Cardiovascular Health: Heart Failure and Pulmonary Embolism
1/138
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
139 Terms
Perfusion
Blood flow through targeted tissues.
Capillary Hydrostatic Pressure
Pressure pushing blood into interstitial spaces.
Peripheral Pulses
Assessment of pulse regularity and warmth.
Capillary Refill
Time taken for color to return, < 2 secs.
Pitting Edema
Indentation remains after pressure is applied.
Non-Pitting Edema
No indentation remains after pressure is applied.
Cardiac Output (CO)
Volume of blood pumped by heart per minute.
Stroke Volume (SV)
Amount of blood ejected with each heartbeat.
Ejection Fraction
Percentage of blood pumped out of ventricles.
Mean Arterial Pressure (MAP)
Average blood pressure in a person's arteries.
Creatinine Kinase (CK)
Enzyme indicating myocardial infarction severity.
Troponin I
Marker for cardiac muscle necrosis.
C-Reactive Protein (CRP)
Indicator of inflammation associated with CAD.
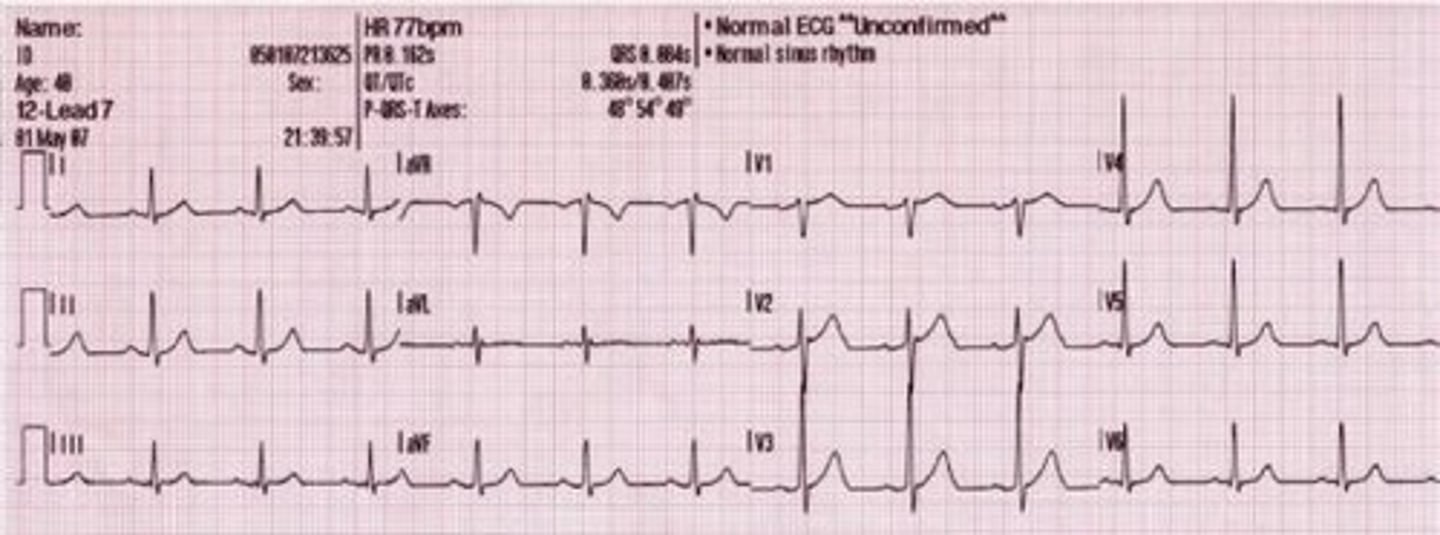
Electrocardiogram (ECG)
Test measuring electrical activity of the heart.
Antihypertensives
Medications to lower blood pressure.
Diuretics
Medications that increase urine output.
Cardiac Glycoside
Medication that increases cardiac output.
Anticoagulants
Medications preventing blood clot formation.
Thrombolytics
Drugs that dissolve blood clots.
Heart Failure
Inability of heart to meet metabolic demands.
Systolic Dysfunction
Impaired contraction of the heart.
Diastolic Dysfunction
Impaired filling of the heart.
Frank Starling Mechanism
Increased stretch leads to stronger contractions.
Neuroendocrine Response
Hormonal response to maintain blood flow.
Ventricular Hypertrophy
Thickening of heart muscle due to workload.
Dilation
Enlargement of heart chambers.
Left Sided Heart Failure
Most common cause of right sided heart failure.
Cardiac Stress Test
Evaluates heart function under stress.
Pacemaker Insertion
Surgical procedure to regulate heart rhythm.
