Bootcamp.com - Respiratory System (10)
1/128
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
129 Terms
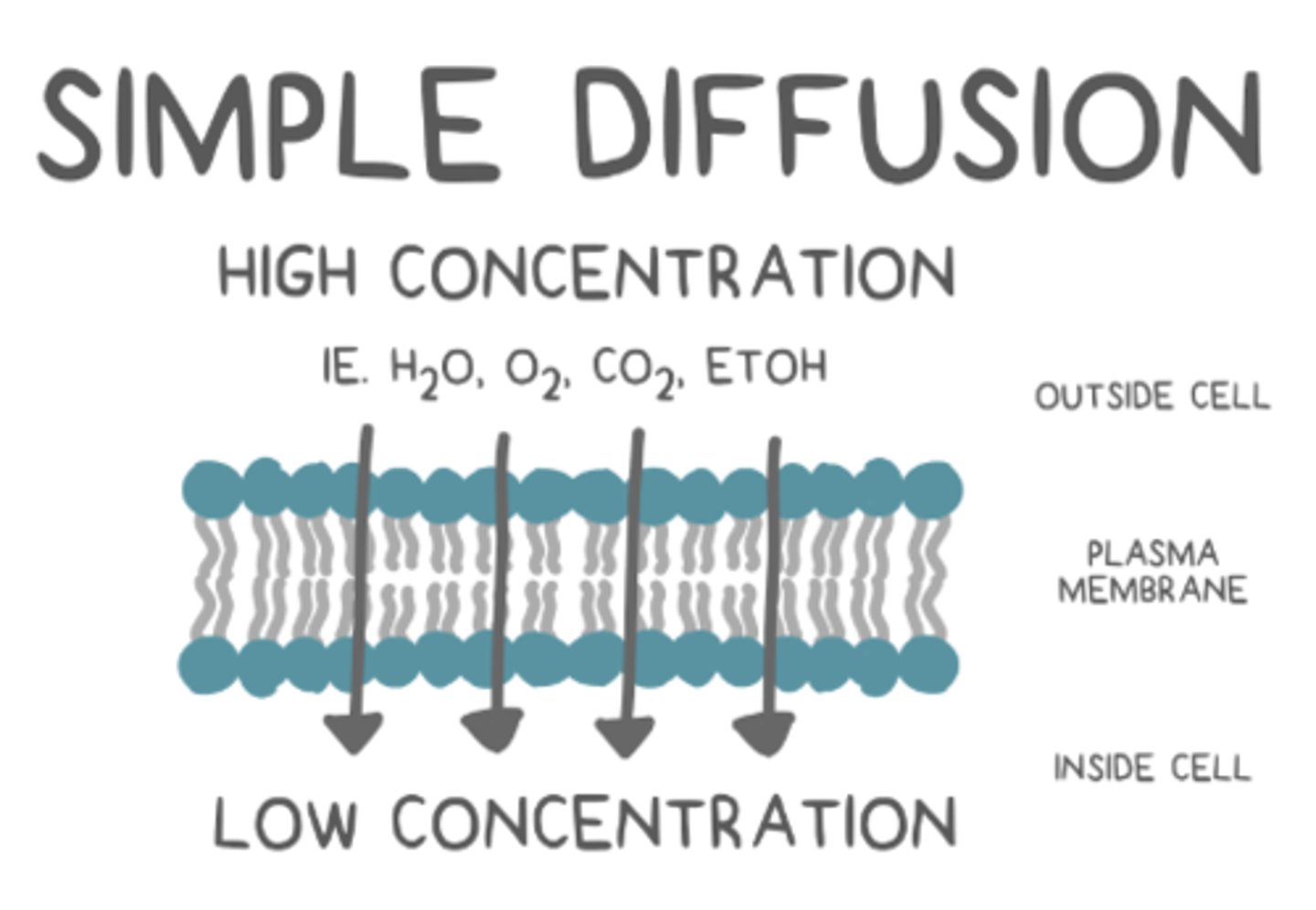
what are the traits of an organism that exchanges gases via simple diffusion?
large surface area of cells in direct contact with moist environment
cnidaria use _____ as their means of gas exchange
simple diffusion
_____ is where molecules travel across a selectively permeable membrane by concentration gradients
simple diffusion
annelida use _____ as their means of gas exchange
simple diffusion
how do earthworms keep their skin moist for simple diffusion?
they secrete and coat themselves in a mucus
arthropoda have _____ to transport a small amount of gasses
hemolymph
what feature do insect tracheal tubes have to enhance gas exchange?
they are moistened at the end to allow oxygen to diffuse in and carbon dioxide to diffuse out
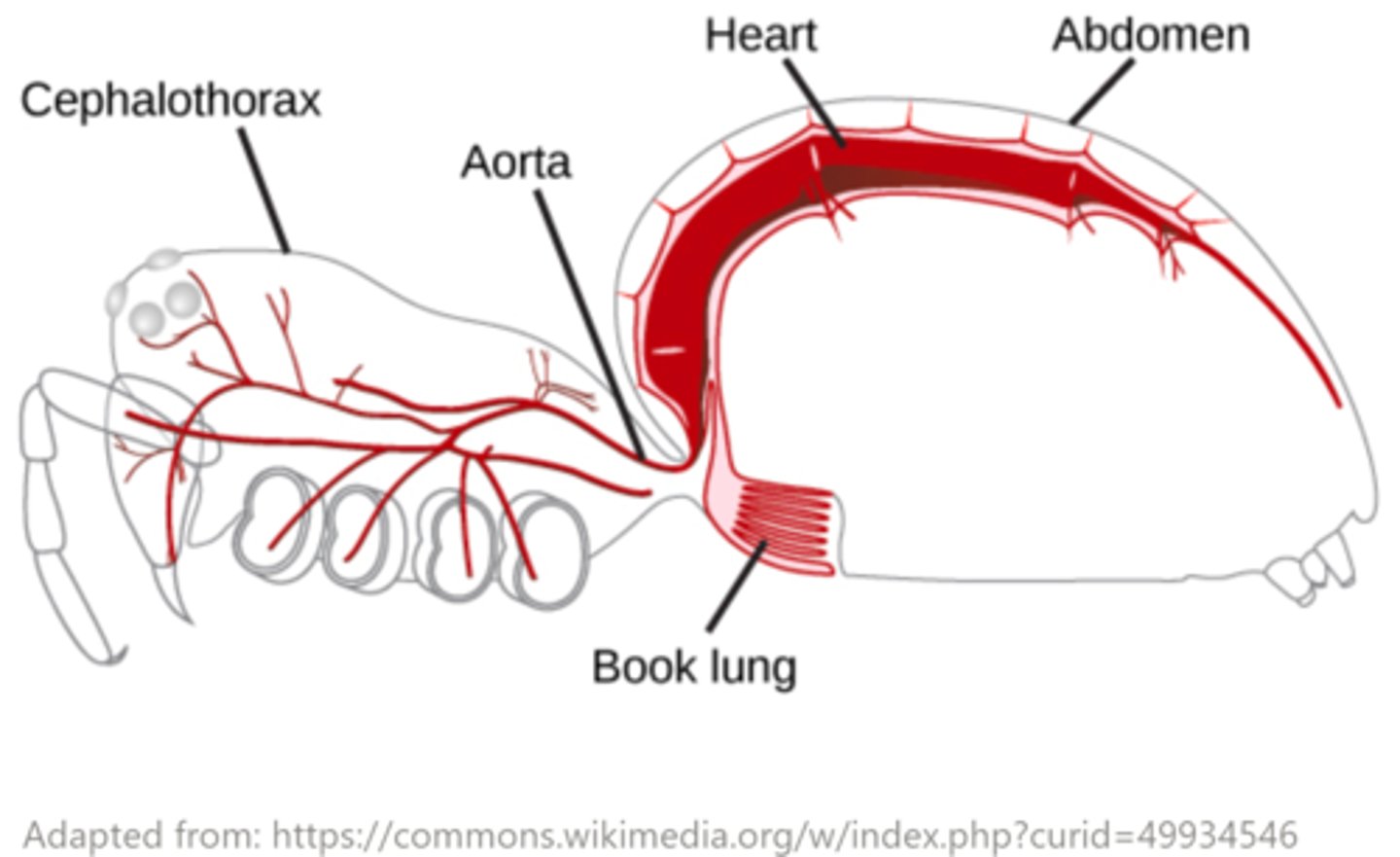
what is the function of arachnid book lungs?
their flat vascularized sheet membranes provide a large surface area for respiration
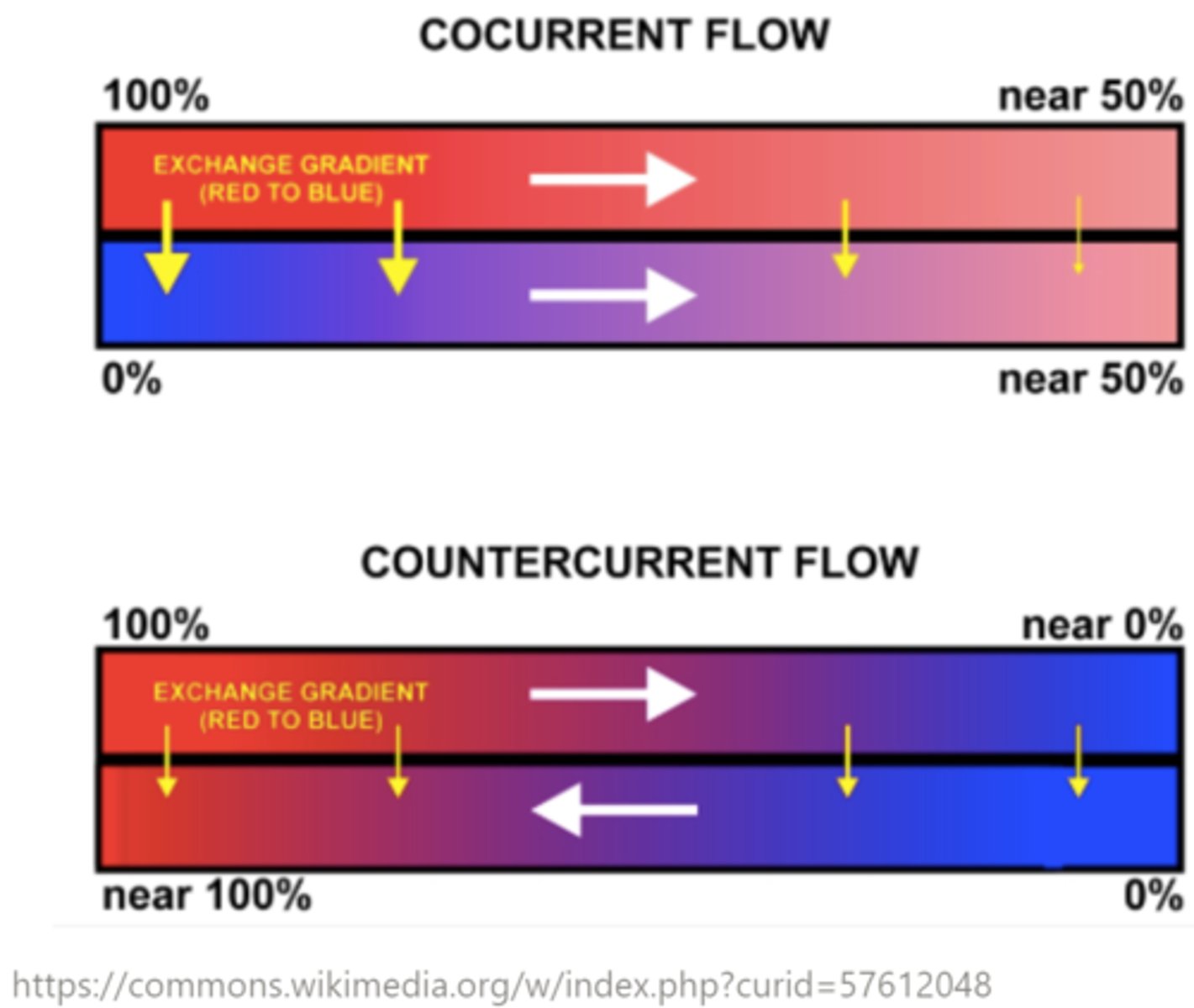
gills have a large surface area for the _____ (concurrent/countercurrent) exchange of gases between the blood and water
countercurrent
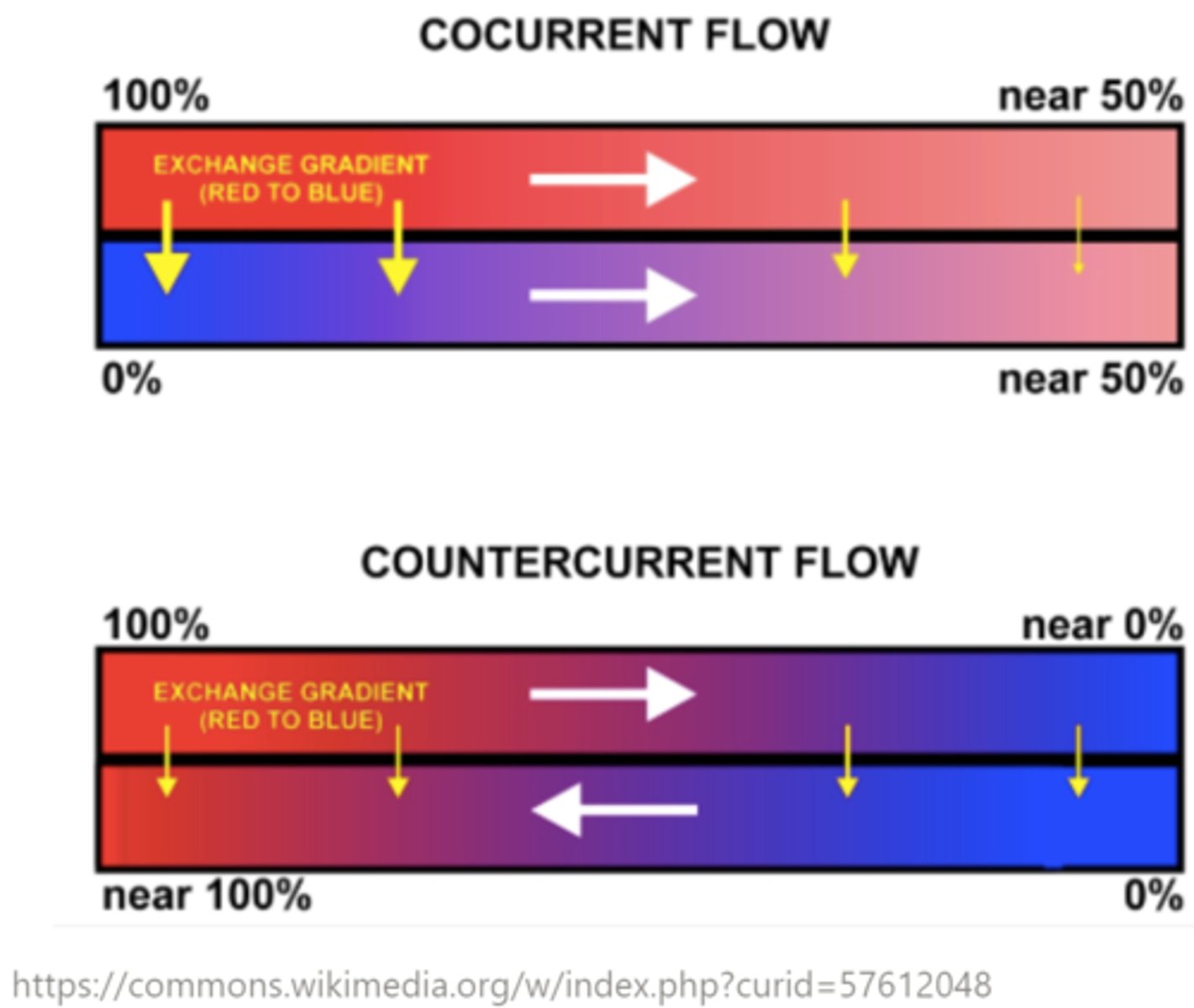
_____ is the gas exchange mechanism where fluids flow in different directions
countercurrent exchange
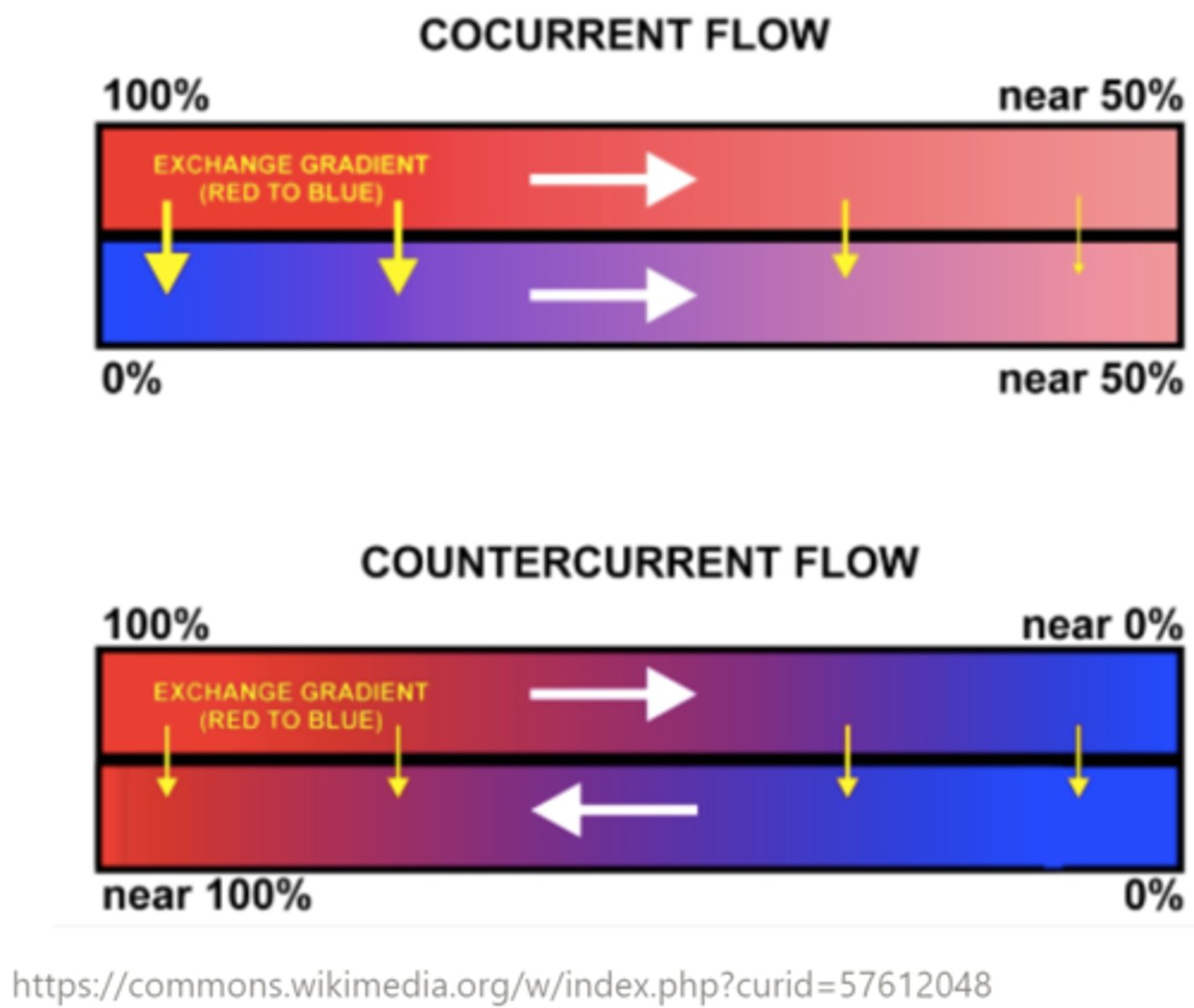
_____ is the gas exchange mechanism where fluids move in the same direction
concurrent flow
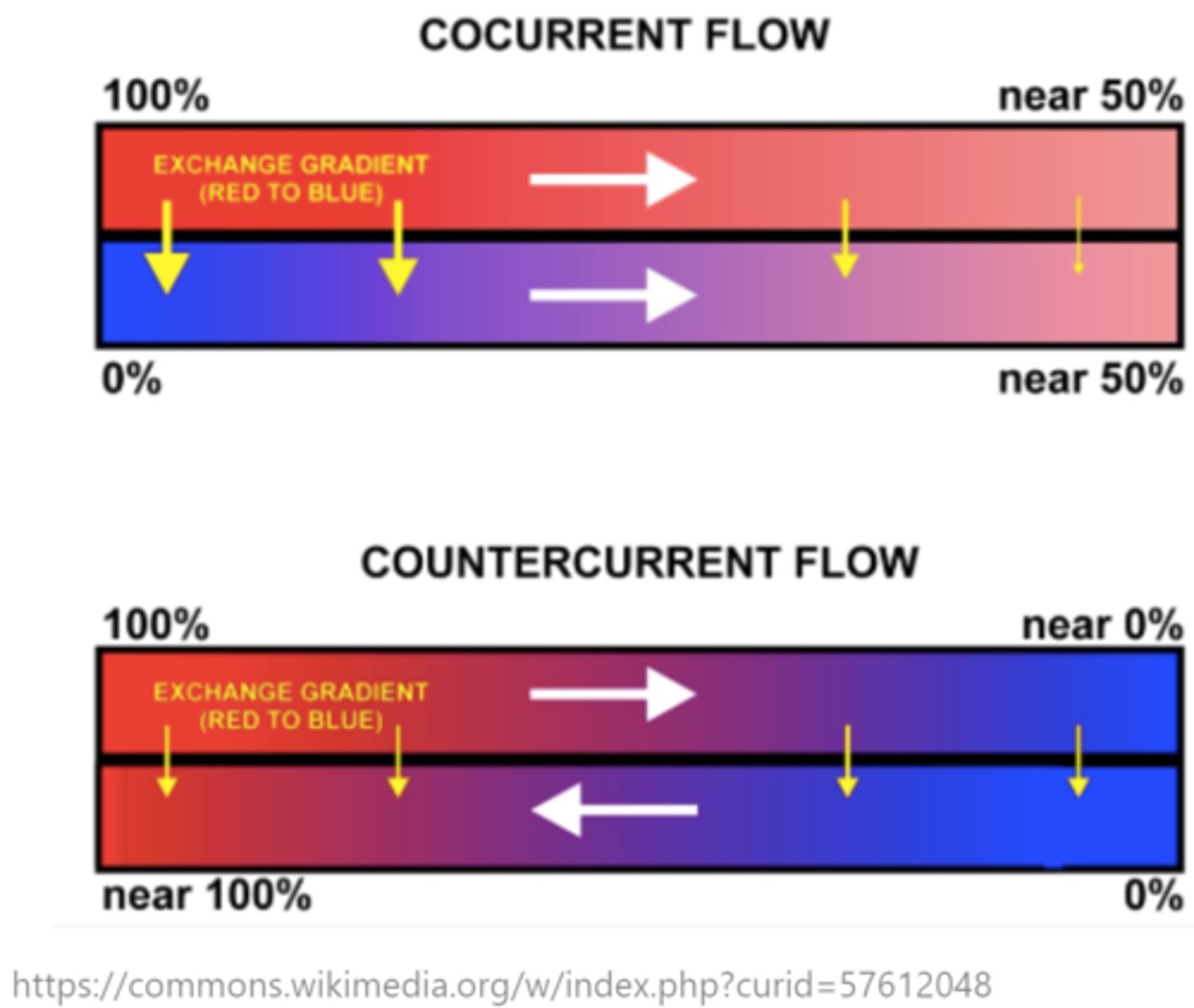
Which is best for diffusion: concurrent or countercurrent exchange?
