Lecture 8 (1): Causes of brain dysfunction (tumors, strokes, contusion & hematoma, mTRI, CTE
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
Encapsulated tumors
20% of tumors
Tumors, aka neoplasms
Meningioma–better type,grow between the menings
Encapsulated: Has a membrane, so you can see the line between healthy region and tumor region. Remove → rare recurrence, great recovery
Benign: Does not invade nearby tissues, and does not metastasize (spread) to other parts of the body
Infiltrating tumors
80% of tumors
Grow diffusely through surrounding brain tissue (no clear lines to seperate healthy and unhealthy brain tissue)
Referred to as Malignant, because (a) Even removing it, (almost guaranteed that) it’s gonna grow back., and (b) Aggressive growth
Metastatic tumors
Some infiltrating brain tumors grow from a body part (tumor fragments) and carried them to the brain via the bloodstream
Quite malignant, usually infiltrating
Commonly originate from breast cancer or lung cancer
Where do most tumors come from?
Glia! Not neurons! In adulthood, we’re not really creating new neurons, that can clump into tumors, instead, from astrocytes or oligodendrocytes, most commonly.
Glioblastoma
Most common type of malignant brain tumor in adults (40%) astrocytes grow out of control.
Most malignant (guaranteed that it grows back even after removing it)
Very very small survival rate
From diagnosis to the end of your life: 14 months (thats including removing the largest part to slow it down
What exactly are strokes?
Sudden-onset cerebrovascular (blood flow in the brain) disorders that cause brain damage
During the stroke, you are disrupting the blood flow in the brain → no oxygen and glucose coming in → lose ATP production → inactive sodium-potassium pump → lose the ability to maintain resting potential, can’t fire action potential → cell death within 5 mins
Infarct
The direct area of dead/dying tissue. By the time you get to the hospital, this part is already dead, so the doctor won’t try to save this part
Penumbra
Dysfunctional area surrounding the infarct — getting some glucose and blood flow, but not enough that it’s dysfunctional.
Tissue in this area may either recover or die (maximize the chance of surviving). Doctors will try to save this region.
Ischemic stroke
The area that has a Clot blocking blood flow in the artery, and any branches after that doesn’t get blood
i.e. resulting from cerebral ischemia
Hemorrhagic stroke
You still have an infarct, but you also have the bleeding in the brain as a secondary concern, cuz (a) blood has a toxic effect (high level of iron), (b) blood is a highway of pathogens (risk of infection)
i.e. resulting from cerebral hemorrhage
Better recovery than ischemic strokes
Cerebral hemorrhage: Aneurysm
Most commonly in arteries than veins
Ballooning of a blood vessel due to a weakened vessel wall → pop
Can be congenital (born with this) or develop later
Risk factors: Diabetes, hypertension, smoking cigarettes, alcoholism, but the biggest predictor is aging (40-60 —2%, 60-80—7%)
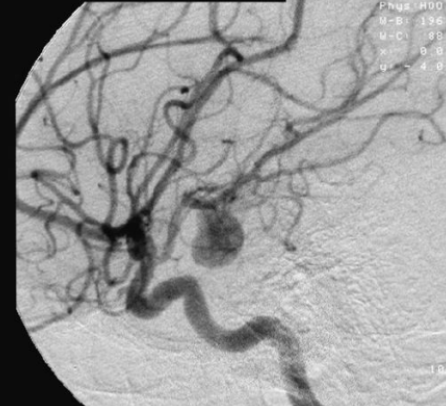
Treatment option 1 for Aneurysm: Clipping
Requires craniotomy (open brain surgery), but slightly lower rate of recurrence than treatment option 2, and permanent solution
Titanium clip (cuz not magnetic, so MRI-safe), clip the neck of aneurysm (where the blood is entering), and the blood in the aneurysm dome (balloon part) will dry and harden, and you just leave it like that! It’s too risky to take it out!
