TBI exam 1
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
63 Terms
Definition of TBI
a traumatically induced structural injury and/or structural injury and/or physiological disruption of brain function physiological disruption of brain function as a result of an external force indicated by new onset of at least one of the following clinical signs immediately following the event:
-Any period of loss of or decreased level of consciousness
-Any loss of memory for events immediately before or after
-Any alteration in mental state(confusion, disorientation, slowed thinking, etc. also known as alteration of consciousness
-Neurological deficits (weakness, loss of balance, change in vision, praxis, paresis/paraplegia, sensory loss, aphasia, etc) that may or may not be transient
- intracranial lesion
How is TBI different from other acquired brain injuries
TBI is a specific type of acquired brain injury and is always caused by an external force
External force
-an object striking the head
-acceleration/deceleration movements
- foreign body penetrating the brain
- forces generated from a blast or explosion
Key components from TBI definition
- ALTERATIONS IN BRAIN FUNCTIONING
- EVIDENCE OF BRAIN PATHOLOGY (lab test results, ct scan, imaging results)
-CAUSED BY EXTERNAL FORCES
Most common causes of TBI
1. falls
2. motor vehicle accidents
Other leading causes:
-Unintentionally being stuck with an object
- Assaults
-Intentional self harm
-Sport injuries
-Abuse
relating to falls -
Hospitalization rates were highest among persons 75 or older
second highest for children 0-4 years of age
Risk factors for TBI
Factors which increase the risk of TBI:
- Alcohol use and abuse