Systolic heart failure
Type of heart failure with reduced EF
Diastolic heart failure
Type of heart failure with preserved EF
Left sided heart failure
Can lead to right sided heart failure
Right sided heart failure
Caused by conditions that restrict blood flow to the lungs
High output heart failure
A type of heart failure characterized by increased cardiac output
Acute heart failure
A sudden onset of heart failure symptoms
Chronic heart failure
A long-term condition where the heart does not pump blood as well as it should
Systolic function
Refers to the contraction phase of the heart
Diastolic function
Refers to the relaxing and filling phase of the heart
Left sided heart systolic failure
Impaired contraction of ventricles to eject sufficient volume of blood into the arteries
Myocardial infarction
A condition that can affect contractility of the heart
Dilated cardiomyopathy
A condition that can affect contractility of the heart
Preload
Increased with decreased contractility
Mitral valve regurgitation
A condition that increases preload
Aortic valve regurgitation
A condition that increases preload
Left sided diastolic heart failure
Characterized by decreased filling and high afterload
Ventricular hypertrophy
A condition that can lead to impaired relaxation of heart muscle
Hypertension
Can cause elevated afterload due to resistance of the outflow
Aortic valve stenosis
Can cause elevated afterload due to resistance of the outflow
Tricuspid valve regurgitation
Can lead to increased preload and decreased contractility
Pulmonary stenosis
A condition that can cause increased pressure in the pulmonary vasculature
COPD
A condition that can cause increased pressure in the pulmonary vasculature
Risk factors of heart failure
Includes CAD, hypertension, diabetes mellitus, congenital heart defects, smoking, obesity, and alcohol abuse
BNP
A test used to diagnose heart failure with values indicating severity
Serum electrolytes
Includes calcium and magnesium, important for diagnosing heart failure
Fluid volume management
Involves monitoring lung sounds, urinary output, and daily weight
Dietary consult
Recommended for patients with heart failure to manage sodium intake
ACEI / ARB
Medications that can cause hyperkalemia as a side effect
Heart transplant
Treatment of choice for end stage heart failure
Pulmonary embolism
Obstruction of blood flow in the pulmonary vascular system, a medical emergency
Virchow's triad
Consists of hypercoagulability, stasis, and endothelial damage
Popliteal veins
Veins located behind the knee that can be involved in thrombus formation.
Iliofemoral veins
Veins in the pelvis and thigh that can be involved in thrombus formation.
Thrombus
A blood clot that forms in a blood vessel and remains attached to its place of origin.
Embolism
A condition where a thrombus breaks loose and travels through the bloodstream to lodge in a vessel.
Pulmonary Embolism (PE)
A sudden blockage in the pulmonary arteries, usually caused by a blood clot from the deep veins in the leg.
D-dimer
A fragment of fibrin formed during the lysis of blood clots, used as a diagnostic marker for clotting.
CT with contrast
A diagnostic imaging technique used to locate pulmonary embolism.
V/Q lung scans
A test that involves injecting isotopes and scanning the lung field to assess ventilation and perfusion.
Chest x-ray
An imaging test used to identify pulmonary infiltrates and pleural effusion.
ECG
An electrocardiogram used to rule out myocardial infarction.
ABG
Arterial blood gas test that initially shows respiratory alkalosis with hypoxemia and metabolic acidosis due to hypoxemia.
End-tidal carbon dioxide (ETCO2)
A measurement that decreases with pulmonary embolism.
Embolectomy
Surgical removal of an embolus.
Heparin
An anticoagulant medication used in bolus and infusion for treating blood clots.
Warfarin
An anticoagulant that requires 5-7 days before discontinuing heparin.
INR
International normalized ratio, a measure of blood coagulation, with a target range of 2-3 for patients on warfarin.
Fibrinolytic therapy
Treatment using clot-busting medications to dissolve blood clots.
Vitamin K
An antidote for warfarin overdose.
Virchow's Triad
A model explaining the three factors that contribute to thrombus formation: stasis of blood flow, hypercoagulability, and endothelial damage.
Deep vein thrombosis (DVT)
Formation of a clot in the deep veins, often in the legs.
Homan's sign
A clinical sign indicating DVT, where dorsiflexion of the foot causes pain.
Doppler ultrasound
A diagnostic test used to visualize blood flow and detect clots.
Venography
An imaging test that uses contrast to visualize veins and detect clots.
Calf exercises
Exercises recommended for clot prevention, especially in patients at risk.
Thrombectomy
Surgical removal of a blood clot.
Fibrinolytics
Medications used to dissolve blood clots, with associated bleeding risks.
Pneumatic compression devices
Devices used to prevent DVT by promoting blood flow in the legs.
Supportive stockings
Compression garments used to enhance venous return and prevent clot formation.
Compression stockings
Elastic garments to prevent blood pooling.
Enoxaparin
SQ anticoagulant for clot prevention.
SCDs
Sequential compression devices for DVT prevention.
aPTT
Monitors heparin therapy, normal range multiplied by 1.5-2.5.
Protamine sulfate
Antidote for heparin overdose.
PT/INR
Monitors warfarin therapy; therapeutic INR is 2-3.
TPA
Thrombolytic agent for clot dissolution.
IVC filter
Prevents clots from entering heart/lungs.
Left Heart Failure
Weak pump due to myocardial damage.
Right Heart Failure
Often results from left heart failure.
Aldosterone
Hormone that retains sodium and water.
ACE inhibitors
Lower blood pressure without affecting heart rate.