Wounds and Other Openings
1/73
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
74 Terms
Acute wound
normal stages of healing within 4 weeks
-results from the sudden loss of anatomic structure in tissue following the transfer of energy, thermal/kinetic/chemical
-typically occur in previously uninjured tissue
Chronic wound
no visible healing at 4 weeks, healing takes >3 months
-dysregulation of one of the phases (commonly inflammatory phase due to infection or tissue irritation)
Class I
clean wound, no signs of infection or inflammation
Class II
clean-contaminated wound, increased risk for infection due to location (GI wounds)
Class III
an outside object has come into contact with skin, high risk of infection
Class IV
considered dirty-contaminated, wounds that have been exposed to fecal material (peri-rectal)
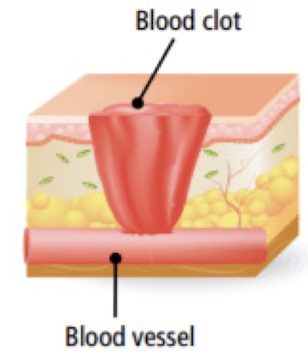
Hemostasis
Which first phase of wound healing occurs within minutes post-injury when platelets aggregate at injury site to form fibrin?
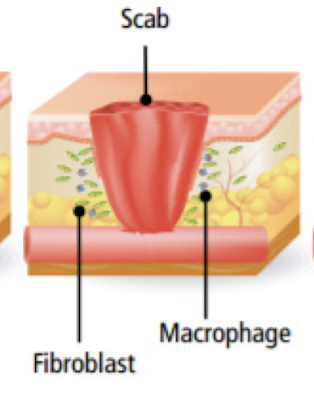
Inflammation
Which second phase of wound healing are bacteria and debris phagocytized and removed and factors released that cause the migration and division of cells of proliferative phase?
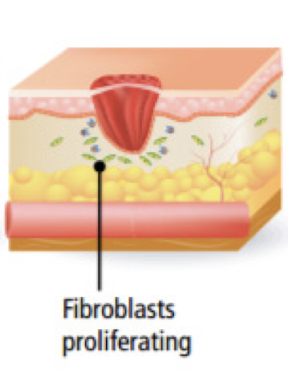
Proliferation
What third phase of wound healing does angiogenesis, collagen deposition, granulation tissue formation, epithelialization, and wound contraction occur?
Remodeling
What fourth phase of wound healing is collagen remodeled and realigned along tension lines and old cells removed by apoptosis?
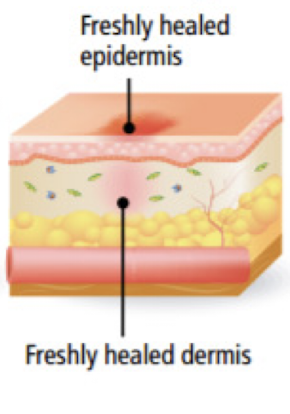
Primary intention
What form of healing occurs when tissue is cleanly incised and anatomically re-approximated, healing usually proceeds without disruption or complication?
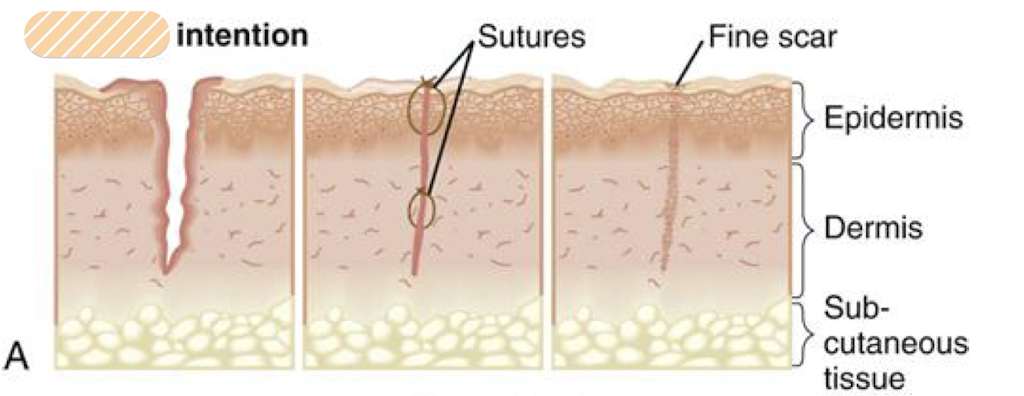
Secondary intention
What form of healing occurs when wound is left open and eventually heals through granulation tissue and migration of epithelial cells?
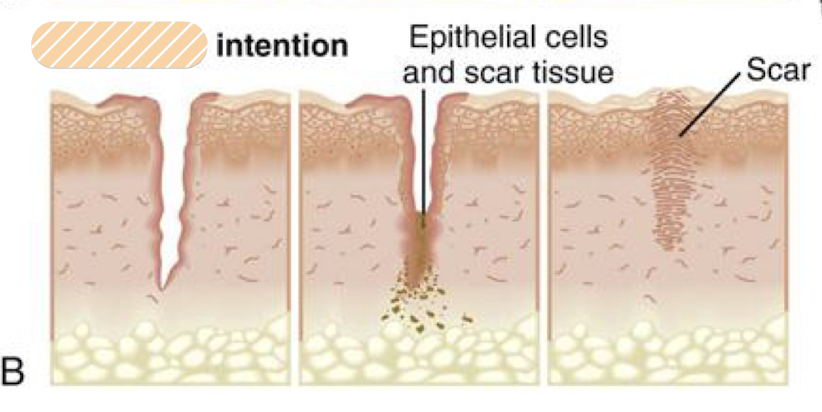
Tertiary intention (delayed primary)
What form of healing occurs when a contaminated wound is left open for a period of time before being surgically closed?
ie. dog bites, infection
epithelialization
What type of wound healing only happens horizontally?
