2. Occlusal forces and the Periodontium
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
what are the physical functions of PDL?
• Attachment of tooth to bone
• Shock absorption
• Space for blood vessels and nerves
• Transmission of forces to bone
what are adaptive functions of PDL?
• Adaptation and remodeling in response to occlusal forces
• Remodeling in response to orthodontic forces
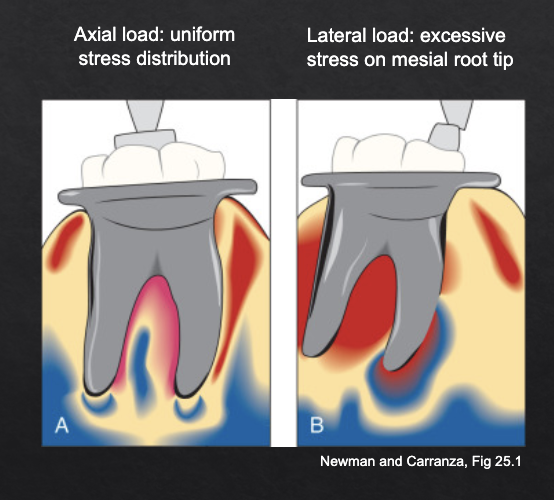
what is considered normal occlusal load in terms of force?
70-150 N
what is considered normal occlusal load in terms of angle?
axial with limited lateral component
what is considered normal occlusal load in terms of duration?
normal chewing is episodic (vs clenching which is continuous)
t/f: there is no/minimal direct contact between antagonist teeth during normal chewing
true
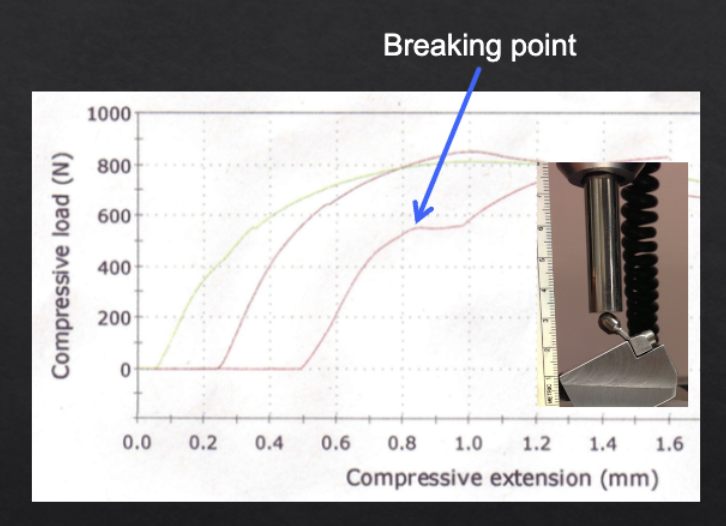
what is considered excessive occlusal load?
force:
angle:
duration:
force: 300-500 N
angle: 30 degrees
duration: 5 million cycles (or continuous)
(as illustrated by implant testing protocols but applies to normal dentition as well)
what dental structures may be damaged under excessive occlusal load?
fracture of tooth and restorations (most common)
fracture of root
damage to periodontium and alveolar bone
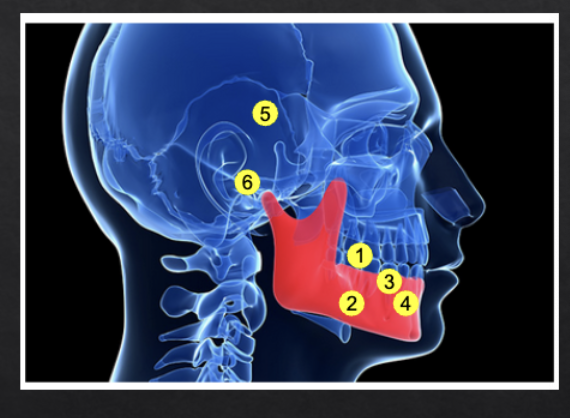
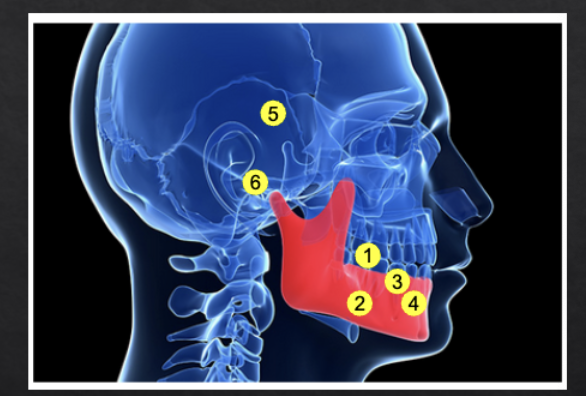
what craniofacial structures may be damaged under excessive occlusal load?