countercurrent; it creates a stronger diffusion gradient than concurrent exchange that allows more O2 to enter the blood and more CO2 to leave
lungs function based on _____ and _____ manipulations
pressure; volume
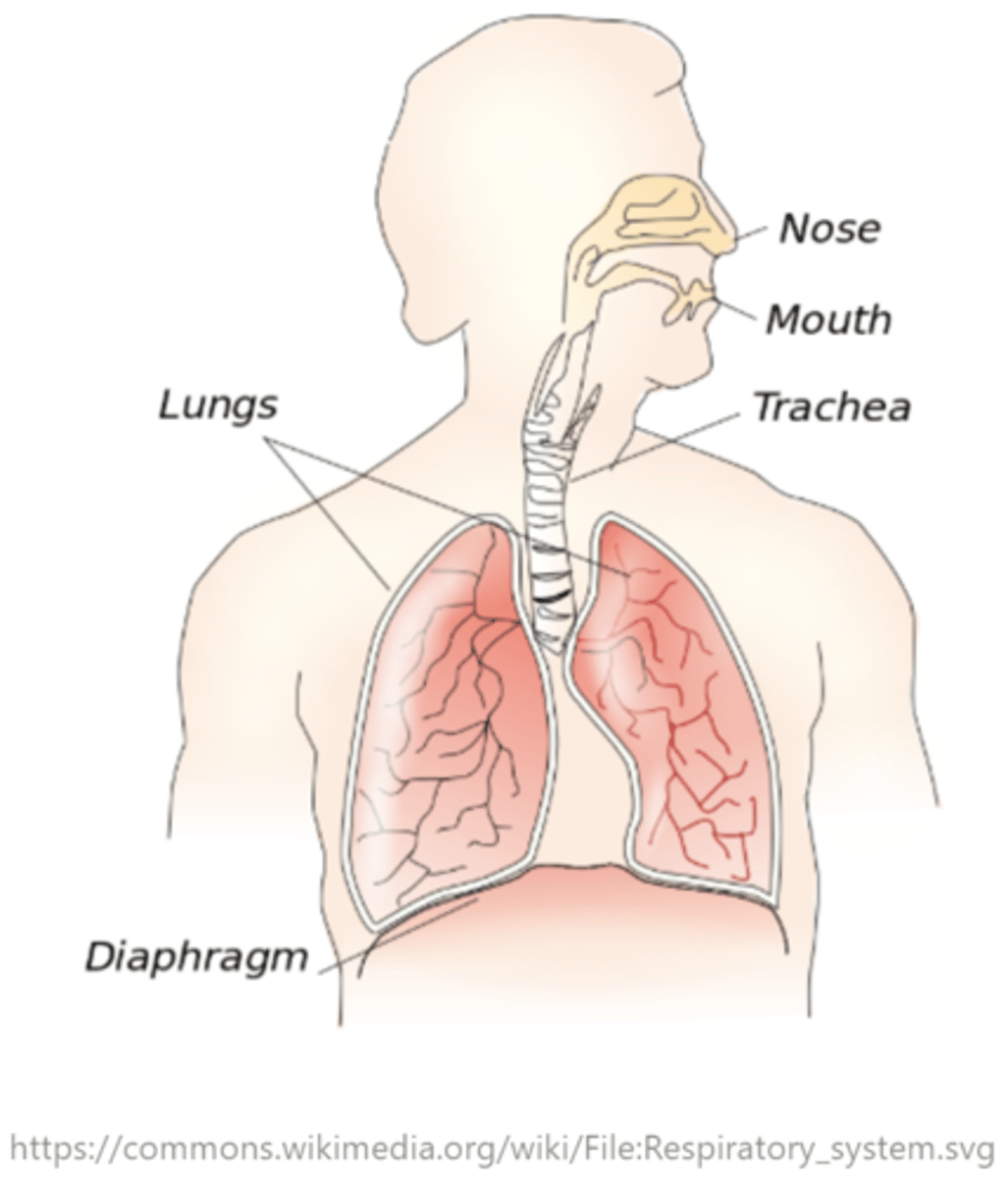
where are lungs found?
thoracic cavity; surrounded by the rib cage
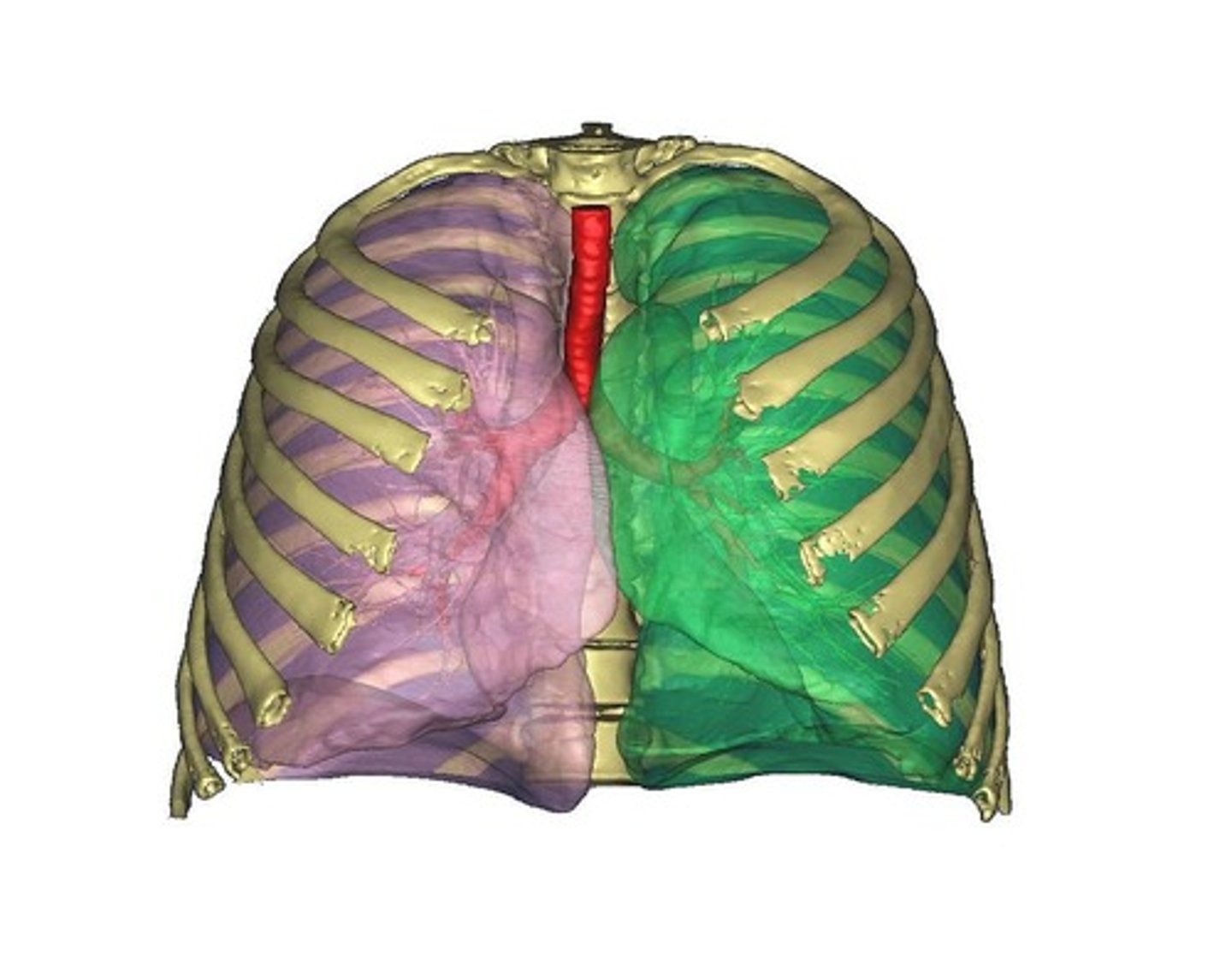
which lung is larger - why?
right; the left lung is smaller to make room for the heart
how many lobes does the right lung have?
3
how many lobes does the left lung have?
2
the _____ is a dual layered membrane that covers each lung
pleura
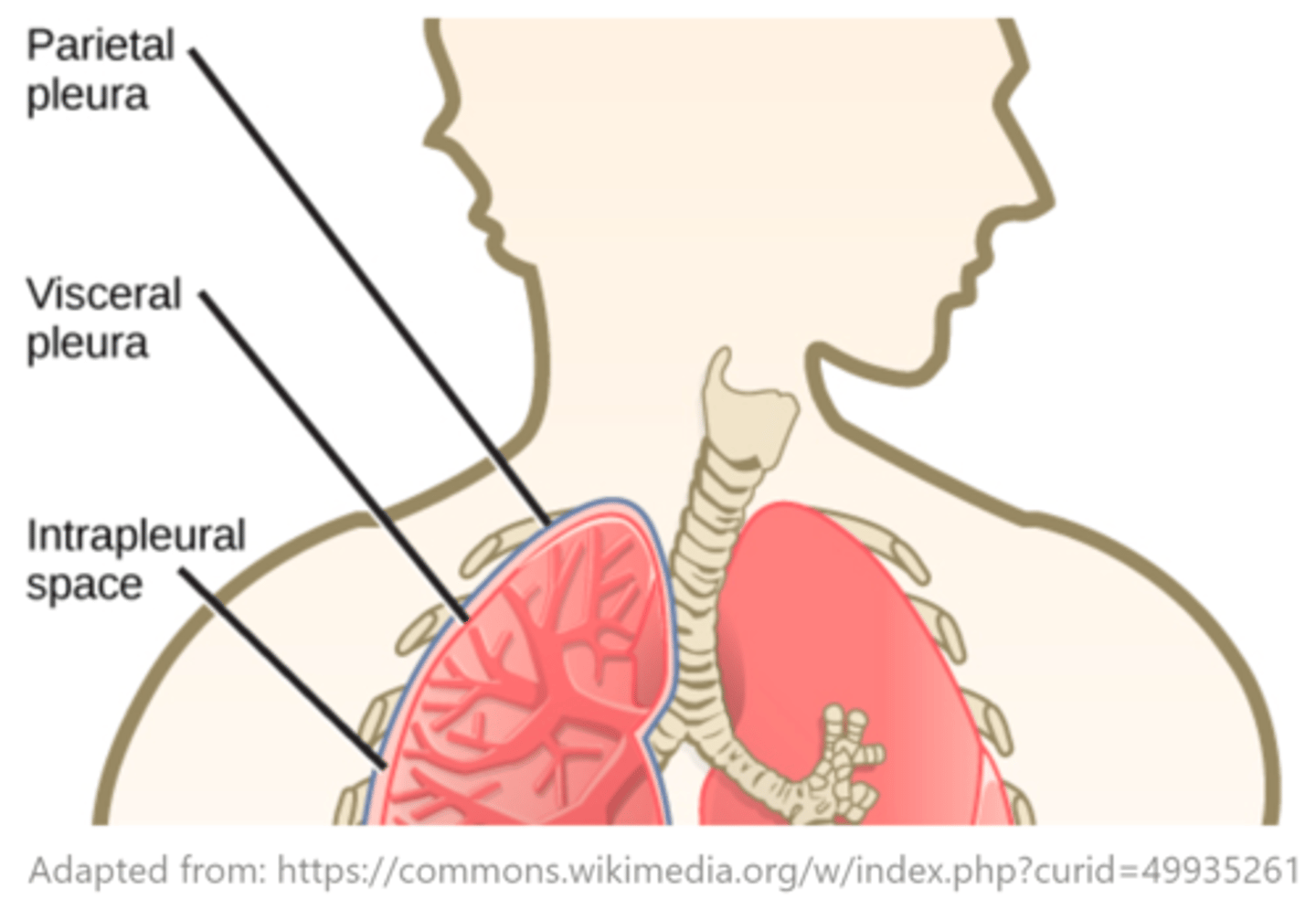
the _____ is the outer layer of the pleura, which makes contact with the thoracic cavity
parietal layer
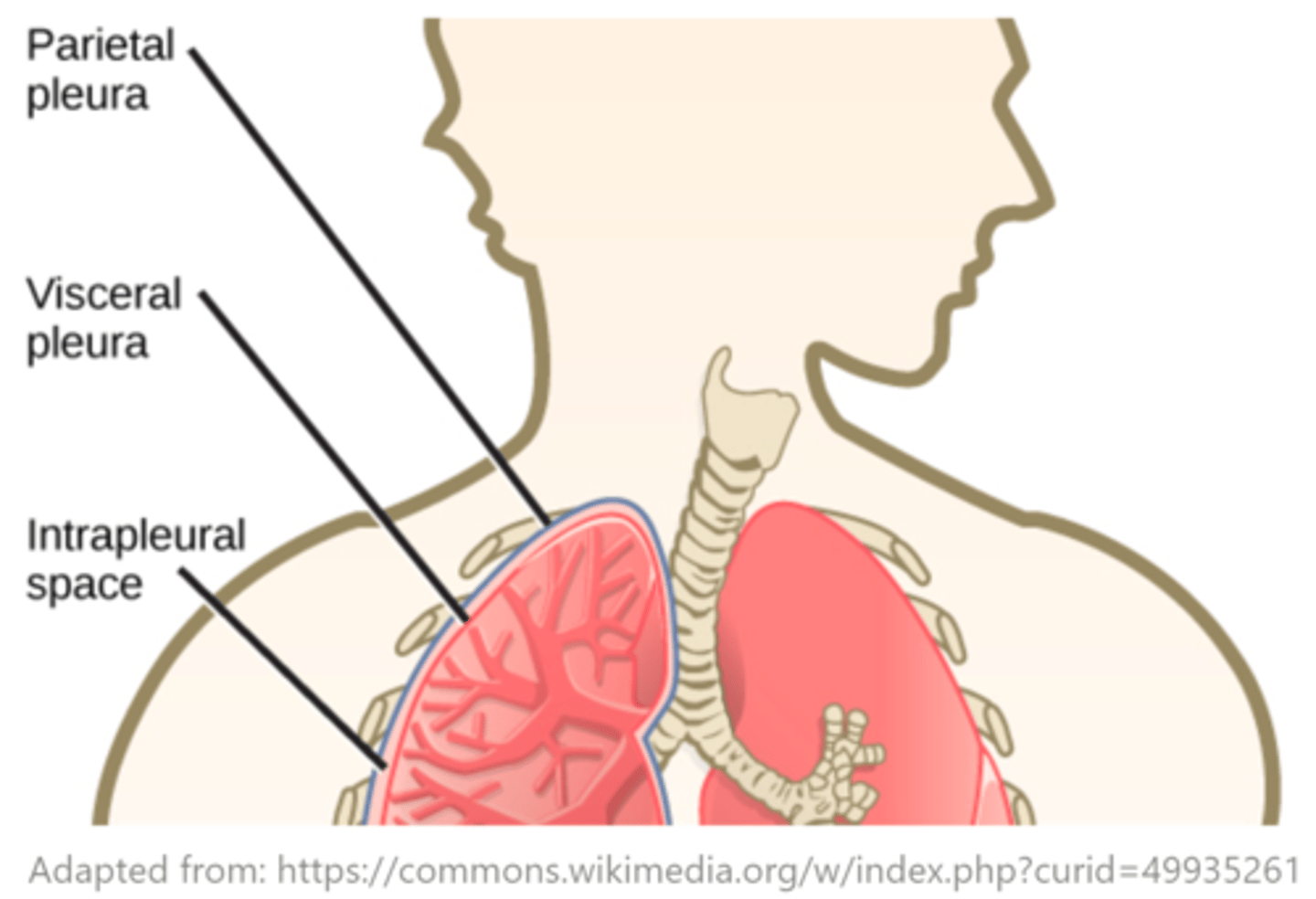
the _____ is the inner layer of the pleura, which makes contact with the lungs
visceral layer
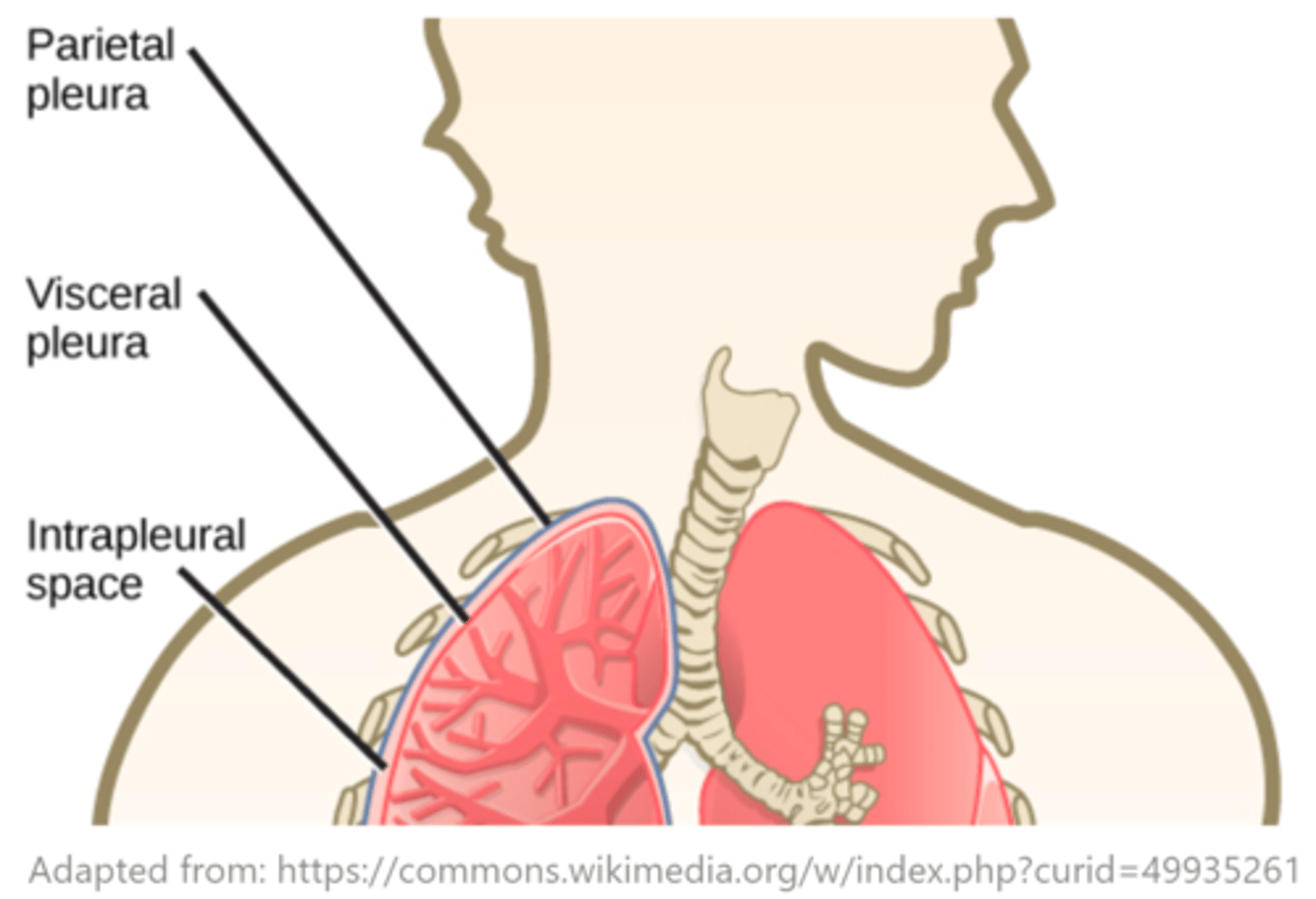
what is the space between the parietal and visceral layers of the pleura?
