PATHO LECTURE 3 (chapter 24) EXAM 2
1/178
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
179 Terms
a human adult has how much blood
5L or 1.3 gallons
blood is made up of what
cellular components (45%) and plasma (55%)
what are the cellular components of blood
erythrocytes (red blood cells), leukocytes (white blood cells), and thrombocytes (platelets)
what are the 5 types of leukocytes
neutrophils, lymphocytes, monocytes, eosinophils, and basophils
what is plasma
pale yellow fluid (extracellular matrix of blood cells)
plasma is made up of what
90% H2O and 10% proteins (albumin, fibrinogen, and globulins)
what is the most important/abundant protein in the blood
albumin
what protein helps in clotting
fibrinogen
what protein has antibodies
globulins
what are the functions of blood
transport of oxygen, carbon dioxide, hormones, nutrients, and metabolic waste products; regulation of body temperature, acid-base balance, and immune response
how many different blood types are there
8
the process of separating blood into its component parts is called what
blood fractionation
how is blood fractionation performed
by centrifuging blood
what is hematocrit
percentage of blood volume that is RBCs
what are the components of centrifuged blood
plasma, buffy coat, and erythrocytes
what is the order of the least dense to most dense components in centrifuged blood
plasma, then buffy coat, then erythrocytes
what is hematopoiesis
process of formation, development, and maturation of blood cells
when does hematopoiesis occur, where does it occur, and what happens in it
starts before birth and continues throughout life
occurs in the bone marrow, liver, and spleen
old cells are continuously replaced with new cells to maintain steady numbers
what are some alternative names for hematopoiesis
hemopoiesis, hematogenesis, and hemogenesis
blood cells are derived from a single pool of stem cells in the bone marrow called what
pluripotent stem cells
pluripotent stem cells give rise to what
lymphoid stem cells and myeloid stem cells
lymphoid stem cells do what
differentiate and eventually develop into B cells, T cells, and NK cells (which are different types of lymphocytes)
myeloid stem cells do what
differentiate and eventually develop along the erythrocyte/megakaryocyte pathway (into erythrocytes and thrombocytes) and the granulocyte/monocyte pathway (into neutrophils eosinophils, basophils, and monocytes)
pathway of pluripotent stem cells into NK cell, T cell and plasma cell
Pluripotent stem cells turn into lymphoid stem cells which turn into NK progenitor, T cell progenitor, and B cell progenitor which turn into NK cell, T cell, and B cell into Plasma cell respectively
pathway of pluripotent stem cells into monocyte
pluripotent stem cell to myeloid stem cell to monocyte progenitor to monoblast to monocyte
pathway of pluripotent stem cells into eosinophils, neutrophils, and basophils
pluripotent stem cell into myeloid stem cell into granulocyte progenitor into eosinophil, neutrophil, and basophil
pathway of pluripotent stem cells into platelets
pluripotent stem cells into myeloid stem cells into megakaryoblast into megakaryocyte into platelets
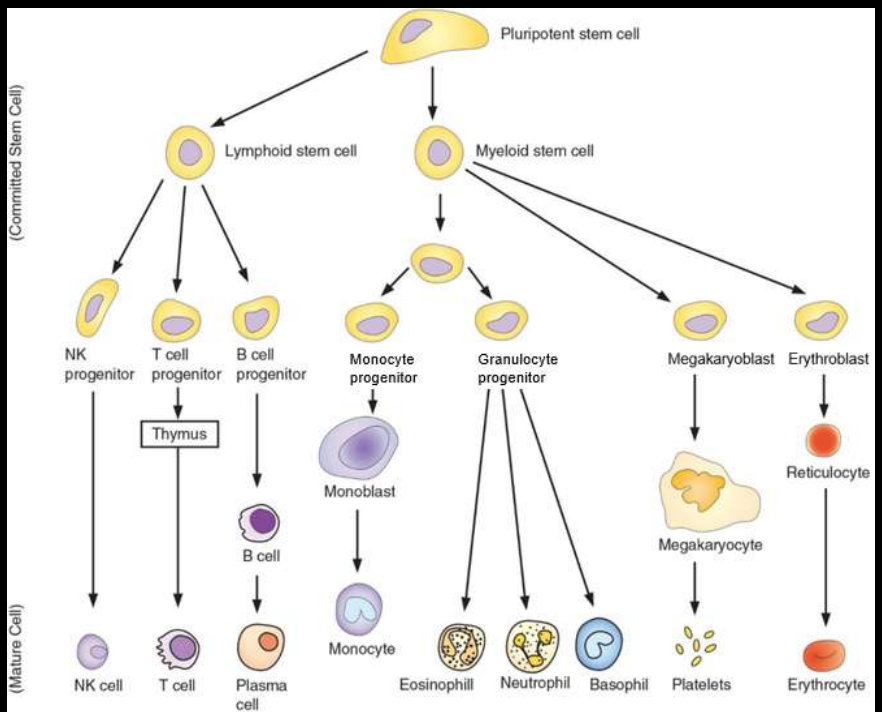
pathway of pluripotent stem cells into erythrocytes
pluripotent stem cells into myeloid stem cell into erythroblast into reticulocyte into eryhtrocyte
what are hematopoietic growth factors
hormone-like regulatory molecules that help in the survival , differentiation, and proliferation of progenitor cells, as well as the functional ativation of mature cells
what is the alternative name of hematopoietic growth factors
colony stimulating factors
what are examples of hematopoietic growth factors
EPO, TPO, and GM-CSF
what is EPO and where is it produced
erythropoietin produced in the kidneys
what is TPO and where is it produced