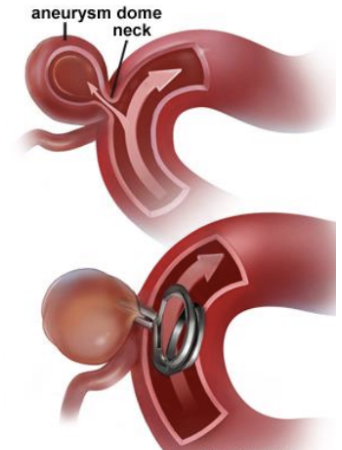
Advantages of clipping (older treatment of aneurysm)
Lower rate of recurrence than option 2, and permanent solution
Risk of clipping (older treatment of aneurysm)
Brain swelling or stroke (due to blood vessel manipulation), Seizures (in some cases), Infection when you put the piece of skull back on, or over-bleeding at the surgical site
Undergo really hard anesthesia (risk of low tolerance of anesthesia as you get older → dangerous)
Treatment option 2 for Aneurysm: Endovascular coiling
Coil is made of platinum (interact w blood → preventing blood from filling it more)
While using the real-time X-ray machine to navigate, cut open the femoral artery (the largest artery, and it’s in your thigh), insert a tube in the thigh, up to the heart, up to the brain, and insert a coil in the aneurysm dome
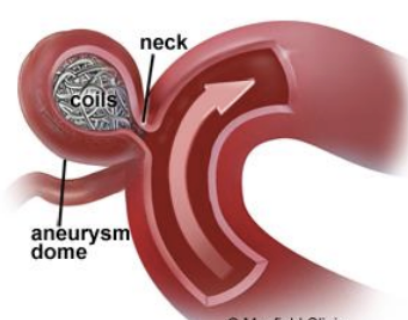
Advantages of endovascular coiling (Newer treatment for aneurism)
FARRRRRR less invasive than clipping, much less risk of infection
Risks of endovascular coiling (Newer treatment for aneurism)
Higher rate of recurrence
Cerebral ischemia
Blockage inside the artery itself
Three main causes of cerebral ischemia
Thrombosis: Plug the artery when it becomes narrow, so anything after is clogged by blood
Embolism: A moving thrombosis (can be anything that’s not blood, piece of fat, tumor tissue, air bubble, etc.)
Arteriosclerosis: Narrowing of the artery + relatively small thrombosis(due to cholesterol), plugging much further in the branch
Thrombosis
Plug the artery when it becomes narrow, so anything after is clogged by blood
Embolism
A moving thrombus (can be anything that’s not blood: piece of fat, tumor tissue, air bubble, etc.)
Arteriorsclerosis
Narrowing of the artery + relatively small thrombus (due to cholesterol), plugging much further in the branch
Ischemia-produced brain damage has three important properties
It takes a while to develop (can be days)
Some parts of the brain are more at risk (e.g. hippocampus—probably cuz it’s more metabolically active → hard to detect through fMRI cuz BOLD level is high in general)
The mechanisms of ischemia-induced damage vary between brain structures
One example of why you get ischemia stroke wayyy later after the blockage: excitotoxicity
Excitotoxicity
Blood clog in penumbra
Less O2 → less energy (ATP)
Na K pumps are not working (that normally maintain resting potential)
Glutamate keeps releasing until too much (glutamate excitory level)
Lots of binding on NMDA receptors → NMDA allow Ca+ to enter the cell
Too much Calcium coming in (Ca usually triggers apoptosis)
ACCIDENTAL apoptosis → Some of the penumbra will die
Apoptosis
Programmed cell death, and it’s normal
Normally, apoptosis is valuable in day-to-day life. On a daily basis, we need millions of cell removal, cuz it’s a major part of development
So what can we do to avoid the apoptosis?
The idea is: Targeting NMDA receptor with the hope of saving penumbra → control the amount of Ca coming in → reduce the likelihood of apoptosis
BUT!!! It hasn’t been effective so far, cuz the Ca is still coming in
On the axon terminal, there’s voltage-gated Ca terminal. If the cell is unable to maintain the resting potential, maybe it accidentally open these gate channels and let the Ca come in anyway
Open-head injuries
Gets through the skull (ex. bullets, 73% of gunshot to head dies on the spot)
Perforating means smth comes in through one side of the skull, to the other side of the skull
Penetrating means coming in just one side
Typically very severe
High risk of infection, complications
High velocity (high speed) worse than low
That’s why gunshot in your head is 90% death rate (So go in ur head slowly is safer)
Closed-head injuries: Contusion
A bruise caused by capillary damage, leading to bleeding under the skin or brain tissue. So you got a crack in the head, but it doesn’t penetrate through the skull.