-grows circumferentially inward (migration)
granulation
What type of wound healing happens bottom-to-top and needs to occur before epithelialization (horizontal migration)?
slow wound healing
Smoking and Diabetes (hyperglycemia) are two comorbidities that dramatically _______
Other factors
-blood supply to wound
-tissue quality
-nutritional status
-vascular insufficiency
-obesity
-immunocompromise/chemotherapy/radiation therapy/steroid use
-compliance with post-op instructions
Immature scar
scar <6 months that is erythematous, raised, ± pain/pruritis
-usually evolve into mature scars by 1 year
-avoid sun exposure to improve healing outcomes

Mature scar
scar 6month-1 year that is narrow, flat, pale/hypo-pigmented

<24 hours
Generally sterile dressing left in place <48 hours
-use aseptic technique if changing dressing _____
Hypertrophic scar
erythematous, thickened and raised within boundaries of original surgical incision that develops within a few weeks post surgery
S/S: scar is firmer than healthy skin with broad and irregular surface after maturation, pain/pruritis common during healing

Keloid
erythematous, bulging and firm, focally raised scar
-can develop months-years after trauma w/o spontaneous regression
-genetic predisposition; increased incidence in African/Asian descent
-located primarily on chest and shoulders, also ear lobes

Pressure ulcer (Decubitus ulcer)
wound caused by pressure, friction/shear
-often hospital-acquired
-Stage I (nonblanchable) occurs <2-6 hours
Prevention:
-turning/positioning, special air mattress, PT/OT
-manage nutrition
-dressing
-wound vacs
-debridement
-skin grafts/flaps
Burns
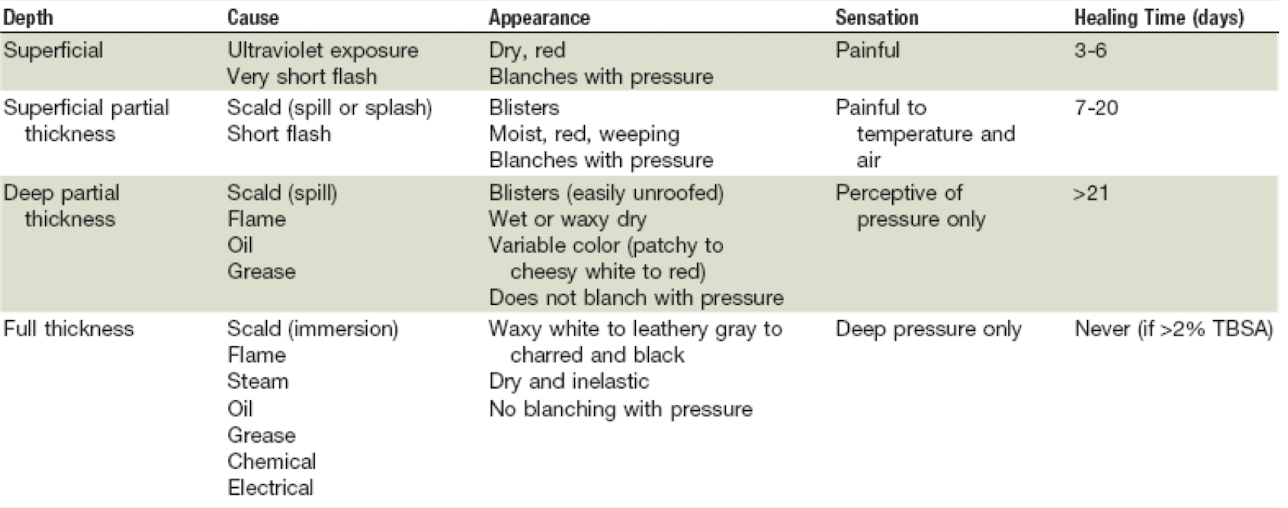
Rule of Nines
-Head and neck 9%
-Each arm (front/back) 9%
-Anterior trunk 18%
-Each leg (front/back) 18%
-Posterior trunk 18%
-Genitals 1%
*indicated for adult patients with BMI<30
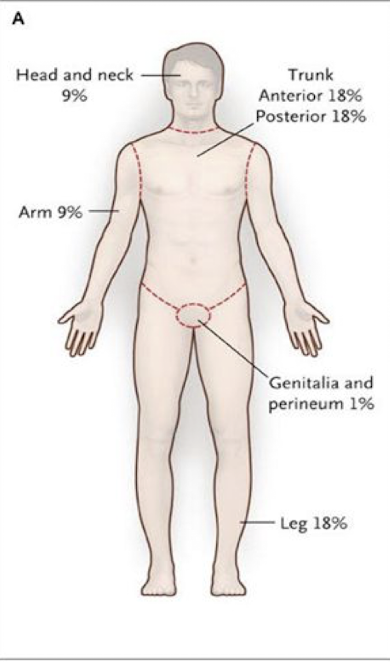
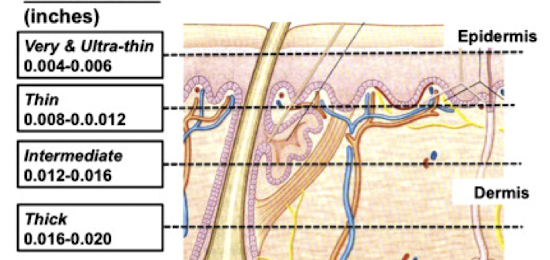
Split thickness skin graft (STSG)
graft that contains the epidermis and a portion of the dermis
-subdivided into very thin, thin, medium/intermediate, thick
-Does NOT maintain original blood supply, rely on recipient region
-donor site is often slowest to heal and most common source of postoperative discomfort
-can be meshed to increase overall size of graft
-multiple sources (autograft, allograft, xenograft, forearm is common
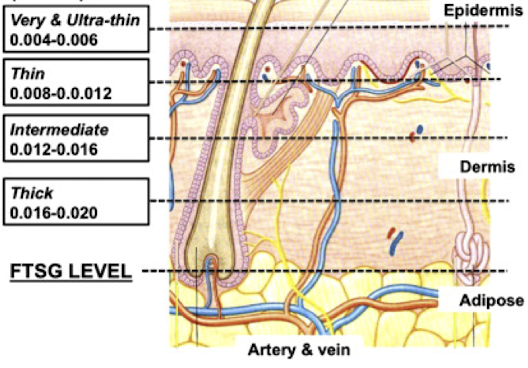
Full thickness skin graft (FTSG)
graft that contains the complete epidermis and dermis, sometimes muscle and fascia
-donor site should be chosen from area with optimal tissue match and least significant scarring: donor site is often slowest to heal and most common source of postoperative discomfort
-Does NOT maintain original blood supply, rely on recipient region
skin graft complications
• continuous pain, numbness, fever, discoloration, redness, swelling, or a breakdown of tissues
• Hematoma or seroma
• Infections
• Rejections
• Durability: thick STSGs or FTSG preferred to cover mechanically demanding areas of the body, including the palms, soles, and joints