-Previous TBI
- Preexisting medical conditions
High Risk Populations:
-Professional athletes
-People incarcerated for criminal offenses
-People in homeless shelters
-Victims of domestic abuse
(males have higher rates of TBI)
Best prognostic indicator for TBI
Post traumatic amnesia
-period during which an individual cannot store and recall an ongoing event
- PTA begins at the time of injury and persists until the patient can recall information for a 24 hour period
What tools are used to measure Post traumatic amnesia
For Adults
-Galveston Orientation and Amnesia Test (GOAT)
-Orientation Log (O-Log)
For children
-Westmead PTA scale for children (WTPAS)
-Sydney Post-TraumaticAmnesia Scale (SYPTAS)
What is the GSC
Glasgow Coma Scale
A key tool used in assessing the level of consciousness in individuals with TBI.
It helps determine the severity of the injury
Prognosis for those with Apolipoprotein E4 allele
associated with poorer outcomes and slower recovery
penetrating (open) brain injury
-skull is fractured and meninges torn, brain is exposed to the environment
-Skull is pierced by an object, and meninges are ruptured
-Could be caused by a bullet, shrapnel, bone fragment, or weapon such as a bat, hammer, or knife
-Classified as high velocity or low velocity
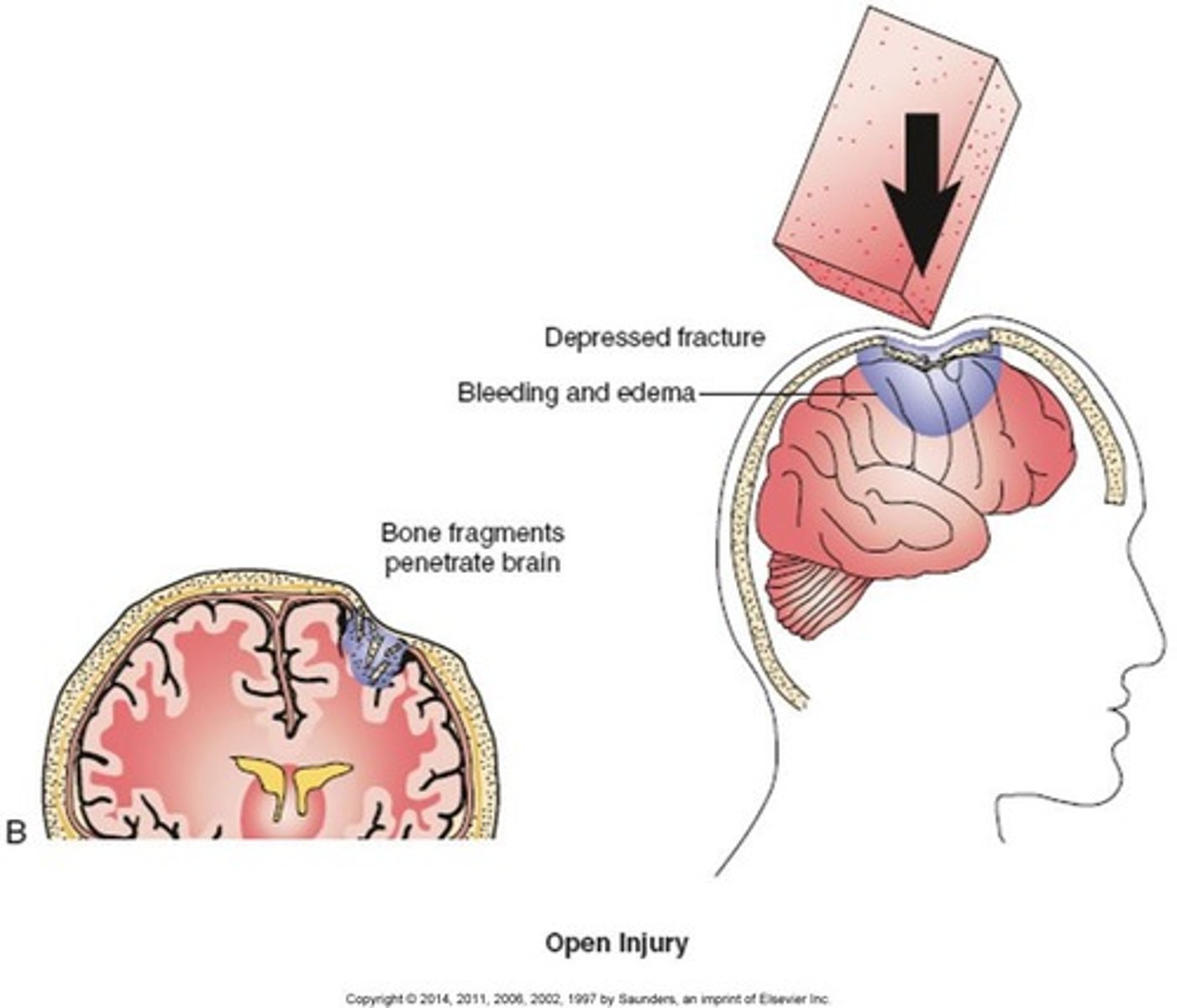
High Velocity penetrating brain injury
-Caused by high velocity objects such as rifle bullets, artillery shells, and shell fragments
-Result in more complex injuries
-Higher mortality rate
-High levels of kinetic energy and resulting shock wave cause: crushing and cutting of brain tissue along the path, shearing and stretching of brain tissue, surrounding area of tissue damage due to leakage of blood into brain tissue