Involve damage to the cerebral circulatory system, producing internal hemorrhaging and a resultant hematoma–The bleeding that harden and clot, that forms within or outside an organ
Occurs where the brain slams against the skull
Epidural hematoma
Bleeding and harden in between the skull and the menings
The least risky one out of all types of hematoma
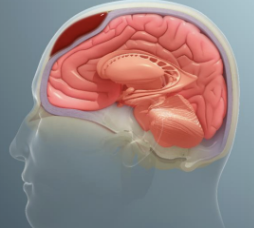
Subdural hematoma
Bleeding and harden between dura mater and arachnoid mater
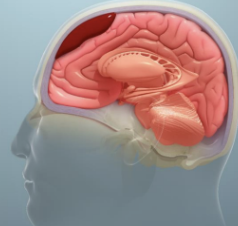
Intracranial hematoma
Bleeding and harden in the brain itself
The worst hematoma
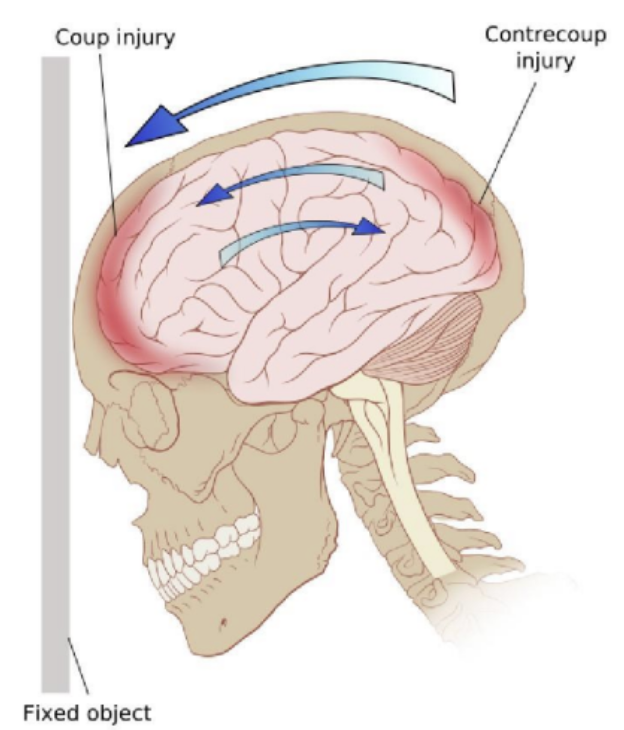
Coup contrecoup injury
When you hit ur head.
Coup Injury (Primary Impact) (called coo injury)
The brain hits the inside of the skull at the site of impact.
This is common in direct head trauma (e.g., falling and hitting your forehead
Contrecoup Injury (Rebound Impact)
The force then causes the brain to slam against the opposite side of the skull.
This often happens in high-impact injuries like car accidents, where the head forcefully jerks forward and backward
Mild traumatic brain injury (mTBI)
Mild trauma to the brain without skull fracture or severe bleeding
When there is a blow to the head but no evidence of contusion (bruising) or other structural damage. It’s not mild tho, there’ll still be disruptions in your life
Typically synonymous with concussion, which is a syndrome, but you can injure your brain without getting a concussion (subconcussive mTBIs)
Temporary damage ex.: Super sensitive to light, sleep disorder, mood, attention span, dizziness
The damage last 8-19 months, and can’t take the blow in the head again during this healing duration
Subconcussive mTBIs
A brain impact that does not cause immediate concussion symptoms but may still lead to cumulative brain damage over time.
Unlike a full concussion, a subconcussive impact does not cause noticeable loss of consciousness or cognitive impairment at the moment of injury.
"Subconcussive" = below the concussion threshold, but still a brain injury.