masticatory muscles
TMJ
can occlusal trauma damage periodontal soft tissues?
can widen PDL space
BUT does not cause:
increased BOP
increased probing depth
attachment loss
can occlusal trauma damage alveolar bone?
can cause tooth mobility
BUT can not cause:
horizontal/vertical bone loss
tooth loss
what is Irving Glickman’s concept of occlusal trauma? (debated)
occlusal trauma jiggles the tooth and “pumps” the infection apically along PDL
vertical bone loss is due to occlusal trauma + inflammation
horizontal bone loss is result of inflammation without occlusal trauma
trauma from occlusion was suggested to be co-destructive factor of bone loss
what do opposing views to Irving Glickman’s concept of occlusal trauma like Waerhaug’s concept suggest?
extent of inflammation alone determines extent of bone loss
thickness of bone determines bone loss type:
thin bone + inflammation = horizontal bone loss
thick bone + inflammation = vertical bone loss
OVERALL: occlusal trauma is NOT a contributing factor to vertical bone loss
what conclusion was reached during the Lindhe & Svanberg (1974) experiment?
while occlusal trauma alone does not cause periodontal attachment loss or bone loss, it may accerlerate existing periodontal disease (effect show in animal experiments)
Acute occlusal trauma results form acute injury (e.g. biting on an olive pit). Acute occlusal trauma results in …?
toothache, percussion sensitivity and tooth mobility
Chronic occlusal trauma occurs in response to chronic overload (e.g. bruxism, faulty restorations or insufficient number of teeth). Chronic occlusal trauma results in..?
often asymptomatic; only tooth mobility is detected clinically
what is the difference between primary and secondary occlusal trauma?
primary → results from excessive occlusal forces
secondary → results from normal occlusal forces on a weakened (reduced periodontium)
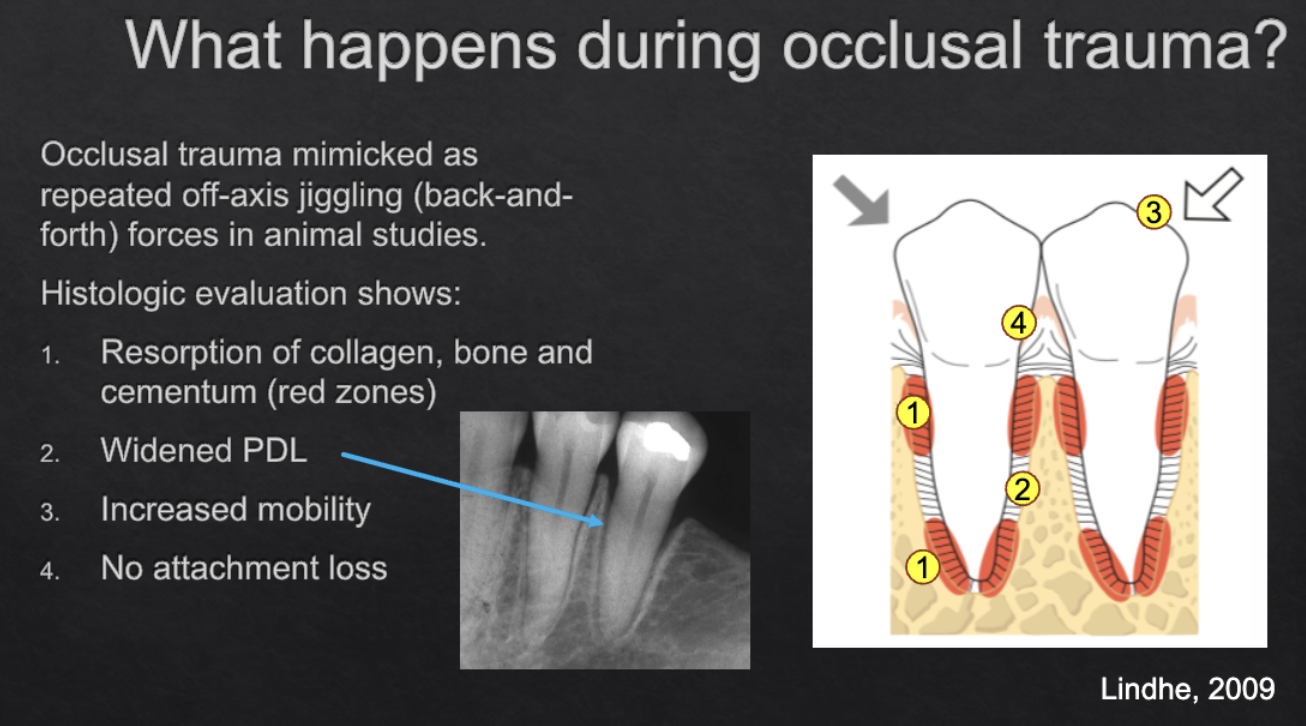
what histologic findings were discovered in animal studies researching occlusal trauma via repeated off-axis jiggling (back-and-forth) forces?