• Primary contracture: immediate reduction in the size of skin graft after it has been harvested/passive recoil of elastin fibers in the dermis.
• Secondary contracture: shrinkage of the skin graft in the wound bed over time.
• Misplacing the graft dermis side up (iatrogenic error)
• Poor cosmetic appearance (mismatched texture, color, or topography which may require additional surgical correction)
• Graft Take: thicker graft has greater metabolic activity and lower nutrient diffusion
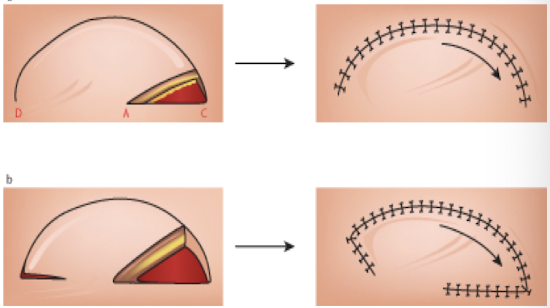
Flaps
Local: has blood supply from at least one artery & vein that relies on perforators for vascularization, can use adjacent tissue rotated in an arc to close defect
Pedicled: has blood supply from at least one artery & vein that relies on perforators for vascularization, rotated
Free: a blood vessel is cut and reconnected via anastomosis
-monitor w/ Doppler US for vascular supply pre and post operation
-AVOID smoking and hyperglycemia
nutrition
Must provide adequate ____ to support increased energy demand during wound healing process
-wound complications increase with severe malnutrition
Labs: CBC, BMP, Cr, BUN, pre-albumin (short-term indicated)
-serum albumin (long-term status)
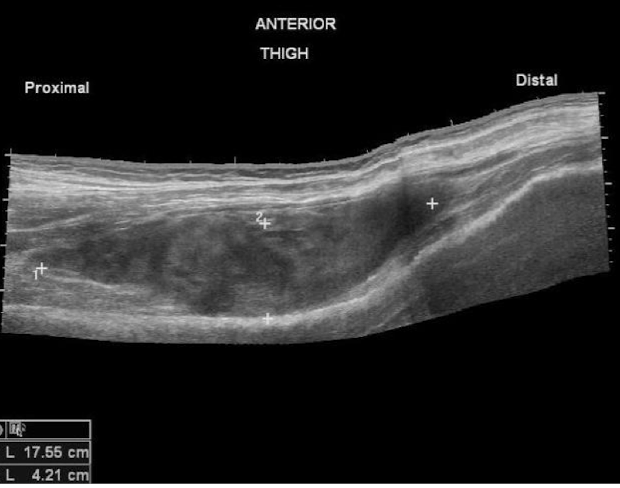
Seroma
pocket of clear secretions/blood plasma and inflammatory fluid produced by injured and dying cells
Tx: most self-limiting reabsorb, may need to aspirate (especially if purulent)
Prevention: drains, suture technique, handling of tissue, compression dressings
Hematoma
abnormal collection of blood outside blood vessel
risk factors: anticoagulation, bleeding disorders
-impairs wound healing ↑ tension and ↓ tissue perfusion
-may cause deep space infection
-may compress structures cause nerve damage
Tx: evacuate expanding hematomas surgically to regain hemostasis, drains, closed suction drainage
Dehiscence
opening or separation of a surgical incision after it has been closed, usually 5-8 days after surgery
-superficial, deep fascial layer
-evisceration of abdominal contents may occur as result
causes:
-inappropriate knots/closure
-incorrect needle/suture material
-too much tension on sutures
-hematomas/arterial bleeding
-misplacement of sutures
-removal of sutures too soon
-poor patient compliance
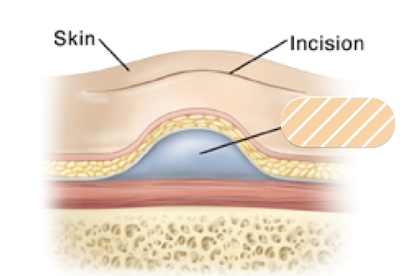
Incisional hernia
small piece of bowel protrudes through weakness or unhealed surgical wound or weakness in abdominal wall
causes: improper closure, increased pressure, pregnancy prior to to healing, noncompliance with physical activity restrictions
S/S: bulge or lump near incision site, nausea/vomiting, fever, abdominal pain, constipation or diarrhea
Tx: surgical correction

Surgical site infection (SSI)
Superficial: ~3-5 days post operative
Deep: ~7 days post-operative
risk factors: smoking and hyperglycemia (diabetes)
Prevention:
-antibiotic prophylaxis within 1 hour of incision
-careful tissue handling
-minimize blood loss
-aseptic technique