Low Velocity penetrating brain injury
-Penetrating object traveling at a lower speed, such as a bat, club, or knife
-Rarer but have a better outcome
-Cause lacerations to the scalp, depressed skull fractures, and localized brain tissue damage along the object path
-Risk of infection if the projective does not exit the skull
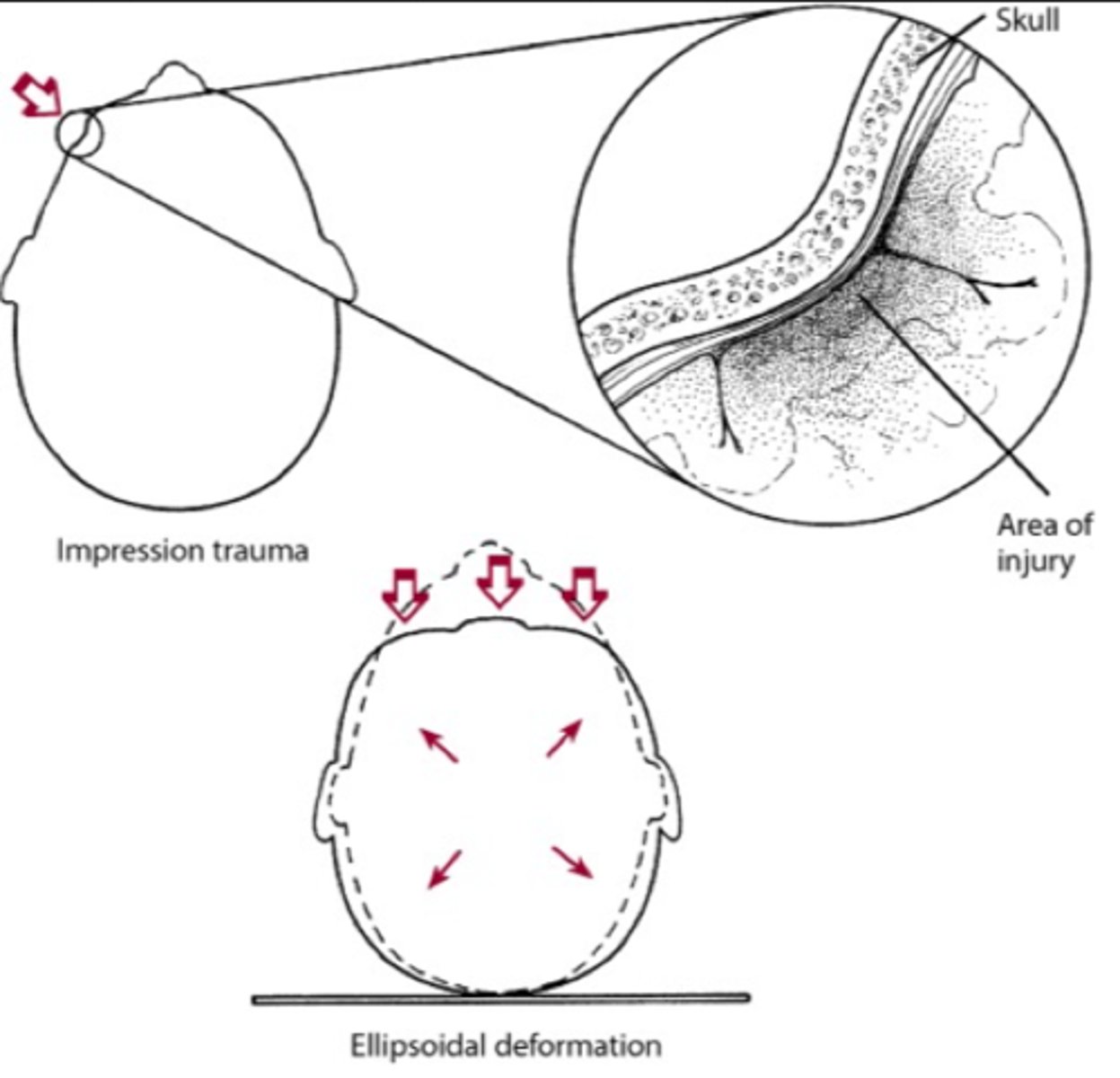
non penetrating (closed) brain injury
-skull and meninges remain intact, brain is not exposed
-classified as non-acceleration and acceleration/deceleration injuries
Non accelerating injuries
-Less severe brain damage
-Injuries are related to the deformation of the skull by the object
-The skull is pushed inward at the point of impact
Impression trauma
localized damage at the point of impact to the meninges and brain cortex
Ellipsoidal deformation
-skull forced by object to more circular shape
-Expansion causes stretching and shearing of brain tissues and blood vessels
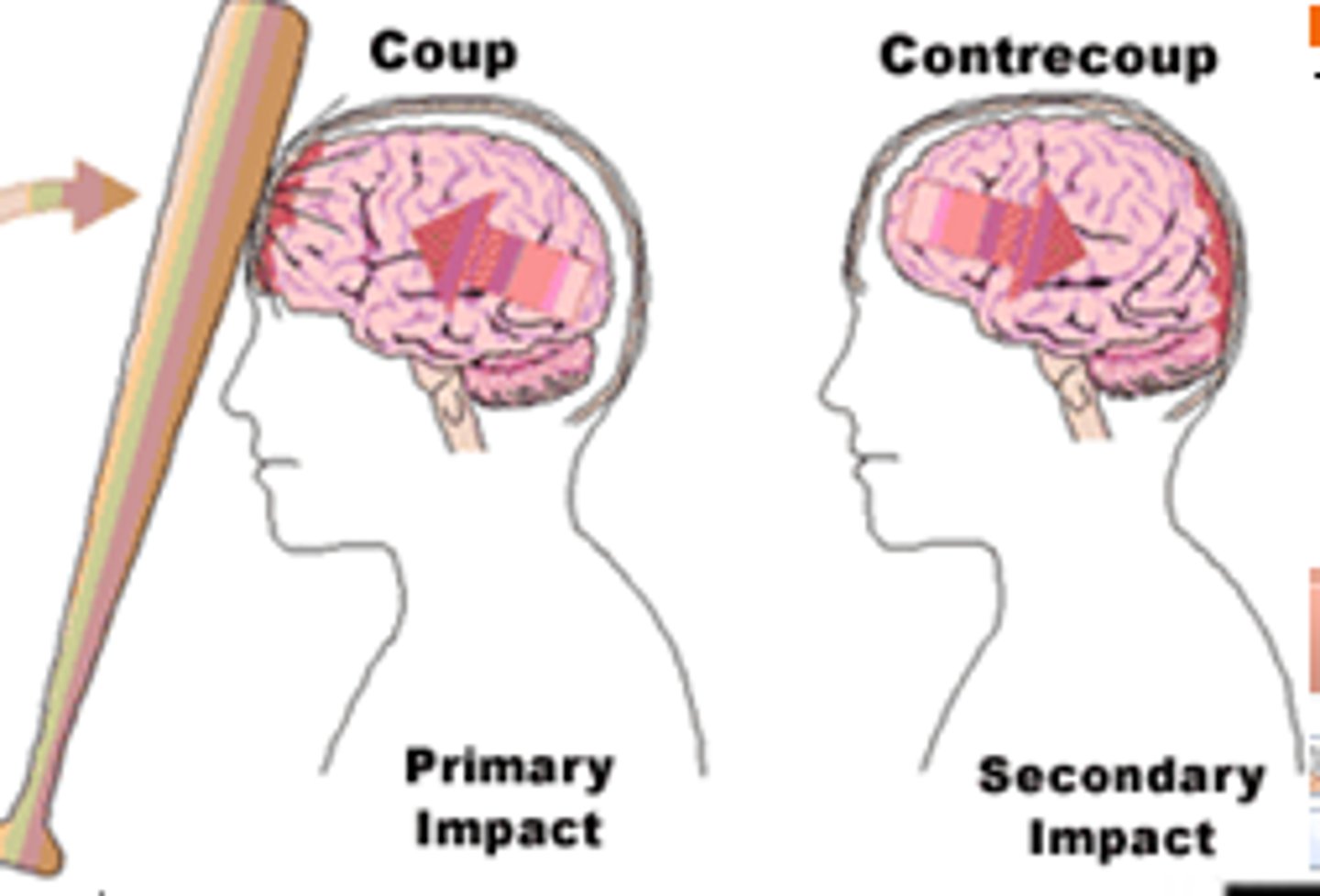
acceleration/ deceleration injuries
- Translational acceleration- travels through the head's center of gravity, pushes the head in one direction, such as forward and backward movement (Linear acceleration)
- Rotational acceleration- force passes through the head other than the center of gravity, the head rotates in a horizontal or vertical direction
Coup and Contrecoup injury
The translational force to the skull causes:
- Positive pressure at the place of impact
-Negative pressure at the place directly opposite the impact
COUP- Damage at the site of impact
CONTRECOUP- Damage at the point opposite the site of impact
Primary effects of TBI
