Cardiovascular System
1/155
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
156 Terms
Pulmonary circuit
Right ventricle pumps deoxygenated blood through the pulmonary arteries to the lungs which oxygenate the blood.
Oxygenated blood is sent from the veins to the left atrium and ventricle.
This is a medium resistance and medium pressure circuit.
Systemic circuit
Left ventricle pumps oxygenated blood through the systemic arteries to capillary beds of organs.
These take in the oxygen and send deoxygenated blood to the right atrium and ventricle through systemic veins.
This is a high resistance and high pressure circuit, except the systemic veins which are low pressure and resistance.
Gut and liver in systemic circuit
The liver has a dual blood supply:
Oxygenated blood from the systemic arteries.
Hepatic portal system: Deoxygenated blood from the gut (contains nutrients)
Blood volume/distribution around the body (3)
Systemic: 84% (64% in veins, 13% in arteries, 7% in capillaries)
Pulmonary: 9%
Heart: 7%
Total blood volume and heart output
~5 litres
Heart output: 5 Litres/minute at rest (can be up to 4x more during exercise).
Outlet valve
Valve between the ventricle and artery that can open and close.
During the filling phase from the veins, the valve is closed to prevent arterial blood from returning to the pump.
During the ejection phase out the artery, the valve is pushed open by the blood forced out.
Inlet valve
Valve between the vein and ventricle that can open and close.
During the filling phase from the veins, it is open to allow blood to enter into the ventricle.
During the ejection phase out the artery, the valve is closed to prevent high-pressure blood in the pumping chamber from returning to the veins.
Atrium
Reservoir upstream of the pump which accumulates venous blood during the ejection phase.
The blood can then enter the ventricle quickly during the filling phase.
Auricle
Extension of the atrium which increases its capacity.
Why are the inlet and outlet of the heart pump close together?
Allows more of the walls to change in size, providing more pumping strength.
Interventricular sulcus
Sulcus between the left and right ventricle of the heart.
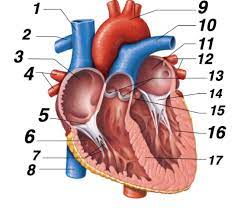
What is 1 called?
Superior vena cava (SVC)
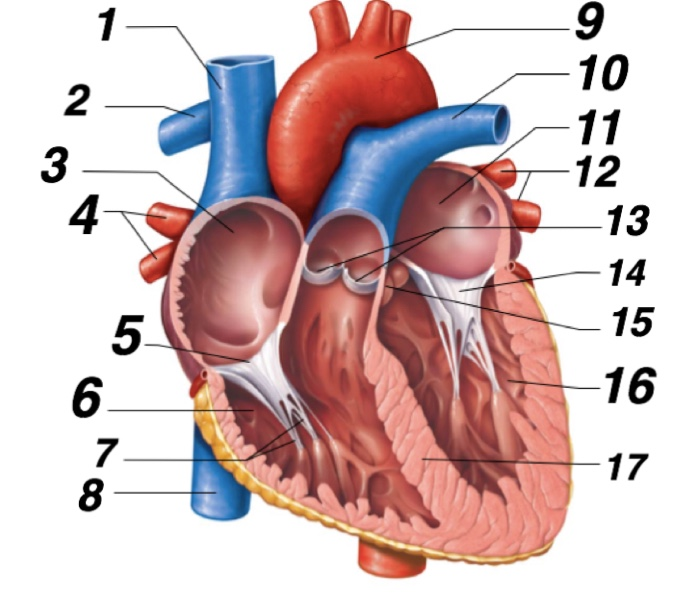
What is 2 called?