pleural space
(intrapleural space)
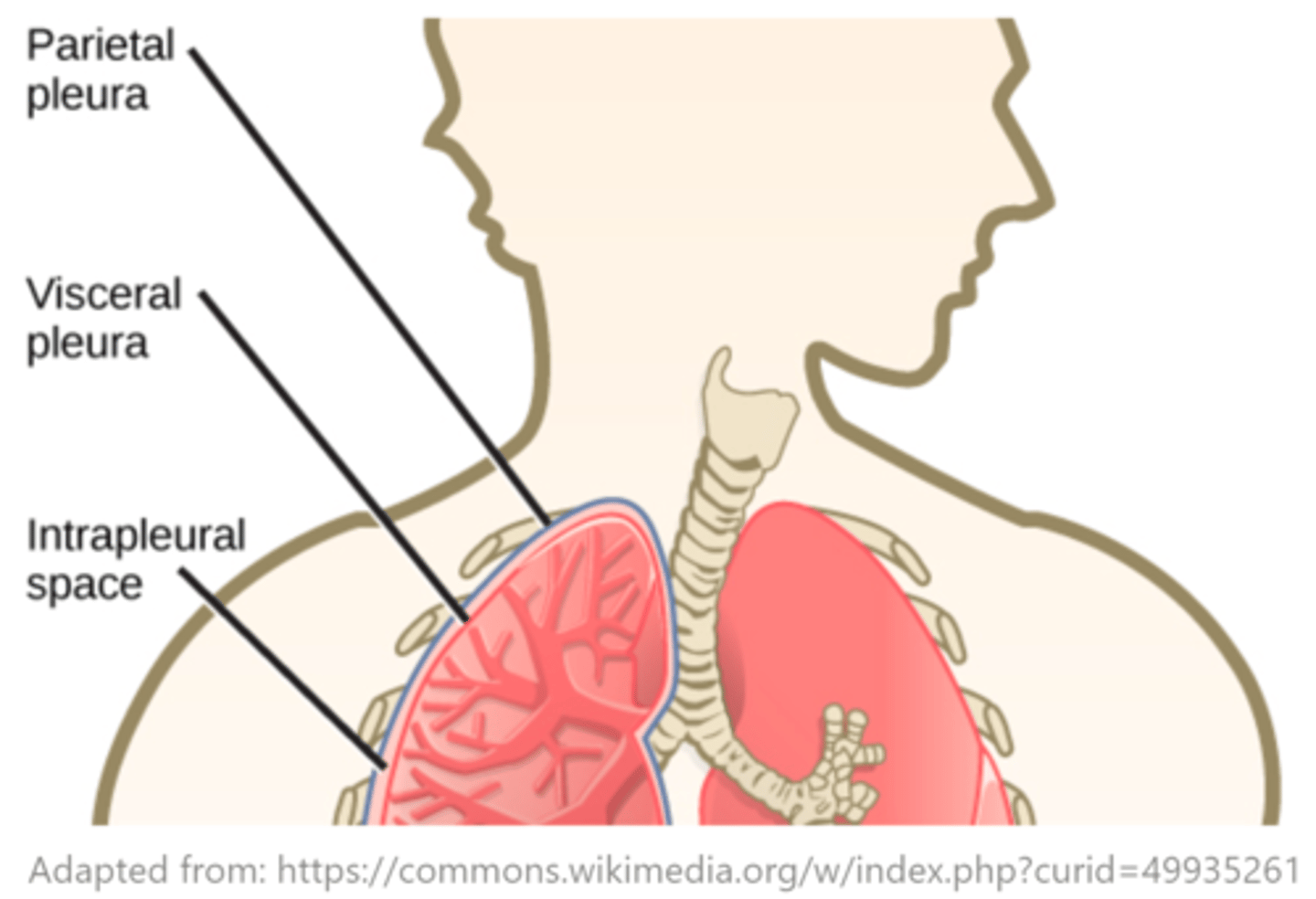
the pleural space contains a fluid that is always at a _____ (lower/higher) pressure than atmospheric pressure
lower
what is the name of the pressure within the pleural space?
intrapleural pressure
what is the function of intrapleural pressure?
it prevents the lungs from collapsing
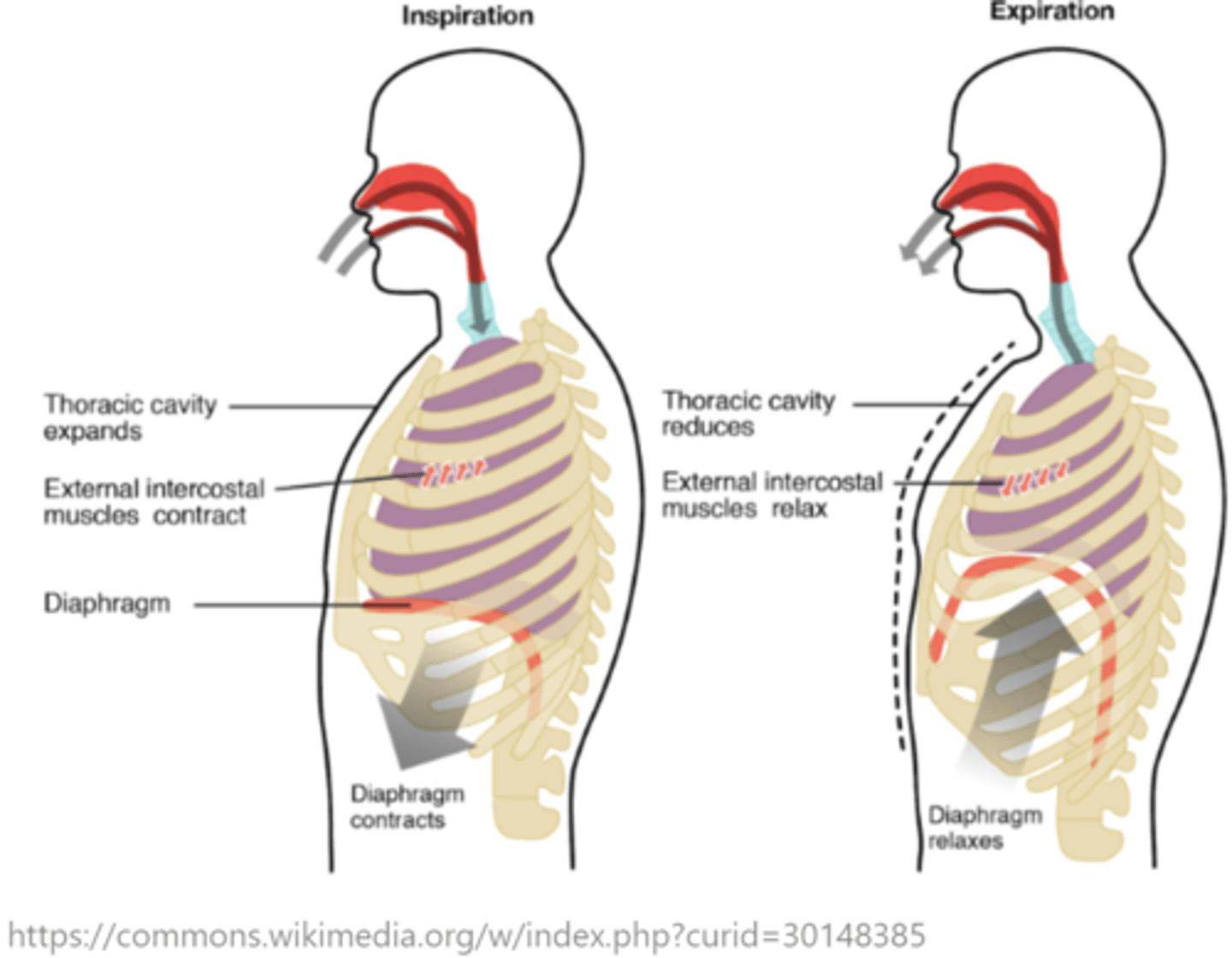
increasing the volume of the _____ is responsible for moving air into the lungs
thoracic cavity
the _____ is a large skeletal muscle at the bottom of the lungs
diaphragm
the diaphragm is innervated by the _____ nerve
phrenic
what is the result of the diaphragm contracting during inhalation/inspiration?
it pulls the lungs downward
the diaphragm and external intercostal muscles contract during _____
inhalation/inspiration
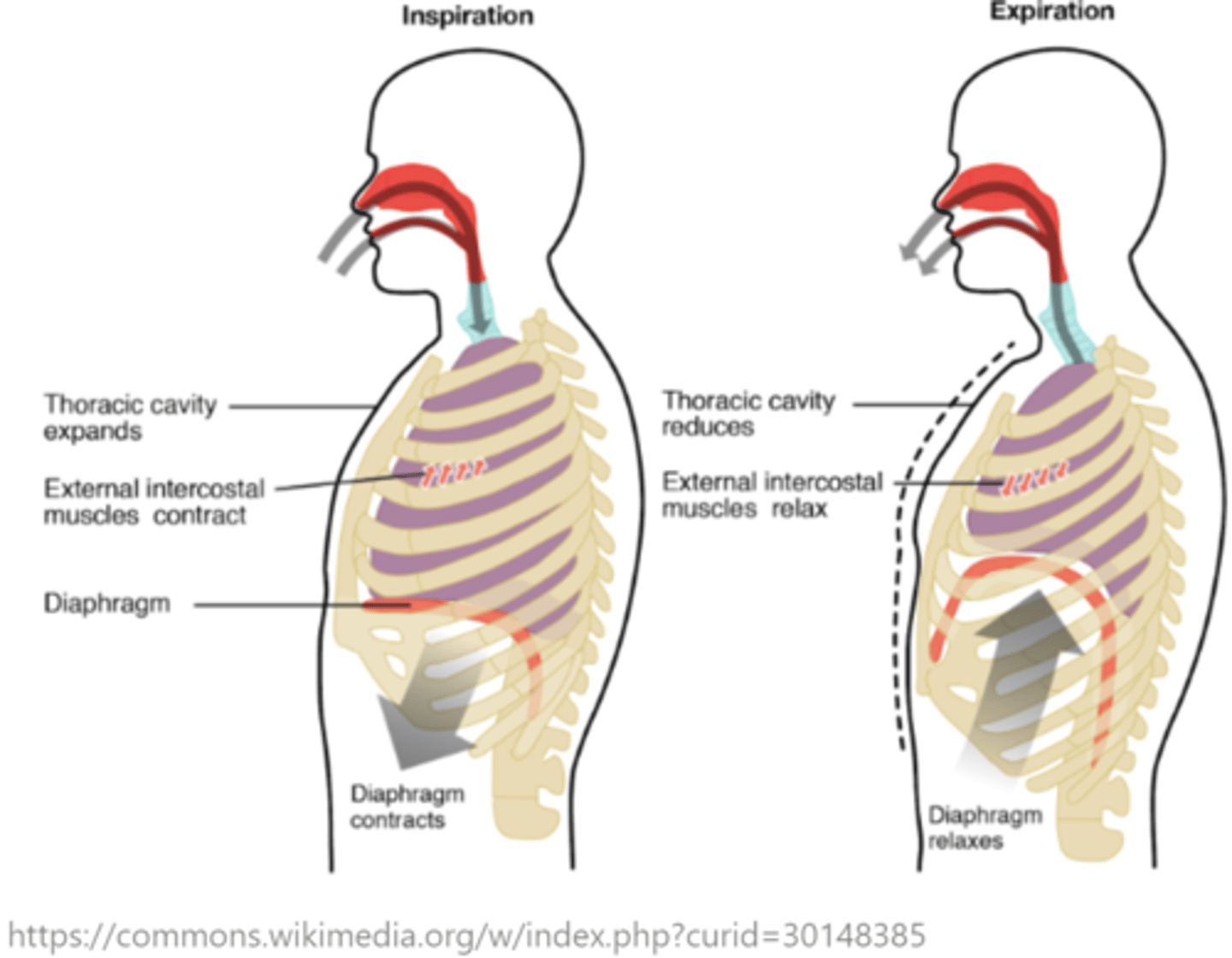
the volume _____ (increases/decreases) during inhalation/inspiration
increases
pressure in the intrapleural space _____ (increases/decreases) during inhalation/inspiration
decreases
volume and pressure are _____ related
inversely
what is the purpose of pulmonary surfactant?
it decreases the surface tension in the lungs, which making inspiration less challenging
the _____ and _____ muscles relax during exhalation/expiration
diaphragm; external intercostal
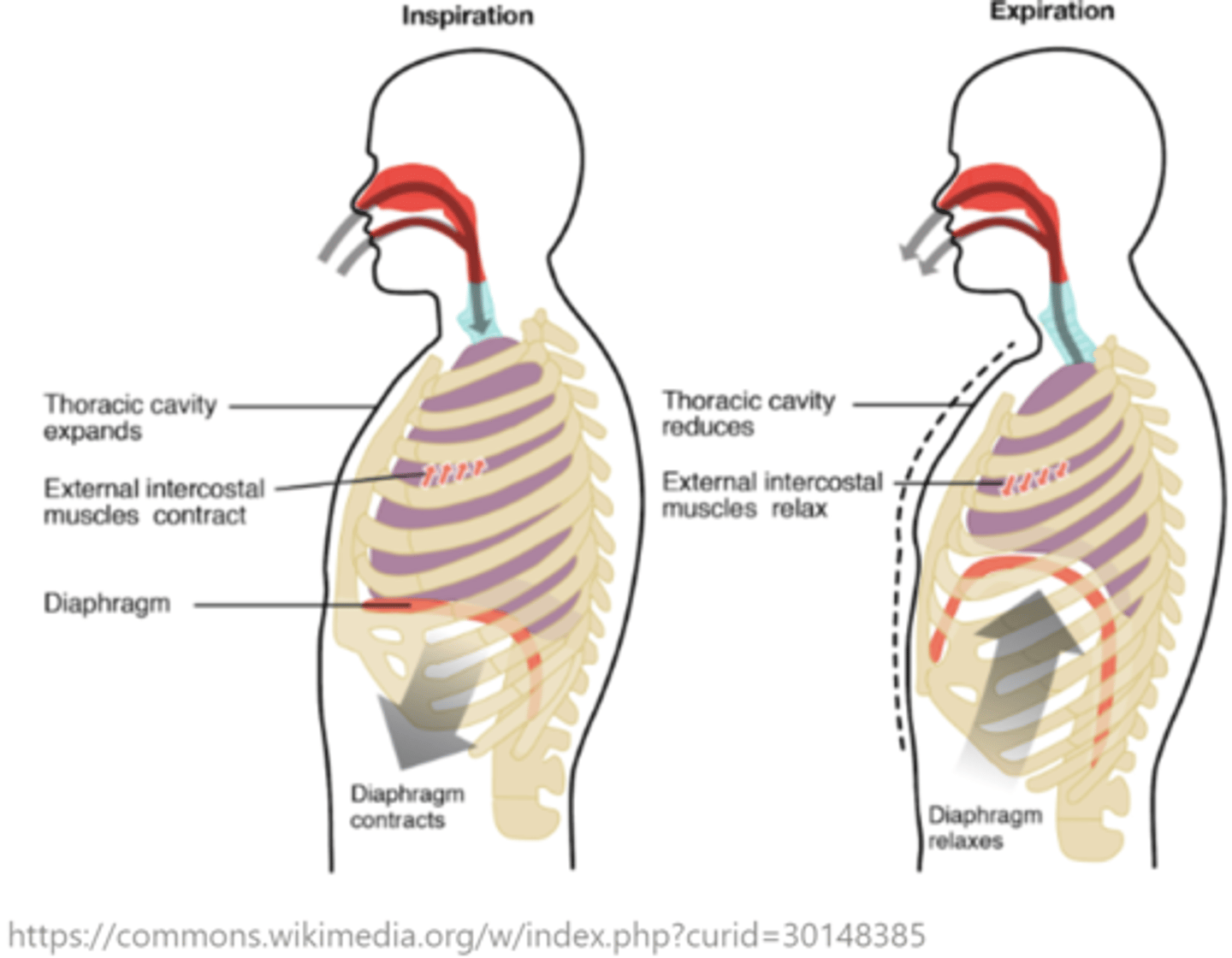
volume decreases during _____
exhalation/expiration
_____ increases during exhalation/expiration
pressure
which intercostal muscles contract to help with exhalation/expiration?
internal intercostals
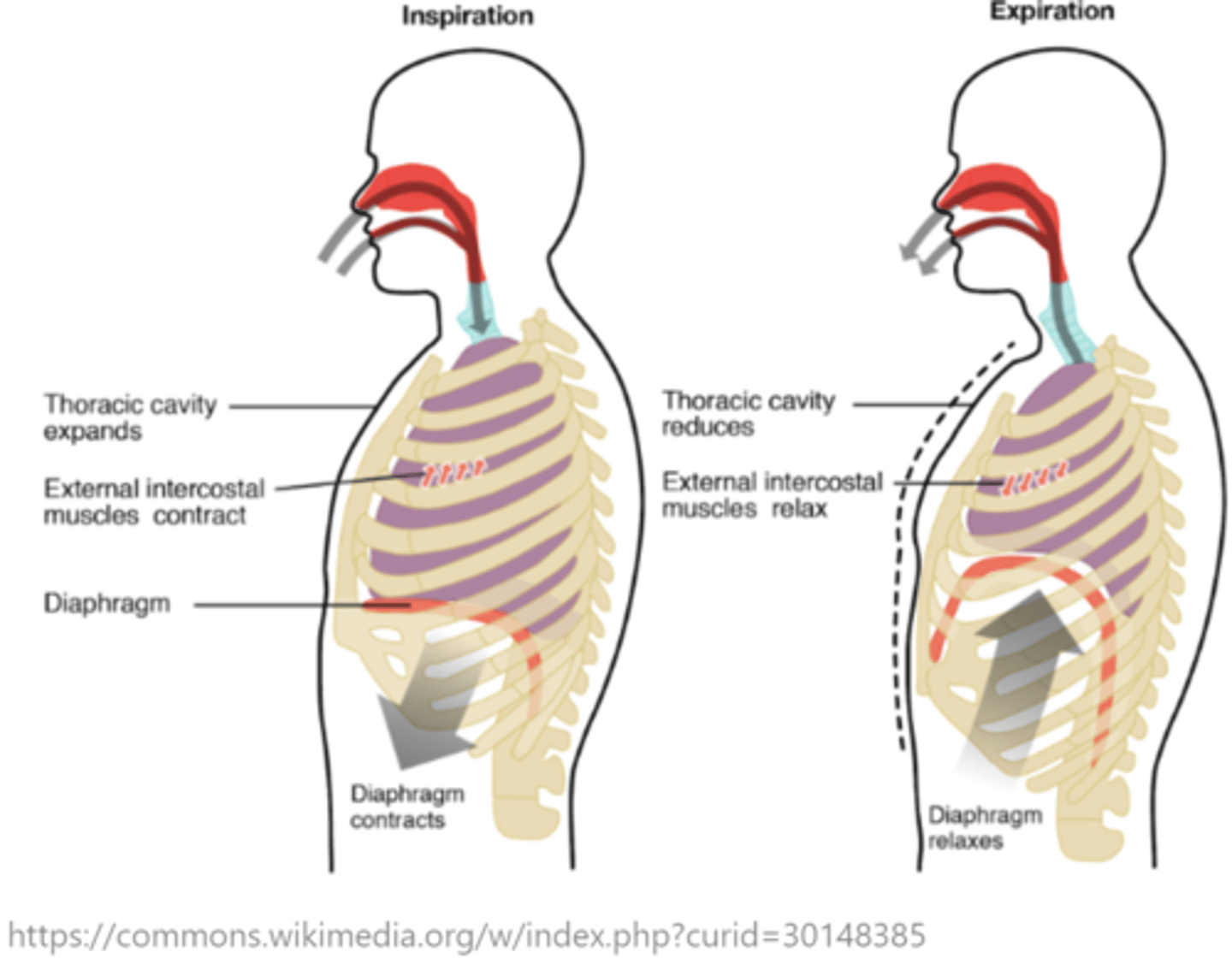
which intercostal muscles contract to help with inhalation/inspiration?
external intercostals
at the beginning of inspiration, the intrapleural pressure begins to _____ (increase/decrease)
decrease
when is intrapleural pressure most negative?
peak inspiration
at the beginning of exhalation, the intrapleural pressure begins to _____ (increase/decrease)
increase
(become less negative)
when is intrapleural pressure least negative?
peak expiration
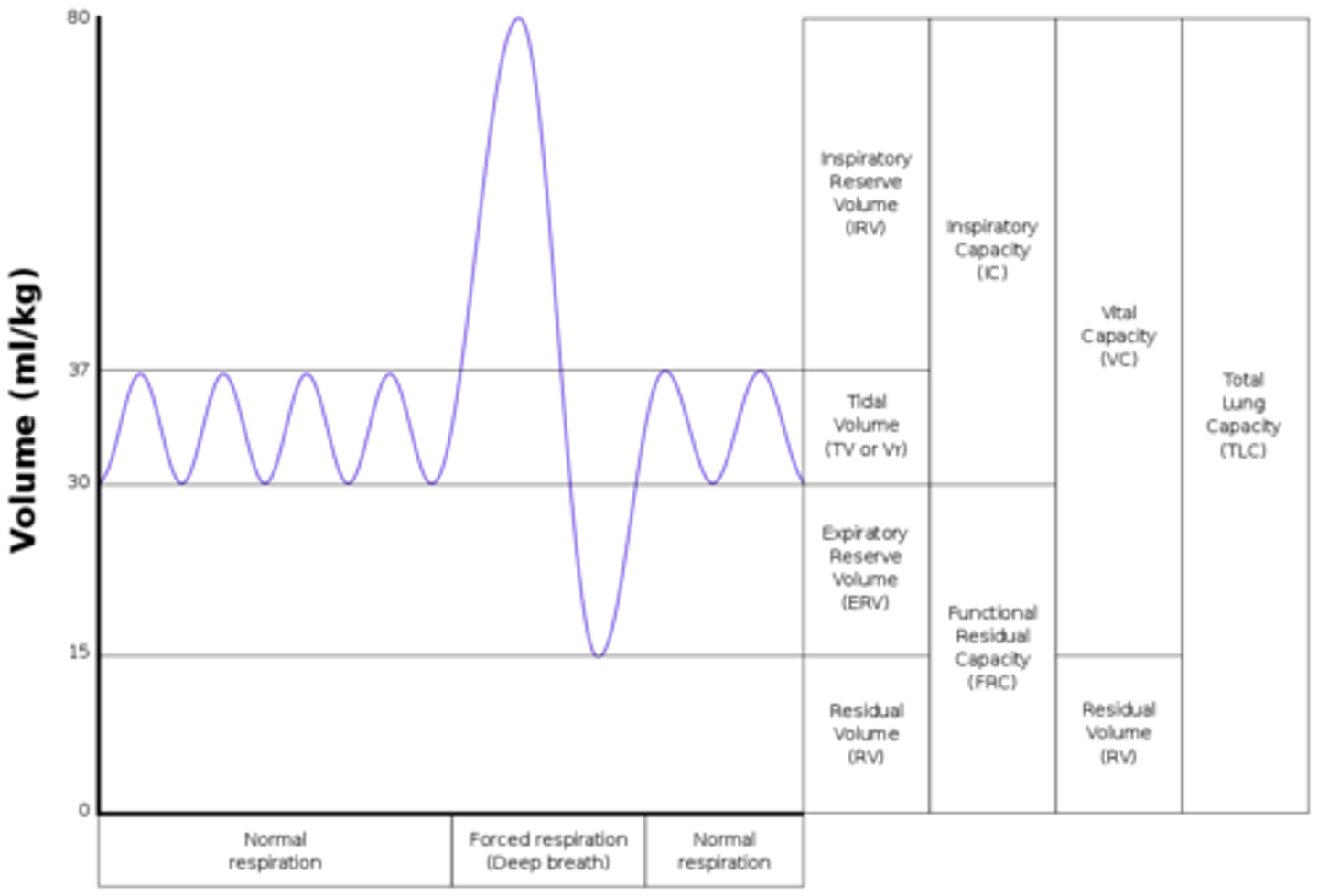
what is tidal volume?
