Lecture 9 - Antidepressants & Anxiolytics Student Version
DEPRESSION
Depression is very common throughout the world, and it consists of a wide variety of symptoms from lethargy to sadness and despair.
Current thought on understanding depression focuses on monoamines, glucocorticoid levels, and a combination of factors.
There are several options of antidepressants for treatment available, including MAOIs, tricyclics, SSRIs, and SNRIs. Individual response to medication can vary greatly.
DSM-5 MAJOR DEPRESSIVE DISORDER (MDD)
Diagnostic Criteria as outlined in DSM-V
Five (or more) of the symptoms have been present during the same 2-week period and represent a change from previous functioning; At least one of these symptoms is a) depressed mood or b) loss of interest or pleasure.
The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The episode is not attributable to physiological effects of a substance or another medical condition.
WHAT IS COMMONLY SEEN IN MDD?
Common Symptoms:
Persistent depressed mood
Diminished interest/pleasure in all or most activities
Significant/abnormal change in weight/appetite
Insomnia/Hypersomnia or other sleep related issues
Psychomotor agitation
Fatigue/Loss of energy
Feeling worthlessness or excessive/inappropriate amounts of guilt
Diminished ability to think or concentrate
Recurrent thoughts of death, suicide ideation or suicide attempts.
THEORIES OF DEPRESSION
Monoamine hypothesis: It is thought that depression is linked to reduced levels of serotonin, norepinephrine, and dopamine. A reduction of serotonin seems to be a key factor in depression. There are abnormalities in the 5-HT receptors seen in depressed individuals.
Glucocorticoid Theory of Depression: The HPA axis controls the body’s response to stress. Heightened cortisol levels encourage DA release and structural change within the mesolimbic DA system. One such change is an upregulation of DA receptors in the ventral tegmental area. Abnormal HPA-axis function precedes the onset of clinical symptoms of depression.
ANTIDEPRESSANTS
First-generation antidepressants: Monoamine oxidase inhibitors (MAOIs) and Tricyclic antidepressants were developed in the late 1950s.
MAOIs: include iproniazid (Euphozid), phenelzine (Nardil), tranylcypromine (Parnate), isocarboxazid (Marplan), selegiline (Eldepryl), moclobemide (Aurorix).
Second-generation antidepressants: The second generation includes the selective serotonin reuptake inhibitors (SSRIs) such as Prozac.
Third-generation antidepressants: These drugs include the serotonin and norepinephrine reuptake inhibitors (SNRIs) that affect the functioning of both of those monoamines. Examples include venlafaxine (Effexor), desvenlafaxine (Pristiq), duloxetine (Cymbalta), mirtazapine (Remeron).
PHARMACOKINETICS
Absorption: Antidepressants are readily absorbed into the body, crossing barriers. They take weeks to fully work. TCAs are absorbed more quickly than the other drugs.
Distribution: Antidepressants readily cross blood-brain and placental barriers.
Elimination: MAOIs have relatively short half-lives, especially compared to TCAs. There is a lot of individual variability. Genetic differences affect the longevity of the drugs.
PHARMACODYNAMICS
MAOIs: inhibit (block) the activity of monoamine oxidase so that molecules of DA, NE, and 5-HT that float freely in the cytosol are not destroyed but, instead, are available for vesicle storage and later release.
Tricyclics: The principal mechanism of action is to block reuptake transporter proteins on the axon terminals of 5-HT and NE neurons so that, after these monoamines are released into the cleft by an action potential, their reuptake is inhibited and their duration of action on the postsynaptic cell is prolonged.
Side effects include dry mouth, constipation, blurred vision, ringing in the ears, and urine retention. Weight gain is also very common.
SSRI/SNRI
SSRIs: SSRIs diminish the ability of presynaptic cells to reabsorb and recycle 5-HT.
SNRIs/Atypicals: The SNRIs and atypicals block the reuptake of 5-HT, NE, and in some cases DA.
Side effects are very minimal for both of these drug classes.
EFFECTS OF ANTIDEPRESSANTS
These drugs do not cause euphoria and are not sold on the street.
Effects on personality: Prozac and other drugs can give confidence to their users.
Effects on sleep: MAOIs can cause sedation or insomnia. Tricyclics have been used to help treat insomnia. Many antidepressants reduce REM and users report more vivid dreams.
Effects on Performance: It is hard to tell if there are changes in performance due to these medications or the underlying depression. Some individuals do experience withdrawal from these medications, all cases should be monitored closely.
Chance of violence: Prozac and other medications have been correlated with violent outbursts.
Higher risk of suicide and suicidal thoughts.
ANXIOLYTICS: SEDATIVE HYPNOTICS
ANXIETY
Anxiety can come in a variety of forms, usually diagnosed using the DSM-V.
Anxiety manifests in a variety of ways and is very common.
fMRI studies show increased activity in the brain, with the location varying per the disorder
OCD and PTSD have been reclassified in the DSM-5, but are still treated with anti-anxiety medications.