-Skull fracture
-Contusion
-Blood vessel laceration
-Hematoma
-Hemorrhage
-Diffuse axonal injury
-Cavitation Effect
Cavitation Effect
-Negative pressure in the area opposite to the impact drops below the vapor pressure level (liquid changes to gas)
-Fluid in the brain converts to a gas in the form of bubbles
-As the negative pressure rises above vapor pressure level, the gas bubbles burst, which destroys brain cells
Skull fracture
-breaking of bony skull
-28-50% given severe TBI, the likelihood of dying is greater
- Increases the likelihood of bleeding in the brain
Contusion
-Bruise on the surface of the brain
-Focal injury where brain tissue comes in contact with bony protuberances of the skull base
-Typically involve only the grey matter
Laceration
-Cuts that may occur to the scalp, meninges, brain, or vascular structures
-Tearing of blood vessels and/or brain tissue due to brain movement across the hard ridges of the skull
Diffuse Axonal Injury
-Damage to axons caused by trauma
- Nerve axons are stretched
-2-3 hours later, stretched axons swell and then can separate
Hematomas and Hemorrhages
Three types
Epidural, subdural, intracranial
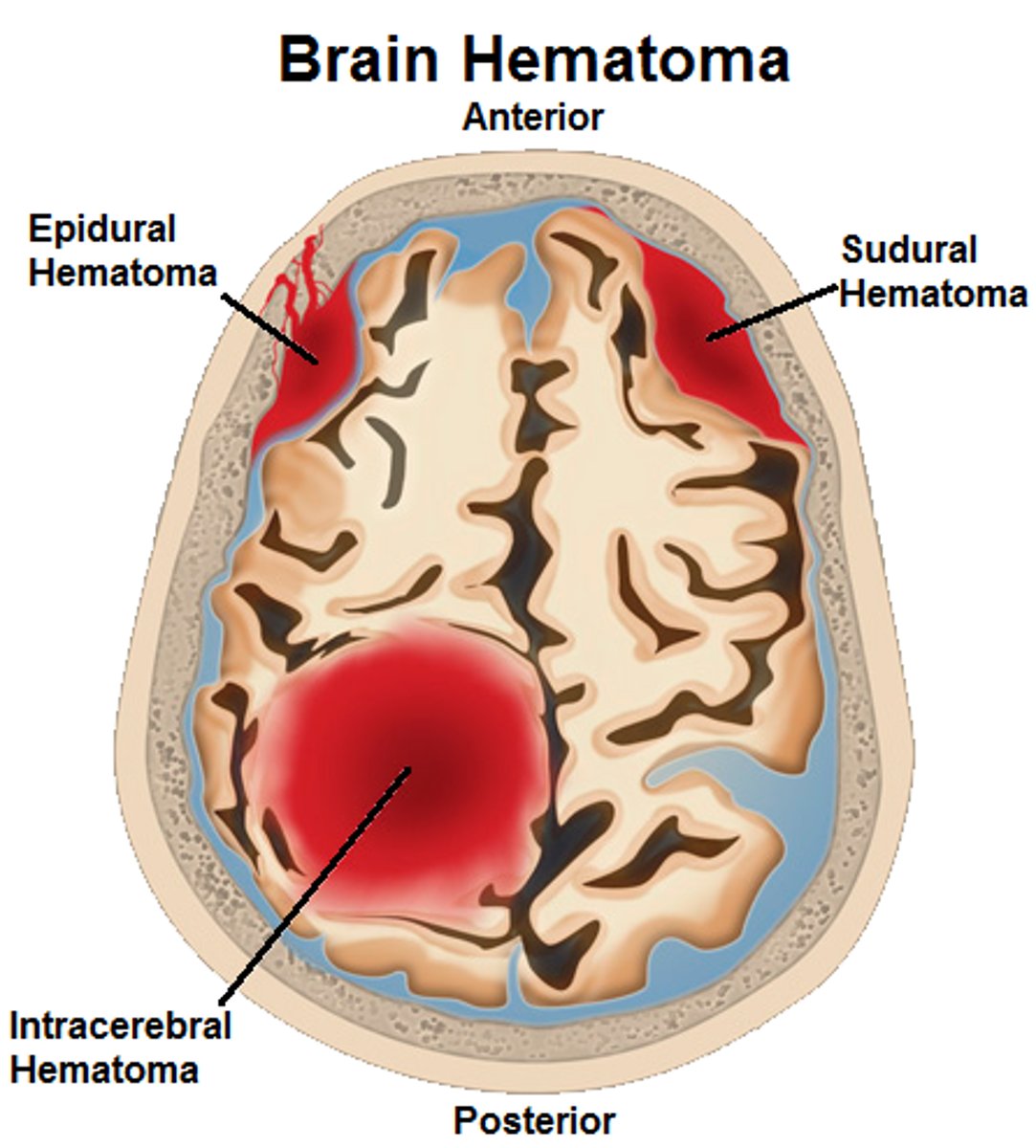
Epidural Hematoma
-Accumulation of blood between the skull and dura mater(outermost layer of meninges)
-Less than 1% of TBIs
-Caused by a laceration of an artery supplying blood to the meninges
-Easily treated if identified quickly
- Most common treatment is surgical removal- not difficult to drain surgically
Subdural Hematoma
-Accumulation of blood beneath the dura mater and above the arachnoid mater
-More common and more serious than epidural hematomas
- Can push inward and cause compression and shift of brain tissue