the volume of air moving through the lungs during normal breathing
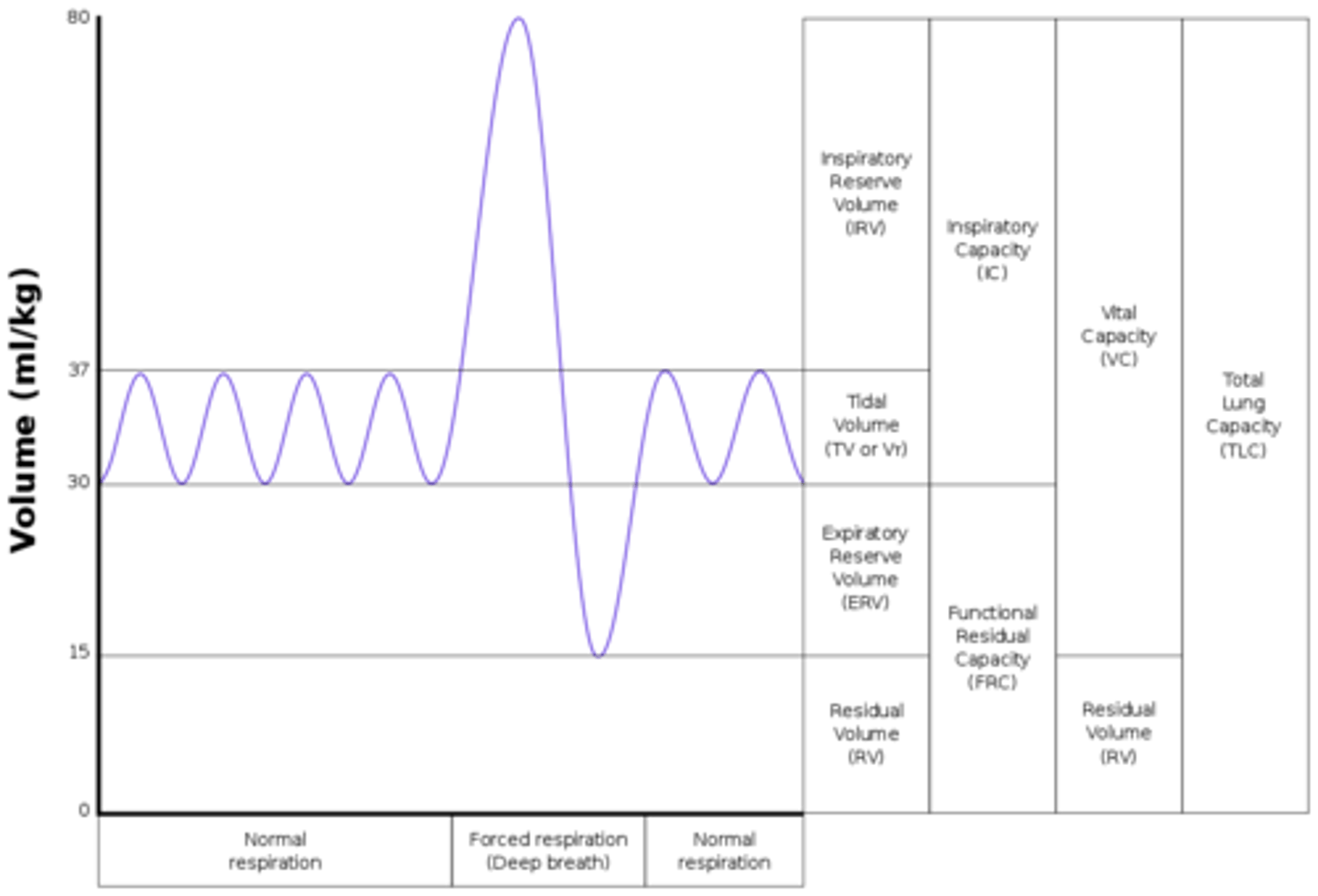
more forceful inhalations allow more air to be inspired than usual (above tidal volume) - what is this volume known as?
inspiratory reserve volume
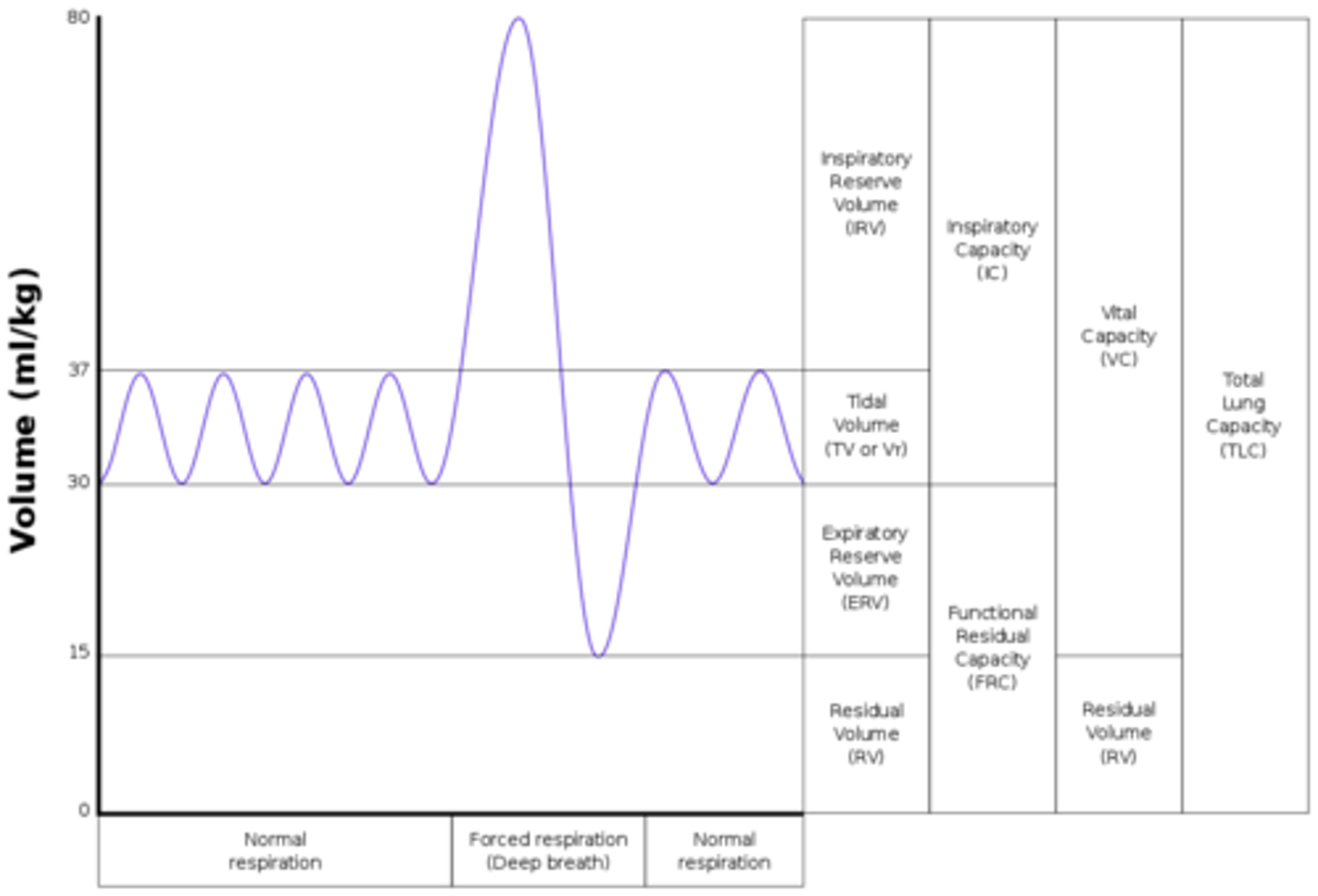
what is the volume of air left in the lungs after a normal tidal exhalation?
functional residual capacity
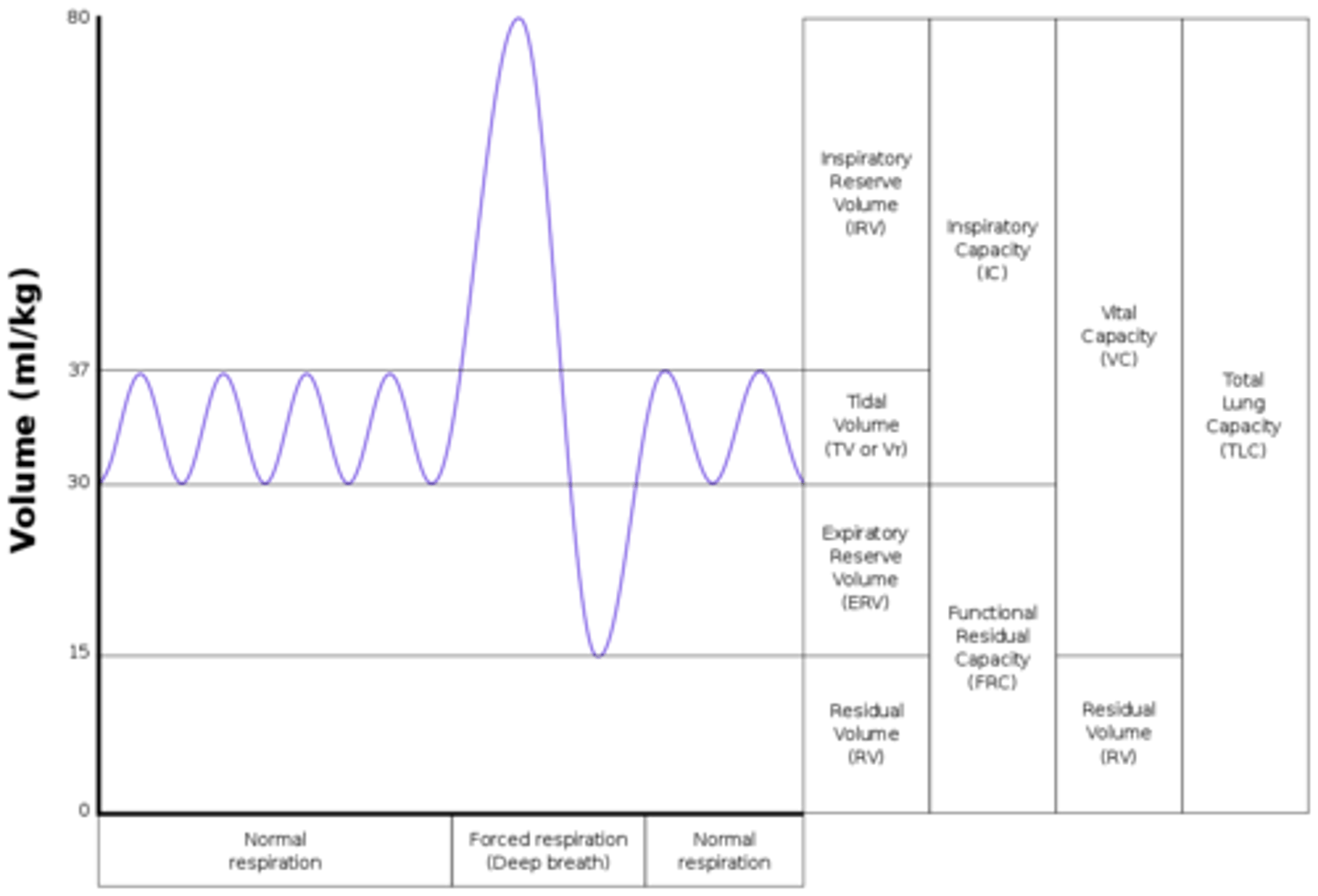
more forceful exhalations allow more air to be expired than usual (below tidal volume) - what is this volume known as?
expiratory reserve volume
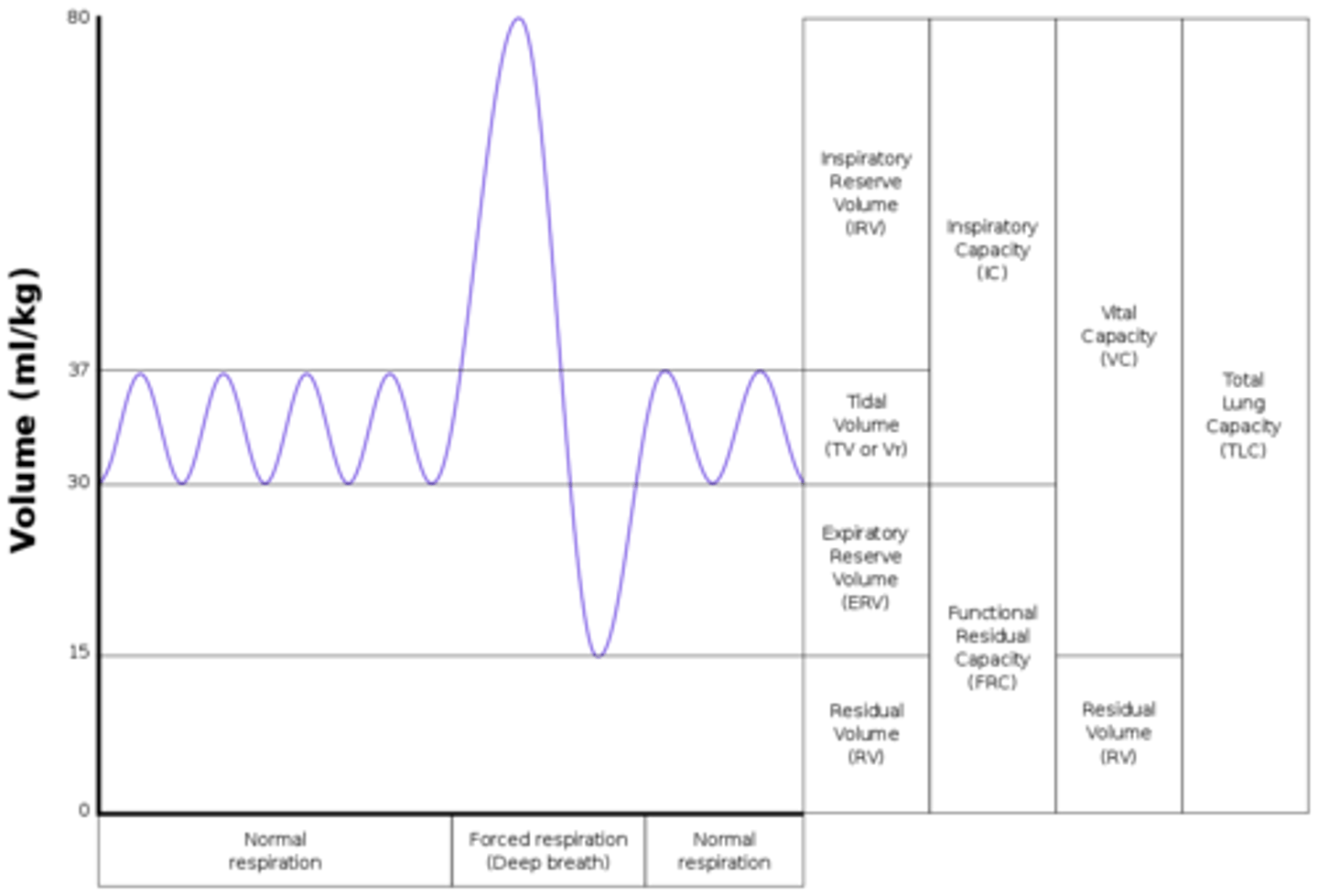
what is the maximum volume of air that could be expired after maximum inhalation?
vital capacity
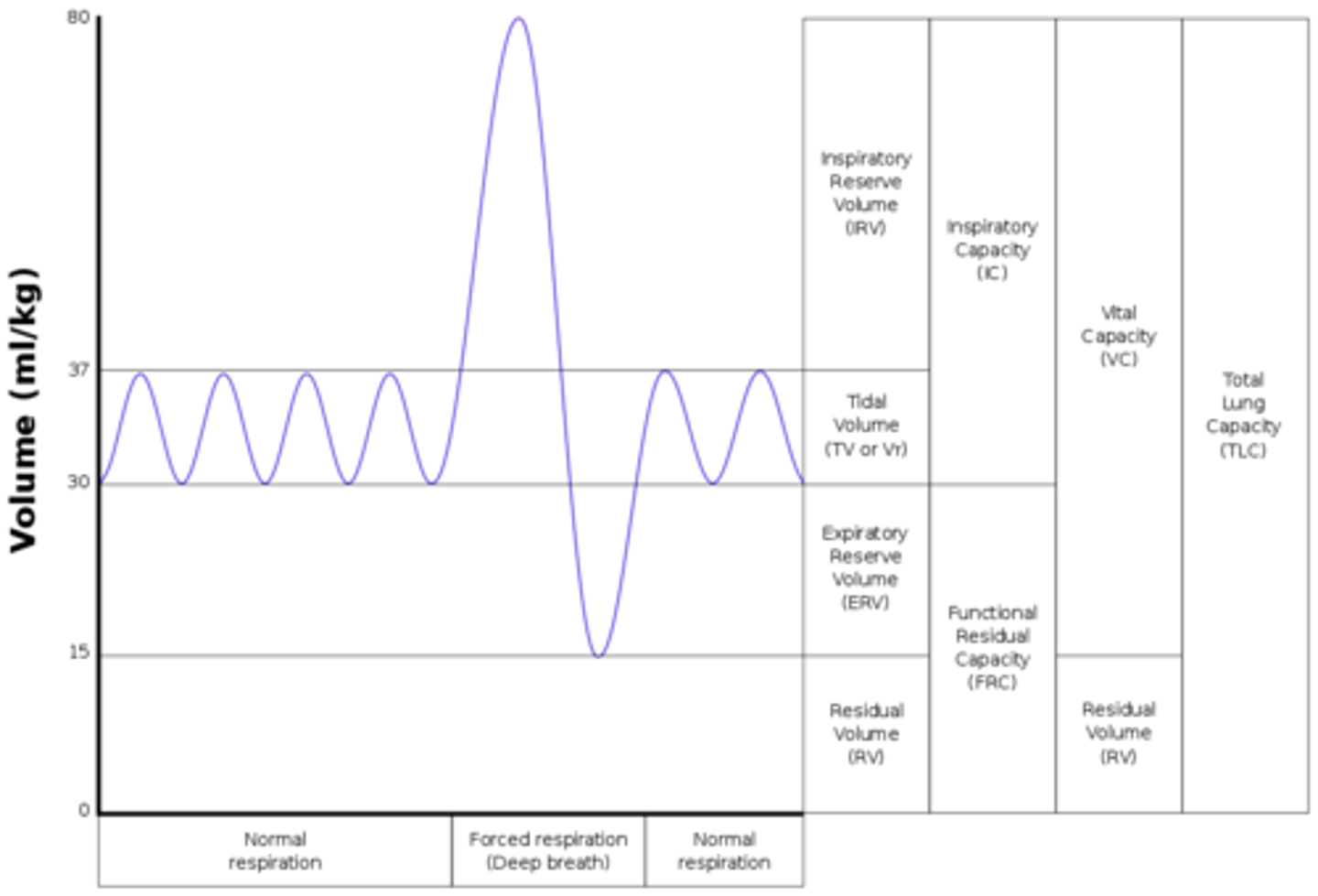
what is the volume the lungs could theoretically hold?