thrombopoietin produced in the liver
what is GM-CSF and where is it produced
granulocyte-monocyte colony stimulating factor produced by endothelial cells
what is hematology
study of blood and blood-related disorders (inncluding their etiology, prevention, and treatment)
what do hematology nurses specialized in
caring for patients who are dealing with different kinds of blood related diorders, including educating them and their families
how are leukocytes classified
based on the presence or absene of enzyme containg cytoplasmic granules
what are the granulocytes and where do they circulate
neutrophils, eosinophils, and basophils that circulate in the blood
what are agranulocytes and where do they circulate
monocytes--circulate in the blood and lymphocytes (B cells, T cells, NK cells)--migrate between the blood and the lymphatic system
what is the most abundant white blood cell
neutrophils
what do the granules of neutrophils appear as when stained
stain lightly with both acidic and basic dyes, apperaring as a neutral pink
how are nuclei set up in neutrophils
nuclei are divided into 3-5 lobes
what is another name for neutrophils and what do they primarily do
polymorphonuclear leukocytes (PMNs) primarily respond to bacterial and fungal infections by phagocytosis and releasing enzymes (first line of defense)
what are the most abundant to least abundant leukocytes
neutrophils, lymphocytes, monocytes, eosinophils, then basophils
how do the granules of eosinophils stain
bright red with an acidic dye known as eosin
how are nuceli divded in eosinophils
divided into 2 lobes
what do eosinophils primarily respond to
primarily respond to parasitic infections by releasing enzymes and other molecules that are toxic to parasites
how do the granules of basophils stain
stain dark blue with a basic dye known as hematoxylin
how are nuclei divided in basophils
divided into 2 lobes
basophils primarily respond to what
allergens by releasing heparin (anticoagulant) and histamine (vasodilator), like mast cells in connective tissues
characteristics of granules in monocytes
lack distinct cytoplasmic granules
nuclei characteristics of monocytes
nuclei are kidney shaped
monocytes primarily do what
respond to bacterial infections by leaving blood vessels at the site of inflammation and transforming into tissue macrophages that pahgocytose bacteria
lymphocytes are similar in size to what
red blood cells
granule characteristics in lymphocytes
lack distinct cytoplasmic granules
characteristics of nuclei in lymphocytes
nuclei are spherical
lymphocytes primarily respond to what
viral infections-B cells and T cell are part of the adaptive immune system (highly specific to a pathogen), but NK cells are part of the innate immune system (not specific)
lymphocytes are what kind of cell and where to the mature and travel to
B cells; mature in the bone marrow, and then travel to the lymph nodes and spleen
upon interaction with a specific pathogen , naive B cells tranform into what
effector B cells; most effector B cells transform into plasma cells and some effector B cells transform into memory B cells
what do plasma cell produce when they are transformed from effector B cells
produce and secrete large volumes of antibodies into the circulation that bind to and destory the pathogen
what can memory B cells recognize
returning pathogens
what do B cells provide
humoral adaptive immunity
T cells leave what and travel where
leave the bone marrow as precursor T cells, travel to the thymus for maturation, and then travel to the lymph nodes and spleen
upon interaction with a specific pathogen naive T cells transform into what
effector T cells
CD4+ helper T cells do what
help plasma cells (terminally differentiated B cells) produce and secrete antibodies
CD8+ cytoxic T cells do what