resorption of collagen, bone, cementum
widened PDL
increased mobility
no attachment loss
Q1. Occlusal trauma may be due to:
A. Accidentally biting on a hard object
B. Clenching while asleep
C. Chewing with just a few teeth left
D. All of the above
D
Occlusal trauma can cause:
A. attachment loss
B. increased mobility
C. vertical bone loss
D. tooth loss
B
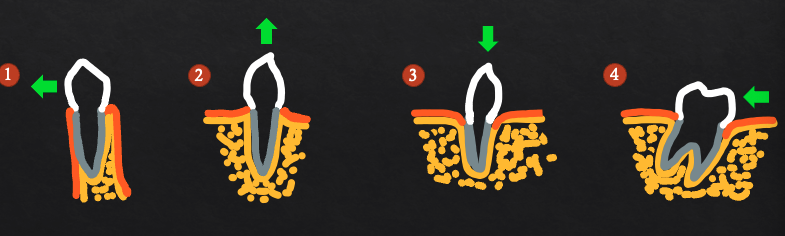
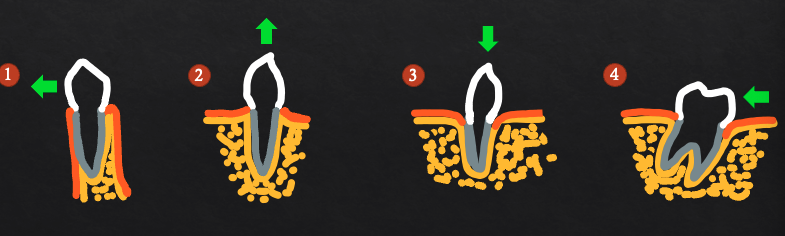
what are the 3 stages of tissue response to acute occlusal trauma (primary)?
injury
repair
adaptation
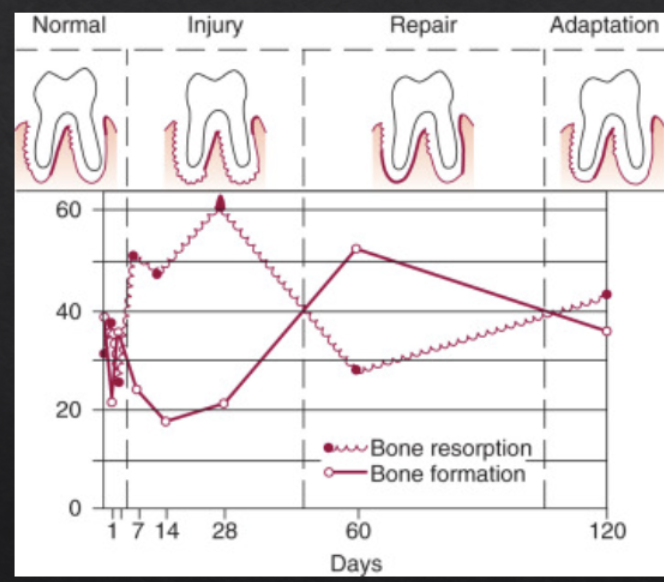
what occurs during stage 1 of tissue response to acute occlusal trauma (primary)?