total lung capacity
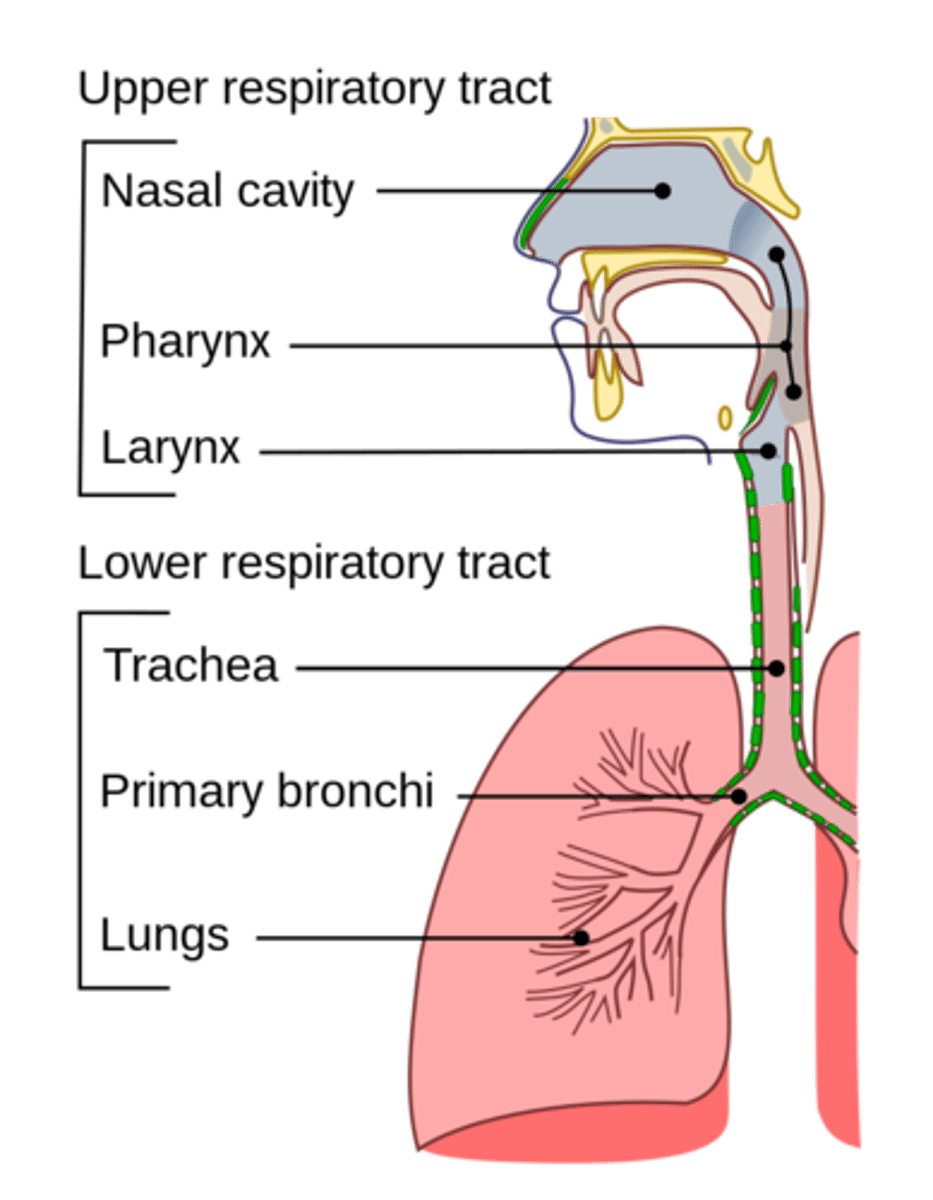
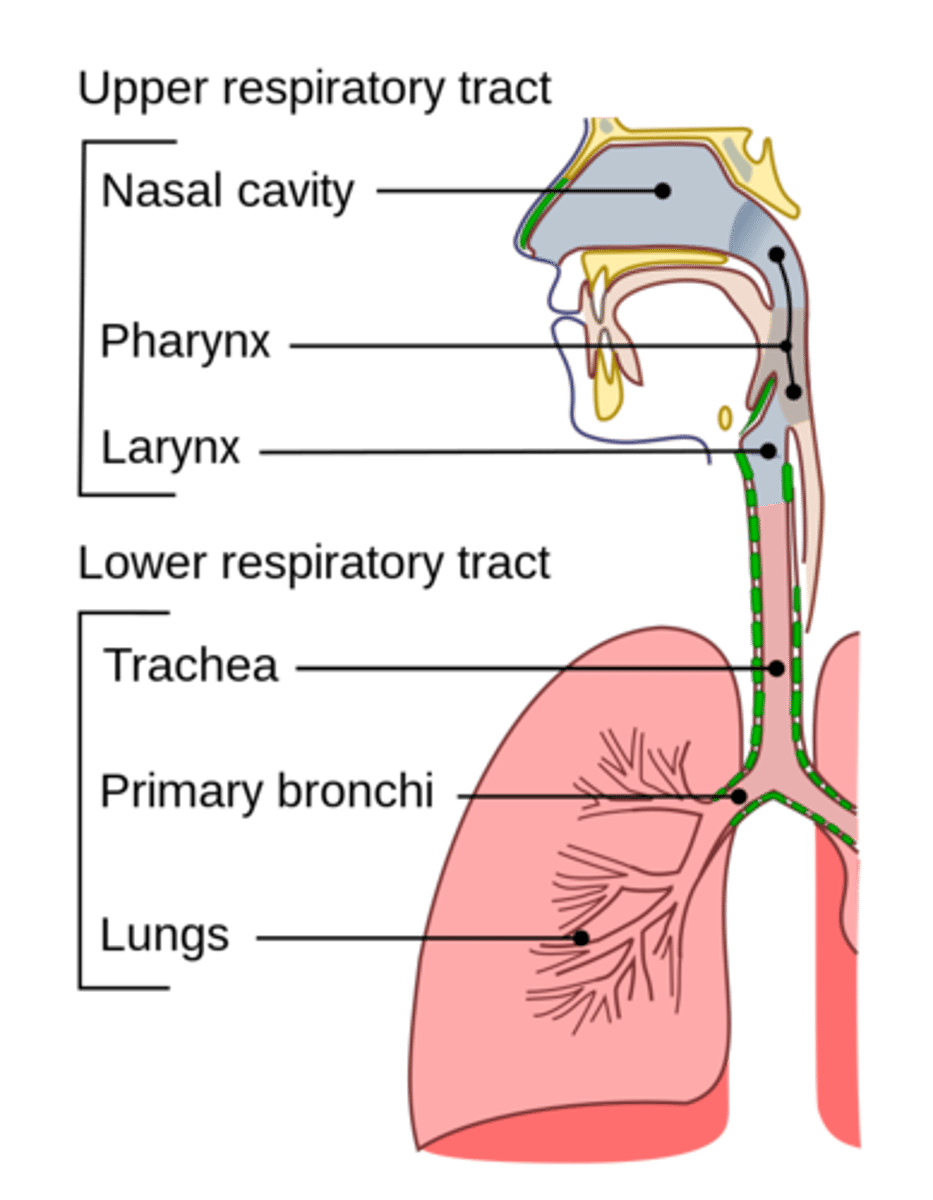
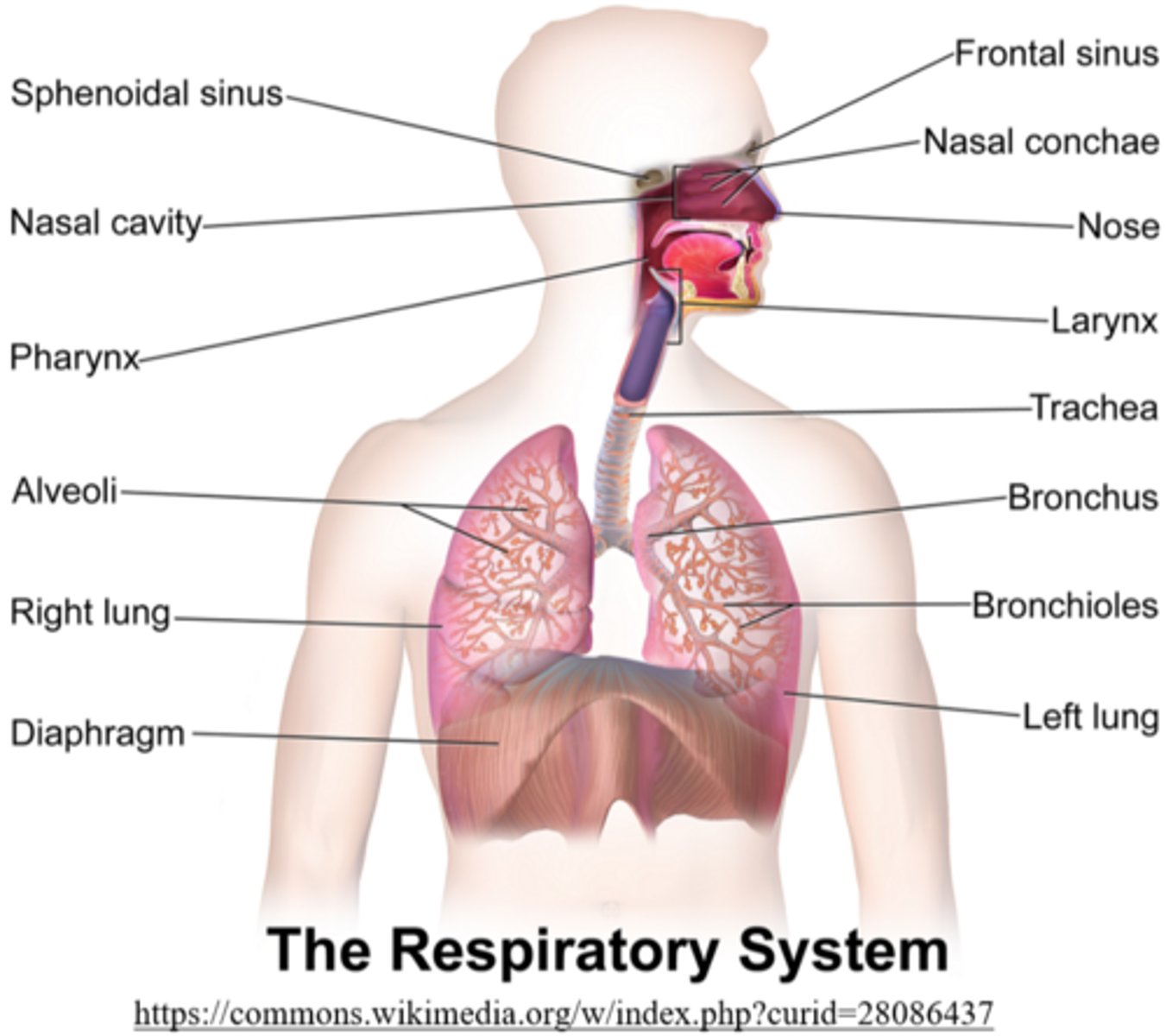
what is the first respiratory structure air makes contact with when air is inspired?
the nasal cavity
what is the function of the nasal cavity?
it warms and moistens incoming air
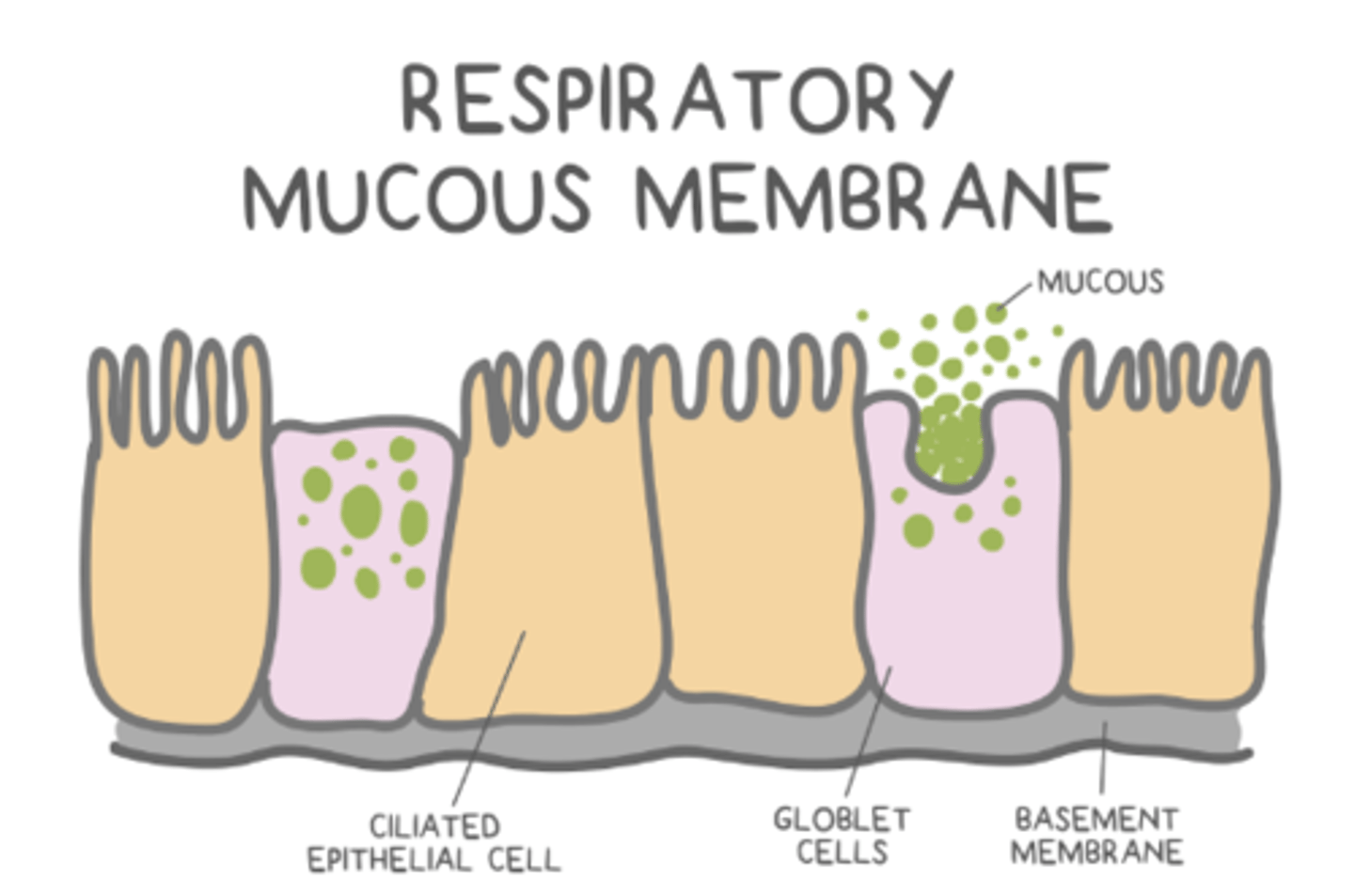
which cell types are found in the nasal cavity?
goblet and ciliated epithelial cells
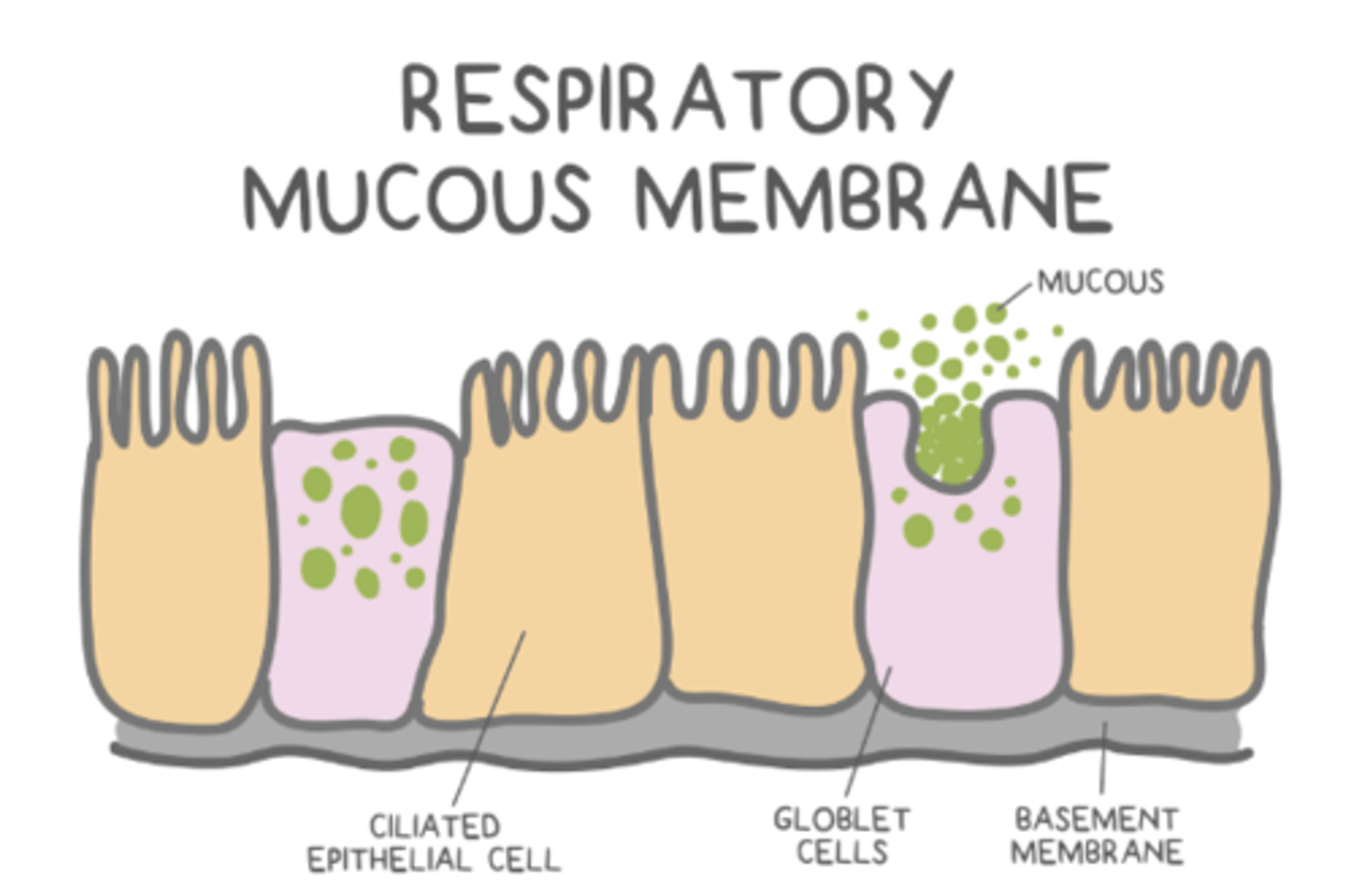
what are the columnar cells that secrete mucus to trap debris from inspired air?
goblet cells
which cells move the debris that gets trapped in goblet cell mucus?
ciliated epithelial cells
the _____ is found after the nasal cavity, and it marks the beginning of the throat
pharynx
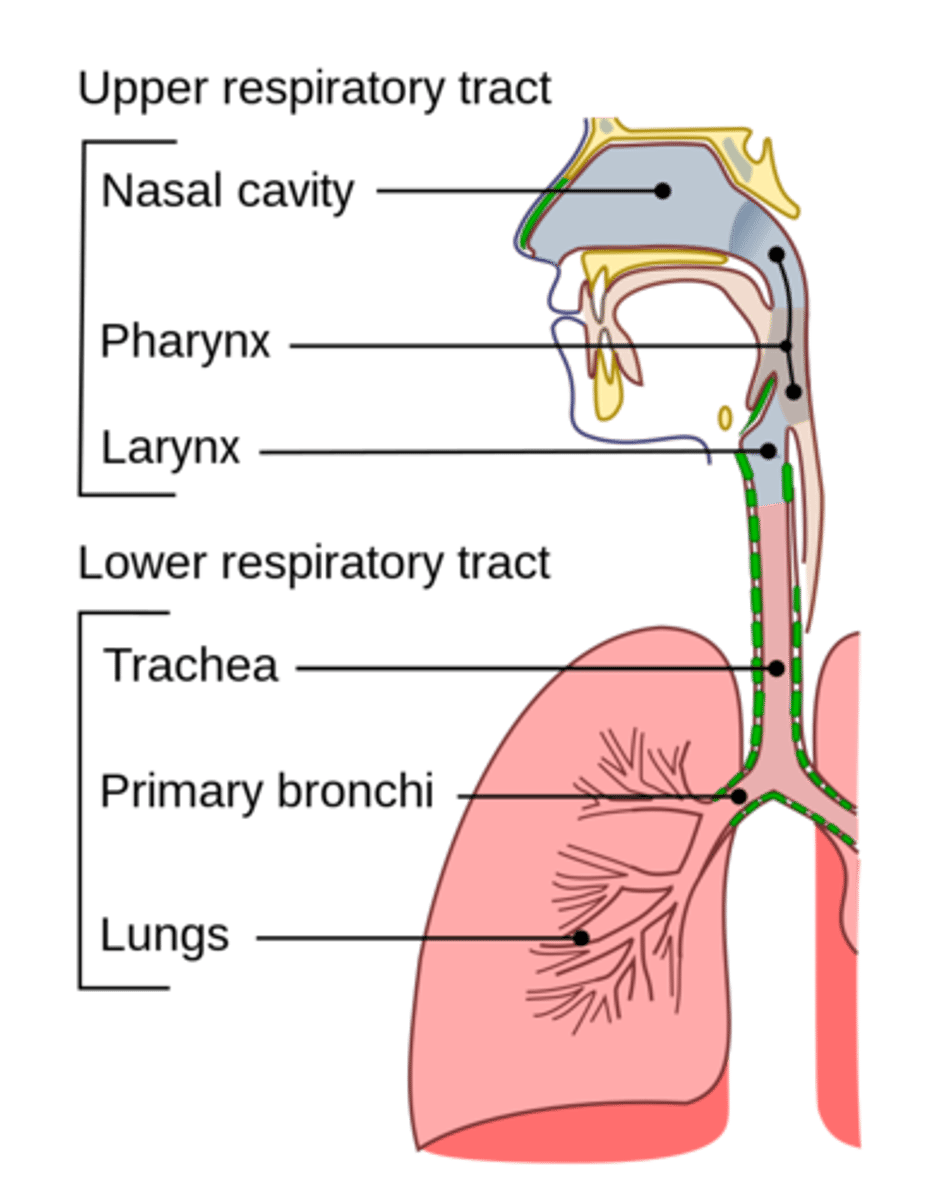
what does the pharynx divide into?