kill intracellular pathogens some effector T cells transform into memory T cells that can recognize returning pathogens
T cells provide what
cell mediated adaptive immunity
NK cells are present where and do what
blood, lymph nodes, and spleen; recognize, bind to, and kill cells that are infected with intracellular pathogens
what cells may play a role in cancer surveillance and control
NK clls
NK cells provide what
innate (inborn) immunity
what are the central (primary) lymphoid tissues
bone marrow and thymus
what happens in bone marrow as a lymphoid tissue
development of lymphocyte progenitor cells and maturation of B cells
what happens in the thymus as a lymphoid tissue
maturation of T cells
what are the peripheral (secondary) lymphoid tissues
lymph nodes, spleen, and mucosa associated lymphoid tissue (MALT)
components of the spleen as they relate to lymphoid tissues
white pulp contains concentrated areas of B and T cells, whereas the red pulp contains blood vessels and acts as a filter by removing pathogens and senescent erythrocytes
mucosa associated lymphoid tissue are located where
GI tract, respiratory tract, and genitourinary system
where are t cells located in the lymph node structure
pericortex
what are non-neoplastic disorders
noncancerous disorders of WBCs
disorders that involve what are most common and what are some examples
neutrophils and lymphocytes; neutropenia, neutrophilic leukocytosis, lymphocytopenia, and lymphocytic leukocytosis
disorders that involve what or what are relatively less common and disorders that involve what are rare
monocytes or eosinophils; basophils
what is neutropenia
abnormally low number of neutrophils
severe reduction of neutrophils to less than 100/ml is what
agranulocytosis
what is the etiology of neutropenia
cancer chemotherapy and radiation therapy, autoimmune disorders, and overwhelming bloodstream ifnection that uses up neutrophils faster than they can be produced
patients become prone to what in neutropenia
recurrent infections (usually bacterial or fungal)--infections may last for a long time and utreated infections can sometimes be fatal
what is the characteristic feature of neutropenia
lack of pus formation at the site of infection and or signs of inflammation, both of which require an adequate number of neutrophils
what is the treatment of neutropenia
antimicrobial agents, specific hematopoietic growth factors
what is neutrophilic leukocytosis
abnormally high number of neutrophils
what is the most common cause of neutrophilic leukocytosis
normal response of the body to a bacterial or fungal infection
what is the etiology of neutrophilic leukocytosis
injuries such as fractures or burns and autoimmune disorders
what are the specific signs and symptoms of neutrophilic leukocytosis
none
what is the treatment of neutrophilic leukocytosis
focus on underlying cause
what is the definition of lymphocytopenia
abnormally low number of lymphocytes
lymphocytopenia may be what
acute (temporary) or chornic (long-term)
what is the etiology of lymphocytopenia
cancer chemotherapy and radation therapy, autoimmune disorders, periods of severe malnutrition, and chronic infections like HIV and disseminated TB
patients become prone to what in lymphocytopenia
recurrent infections (usually viral), infections may last for a long time, and untreated infections can sometimes be fatal
how does diagnosis occur for lymphocytopenia
usually by chance when a complete blood count is done for some other reason
in lymphocytopenia, decreases could involve what
B cells, T cells or NK cells
what is the treatment for lymphocytopenia
antimicrobial agents, gamma globulins (substances rich in antibodies) to prevent recurrent infections
what is lymphocytic leukocytosis
abnormally high number of lymphocytes
lymphocytic leukocytosis increases could involve what
B cells, T cells or NK cells