Right pulmonary artery
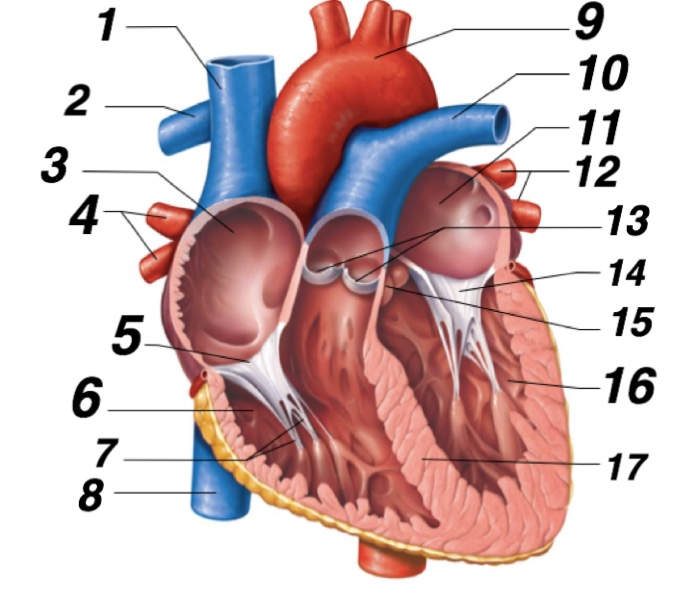
What is 3 called?
Right atrium
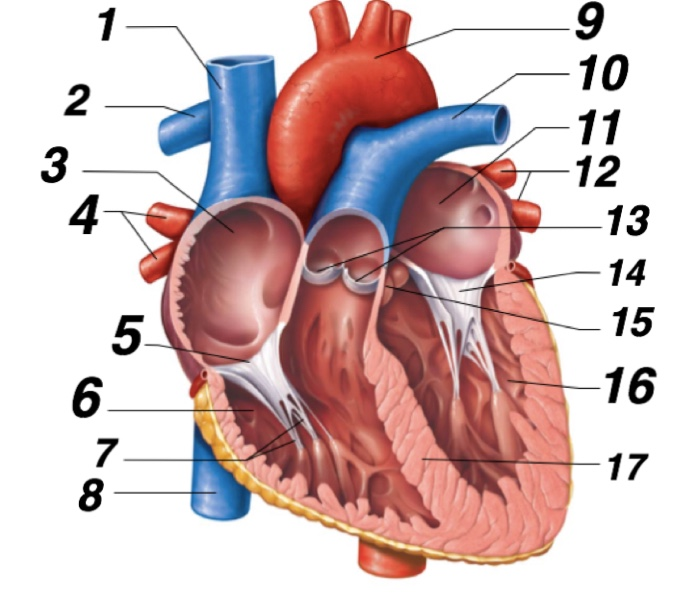
What is 6?
Right ventricle
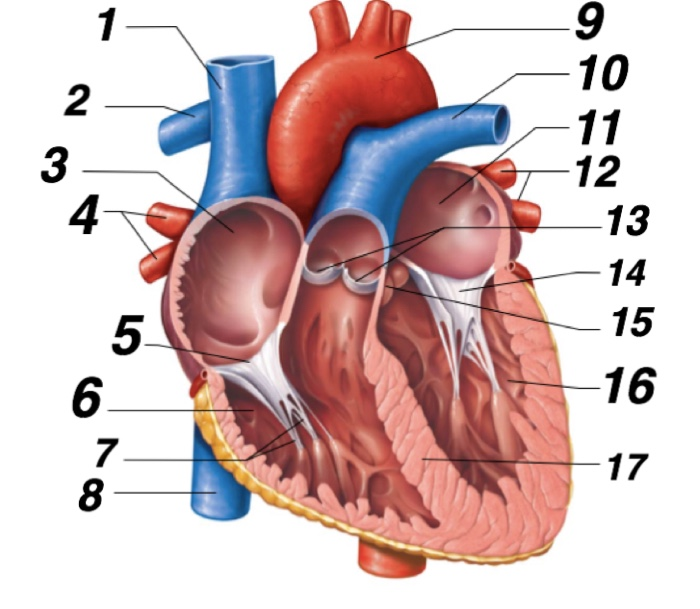
What is 7?