These disorders tend to present with both depression and with insomnia.
SEDATIVE HYPNOTICS
Barbiturates and benzodiazepines have both been shown to be effective at lowering the symptoms of anxiety and may improve sleep.
A variety of historical factors helped lead to the development of anti-anxiety drugs.
Barbiturates were first, but they had negative side effects and high risks of dependency.
Benzodiazepines were developed later and have been shown to be safer than barbiturates.
Both drugs work with GABA receptors to help modulate anxiety and its symptoms.
HISTORY OF SEDATIVE HYPNOTICS
Alcohol only depressant used until late 1800s
Late 1800s: Barbiturates replaced alcohol as a medicinal sedative
Early 1900s: Benzos replaced barbiturates as sedatives/hypnotics/anti-anxiety agents
1960s: Benzos replaced barbiturates as sedatives/hypnotics/anti-anxiety agents
1970s: Social problems related to benzos due to misuse
SEDATIVE HYPNOTICS
Barbiturates and benzodiazepines have a strong effect on many behaviors, ranging from sleep to driving.
Barbiturates have a high risk for dependency & benzodiazepines also have a risk for dependency, although relatively less dependance liability.
Withdrawal from benzodiazepines must be completed carefully with physician supervision.
SEDATIVE HYPNOTICS
Barbiturates and benzodiazepines treat both anxiety and provide sedation and are about two-thirds of all prescribed drugs.
Nonbenzodiazepines include Ambien and are fairly safe.
Therapeutic properties: The principal mechanism of action is the modulation of GABAA receptor activity, but the drugs have different binding sites.
Anxiolytics and sedative-hypnotics share properties with alcohol, with inhaled solvents, and with other substances generally called depressants or general anesthetics.
PHARMACOKINETICS
SEDATIVE HYPNOTICS
Absorption: Both barbiturates and benzodiazepines are weak acids and absorption from the digestive tract is quicker than when it is intramuscular.
The various benzodiazepine drugs range quite widely in their lipid solubility and, as a result, vary in their speed of absorption.
Age heavily influences absorption rates. Alcohol also affects absorption.
Distribution/Elimination: Highly lipid-soluble substances pass easily through the blood–brain barrier and their effects on the brain are quickly felt, but the effects are short-lived.
Half-life and lengths of activity are unique in this drug class…
SEDATIVE HYPNOTICS
PHARMACODYNAMICS
SEDATIVE HYPNOTICS
Neuropharmacology: Barbiturates and benzodiazepines’ effects are mediated primarily by their ability to modify transmission of the inhibitory transmitter GABA, specifically at the GABAA receptor.
They are allosteric modulators; they have their own binding sites on the GABAA receptor complex that, when occupied, enhances the effects of GABA binding.
SEDATIVE HYPNOTICS
Z drugs are nonbenzodiazepine hypnotics, including zolpidem, primarily cause sedation.
These work in a similar fashion to what we see with traditional benzos.
SEDATIVE HYPNOTICS EFFECTS
SEDATIVE HYPNOTICS
Effects on the Body: The effects of barbiturates are dose-dependent, and at high doses, they can have life-altering effects.
Benzodiazepines are safer (relatively) and can be used for a variety of conditions.
Effects on Sleep: Benzodiazepines are effective with sleep, Z drugs even more so with their short half-lives.
There is often a withdrawal period when discontinuing these drugs.
SEDATIVE HYPNOTICS
Subjective Effects: Euphoria and liking for the drug have been reported with benzodiazepines, but not consistently.
Effects on Memory and Performance: Retrograde memory does not seem impacted by benzodiazepines, but the ability to make new memories can be impacted, especially with alcohol use.
There is an impact on explicit memory, but not with implicit memory except for lorazepam use.
SEDATIVE HYPNOTICS
Laboratory studies with humans and self-administration: Johanson and Uhlenhuth (1980) conducted an experiment where people chose d-amphetamines more than placebos but did not choose diazepam more than a placebo.
Roland Griffiths later found that barbiturates are a positive reinforcer.
Human Self-Administration Outside the Laboratory: People frequently continue to take benzodiazepines beyond the prescribed time/amount, and they are associated with dependency.
On the street, benzodiazepines are often taken with another drug.
SEDATIVE HYPNOTICS
HARMFUL EFFECTS SEDATIVE HYPNOTICS
Overall, benzodiazepines are relatively safe, although there is some link with possibilities of birth defects.
Effects on reproduction: There is some link between benzodiazepines and birth defects and also issues with delivery.
Few issues are reported with men.
HARMFUL EFFECTS SEDATIVE HYPNOTICS
Risk of overdose: Benzodiazepines are much safer than barbiturates, BUT these do have OD potential. Alcohol has a serious impact on the risk of overdose.
Anxiolytic and sedative-hypnotic dependence: Tolerance is often noted, and care must be taken with stopping the medication.
