3.2 Psychosocial Aspects of Aging and Frail Elderly
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
what is seen in cognitive decline?
mental processing speed decline
sensory-perceptual changes
sensitivity to visual contrast and sound
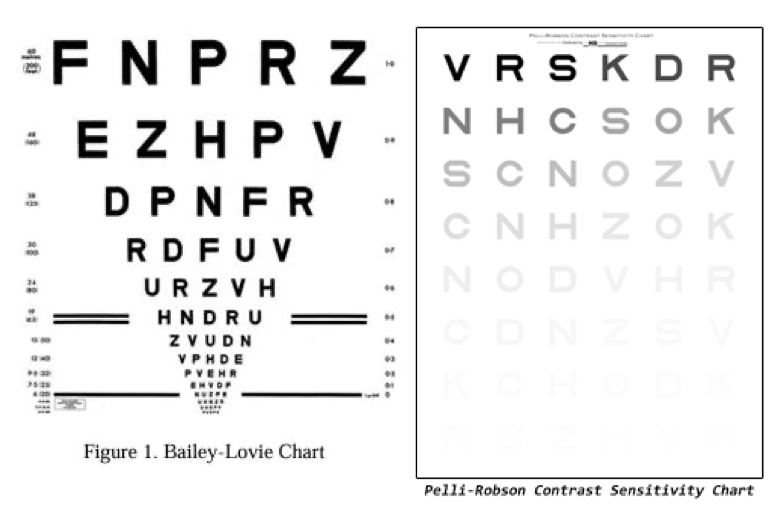
what is this test checking for?
cognitive decline
what are signs of memory decline?
no definitive conclusions
difficulty with multi-memory tasks
frontal lob shrinkage
working memory decline
long term memory less affected than short term memory
what is fluid intelligence?
the ability to process new general information that requires no specific knowledge
what is crystallized intelligence?
knowledge that must be learned or memorized
when does intelligence start to decline?
sixties or seventies
as we increase in age, fluid intelligence…
decreases
how is learning affected as we age?
slower but once something is learned the rate of forgetting is no faster than young ones
sensory deficits affect learning
what is tested in the Mini Mental Status Exam?
test of cognitive function among the elderly
includes orientation, attention memory, language, and visual spatial skills
what is the single cutoff for the MMSE that is considered abnormal?
< 24
what value of the MMSE indicates increased odds of dementia?
<21
what value of the MMSE indicates decreased odds of dementia?
>25
what score range on the MMSE is indicative of no cognitive impairment?
24-30
what score range on the MMSE is indicative of mild cognitive impairment?
18-23
what score range on the MMSE is indicative of severe cognitive impairment?
0-17
elderly patients with college education who present with complaints of cognitive decline and score ___ on the MMSE are at greater risk of being diagnosed with dementia
< 27
what are the 3 Ds of confusion?
delirium
dementia
depression
what causes delirium?
medication interaction
benzos
life-threatening illness
sepsis
what is delirium?
acute brain syndrome
confusion, changes level of consciousness, difficulty concentrating
difficulty with immediate recall, short term memory, maintaining attention
often have hallucinations
how long does delirium last?
hours to weeks
usually return to normal once the problem has been fixed
symptoms of hyperactive delirium
agitated
mood swings
angry
belligerent
aggressive towards caregivers
symptoms of hypoactive delirium
extreme drowsiness
fatigue
indifference
how do you manage pts with delirium?
hydration
want to help flush out meds if that is what is causing the problem
calm and quiet environment
low level of lightening without shadows, natural lighting
simple, clear instructions
familiar objects, individuals
visual hearing aids
maximize all their senses
avoid restraining agitated pt with delirium
avoid feeding into hallucinations → reorient
what test is used to measure if a pt is in a state of delirium or not?
Confusion Assessment Method for the ICU (CAM-ICU) Flowsheet
what are the signs of dementia?
enlarged ventricles, shrinkage cortex and hippocampus
loss of memory
lose daily living skills
personality changes
develops over a number of years and slowly worsens
why are pts with dementia at a higher risk of injury with falls?
cortex shrinkage, more room for the brain to move within the cranium
what are the types of dementia?
Alzheimer’s Disease
Vascular Dementia
Vitamin B12 deficiency
over- or under-active thyroid gland
excessive alcohol use
what percentage of dementia is Alzheimer’s?
70%
what percentage of dementia is vascular dementia?
17%
how do you manage pts with dementia?
simplify
explain
reorient
slow down
avoid change
one step at a time
take care of yourself
what are the cognitive symptoms of depression?
poor concentration
low self-esteem
indecisiveness
guilt
hopelessness
inability to concentrate
suicidal ideations
what are somatic symptoms of depression?
fatigue
altered sleep patterns
weight gain or loss
tearfulness
agitation
heart palpitations
overall weakness
what are the affective symptoms of depression?
sadness
anxiety
irritability
fear
anger
depersonalization
feelings of isolation
what is the score cut off for depression on the Geriatric Depression Scale?
> 5 = depression
what is another questionnaire that measures depression but is not specific to geriatric populations?
patient health questionnaire - 9 (PHQ-9)
how do you manage pts with depression?
resistance training/group exercise
referral to PCP → worsening depression needs to be treated ASAP
be aware of the treatment plans and goals
shift the pts focus to other situations
their dog or grandkids (something that makes them happy)
motivation → emphasizing strength and positive feedback
what is fear of falling associated with?
decreased satisfaction with life
increased frailty
increased depressed mood
increased recent falls
decreased mobility
decreased social activities
how does gait change with decline?
reduced gait speed, stride velocity
increased gait variability
significantly longer anticipatory postural adjustment phase during gait initiation
difficulty with dual task
what is the biomedical definition of frailty?
disease and illness of the frail population (multiple diseases, numerous chronic conditions, require long-term hospital care)
what is the functional definition of frailty?
lose the ability to perform ADLs and need assistance
(institutionalized, dependent on others for ADL care, debilitated and could not survive without substantial help, need long-term help with basic ADLs)
what is the systems definition of frailty?
takes into account various interlocking physical, psychological, and social complexes
(diminished ability to carry out practical. and social ADLs, have poor functioning in physical, cognitive, emotional, sensory, and social functions)
what factors influence frailty?
financial
cognitive
level of education
interpersonal
physical
psychological
self rated
living arrangement
what is an independent risk factor for admission to an institution?
cognitive impairment
who is eligible for home care?
dr must certify that you are home bound
leaving your home isn’t recommended because of your condition
you condition keeps you from leaving home without help
leaving home takes considerable and taxing effort
can only leave for dr appt, church or hair appointment
what are the predictors and risk factors for institutionalization?
physical function
restricted mobility
social resources and support
health perception
socioeconomic status
health-care system
it is estimated that 60% of people older than 65 years and are dependent in __-__ ADLs reside in nursing homes
5-7 ADLs
independent mobility outside of the home has been found to be associated with lower risk of what?
institutionalization
low quantity of social relationships is associated with what?
increased risk of death and institutionalization
what is an iatrogenic illness?
unintended and harmful condition resulting from a diagnostic or therapeutic intervention
accidental injury occurring in an institutional setting
what are the MSK problems associated with bed rest and immobility?
muscle weakness and atrophy
dec endurance
contracture
osteoporosis
what are the cardiopulmonary problems associated with bed rest and immobility?
inc heart rate
dec cardiac output
orthostatic hypotension
venous thromboembolism
what is failure to thrive?
medical diagnosis
impaired physical function
weight loss
depression
cognitive impairment
dehydration
what makes a hostile physical environment?
raised beds
shiny floors
restraints
lots of equipment