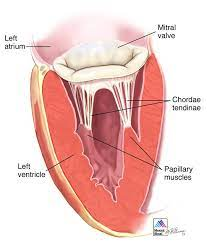
Chordae tendineae
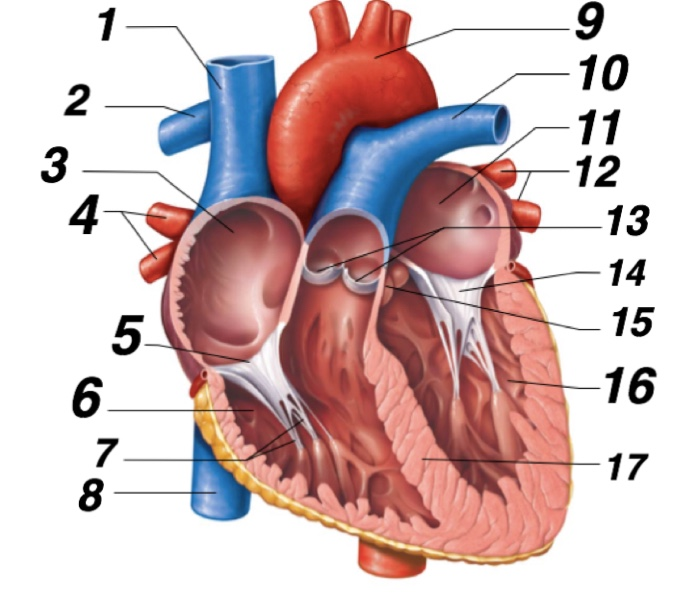
What is 8?
Inferior vena cava
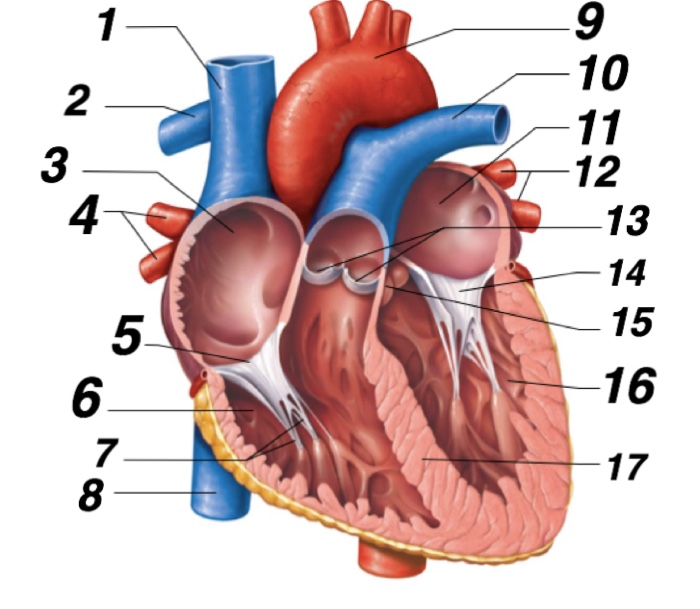
What is 9?
Aorta
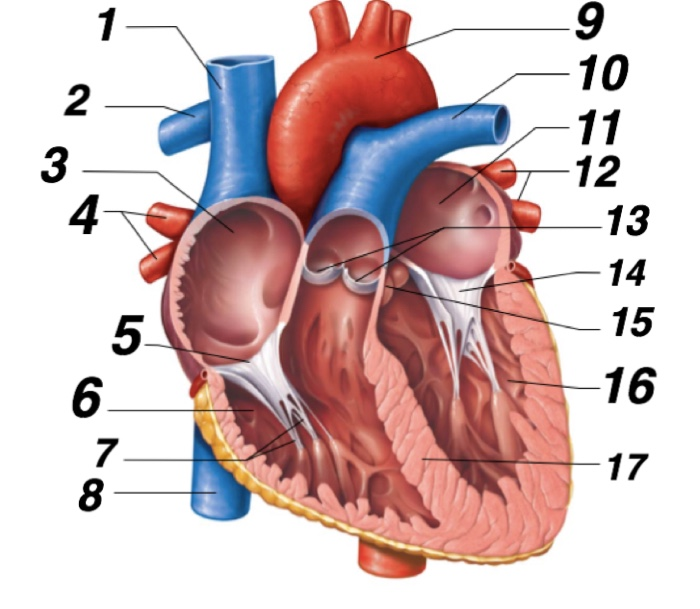
What is 10?