-normothermia to optimize pH and oxygen
Tx: antibiotics (IV or oral), I&D and leave open to heal by secondary intention, drain and pack abscess, explore in OR, debridement, Wound Vac
Abscess
collection of pus, can be indication for or complication of surgery
Tx: surgical I&D or OR washout, interventional radiology drain, antibiotics or local wound care
-Empiric tx (cover Staph/Strep) or defined if culture for MSSA and MRSA
MSSA: cephalexin, dicloxacillin, doxycycline, clindamycin, TMP/SMX
MRSA: doxycycline, clindamycin, TMP/SMX
IV: vancomycin, linezolid, daptomycin, clindamycin, ceftaroline (5th gen ceph), tigecycline
Necrotizing fasciitis (NSTI)
Rapidly progressive and potentially fatal infection of connective tissue/collagen fibers and tissue necrosis of hypodermis along fascial planes; Group A Streptococcus most common, Clostridium perfringens (gas gangrene)
Risk factors: elderly, burns, immunocompromised, DM, alcohol use disorder, malnutrition, obesity, unhoused, surgical wounds, puncture wounds, urinary catheters
S/S: severe pain (out of proportion to minor trauma), fetid odor, fever/SEPSIS; cellulitis, tenderness to palpation outside borders, crepitus, bullae, ecchymosis, paresthesia, hypotension, gas on plain film
Labs: WBC >15.4K, BUN>15mg/mL, serum sodium <135 to differentiate from SSTI cellulitis
Tx: emergent surgical exploration and debridement + broad spectrum antibiotics (Carbapenem + Vancomycin + Clindamycin) + hemodynamic support
Eschar
dead tissue found in full-thickness wound that impedes normal healing
-may occur after burn injury, gangrenous ulcer, necrotizing fasciitis
*NOT A SCAB

Scab
crust formed by coagulation of blood or exudate on superficial or partial thickness wound
Debridement
remove necrotic and devitalized tissue and debris, which acts like a foreign body and delay healing and may prolong the inflammatory phase of wound healing
-bloody tissue provides O2 and nutrients
Debridement
Sharp: dead tissue removed with sharp instrument, will not bleed
Autolytic: moist dressing allows the body to break down dead tissue
Enzymatic: chemical applied to breakdown dead tissue
Mechanical: wet to dry, pulse lavage, (maggots)
Serous
Clear straw colored exudate, thin and watery
-normal, possibly sign of infection
Fibrinous
Cloudy thin exudate, contains fibrin protein strands
Serosanguinous
Clear pink thin watery exudate, normal with wound healing

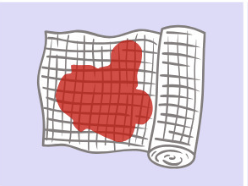
Sanguinous
Red, thin watery exudate, indicates trauma to blood vessles
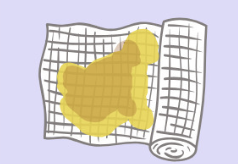
Purulent
Yellow, grey, green thick exudate, indicates infection with pyogenic organisms and other inflammatory cells
Haemopurulent
Dark, blood-stained exudate, contains neutrophils, dead/dying bacteria and inflammatory cells, established infection is present
Haemorrhagic
Thick red exudate, indicates infection or trauma, capillaries readily break down and spontaneous bleeding occurs
Controlled drainage
prevents pockets/dead space
• Closed-suction drain (JP, Blake, etc.)