-Surgical treatment is common for acute cases
Intracranial Hematoma
-Intracerebral hemorrhage- rupture of blood vessels in the brain
-Often occurs in the subarachnoid space when rotational forces tear an artery or vein, Also occur in the lateral ventricles
- Most serious and most difficult to treat
Secondary Effects
-Neuronal degeneration
-Cerebral edema
-Delayed intracerebral hemorrhaging
-Increased Intracranial Pressure
Neuronal Degeneration
-DAI and disruption of the blood brain barrier leads to a release of chemicals
-Chemicals act as toxins and cause dysfunction of neurons
Cerebral Edema
-Consequence of a disruption of the blood-brain barrier or to the membranes surrounding the nerve cells
-Almost always occurs at the primary site of injury
- Two forms: vasogenic and cytotoxic
-Increases the fluid content in the cranium= less space so structures become compressed
- Craniectomy= a surgical procedure where a portion of the skull is removed to allow the brain to expand, typically in response to swelling or increased intracranial pressure
Delayed Intracerebral Hemorrhaging
-Often occurs as a primary effect
-If it is delayed by hours, days or weeks then it is a secondary effect
-Delay in bleeding occurs from swollen tissues
Increased Intercranial Pressure
-End result of secondary mechanisms
-Most common cause of death
-Rapid and uncontrolled pressure rises can destroy brain tissue and cause death
- Normal is 5-15 mmHg adult, 3-7 mmHg children
Damage occurs > 40 mmHg
> 60 mmHg leads to death
Primary Phase waves of effects from Blast Injury
Impact of the over-pressurization wave with body surfaces resulting in tympanic membrane rupture, abdominal hemorrhage, concussion, eye rupture, blast lung