Left pulmonary artery
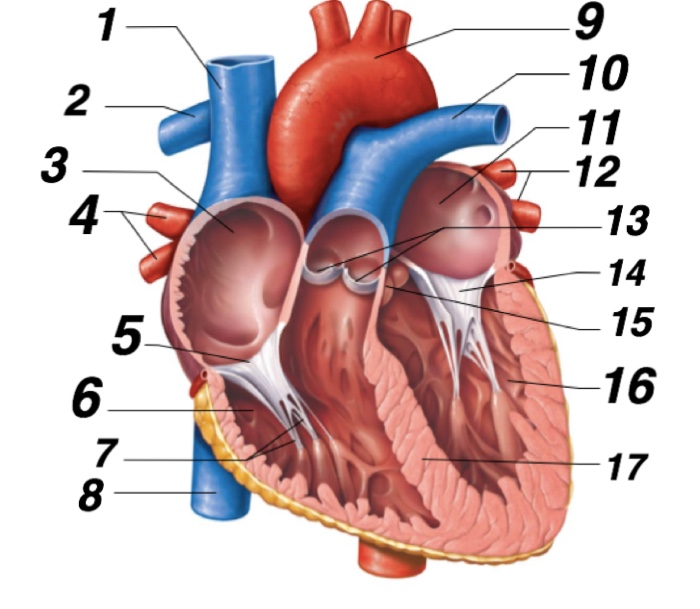
What is 11?
Left atrium
What is 16?
Left ventricle
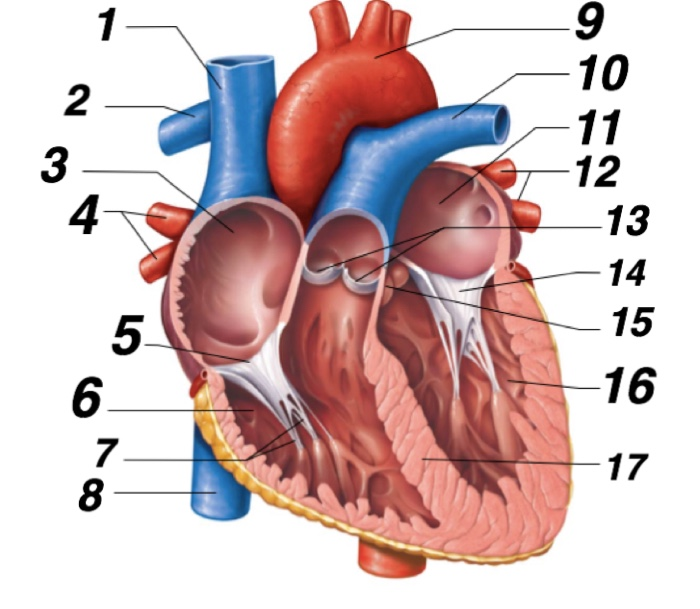
What is C?
Pulmonary trunk
Pulmonary circuit vs systemic circuit direction in body:
Pulmonary goes more horizontal (lung ←> heart)
Systemic goes more horizontal (heart to brain, heart to body)
Peak pressure of right ventricle vs left ventricle
Right: 27mmHg
Left: 120mHg
Peak pressure of right atrium vs left atrium
Right: 5mmHg
Left: 8mmHg
Size comparison of left ventricle, right ventricle, right atrium.
LV>RV>RA
Since the left ventricle works harder to pump, so the muscle has built up more.
Tricuspid valve description and function
3 valve flaps between the right ventricle and right atrium (aka. right inlet valve)
Open to let blood flow from right atrium to right ventricle.
Mitral/Bicuspid valve description and function
2 valve flaps between the left ventricle and left atrium (aka. left inlet valve)
Open to let blood flow from left atrium to left ventricle.
Pulmonary valve
Right outlet valve.
Pushed open by blood pressure to let blood flow from the right ventricle to right aorta.
Aortic valve
Left outlet valve.
Pushed open by blood pressure to let blood flow from the left ventricle to left aorta.