• Penrose drain
• Packing tape
• Negative pressure dressing (wound vac)
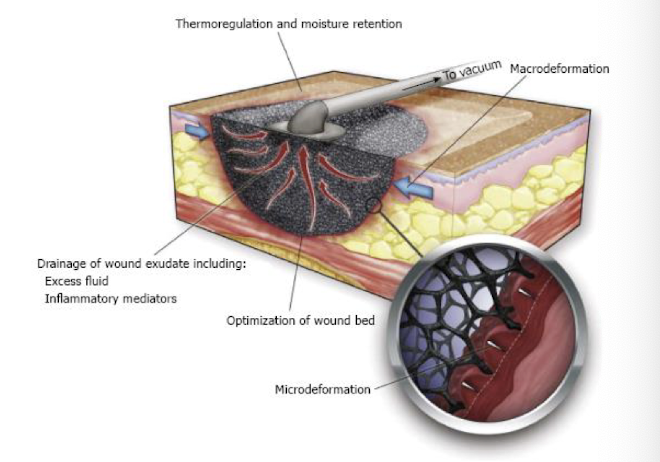
Wound VAC (Vacuum Controlled Assisted Closure)
Negative pressure wound therapy (NPWT); wound dressing systems that continuously or intermittently apply sub-atmospheric pressure to the system, which provides a positive pressure to the surface of a wound
Indications:
• Dehisced surgical wounds
• Complex operative wounds left open to heal by secondary intention
• Diabetic ulcers
• Chronic wounds
• Acute wounds
• Pressure ulcers
• Flaps and grafts
• Chronic or acute enteric fistulas
-Uninfected wound: change dressings q24-48 hours
-Infected wound: changes dressings q12-24 hours
-Do not stop or remove suction for >2 hours
-Discontinue with adequate granulation that allows change to conventional dressing, split thickness graft or flap closure
-also d/c with extreme pain, excessive bleeding, alternative treatment, local or spreading infection
Hyperbaric Oxygen therapy (HBO)
inhalation of 100% oxygen delivered at pressure of >1 atmosphere (ATA) in enclosed chamber
-adjunct or primary treatment that promotes wound healing by stimulating fibroblast, collagen synthesis, epithelialization, controlling infection
Indications:
• select non-healing wounds (Diabetic ulcers of the lower extremities)
• Chronic refractory osteomyelitis
• Compromised skin grafts and flaps
• Crush injury/acute traumatic peripheral ischemia
• Compromised skin flap or skin graft
• Crush injury of extremity
• Severe "flesh-eating" infections (i.e., gas gangrene, necrotizing soft tissue)
• Brain abscess
• Soft tissue radionecrosis and osteoradionecrosis
• Thermal burn
• Sudden deafness
• Vision loss, sudden and painless
*carbon monoxide poisoning, decompression sickness (bends), and arterial gas embolism are primary indications
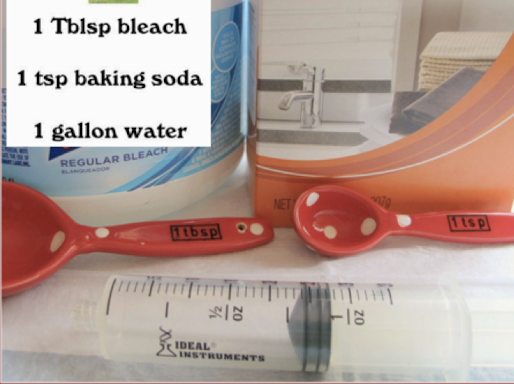
Dakin’s solution
type of hypochlorite solution bleach, can be used for MRSA
-used for diabetic foot ulcers, venous leg ulcers, pressure ulcers, post surgical wounds, 1st and 2nd degree burns, grafted donor sites
-may decrease bacterial burden on the skin, associated inflammation with atopic eczema
Surgical drain
