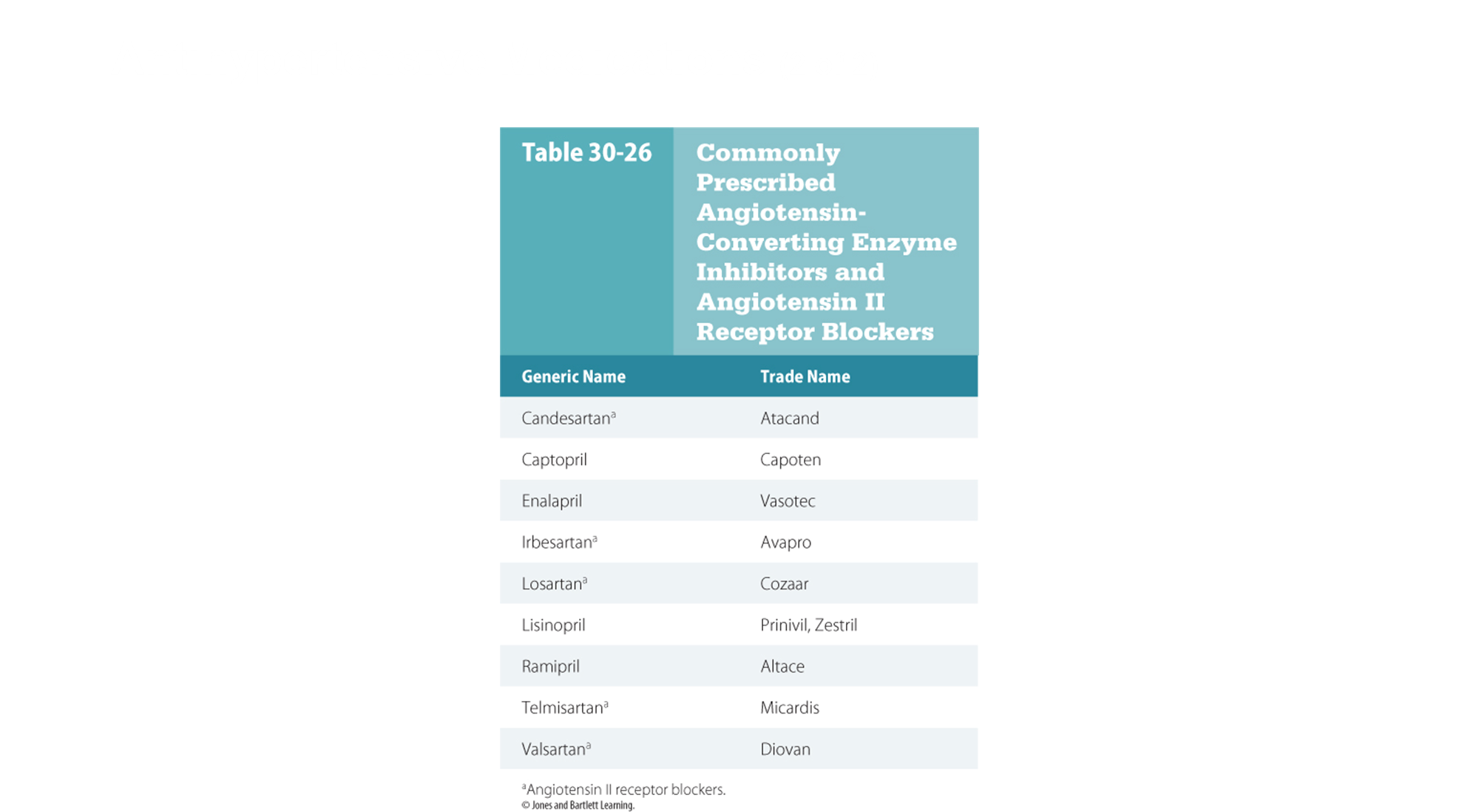
Antihypertensive Medications
anticoagulant medications
§Blood thinners
§Diminish the ability of the blood to clot
§Prescribed to patients who have had recurrent problems with blood clots and to patients who might be prone to develop clots
§Apt to bleed excessively
§Traditional oral anticoagulant drug is warfarin (Coumadin); newer medications include dabigatran (Pradax), rivaroxaban (Xarelto), and apixaban (Eliquis).
Antiplatelet Medications
Medications interfere with platelet aggregation and clot formation
Prescribed to patients with CHD and those with a coronary artery stent
Useful in the setting of AMI
Patients apt to bruise easily or bleed excessively
Most common antiplatelet medication is ASA; alternatives include dipyridamole (Aggrenox, Persantine) and ticlopidine (Ticlid). Other newer antiplatelet agents that are commonly administered for an acute STEMI include: clopidogrel (Plavix), ticagrelor (Brilinta), and prasugrel (Effient).