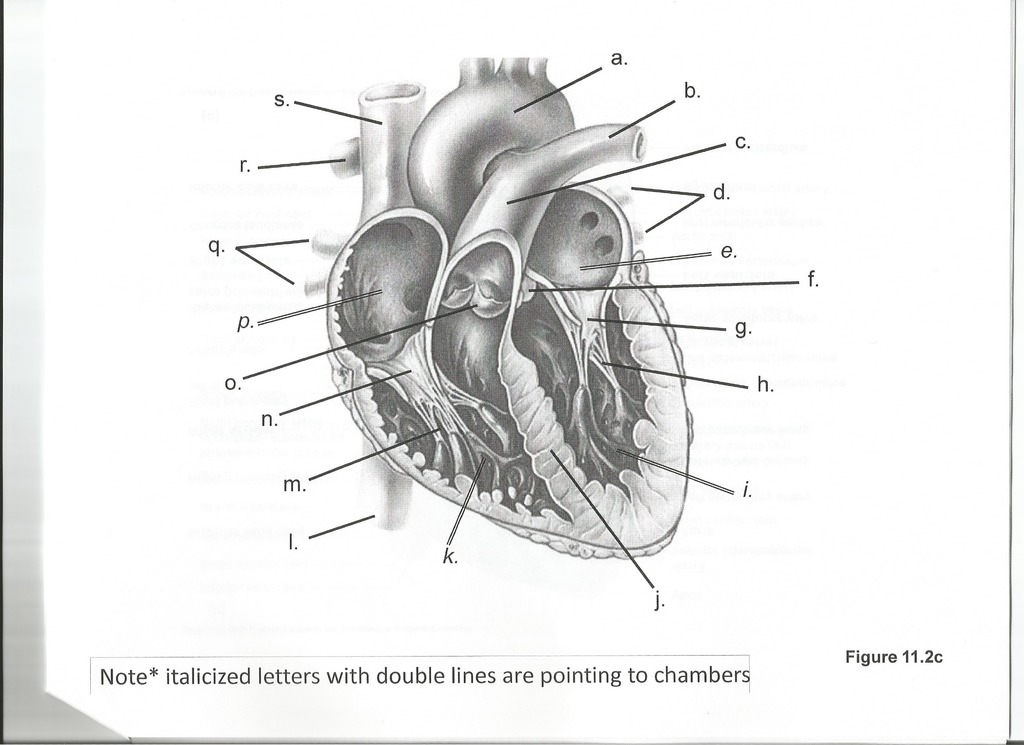
Chordae tendineae
Strong fibrous connections between the valve leaflets and papillary muscles in the heart.
Prevent the leaflet from swinging back into cavity.
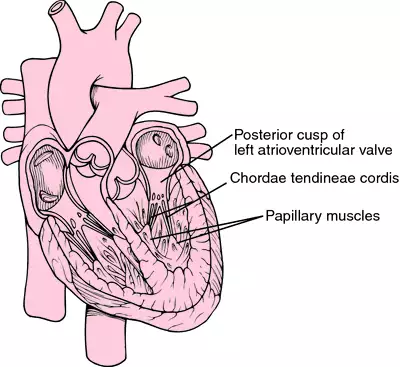
Papillary muscle
Prevent the valves from opening when the ventricles contract.
Left ventricle shape
Hollow cone with thick muscular walls.
Forms the core of the heart.
Right ventricle shape
Pocket shaped - lumen is a crescent shape.
Sits on the side of the left ventricle.
Left vs Right ventricle: Wall thickness ratio
Left: Right
~3:1
Left vs Right ventricle: Peak pressure ratio
Left: Right
~5:1
Left vs Right ventricle: Wall thickness vs peak pressure
Left ventricle wall is only 3 x thicker than right ventricle wall, yet generates 5 x the pressure.
Cusps of the outlet valves (pulmonary & aortic)
Both outlet valves have 3 cusps described by their semilunar shape.
Cusps are shaped like a small pocket.
Lack cords.
Cusps of the inlet valves (tricuspid & mitral)
Both outlet valves have 3 cusps described by their semilunar shape.
Cusps are flat flaps.
Free edges are restrained by cords.
Mechanism of outlet valves - Blood is pushing out of the ventricle:
Ventricular pressure>aortic pressure, so blood is pushing out.
The cusps are passively pushed to the sides by the blood pressure, allowing free blood flow out into the aorta.
Mechanism of outlet valves - Blood is coming into the ventricle from the atrium:
Ventricular pressure<aortic pressure, so blood pushes back from the aorta.
This pressure forces the free edges of the cusps together in the middle, preventing blood flow.