tube to remove pus, blood, other fluids from wound, space, body cavity
-Open (Penrose) or closed (JP connected to suction)
-may be active or passive: suction or left to drain by gravity
-remove as soon as possible (decrease output)
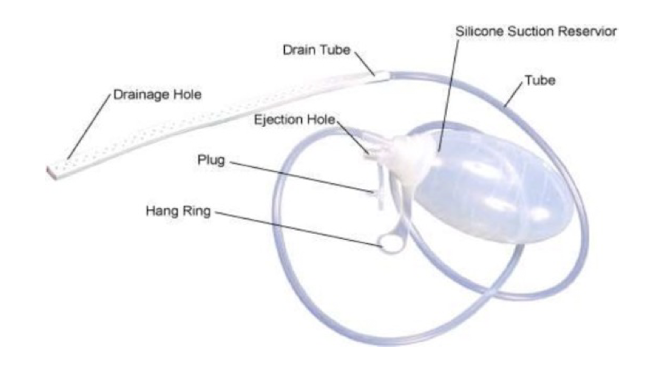
Jackson (Pratt and Hemovac)
closed, active surgical drain: connects to negative pressure device
-often used to drain wound/incision
Penrose
open, passive surgical drain: rubber tube allows for drainage
-often used for infection/abscess
-monitor for contamination

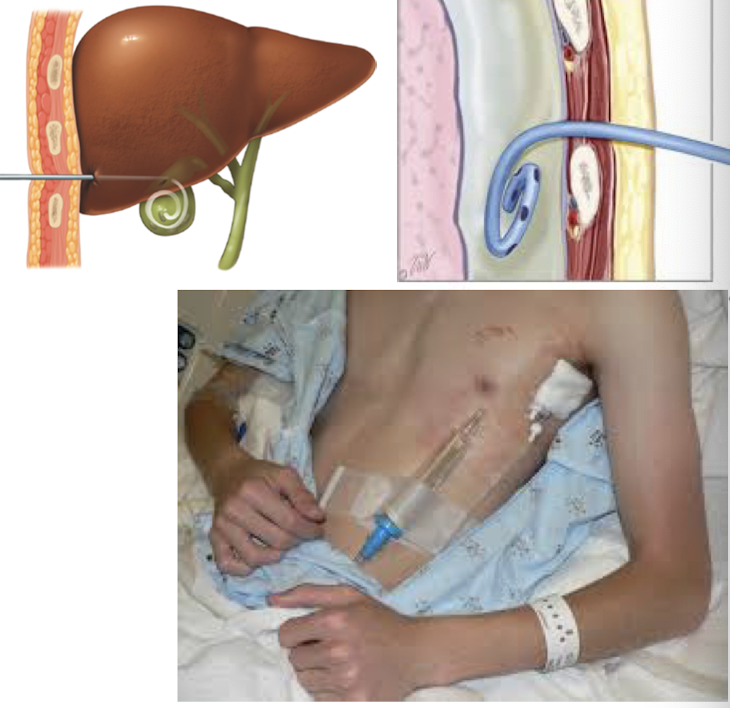
Pigtail drain
closed, passive percutaneous catheter used to remove body fluid from organ/duct
-placed and removed by interventional radiology ONLY
Indications:
• Pleural fluid/air drainage (with a flutter valve)
• Urine from kidney (nephrostomy)
• Bile from gallbladder (cholecystostomy)
• Intra-abdominal abscess
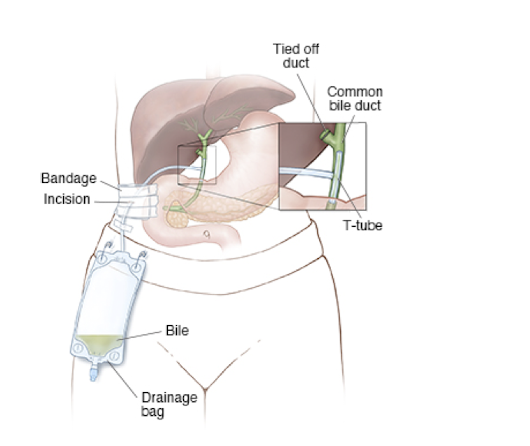
T-tube
closed, passive drain used to stent and drain the common bile duct after choledochotomy
Thoracostomy tube (Chest tube)
closed, active drain, creates negative pressure to allow reexpansion of the lung, drain, seal and apply suction to pleura-evac-system
-drains fluid/blood/air/purulence from intrathoracic space
Removal: when output <2mL/kg/day, need CXR 1-3 hours on ventilated patient
contraindications: overlying infection, pulmonary adhesions, diaphragmatic hernias, coagulopathies, anticoagulation meds
placed between 4th or 5th intercostal space at mid-axillary line (over 5th or 6th rib); tip will be in the pleural space

Urinary catheter
closed, passive gravity drain of urine, inserted as sterile procedure
• Condom catheter
• Foley (transurethral)
• Suprapubic
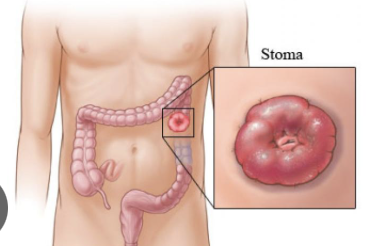
Ostomy
surgical opening which results in a stoma
-in GI or urinary tract can be used to drain waste products or provide food/medication/hydration
-can be permanent or temporary

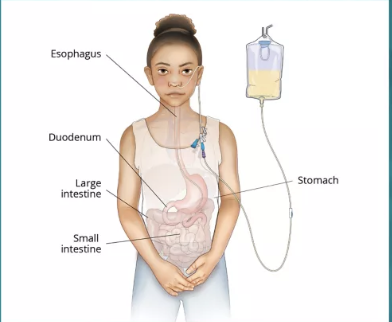
Gastrostomy (G-tube)
long term feeding tube that enters in the stomach, used for feeding and medications
-Percutaneous endoscopic gastrostomy tube (PEG tube) used for feeds and meds. Performed under endoscopy
-Mic-Key Button G tube (low profile)

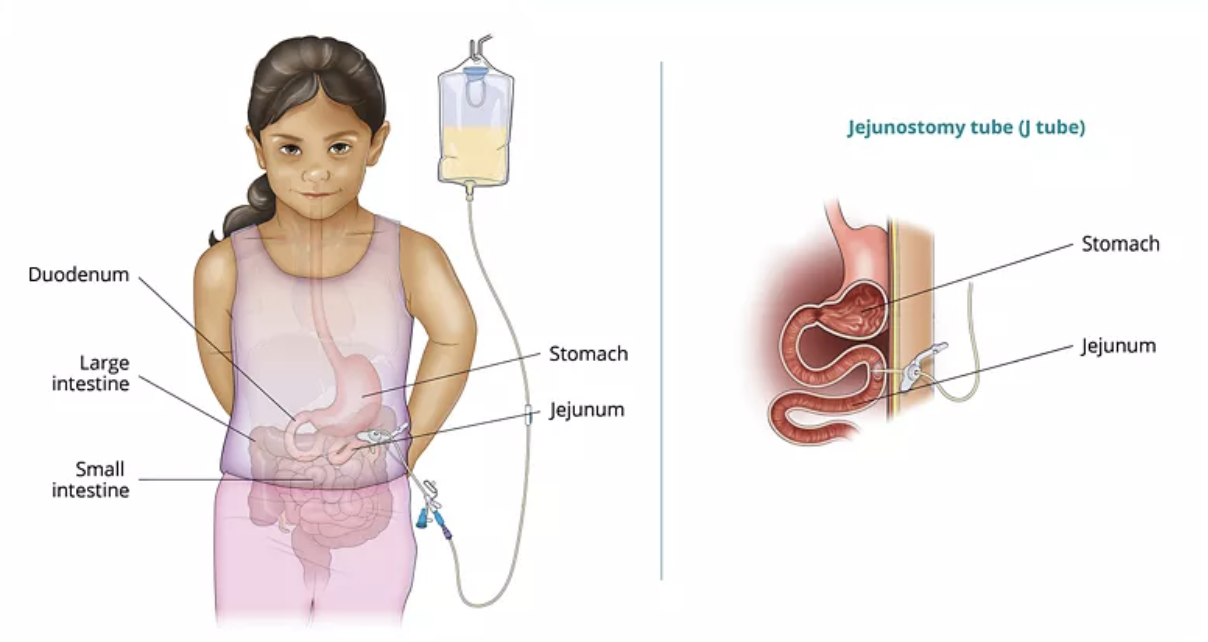