This is thought of as the major drawback/risk of utilizing these drugs.
HARMFUL EFFECTS SEDATIVE HYPNOTICS
Tolerance: Some behavioral effects have been noted with acute tolerance.
With repeated use, there is less effectiveness with modulating GABA. Tolerance is related to dose and duration.
Cross-tolerance is often noted, which suggests that tolerance to barbiturates and benzodiazepines may arise from mechanisms that are similar, but not identical.
HARMFUL EFFECTS SEDATIVE HYPNOTICS
Withdrawal: Withdrawal from barbiturates may be blocked with benzodiazepines.
Withdrawal from benzodiazepines occurs in two forms: sedative-hypnotic and low-dose withdrawals.
Managing benzodiazepine withdrawal: Supervision of those withdrawing from extended use of benzodiazepine is necessary, including possible hospitalization, gradually reducing the dose, and exploring behavioral therapies.
DO YOU KNOW OF ANY UTILITY OF THESE DRUGS? (HINT: WE HAVE TALKED ABOUT THIS BEFORE..) THOUGHT QUESTION
ALCOHOL WITHDRAWAL SYNDROME
Joe is at a party and he stopped drinking an hour ago. There is alcohol still in his blood, but it is declining quickly (BAC is declining). He is experiencing tremors, muscle weakness, increased HR, and he does not feel like eating.
What stage of the alcohol withdrawal syndrome?
Why are all of these withdrawal symptoms occurring?
ALCOHOL WITHDRAWAL SYNDROME
ADAPTATION: Body wants to maintain homeostasis
Inhibitory effect of GABA
Excitatory effect of Glutamate
While you are drinking
ALCOHOL WITHDRAWAL SYNDROME
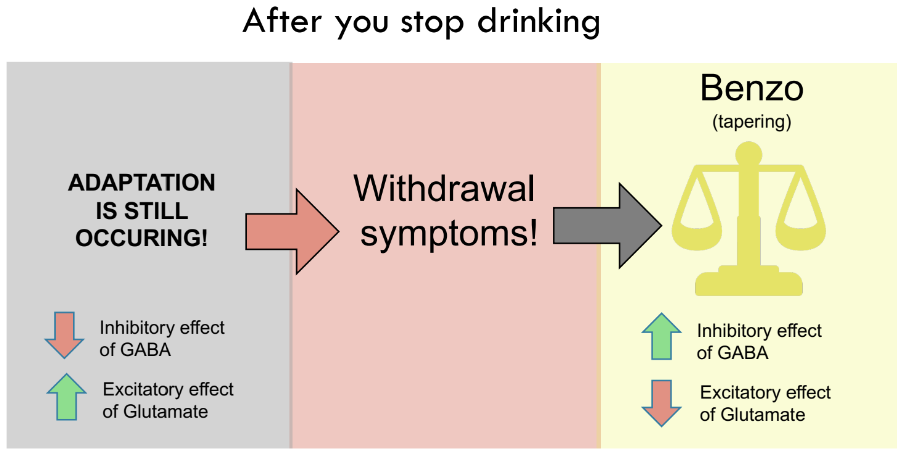
After you stop drinking
ADAPTATION RESPONSE IS STILL OCCURRING (but no more alcohol)!
Inhibitory effect of GABA
Excitatory effect of Glutamate
Withdrawal symptoms!
ALCOHOL WITHDRAWAL SYNDROME
Joe is at a party and he stopped drinking an hour ago. There is alcohol still in his blood, but it is declining quickly (BAC is declining). He is experiencing tremors, muscle weakness, increased HR, and he does not feel like eating.
What should/can be administered to help deal with this stage of the alcohol withdrawal syndrome? (HINT: this will reduce the chance Joe will go into the next stage)
ALCOHOL WITHDRAWAL SYNDROME
Joe can be administered a benzo to help him deal with the alcohol withdrawal syndrome and he is starting to feel better.
Why/how did the benzo help? What’s happening inside the body?
ALCOHOL WITHDRAWAL SYNDROME
ALCOHOL WITHDRAWAL SYNDROME
Stage Description Symptoms Medication
One: Occurs within hours of drinking cessation; still alcohol in the blood, but declining rapidly (i.e., decline in BAC)
Tremors, muscle weakness, agitation, irritability, insomnia, increased heart rate, loss of appetite, excessive sweating
Benzodiazepine (e.g., Valium)
Two: Within 24 hours after stopping drinking; BAC declining, approaching 0
Auditory, visual, tactile hallucinations
Benzodiazepine (e.g., Valium)
Three: Delirium Tremens (DT); onset between 24 and 48 hours after drinking; BAC at 0; duration up to 4 days (Up to 15% mortality rate)
ALL SYMPTOMS ABOVE + Severe agitation, confusion and disorientation. Marked hallucinations and delusions (followed by amnesia). Rapid heart rate; hyperthermia
Benzodiazepine (e.g., Valium)