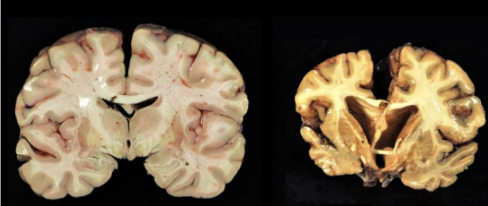
Chronic traumatic encephalopathy (CTE)
A form of dementia, same as how Alzheimer’s is also a form of Dementia
Triggered by repeated blows (hitting ur head to a hard object) to the head, even though you’ve never had a concussion
A progressive, irreversible neurodegenerative disease. Will still progress, even when you stop taking blows to the head
Not just professional athletes, not concussion. You don’t necessarily need to have concussions to get this disorder
99% Guaranteed that if you play in the NFL, you’ll have this disorder
4 stages of CTE
Confusion, disorientation, headaches
Lapses in memory, social norms, impulsivity, judgement
And 4: Progressive dementia, movement disorders (Parkinsonism), speech disorders, depression, suicidality
Pathological aggression, jealousy, and paranoia are common
Tau
Tau is a protein, binding to the cytoskeleton → stabilizes cytoskeleton → change and break down cytoskeleton to rebuild it
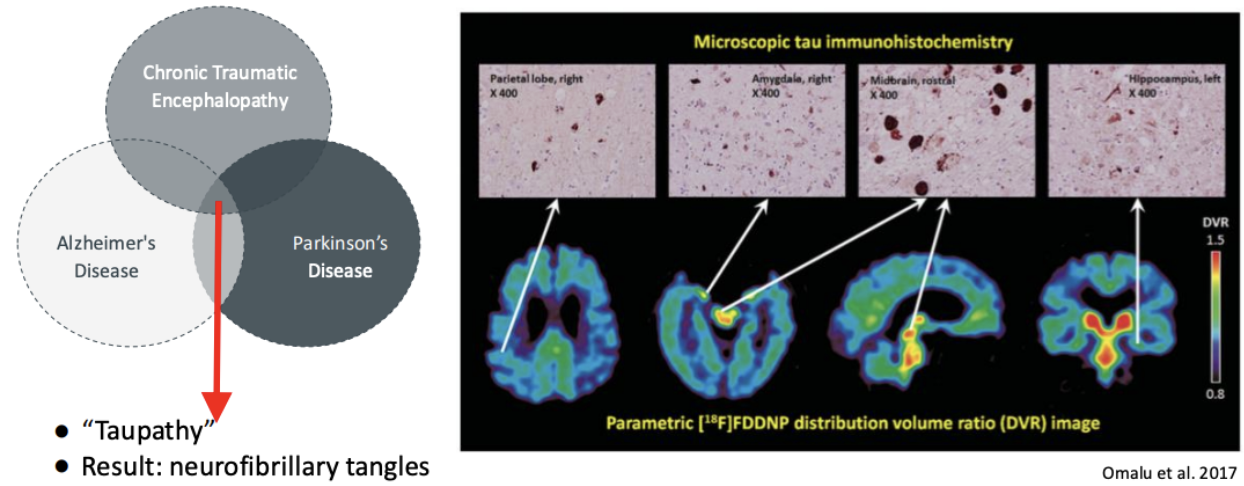
Is Tau a cause of CTE?
Tau is NOT necessarily a cause of CTE, because tau can also be seen in Alzheimer’s (AD), Parkinson’s (PD)
A clear marker of CTE, but relies on postmortem staining (after death)
Neurofibrillary tangles
Tau tangles.
When tau is hyperphosphorylated, it aggregates, and the cytoskeleton becomes unstable
(COULD be a cause of CTE)
Tau progression in CTE vs. AD
In CTE: The medial temporal lobe (memory) is the first place to spread out! The little spots seen around the cortex first
In AD: Spread from the deeper region first
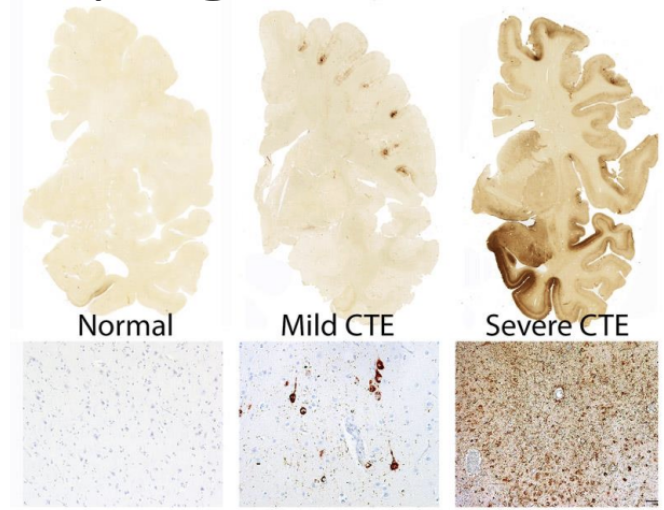
Where does Tau spread first? (Sulci/gyri)
Sulci first (the inner fold). The most common theory of why this is, is cuz you are having a series of micro-hemorrhages from taking blows to the head, so you have small bleeds in your brain. Blood has toxic effects (ex. iron), and the vessels run in the folds (sulci) than on gyri.
Taupathies
PET (detects protein) uses radioactive marker that binds to hyperphosphorylated tau
It works, detects in brainstem (deeper part), but doesn’t detect in the cortex (which is where tau grows first in CTE)