Jejunostomy tube (J-tube)
long term feeding tube that enters through jejunum and bypasses the stomach to access small intestine
-used to feed, low aspiration risk
Nasogastric tube (NG tube)
Salem (double lumen): most common; used for irrigation of stomach food and enteral tube feedings (not preferred for long-term)
Levin (single lumen): used for stomach decompression, withdrawing specimens, washing stomach free of toxic substances and irrigating stomach and treating upper GI bleeds; can be used to administer meds or feedings, not preferred
Ilieal conduit
most common form of urinary diversion (urostomy), placed after cystectomy due to bladder cancer
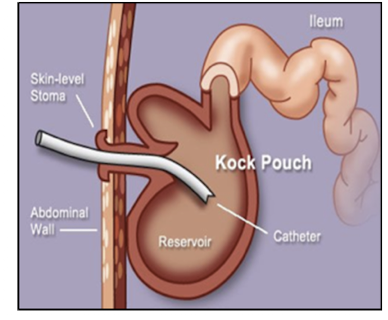
Continent iliostomy
urostomy pouch made from ileal loops, intermittent access to drain pouch as alternative urinary diversion (ilium to abdomen)
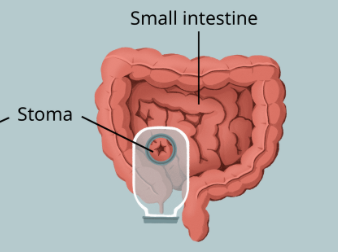
Iliostomy
surgically created opening in the abdomen in which a piece of the ileum (small intestine) is brought through the abdominal wall to create a stoma
-sections of small intestine and large intestine have been removed or require bypass
-liquid waste with digestive enzymes can be corrosive to adjacent skin
Temporary: may be required when a surgical site lower in the digestive tract needs time to heal; “loop stoma”
Permanent: may be required when the large intestine is removed and reconnection to the anus isn’t feasible; “end stoma”
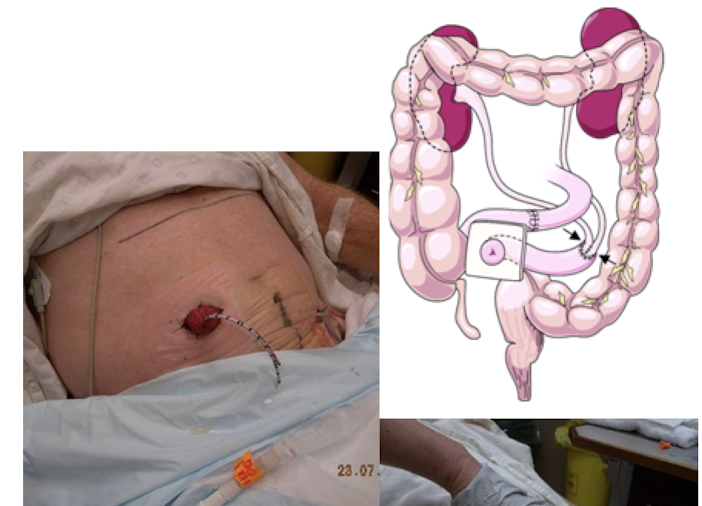
Colostomy
allows stool to bypass diseased/damaged colon through connection of colon mucosa to abdominal skin wall for stool drainage into collection pouch
-section of colon may be removed for infection, ulcerative colitis, trauma, ischemia, cancer resection
Tracheostomy
ostomy between 2nd and 3rd tracheal rings for breathing, definitive invasive infraglottic surgical airway
indications:
• Vocal cord paralysis
• Anaphylaxis
• Esophageal tumor
• Upper airway obstruction
• Neurologic disease
• Traumatic neck/mouth injuries
• Airway burns/inhalation injuries
• Laryngeal injury
gold standard long-term maintenance of airway in adults and children (cricothyrotomy is not performed in children)
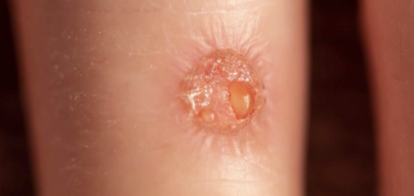