PDL inflammation (microscopic vascular changes)
bone resorption (microscopic)
widened PDL
increased tooth mobility
what occurs during stage 2 of tissue response to acute occlusal trauma (primary)?
no more inflammation
formation of new PDL, bone, cementum
what occurs during stage 3 of tissue response to acute occlusal trauma (primary)?
widened PDL + tooth mobility remains
these compensate for persistent occlusal trauma (aka it’s not going to keep getting worse and worse, the periodontium adapts to the “new normal” but this doesn’t mean treatment like an molar implant is not indicated)
no pocketing, no attachment loss
normal occlusal forces on a reduced periodontium may cause which type of occlusal trauma? this can be caused by…?
secondary
existing attachment/bone loss
too few remaining teeth (no molars)
what are the consequences of secondary occlusal trauma?
same as primary
widened PDL
increased mobility
but NO progression in attachment loss
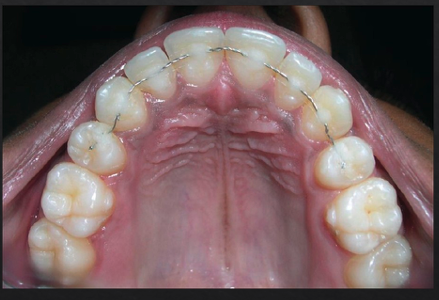
what are clinical signs of pathologic tooth migration (a form of secondary occlusal trauma)?
periodontitis
increased mobility
new interproximal gaps
tooth extrusion

pathologic tooth migration is generally a sign of mild/moderate/severe advanced disease
severe
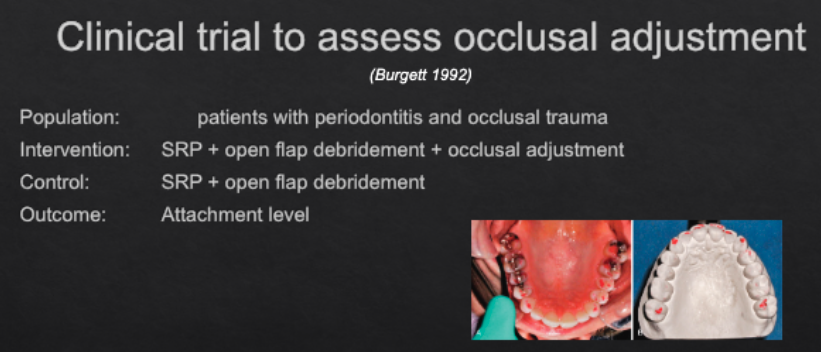
in this experiment/clinical trial, what was the result/conclusion?
occlusal adjustment resulted in minimal but measureable (0.5 mm) increase in attachment gain
occlusal trauma can cause…? (2)
but occlusal trauma by itself does NOT cause…? (2)
Occlusal trauma can:
••• Increase tooth mobility
••• Cause widened PDL
But occlusal trauma by itself does not cause:
••• Periodontal attachment loss
••• Bone loss
There is a physiological tooth mobility due to the orientation and elasticity of periodontal ligament fibers.
Under normal forces this physiological mobility is up to…?
100 microns (0.1mm)
How does physiological mobility vary from tooth to tooth?
larger on single-rooted anterior teeth and less on multi-rooted molars
what factors determine tooth mobility?
Height of the alveolar bone in relation to the length of the root
more bone loss means more mobility
Width of the periodontal ligament space
wide PDL means more mobility
Shape and number of roots
more roots and thicker roots means less mobility
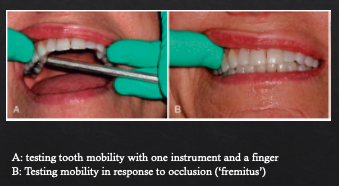
how is tooth mobility assessed?
by moving the crown in a bucco-lingual direction with two instruments or with one instrument and a finger
what classificaiton system do we use to grade tooth mobility?
Miller classification
No mobility: <0.1 mm
Grade I: 0.1-1mm
Grade II: more than 1mm
Grade III: vertical or twist mobility
what are causes of tooth mobility?
occlusal trauma
periodontal abscess
periodontitis
root fracture
treatment of tooth mobility depends on the ______.
cause
how is tooth mobility caused by occlusal trauma treated?
occlusal adjustment, distributing occlusal forces (molar support)
how is tooth mobility caused by periodontal abscess treated?
elimination of cause (SRP, root canal treatment)
how is tooth mobility caused by periodontitis treated?
SRP, splinting for patient comfort
how is tooth mobility caused by root fracture treated?
extraction, implant placement

splinting of teeth
what are some indications for splinting teeth?
For patient comfort on mobile teeth
Pathologic tooth migration
Guided tissue regeneration on mobile teeth
Prosthetics where multiple abutments needed
what is a prerequisite to splinting?
control of periodontal inflammation
t/f: splinting itself induces periodontal regeneration
false. Splinting only mechanically stabilizes teeth, it does NOT by itself induce periodontal regeneration

what consequences may occur when there is no occluding antagonist to a teeth?