the larynx and esophagus
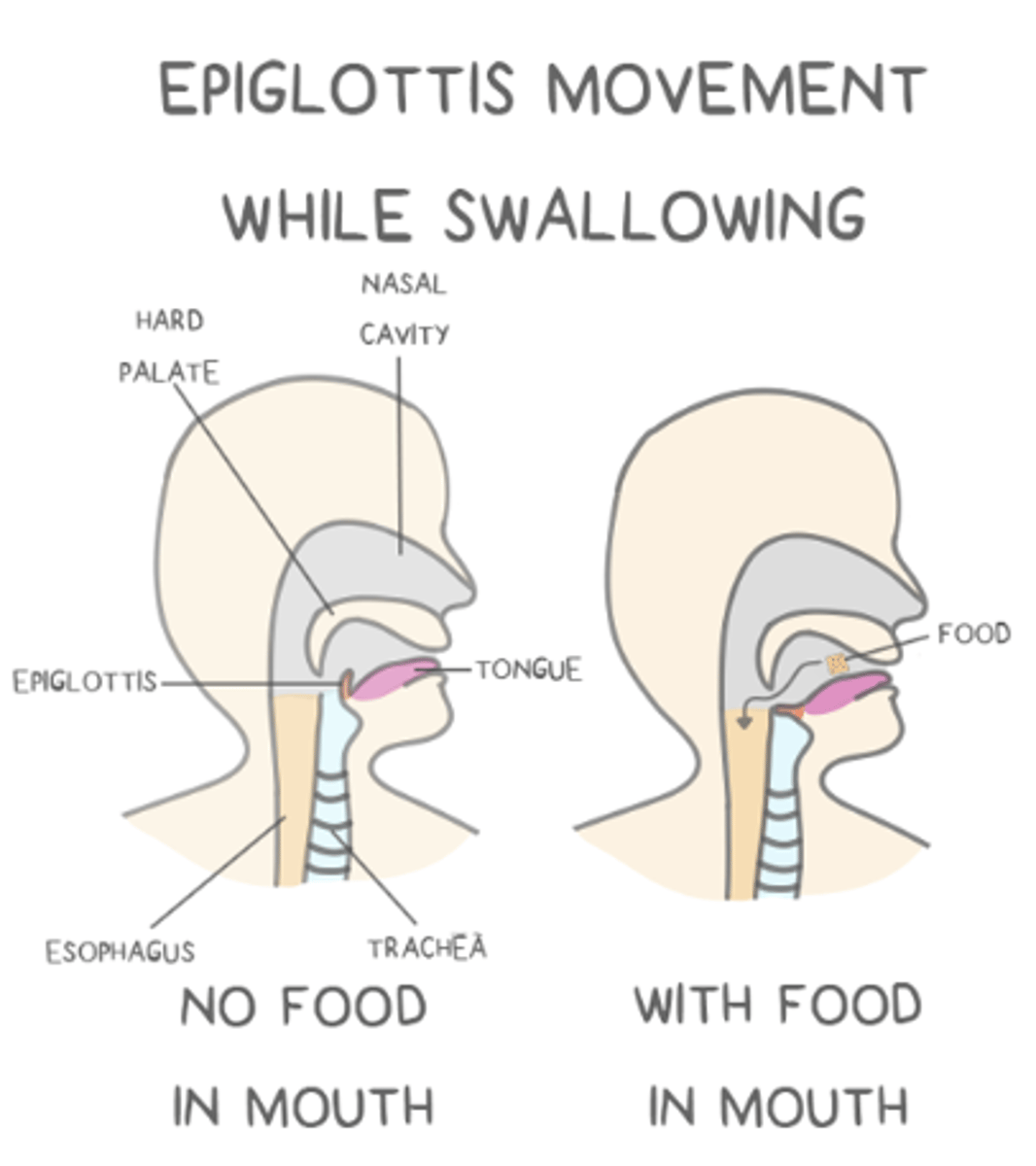
the _____ is the structure in the throat that diverts food/air into their appropriate tubes
epiglottis
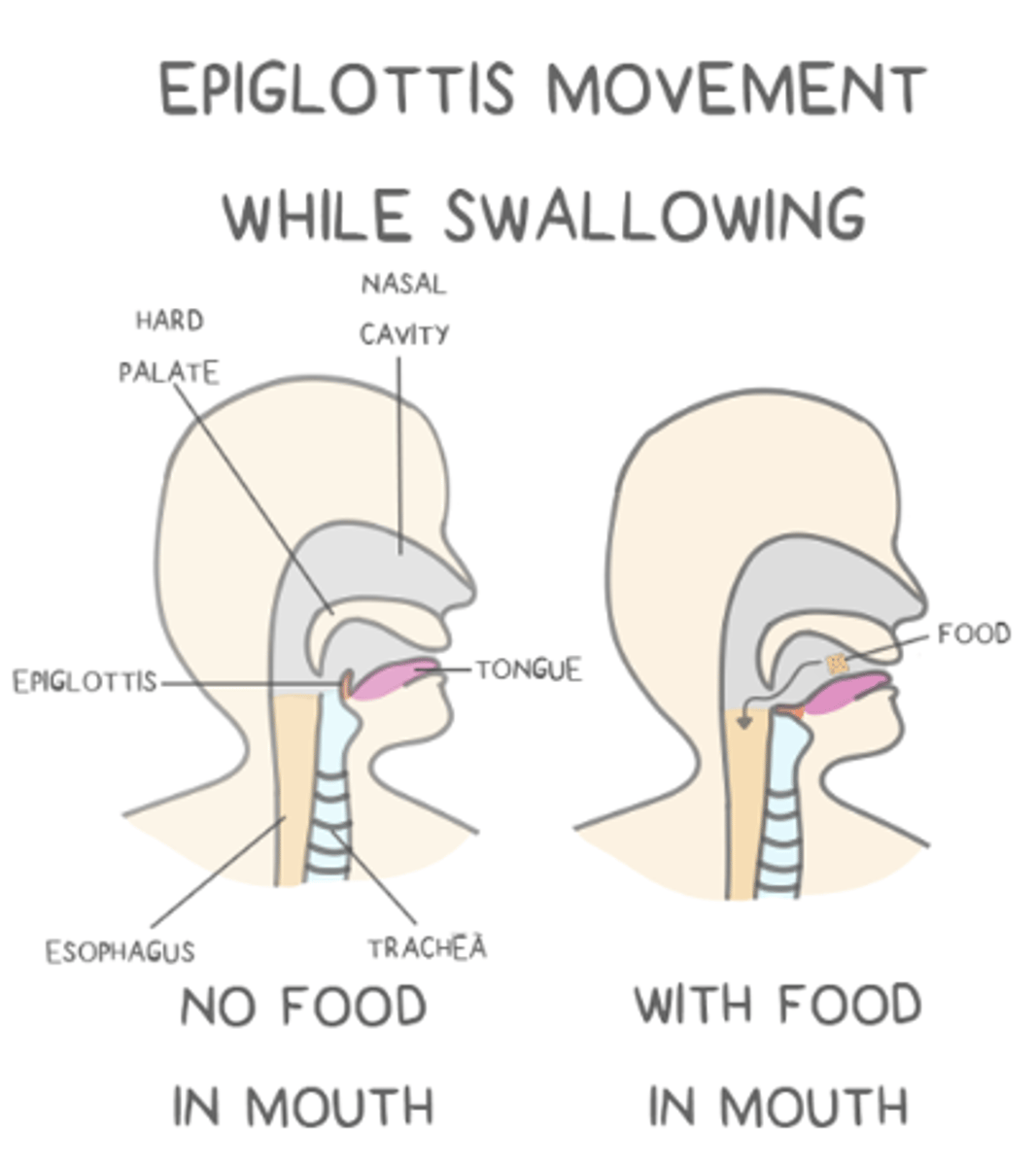
the epiglottis prevents food from entering the _____ by covering it during swallowing to divert food/fluid into the _____
larynx; esophagus
after the larynx, air flows into the upper _____
trachea
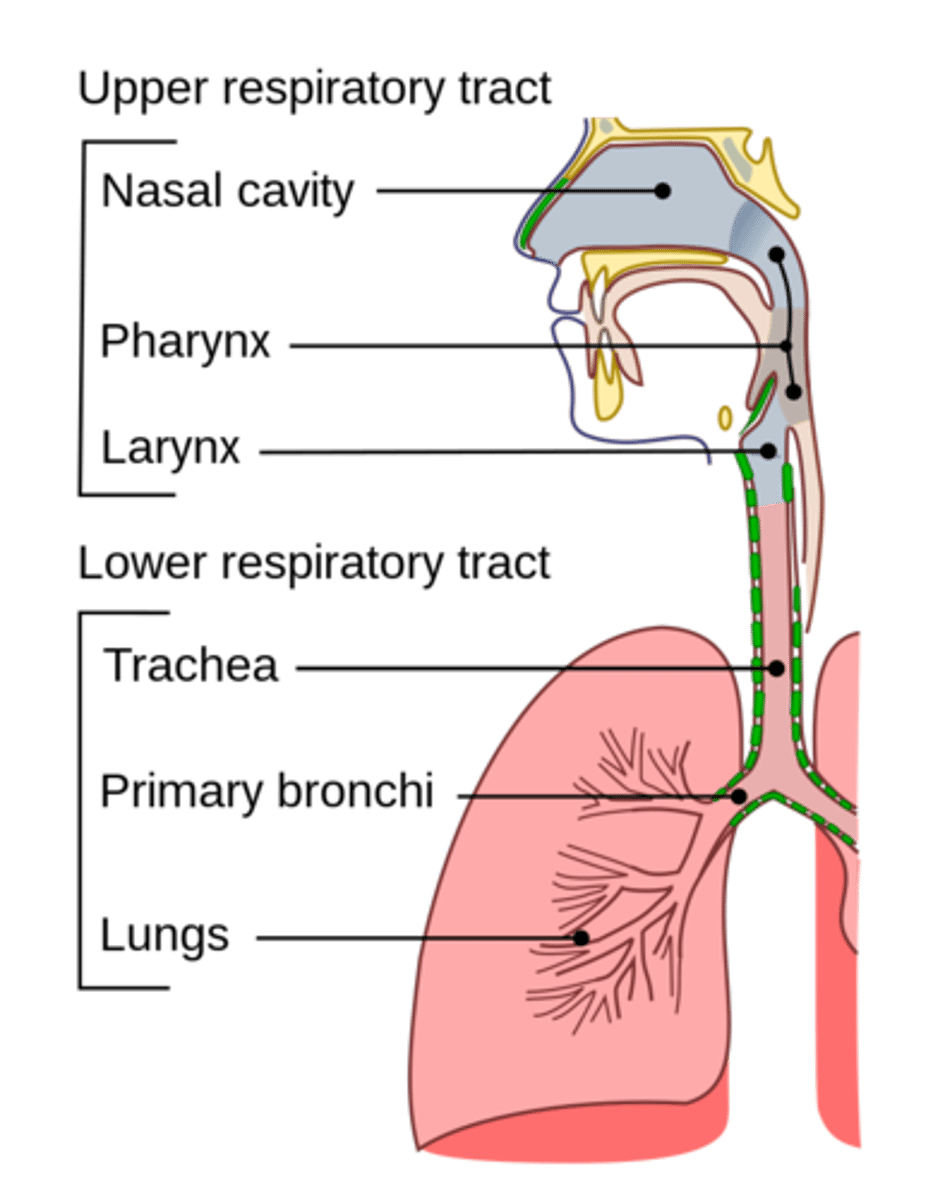
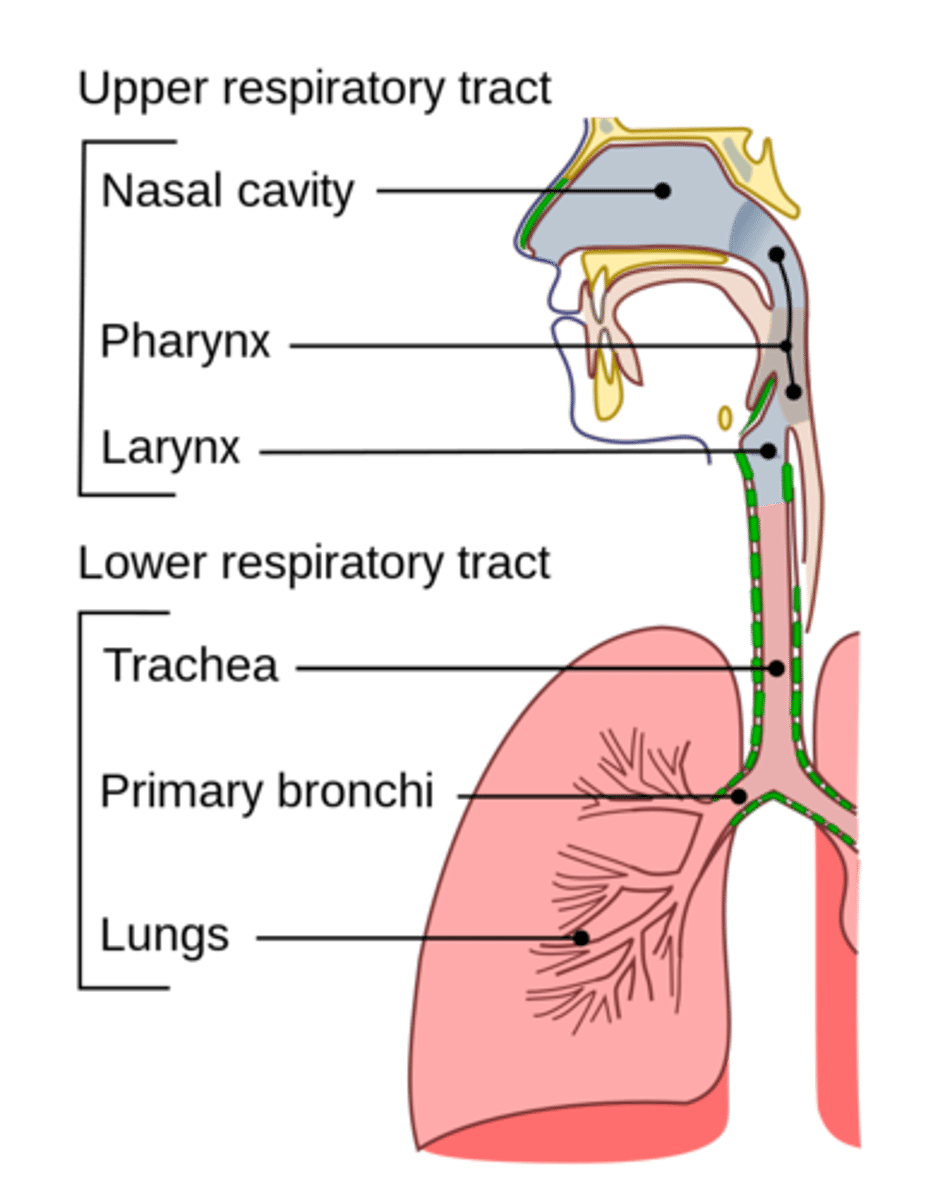
what are the components of upper respiratory tract?
nasal cavity; oral cavity; pharynx; larynx
the trachea is reinforced by C-shaped _____ to prevent collapse
cartilage
the trachea is covered in _____ cells that filter the air
ciliated epithelial
the trachea splits into the _____
bronchi
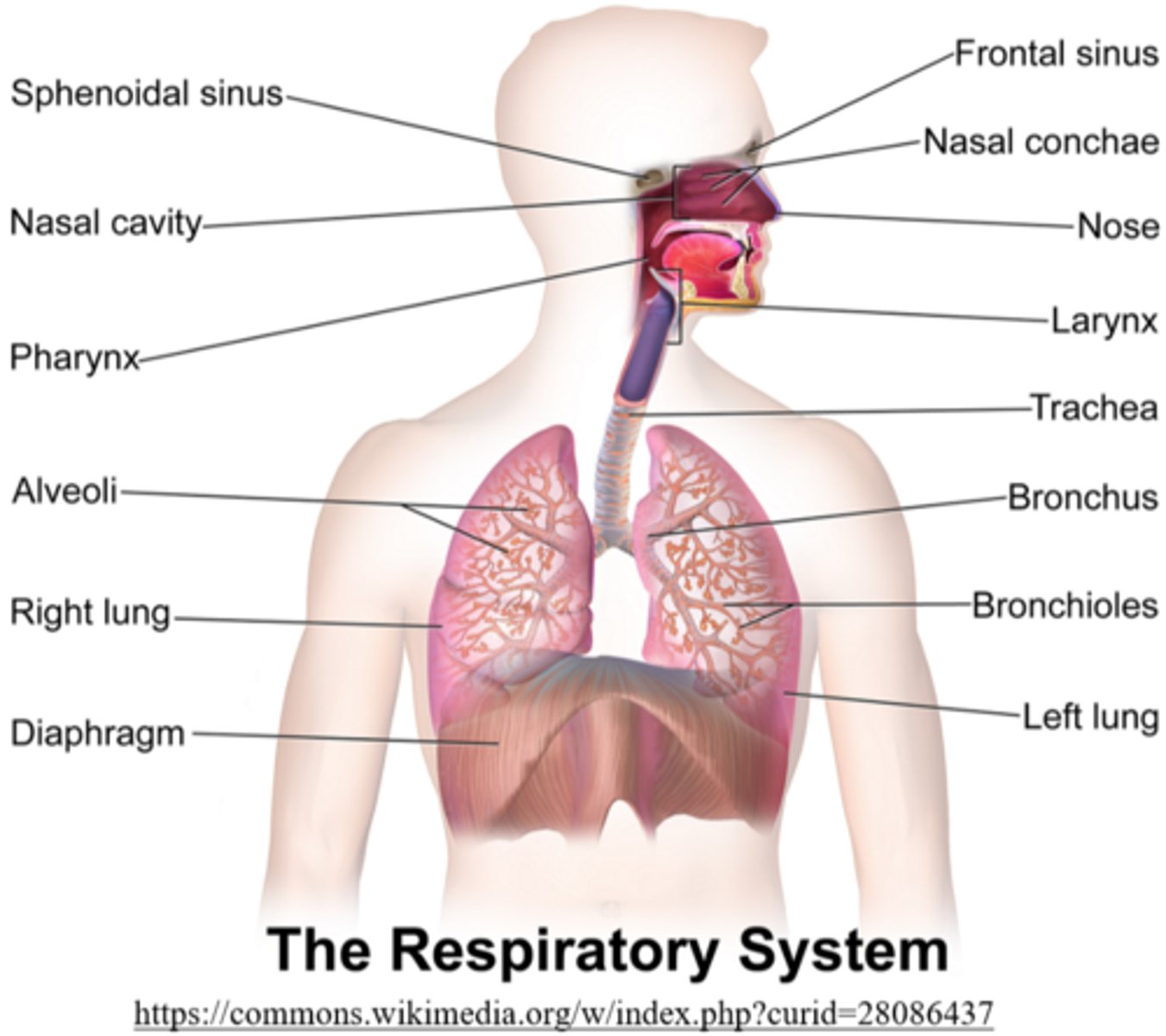
bronchi branch into _____, which further branch into _____
bronchioles; alveoli
type 1 alveolar epithelial cells are responsible for _____ of the alveoli
structural support
type 2 alveolar epithelial cells are responsible for _____ into the alveoli
surfactant secretion
what does the surfactant produced by type 2 alveolar epithelial cells do?
it prevents alveoli from collapsing
what are the components of lower respiratory tract?
trachea; bronchi; bronchioles; alveoli
what is the pathway of air in the human respiratory system?
nasal cavity/oral cavity --> pharynx --> larynx --> trachea --> bronchi --> bronchioles --> alveoli
air travels from the nose to the lung alveoli for gas exchange in _____ (internal/external) respiration
external
gas exchange occurs between the blood and body tissues in _____ (internal/external) respiration
internal
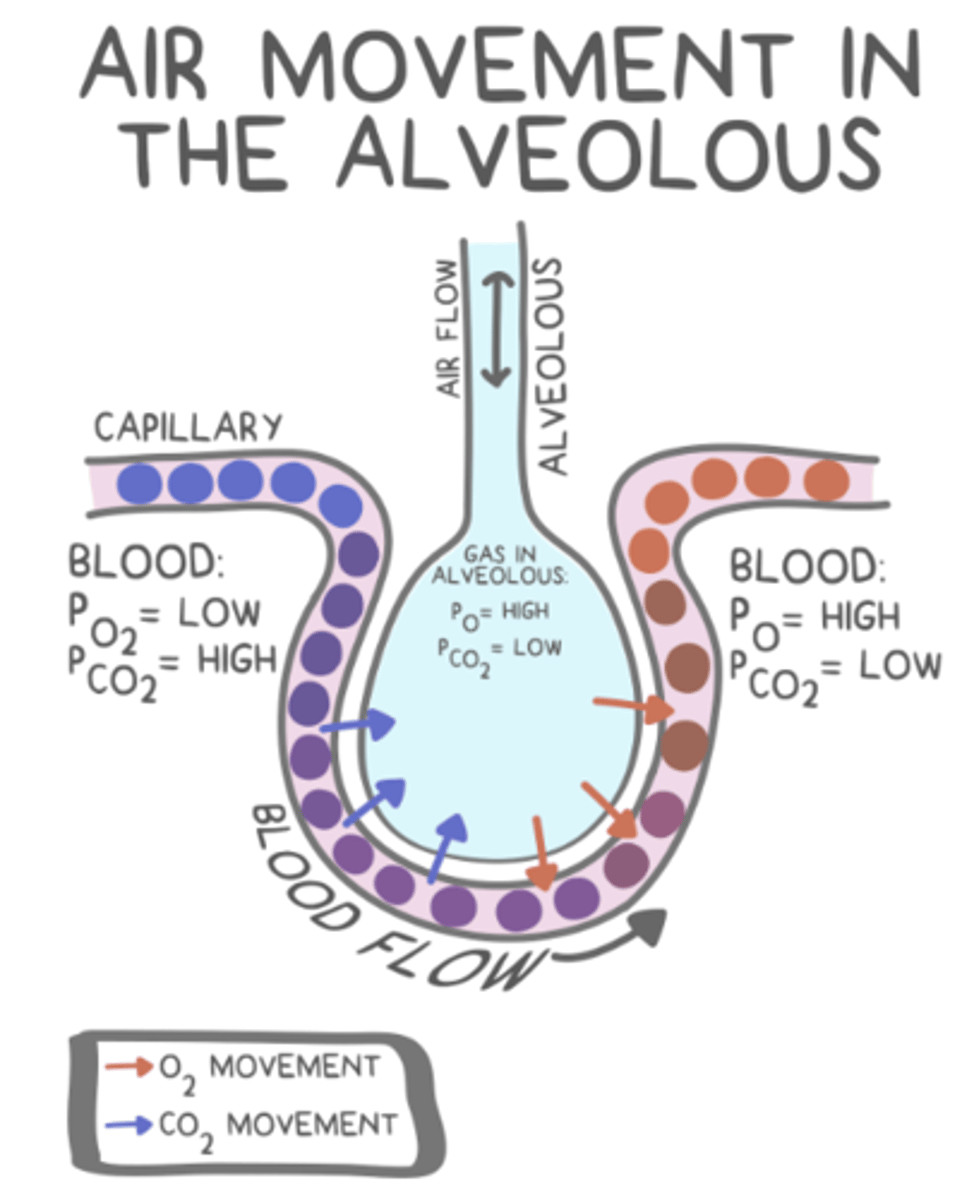
gas exchange occurs due to differences in _____
partial pressure
_____ refers to the pressure exerted by one gas in a mixture of gases
partial pressure
why does simple diffusion of gases not require energy?