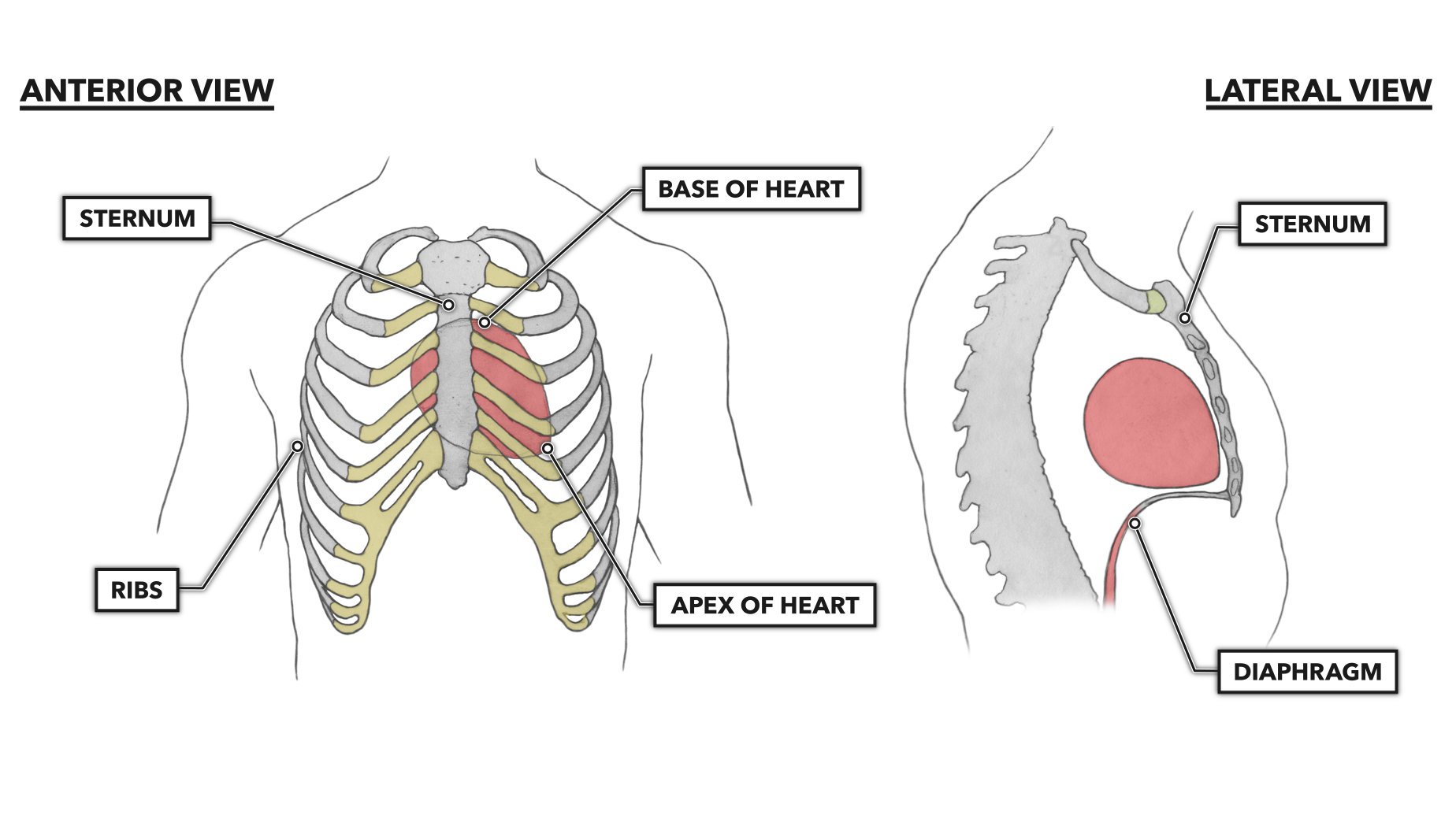
General orientation of the heart in the body
~1/3 of the heart lies to the right of the midline of the body.
~2/3 of the heart lies to the left of the midline of the body.
Apex of the heart
Points inferiorly, anteriorly, and to the left.
(down, forwards, and left)
Heart: Right border
Formed mainly by the right atrium
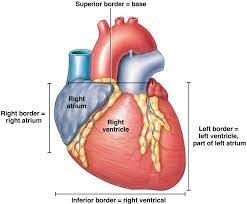
Heart: Left border
Formed mainly by the left ventricle (and partially left atrium/auricle)
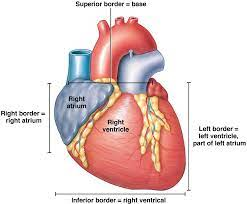
Heart: Inferior border
Formed mainly by the right ventricle
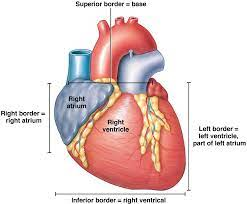
Heart: Superior border
Formed mainly by the blood vessels
Base of the heart.