Secondary Phase waves of effects from Blast Injury
Blast winds behind the pressure cause flying debris (bomb fragments), resulting in eye penetration, open head brain injury
Tertiary Phase waves of effects from Blast Injury
The individual thrown by blast wind, causing bone fractures, traumatic amputations, crushing injuries, closed and open head injuries
Quaternary Phase waves of effects from Blast Injury
Injuries due to explosive products(heat and light) and from exposure to toxic substances from fuels, metals and gases, cause burns, injury, or incapacitation from inhaled toxic fumes
Quinary Phase waves of effects from Blast Injury
refers to consequences of post-detonation environmental contaminants, including chemical, biological, and radiological substances; causes chemical burns, radiation exposure, viral or bacterial infections
Polytrauma
occurs when a person experiences injuries to multiple body parts and organ systems, often, but not always, because of a blast-related event
Conciousness
State of awareness of self and the environment with appropriate arousal or wakefulness
Coma
-No eye opening or visual pursuit
-Unable to follow instructions
-No speech or other forms of communication
-No purposeful movement in response to painful stimuli, light or sound
-Not due to paralytic agent, sedatives another psychiatric disorder
-No evidence of cognitive motor dissociation
-"Neither awake nor aware"•
-Lasts 2-4 weeks, and then sleeping and waking states are discernible
-Time-limited condition that leads to death, recovery of consciousness, or transition to unresponsive wakefulness syndrome