molecules move passively down their concentration gradient
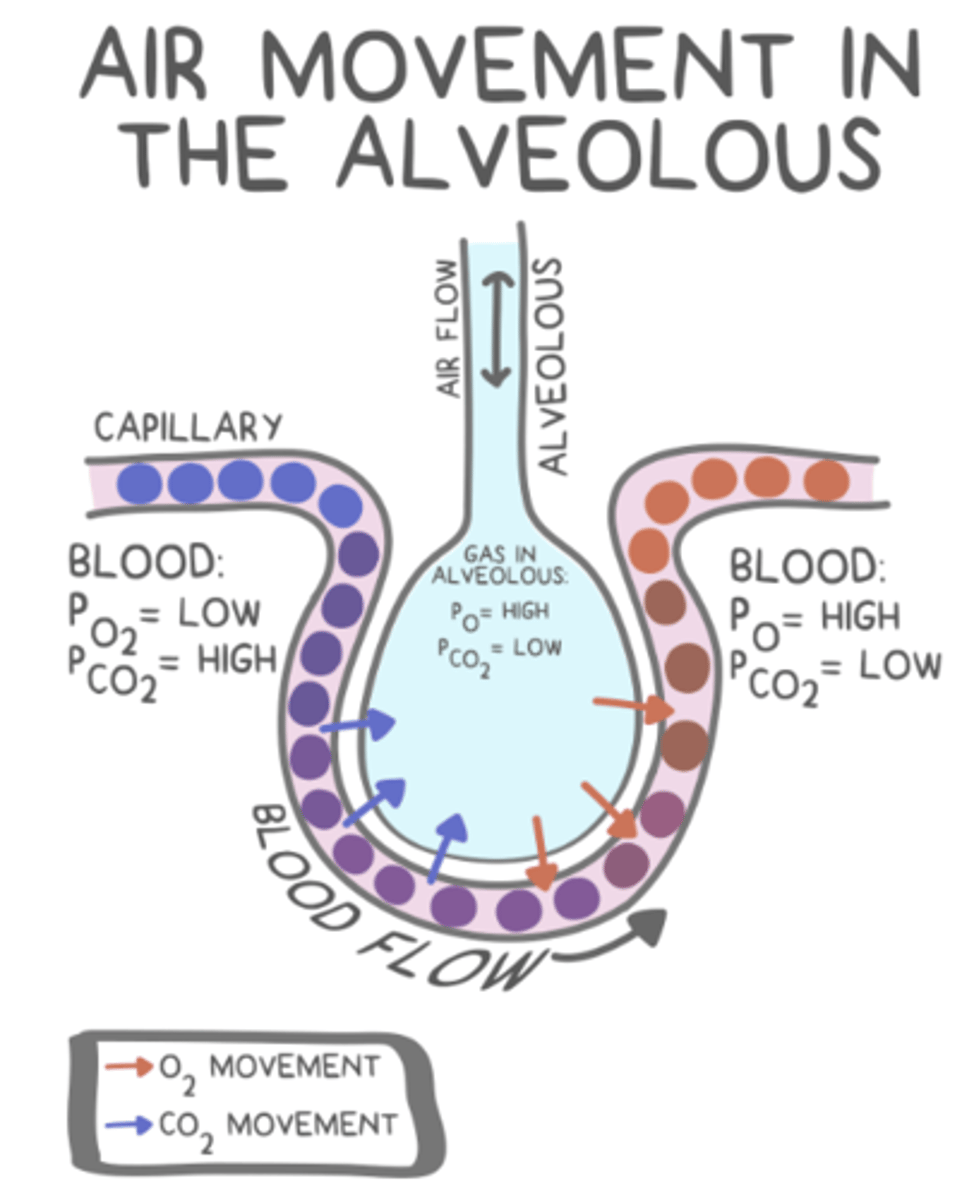
air entering the alveolus has a _____ (high/low) partial pressure of O2 and a _____ (high/low) partial pressure of CO2
high; low
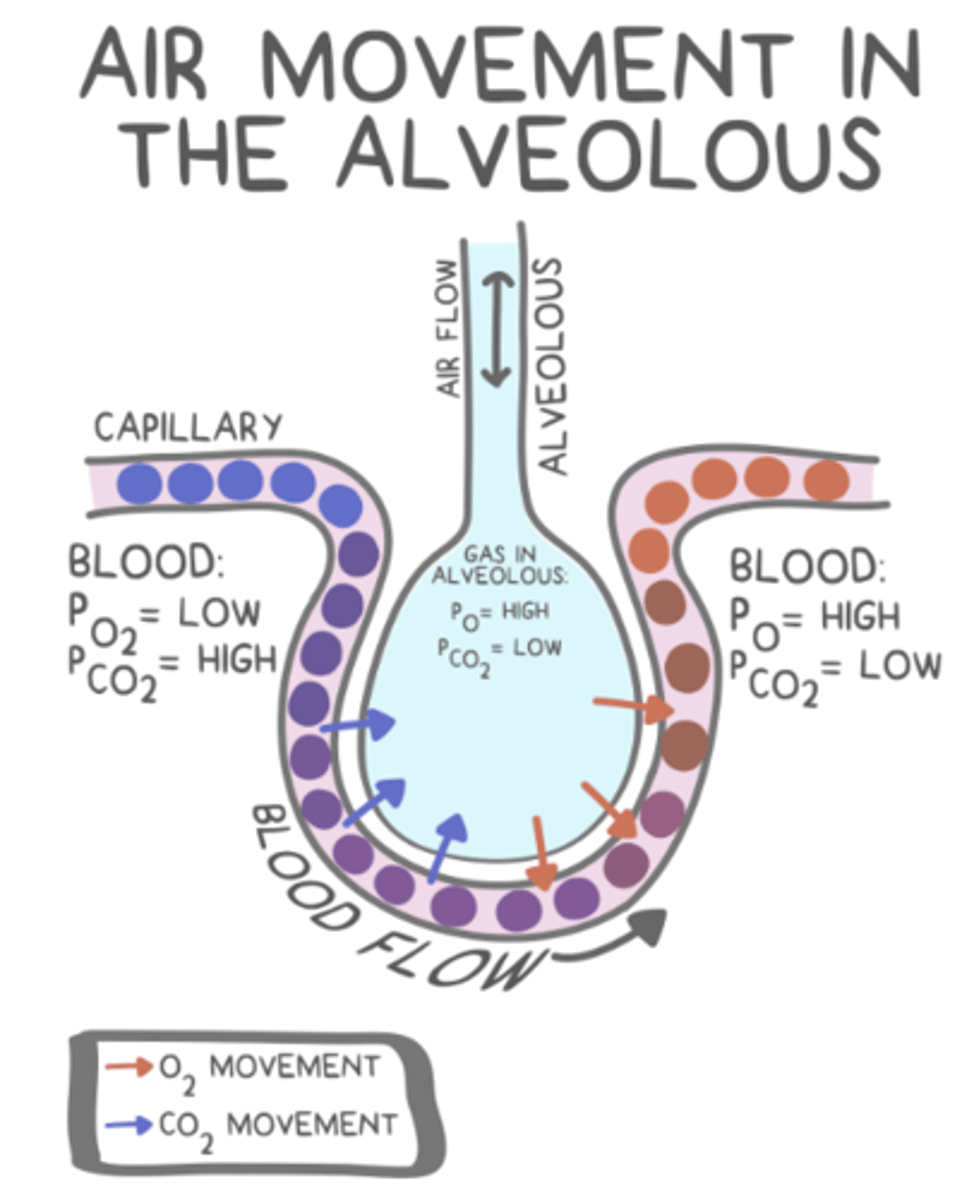
blood arriving at alveolar capillaries has a _____ (high/low) partial pressure of O2 and a _____ (high/low) partial pressure of CO2
low; high
erythrocytes (RBCs) house millions of _____, which carry oxygen
tetrameric hemoglobin polypeptides
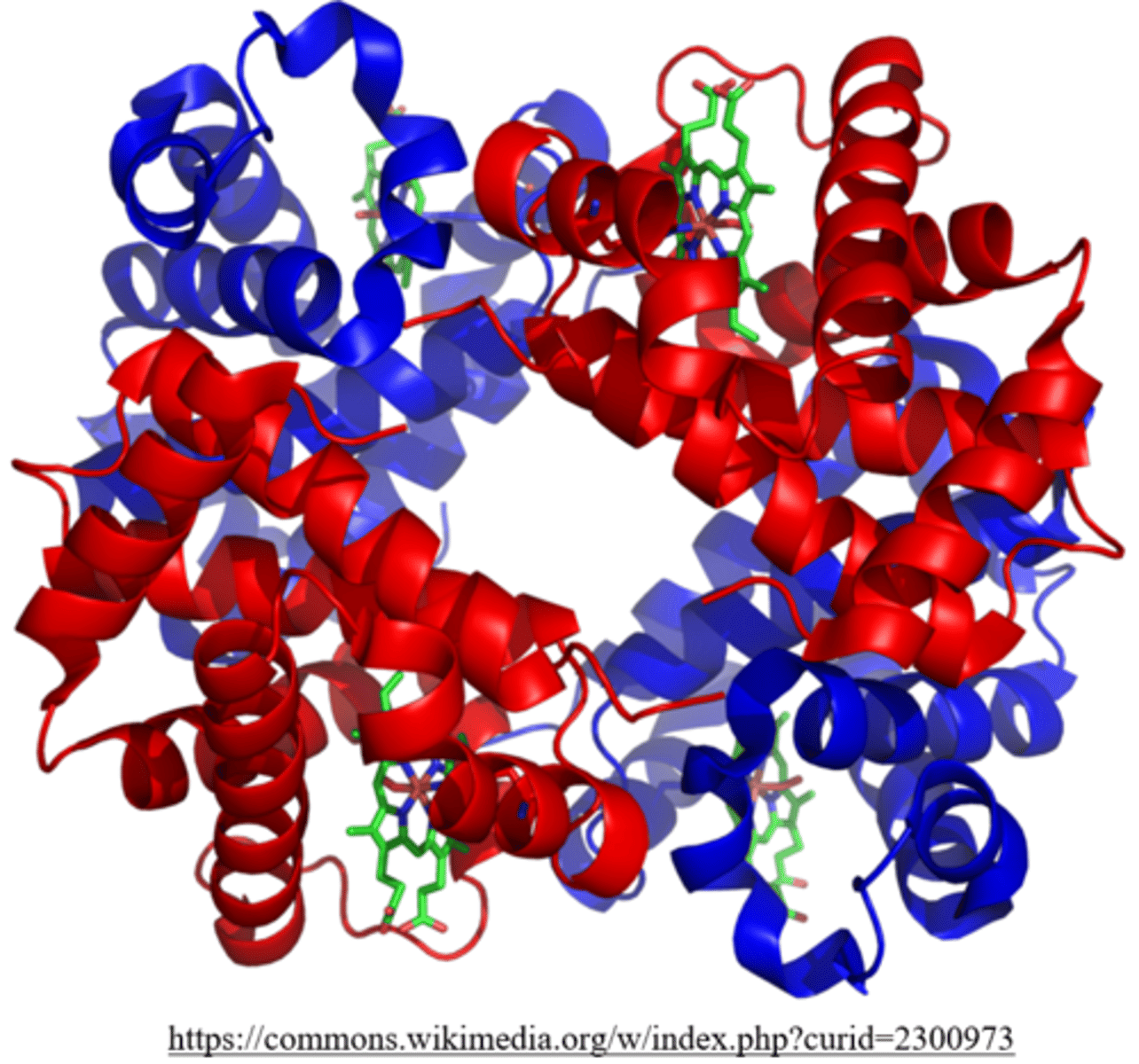
_____ are organic cofactors that assist hemoglobin binding to oxygen
heme groups
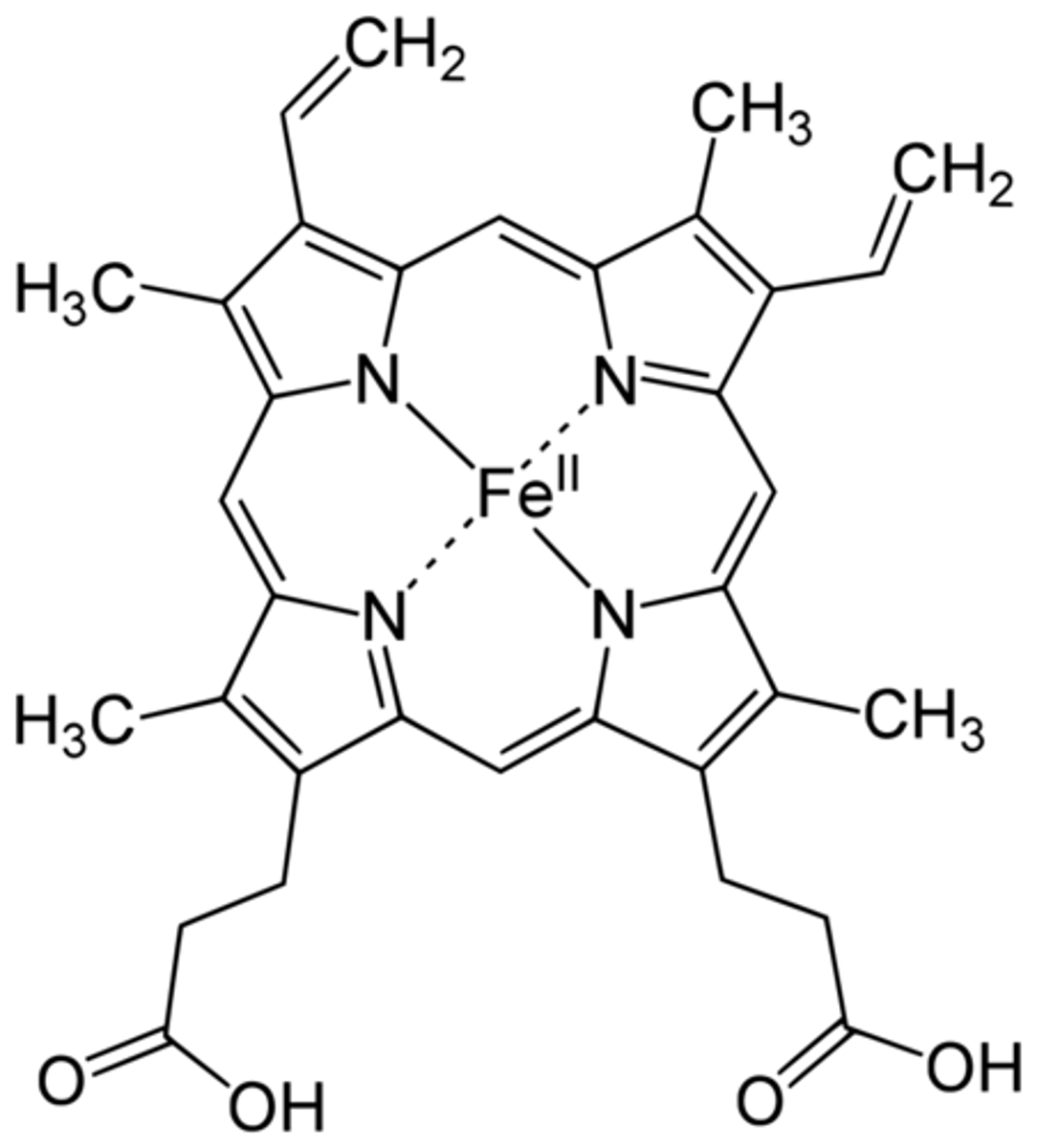
heme from broken down hemoglobin forms _____, which is a component of bile
bilirubin
approximately 98% of O2 is transported through the blood as _____
oxyhemoglobin (HbO2)
approximately 2% of O2 is transported through the blood as _____
O2 dissolved in plasma
_____ has a 200x greater affinity for hemoglobin than O2
carbon monoxide (CO)
carbon monoxide (CO) makes _____ (HbCO), which suffocates cells
carboxyhemoglobin
what is it called when hemoglobin is bound to CO2?
carbaminohemoglobin (HbCO2)
how does most carbon dioxide travel in the blood?
as bicarbonate anion (HCO3-)
what is the term that describes how binding/unbinding of one molecule makes binding/unbinding of another easier?