Thoracic width: Healthy heart ratio
Thoracic width: Healthy heart
2: <1
(i.e. heart should be less than 50% of the thoracic width)
Pericardium constituents (inner to outer)
Visceral pericardium
Pericardial space (serous fluid)
Parietal pericardium
Fibrous pericardium
Visceral pericardium description
Made of a single layer of squamous mesothelial cells.
Adheres to the heart.
Forms the outer surface of the heart (epicardium)
In reference to the heart wall, it’s called: Epicardium
In reference to the pericardia, it’s called: Visceral pericardium
Pericardial space description
Very thin space between the visceral and parietal pericardia.
Contains a very small amount of serous fluid, which allows the pericardia to slide without friction as the heart beats.
Parietal pericardium description
Made of a single layer of squamous mesothelial cells.
Lines the fibrous pericardium.
Fibrous pericardium description
Thick fibrous sac made of collagen.
Supports the parietal pericardium.
Layers of the heart (inner to outer)
Inside:
Inside ventricle (blood)
Heart wall:
Endocardium
Myocardium (cardiac muscle)
Epicardium*
Pericardium:
Visceral pericardium*
Pericardial space (serous fluid)
Parietal pericardium
Fibrous pericardium
Outside:
Outside pericardial sac
**Same thing, different name depending on part of the structure being referenced.
Cardiac tamponade
When too much fluid accumulates in the pericardial space.
Compresses the heart, decreases cardiac output.
Leads to myocardial infarction (heart cell death).
Leads to death if pressure isn’t relieved to allow heart to beat properly.
Fibrous ‘skeleton’ of the heart
Made of touch elastic tissue.
Said to surround each of the valves (tricuspid, pulmonary, mitral, aortic).
In reality, surrounds mitral and aortic valves (left), while tricuspid ring is incomplete and pulmonary ring is absent.
Fatty connective tissue is still present in areas with incomplete fibrous skeleton.
Sinoatrial node (SA node)
‘Natural pacemaker’
Cluster of cardiac myocytes able to generate spontaneous action potentials to set the rhythm of the heart.
Conducts action potentials to the atrial muscle
Atrioventricular node (AV node)
Able to slowly depolarise/repolarise action potentials.
Conducts action potentials from the atria to the ventricles with a delay.
Atrioventricular bundle (of His)
Branch of fibers (nerve cells) that extends from the AV node.
Conducts action potentials from the AV node to the Purkinje fibres.
Pathway of action potentials in the heart
Sinoatrial node conducts it slowly (0.5m/s) to the atrial muscle. Causes even atrial contraction.
Atrioventricular node conducts it very slowly (0.05m/s) from the atria to the ventricle. Results in a 100ms delay between atrial and ventricular contraction.
Atrioventricular bundle conducts it fast (5m/sec) to the Purkinje fibres. Causes uniform rapid ventricular contraction (systole).
Purpose of delay between atrial and ventricular contraction caused by atrioventricular node:
Allows both atrial and ventricular contraction to occur.
Due to the strength of ventricular contraction, it would override atrial contraction if they occurred at the same time.
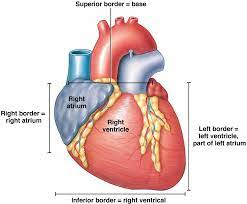
Cardiac cycle steps/stages
Ventricular filling
Atrial contraction
Isovolumetric ventricular contraction (systole)
Ventricular ejection
Isovolumetric ventricular relaxation
Then back to ventricular filling ⤴
Ventricular filling
Ventricular pressure < Atrial pressure
So, blood moves down the pressure difference into the ventricle by pushing open the mitral valve (passively).
Ventricle fills to ~80% of its capacity.
Atrial contraction
Left atrium contracts to complete the ventricle filling.
Causes a small rise in arterial pressure.
Small due to atrial muscle layer being thin.
And, no valves preventing backflow from the atrium to the veins.
Isovolumetric ventricular contraction (systole)
After the 100ms delay (caused by the AV node), the ventricle begins contracting.