Unresponsive Wakefulness Syndrome
-No evidence of awareness of self or environment, and an inability to interact with others
-No evidence of sustained, reproducible, purposeful, or voluntary behavioral responses to visual, auditory, tactile, or noxious stimuli
-No evidence of language comprehension or expression
-Intermittent wakefulness manifested by the presence of sleep-wake cycles
-Sufficiently preserved hypothalamic and brain-stem autonomic functions to permit survival with medical and nursing care
-Variably preserved cranial-nerve reflexes
"Wakefulness without awareness"
Spontaneous movements
Minimally Conscious State
At least one of the following behaviors must be demonstrated on a reproducible or sustained basis:
- Following simple commands
- Gestural or verbal yes/no responses, regardless of accuracy
-Intelligible verbalization
-Purposeful behavior, including movements or affective behaviors that occur in contingent relation to relevant environmental stimuli and are not due to reflexive activity
-movements or emotional responses triggered by environmental stimuli
Post traumatic Confusial State
-All four of the following core features must be present:
-Disturbances of attention: Reduced ability to focus or sustain attention
- Disorientation: Impaired orientation to place, time,and situation
Disturbances of memory: Impaired ability to encode and recall new information
- Fluctuation: The character and severity of the disturbance waxes and wanes during the course of the day
locked in syndrome
-A condition in which a patient is aware and awake but cannot move or communicate verbally because of complete paralysis of nearly all voluntary muscles except the eyes.