cooperativity
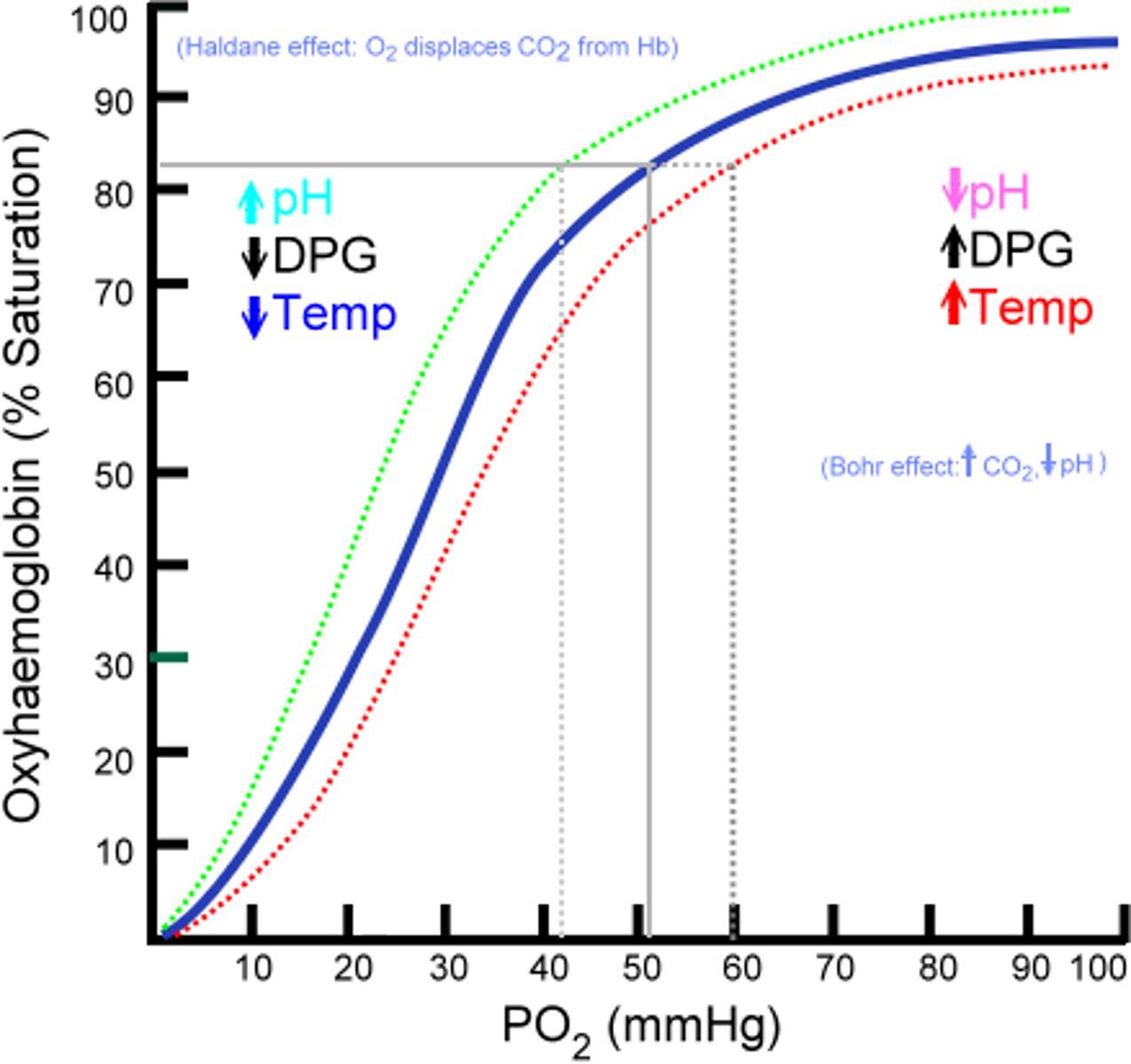
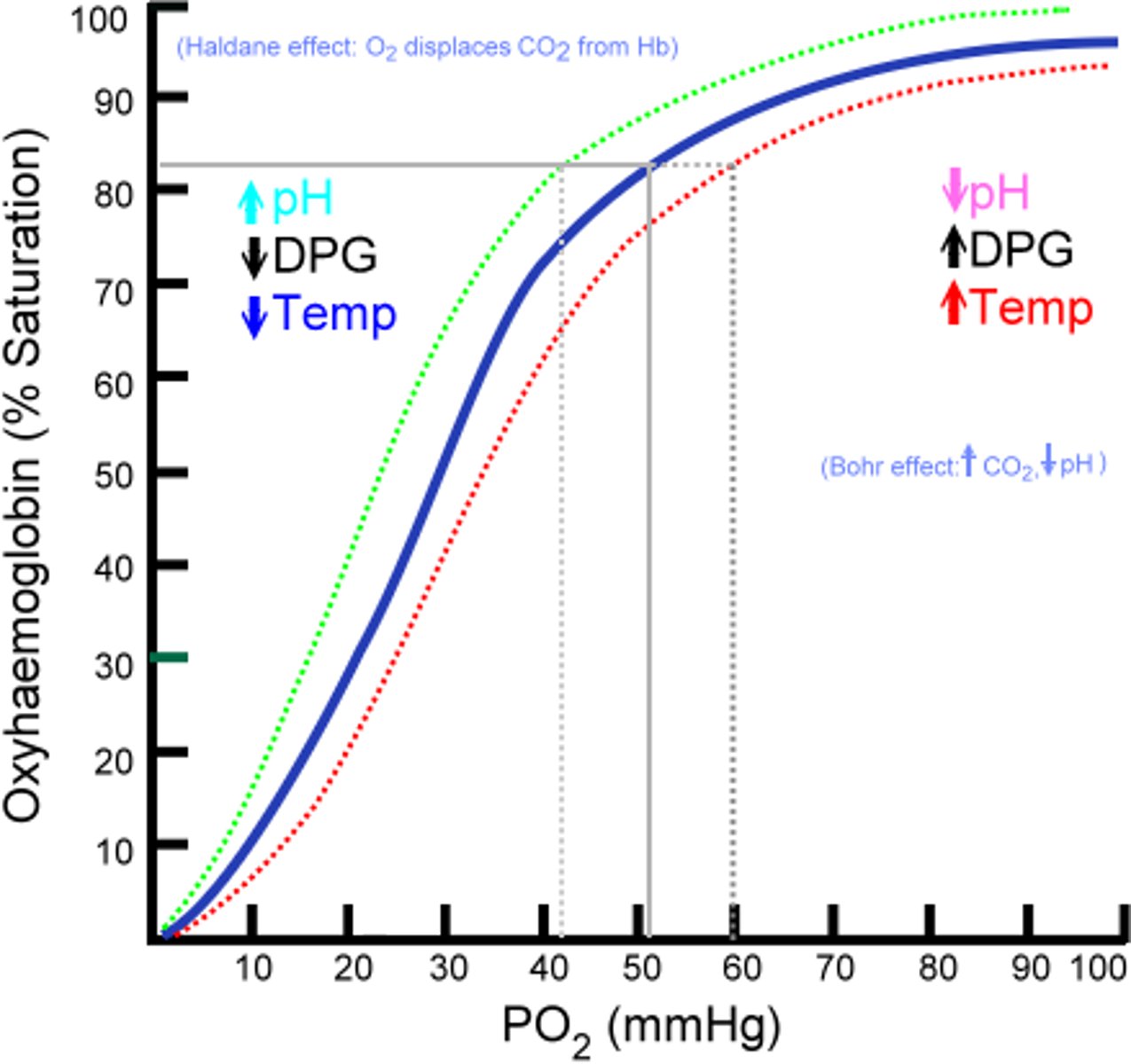
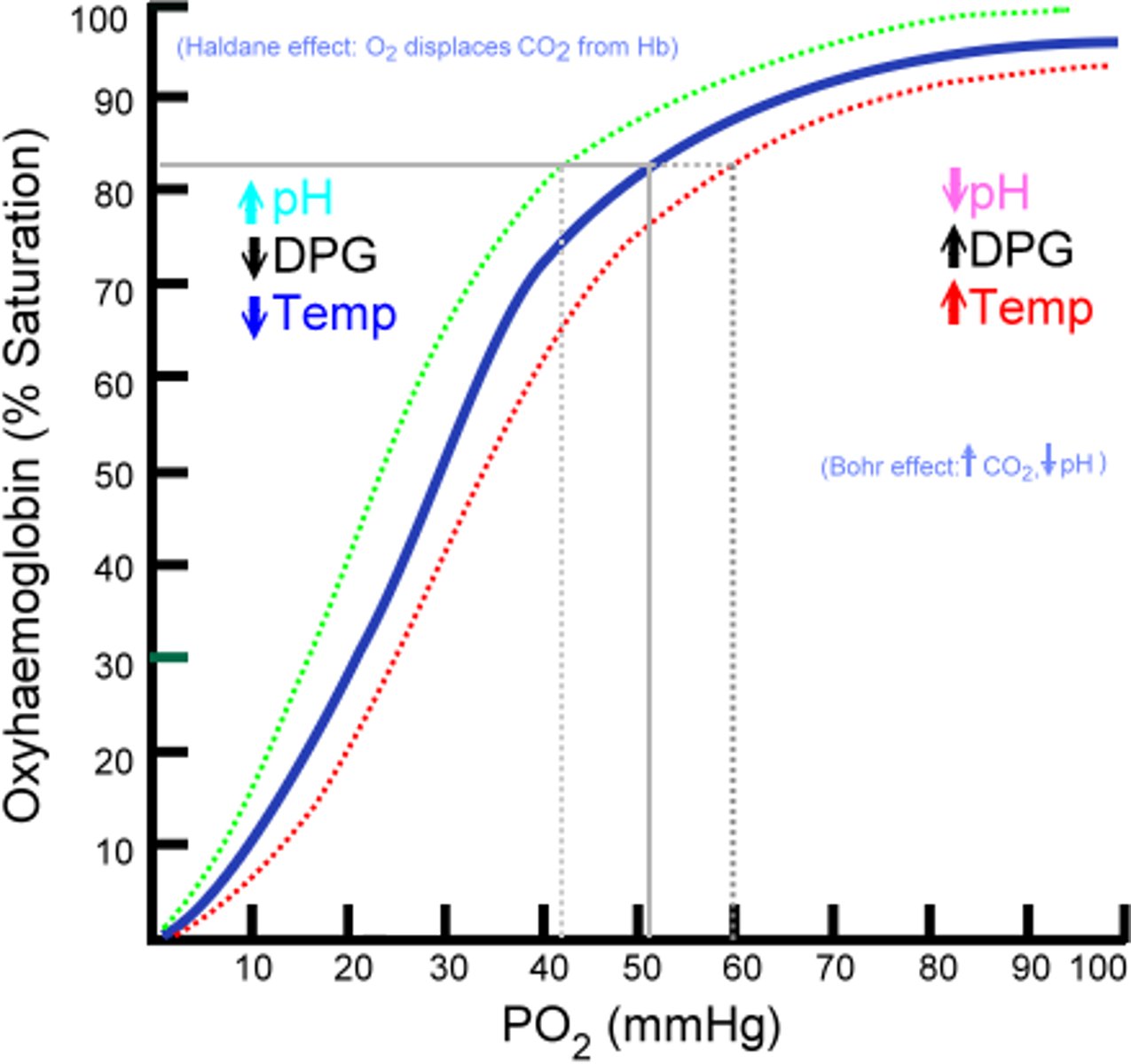
the _____ describes the percentage of hemoglobin that is saturated with O2 under various conditions
oxygen dissociation curve
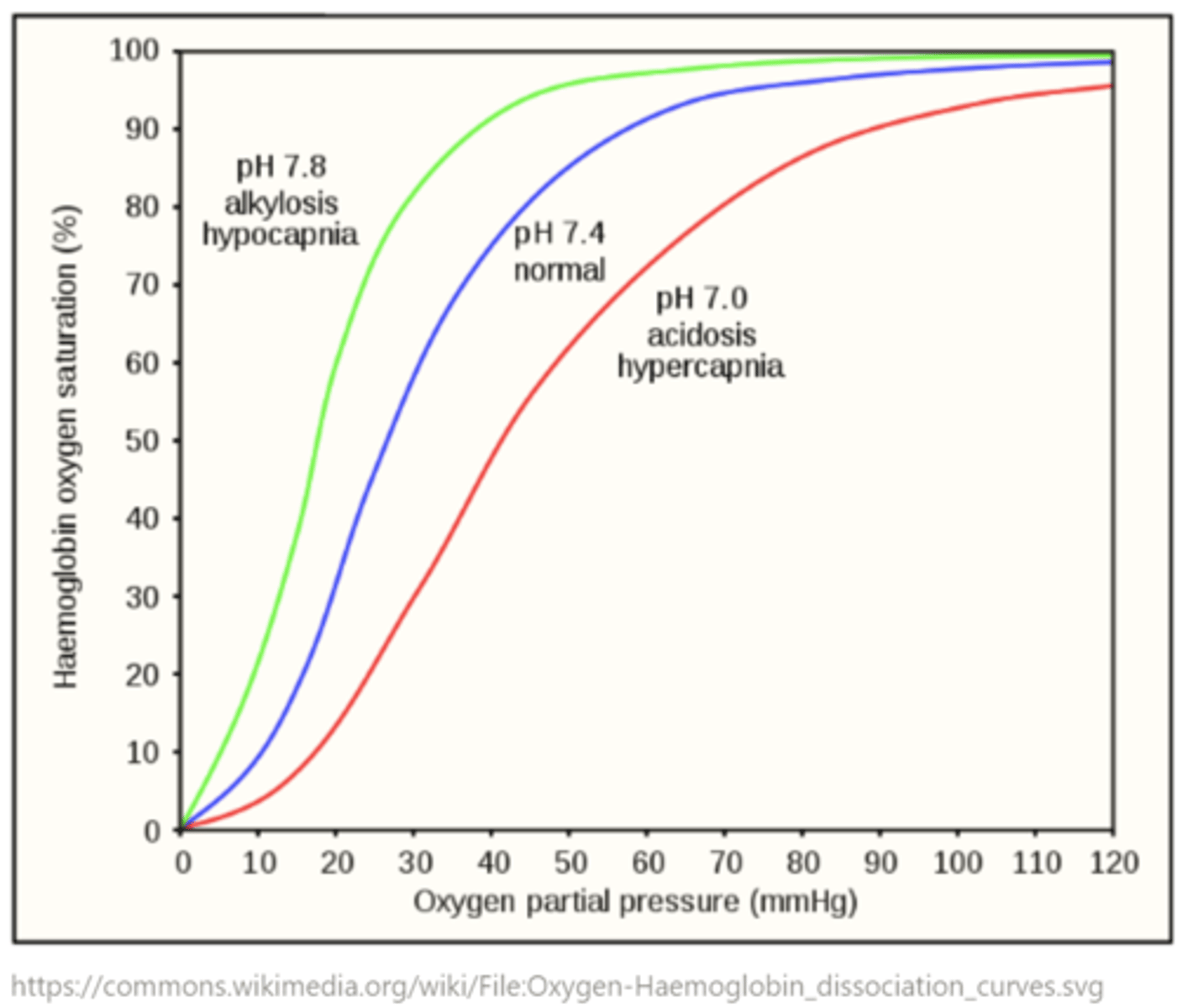
hemoglobin binds more tightly to O2 in a _____ (right/left) shifted oxygen dissociation curve, which means it is harder to release O2 to the tissues
left
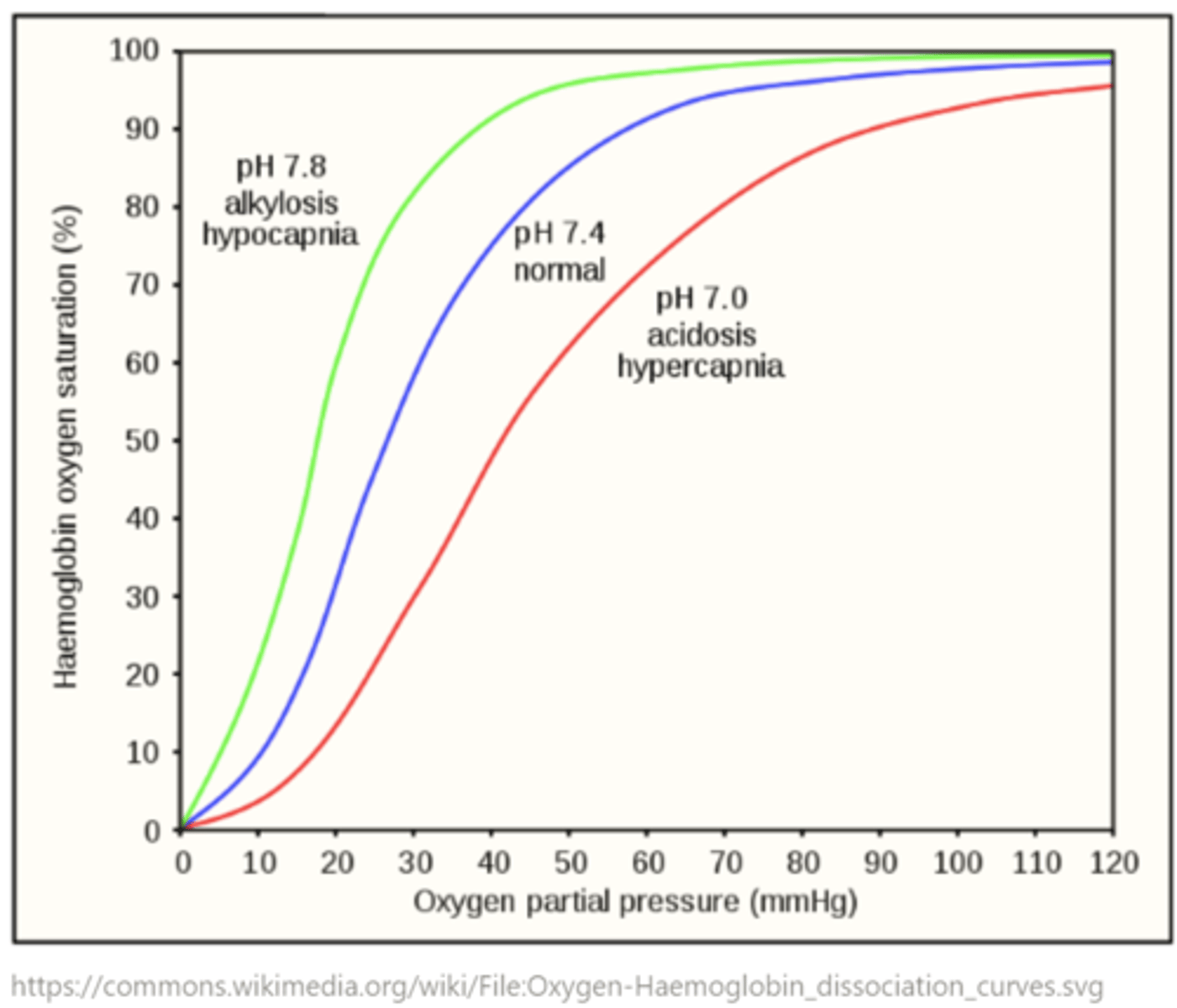
hemoglobin binds more loosely to O2 in a _____ (right/left) shifted oxygen dissociation curve, which means it is easier to release O2 to the tissues
right
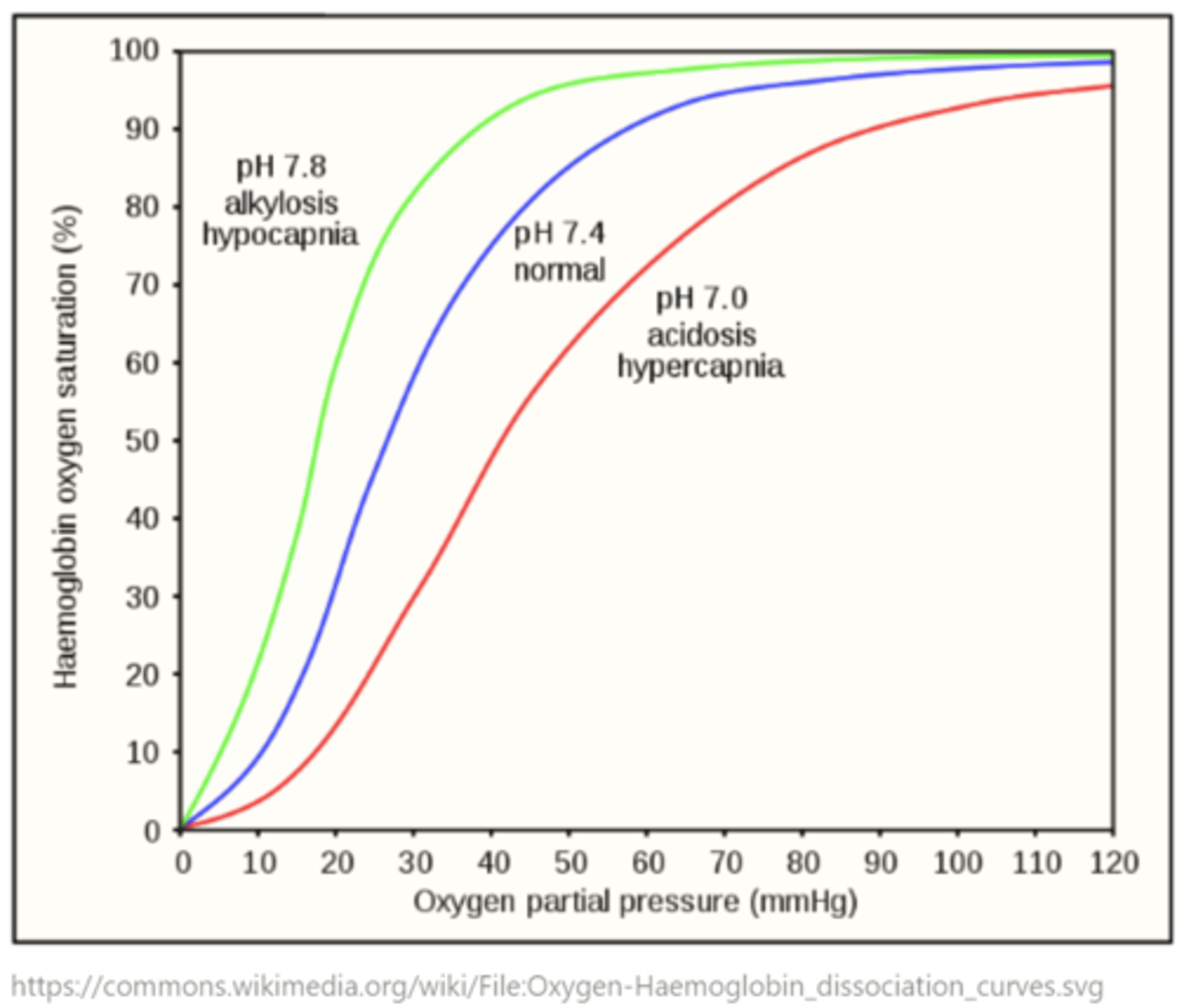
when is a right-shifted curve important?
anemia; high altitudes; vigorous exercise
what does anemia entail?
low levels heme iron (ferrous - Fe2+)
high partial pressures of carbon dioxide create _____ (right/left) shifted oxygen dissociation curves - why?
right; lower hemoglobin affinity for O2 makes it easier to release O2 to the tissues
how do high partial pressures of CO2 create a right-shifted oxygen dissociation curve?
decreases the pH (increases the H+) concentration due to the bicarbonate buffering system, which leads to reduced hemoglobin (H+Hb)
decreased pH (increased H+ concentration) creates _____ (right/left) shifted oxygen dissociation curves by reducing hemoglobin to H+Hb
right
(lower hemoglobin affinity for O2 - easier to release O2 to the tissues)
low partial pressures of carbon dioxide create _____ (right/left) shifted oxygen dissociation curves
left
(higher hemoglobin affinity for O2 - hemoglobin wants to hold onto O2 more tightly)
reduced hemoglobin (H+Hb) creates _____ (right/left) shifted oxygen dissociation curves
right
(lower hemoglobin affinity for O2 - easier to release O2 to the tissues)
decreased partial pressures of carbon dioxide lead to left shifted curves because it leads to lower concentration of _____ by the bicarbonate buffering system
H+ (lower H+ concentration --> increased pH)
increased pH (decreased H+ concentration) creates _____ (right/left) shifted oxygen dissociation curves
left
(higher hemoglobin affinity for O2 - hemoglobin wants to hold onto O2 more tightly)
why does an increased pH (decreased H+ concentration) left-shift the oxygen dissociation curve?
not as many H+ are available to displace oxygen from hemoglobin - aka to reduce hemoglobin to H+Hb
increased temperature will result in a _____ (right/left) shifted oxygen dissociation curve
right
(higher temperature increases the metabolic rate - aka increases the cellular requirement for oxygen)
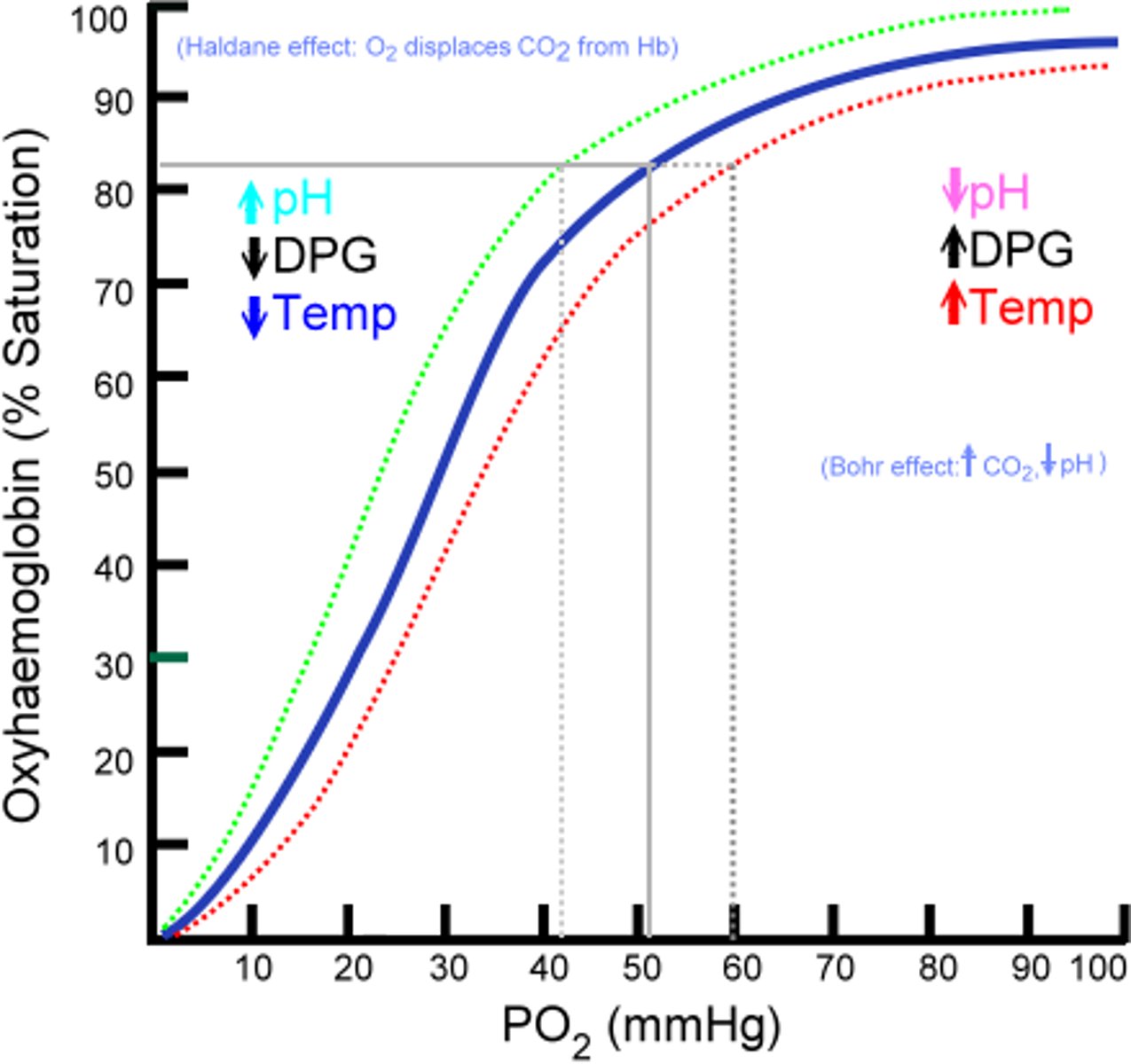
increased temperature --> increased metabolic rate --> increased _____ (metabolic byproduct), which leads to a _____ (right/left) shifted oxygen dissociation curve
2,3-BPG; right