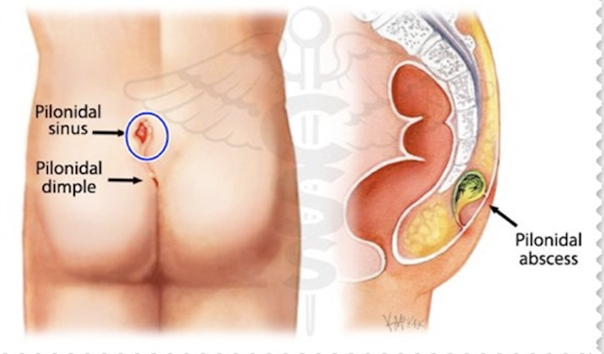
Pilonidal cyst (sinus)
congenital or acquired, AMAB, 30-45yo, prolonged sitting/slouching, large amounts of body hair, obesity, inactivity
Tx: antibiotics (Augmentin, Cipro/Flagyl, Bactrim if acutely infected) + incision and drainage
-surgical referral to remove the tract/sac
Fistula
abnormal communication between:
• two hollow viscus lumens/organs (internal)
• hollow organ/viscus lumen and the skin (external)
• two vessels
risk factors: prior trauma/surgery, cancer or infection/inflammation
Types: Enterocutaneous (GI-skin, colonic); Anal, Bladder, Vascular
Fistula
• High output fistula (>500 cc/day)
• Intestinal destruction (50% of circumference)
• Short segment fistula 2.5 cm (long ones close easier)
• Foreign body (e.g., G-tube)
• Radiation
• Infection
• Epithelization (e.g., colostomy)
• Neoplasm
• Distal obstruction
predisposing factors that maintain patency of ____: “HIS FRIEND”
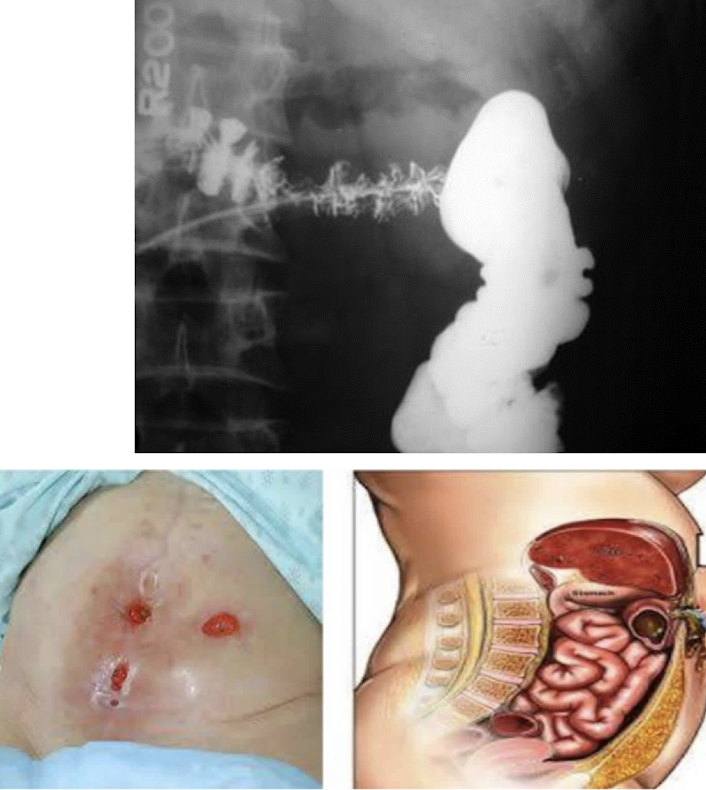
Enterocutaneous fistula
abnormal connection of GI tract to skin
Causes:
• Anastomotic leak
• Trauma/injury to the bowel/colon
• Crohn’s disease
• Diverticulitis
• Inflammation/infection
Dx: CT scan to r/o infection/abscess, fistulogram
Tx: NPO, nutrition (TPN), drain abscess, surgical operation and resection
Complications: high-output, malnutrition, skin breakdown
Colonic fistula
subtypes: Colovesical (most common type), Colocutaneous, Colovaginal, Coloenteric fistulas
-Diverticulitis (most common cause), Cancer, Inflammatory Bowel Disease, Foreign body, Irradiation
Dx: CT with oral contrast, barium enema, cystogram, cystoscopy
Tx: segmental colon resection and primary anastamosis, repair/resection of organ
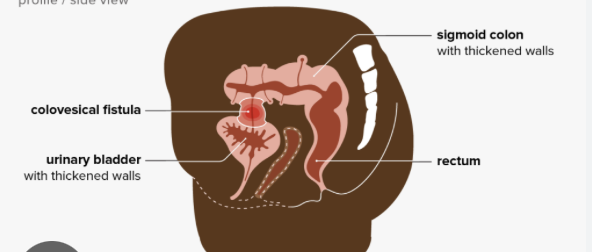
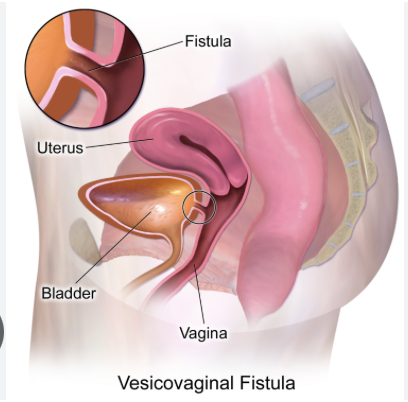
Bladder fistula
Vesicoenteric: 50% due to sigmoid diverticulitis causing pneumaturia, fecaluria (air or stool in urine)
Vesicovaginal (obstetric fistula): secondary to GYN procedure causing urinary leak through vagina
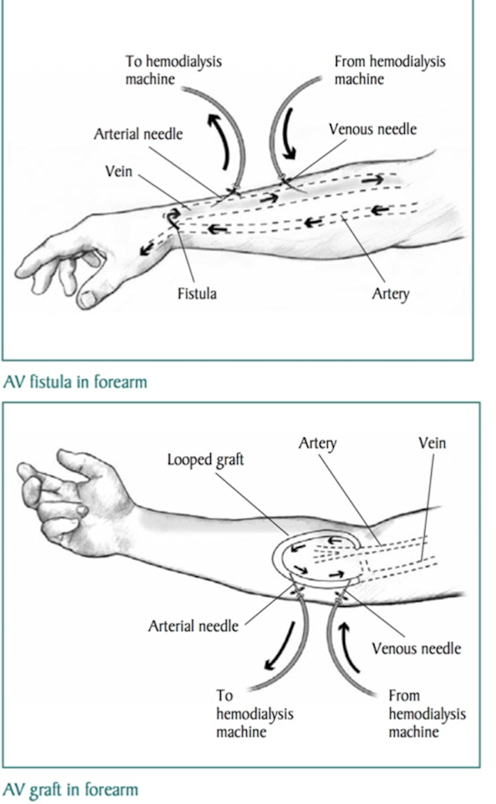
Vascular fistula
abnormal connection or passageway between artery and vein
-may be congenital, surgically created for hemodialysis, acquired during trauma or erosion of arterial aneurysm