-Complete paralysis of voluntary muscles except for vertical eye movements and blinking, with preserved consciousness and cognition
Best tool for ongoing assessment and monitoring change of DOC
-JFK CRS-revised is the most recommended tool, has the best psychometric properties
-Coma/Near Coma Scale
-Glasgow Coma Scale
- JFK Coma Recovery Scale-Revised
-Western Neuro Sensory Stimulation Profile
-Disorders of Consciousness Scale
-Sensory Modalities and Rehabilitation Technique
Monitor facial expression, reflexive movements, voluntary movements of limbs, eye opening/closing, and visual scanning/tracking in response to sensory stimuli
Assessment Guidelines
-Administer adequate stimulation to ensure arousal is maximized
-Address factors affecting arousal (i.e., medication)
- Elicit behavioral responses through verbal instruction, not involving behaviors that frequently occur on a reflexive basis
-Incorporate commands following trials or behaviors that are within the capability of the patient
-Investigating a variety of different behavioral responses using a broad range of eliciting stimuli
-Conduct procedures in a distraction-free environment
-Reassess with systematic observation and reliable measurement strategies to validate the initial assessment
-Consider observations of family members, caregivers, and professional staff participating in daily care in designing assessment procedures
Ranchos Level 1
-no response, total assistance
-Complete absence of observable change in behavior when presented with visual, auditory, tactile, proprioceptive, vestibular, or painful stimuli
Ranchos Level 2
-Generalized Response: Total Assistance
-Demonstrates generalized reflex response to painful stimuli
-Responds to repeated auditory stimuli with increased or decreased activity
-Responds to external stimuli with physiological changes; generalized, gross body movement; and/or non-purposeful vocalization
-Responses noted above may be the same regardless of the type and location of stimulation
- Responses may be significantly delayed
Ranchos Level 3
-Localized Response: Total Assistance
-Demonstrates withdrawal or vocalization to painful stimuli
-Turns toward or away from auditory stimuli
-Blinks when strong light crosses the visual field
-Follows moving objects passed within the visual field
-Responds to discomfort by pulling tubes or restraints
-Responds inconsistently to simple commands
-Responses directly related to the type of stimulus
-May respond to some persons but not others
Sensory Stimulation
-A treatment of impaired consciousness
-Provide sensory input through a variety of modalities
-Systematic and organized stimulation
-To monitor changes, prevent sensory deprivation, facilitate recovery regarding arousal, promote neuroplasticity
Mild TBI definition
An acute brain injury resulting from mechanical energy to the head from external physical forces.
Operational criteria for clinical identification include: 1 or more of the following:
- confusion or disorientation
-loss of consciousness for 30 minutes or less
-post-traumatic amnesia for less than 24 hours
-and/or other transient neurological abnormalities such as focal signs, seizure, and intracranial lesion not requiring surgery
Recovery time from mild TBI
-Recovery for adults usually occurs within 14 days of the injury
-Recovery for children usually occurs within one month of the injury
Factors which impact recovery with MTBI
history of any of the following:
-sleep disorder
-learning disability
-migrane/ headaches
-females
-previous TBI
-lower socioeconomic status, education, cognition
-truama/psychosocial concerns
motivational interviewing
-Method of engaging the patient to explore areas of concern and identify functional goals
"Way to work with a patient rather than on a patient"
Key Principles:
-Express empathy
-Develop discrepancy
-Roll with resistance
-Support self-efficacy
OARS
Open ended
Affirmation
Reflection
Summary
Treatment of mTBI in acute phase
The purpose of the initial visit is to acknowledge symptoms, provide education, and track and facilitate the resolution of symptoms to assist the individual in returning to their pre-injury state.
What do the guidelines for treatment of persistent symptoms include
Treatment included:
-direct attention training (DAT)
metacognitive strategy instruction (MSI) to facilitate self-regulation of states of mind, academic tasks, and study skills
-training assistive technology for cognition (ATC) for use in school
-psychoeducational supports, which included symptom monitoring paired with goal setting and/or concussion education
Management of sports related concussion
1. Baseline testing
2. Acute (Sideline)/Post injury Assessment
3. Subacute and Chronic Recovery Assessment
Sports related concussion risk factors including age effects
-Developing brains are more susceptible to neurochemical and metabolic changes
-Axons are not as myelinated so more vulnerable to injury
-Less developed cervical and shoulder musculature resulting in a decreased ability to absorb mechanical energy
-High school athletes (ages 14- 18)were found to have prolonged cognitive recovery following concussion compared to college athletes
Second impact syndrome
repetitive head injury syndrome
- Second head injury before symptoms of an earlier injury have resolved
-Happens most often to those participating in sports or it could happen to those in combat
Chronic Traumatic Encephalopathy (CTE)
- Progressive, neurodegenerative condition that affects cognition and mental health due to repeated mTBIs
-Build-up of protein called tau
- Clinical symptoms- changes in mood(depression and anxiety) and behavior (aggression, paranoia, impulsivity) followed by memory loss and parkinsonism, and then further cognitive decline