Thin PDL
Reduction in bone density
Supra-eruption of tooth
Apparent attachment loss
Furcation exposure
what principle applies to the periodontium as demonstrated by the consequences of lack of occlusion?
use it or lose it
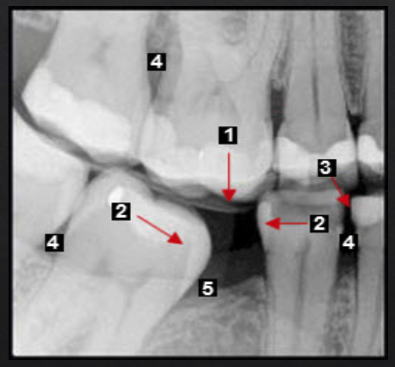
Posterior bite collapse as a result of 1st molar extraction demonstrates multiple occlusal issues that may result in periodontal problems such as
Super-eruption, resulting in root and furcation exposure
Molar tipping, creating a pseudopocket (5)
Open contact, a risk factor for food impaction and gingival inflammation (4)
what are wedge-shaped defects in the buccal cervical region of the tooth?
non-carious cervical lesions (NCCLs)
what are 2 chief mechanisms of non-carious cervical lesions?
Abrasion (toothbrush and toothpaste)
Abfraction (micro-cracks due to occlusal trauma)
t/f: non-carious cervical lesions show signs of periodontitis.
false
Increased frequency of NCCLs are found in subjects with…?
Improper brushing technique (horizontal scrubbing) causes 2-3x more wear than vertical brushing
Excessive manual force
Hard bristle toothbrush
Frequent brushing (twice a day vs once a day)
what is the loss of hard tissue in the cervical region of the tooth by non-axial forces exerted on the occlusal surface, which cause microfractures of dental tissues in areas of stress concentration?
Abfraction
The chief supporting evidence for abfraction comes from …?
computer modeling of stress development in teeth after lateral loads
what is the current accepted concept of the cause of NCCLs?
toothbrush abrasion AND chemical erosion due to acidic foods/drinks
Tooth is suspended in socket by PDL fibers
Low PDL fiber strain leads to…?
High PDL fiber strain leads to…?
bone resorption
bone formation
can there be tooth movement without PDL?
no
moving tooth through cortical bone can lead to…? (1)
creates bony defects (dehiscence)
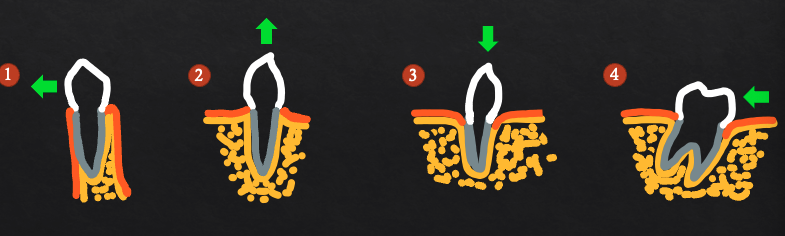
extrusion can lead to…? (2)
bone and gingiva will follow (benefiticial for implant planning)
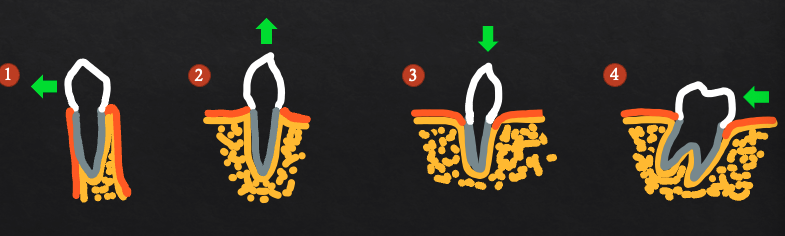
intrusion can lead to…? (3)
unlikely to create new attachment
may create deeper pockets
molar uprighting may lead to…? (4)
eliminating mesial pocketing
may expose furcation
can orthodontic treatment be done in a perio pt?
yes as long as periodontium is inflammation-free
Active periodontitis on the other hand may be aggravated by orthodontic treatment
t/f: Orthodontic treatment may improve the chances of saving periodontally compromised tooth
true
t/f: Tooth movement causes attachment loss in the absence of inflammation
false. Tooth movement does not cause attachment loss in the absence of inflammation
Q3. Tooth #24 can be moved bucco-lingually more than 1mm but not in any other direction. What is the grade of mobility?
0
I
II
III
II
Q4: Which of the following root exposures is caused PRIMARILY by inflammation?
A.Non-carious cervical lesion
B.Periodontitis
C.Orthodontic extrusion
D.Tooth super-eruption
B