So, blood lifts backwards towards the atrium, pushing the mitral valve closed (This is the first heart sound).
Even as ventricular pressure increases: Atrial pressure > Ventricular pressure > Arterial pressure.
Meaning, both the inlet and outlet valves remain closed, isolating the ventricle from the rest of circulation (for ~0.05s (very short)).
Ventricular ejection
Systole (isovolumetric ventricular contraction) continues, but now Ventricular pressure > Aortic pressure.
Blood moving down the pressure gradient pushes open the aortic valve cusps (passively), allowing blood to move out of the ventricle.
Since blood is ejected into the aorta faster than it can run off into the distributing arteries, ventricle and aorta pressure continues to rise.
Later in this phase, rate of ejection < rate of run-off, so aortic and ventricular pressures level off, then decrease.
Isovolumetric ventricular relaxation
The ventricle relaxes, so ventricular pressure drops suddenly.
Blood flow reversing in the aorta trying to reenter the ventricle pushes the aortic valve closed (second heart sound).
Even as ventricular pressure decreases, Atrial pressure > Ventricular pressure > Arterial pressure.
Meaning, both the inlet and outlet valves are closed again, isolating the ventricle from the rest of circulation again (for ~0.05s (very short)).
When this phase is completed, the heart re-enters the stage of ventricular filling.
Tunica meaning
An enclosing or covering membrane or tissue
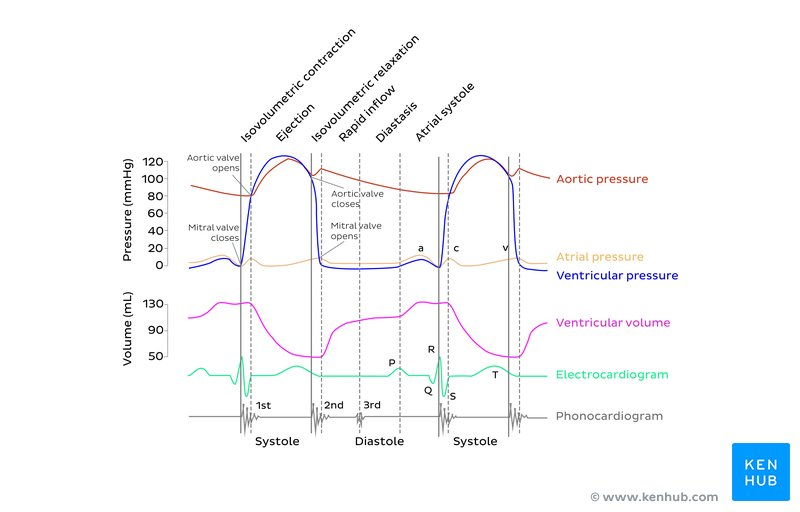
Blood vessel types (6): From heart to cells, back to heart:
Elastic arteries
Muscular arteries
Arterioles
Capillaries
Venules
Veins
Elastic artery
Size
Structure
Function
~Human finger width (largest artery in the human body)
Closest to the heart; Many sheets of elastin in the middle tunic.
Overall, they smooth the pulsatile flow of blood leaving the ventricles (controls blood flow; can protect delicate vessels).
During systole (contraction), they expand to store the bolus of blood leaving the ventricle
During diastole, they push blood out into the arterial tree via elastic recoil.
Muscular arteries
Size
Structure
Layers
Function
Rate
Ranges from the width of a pin to a pencil.
Many layers of circular smooth muscle wrapped around the vessel in the middle tunic.
Similar structure to veins, but have much more muscle and connective tissue; Consists of 3 layers (in to out):
Inner ‘Tunica Interna/Intima’.
Middle ‘Tunica Media’ with smooth muscle under control of the autonomic nervous system.
Outer ‘Tunica Externa'/Adventitia’ which attaches to other organs.
Distributes blood around the body at high pressure (lungs at medium pressure).
Rate of blood flow is proportionate to the fourth power of the radius, so the rate is adjusted by varying the vessel’s radius using smooth muscle (Flow = k * Radius⁴). Small change in radius = Big change in rate.
Arteriole
Size
Structure
Function
~Thickness of one human hair.
Lining of endothelial cells surrounded by 1-3 layers of circular smooth muscle. Have the thickest muscular wall relative to their size than any other blood vessel.
Control blood flow into capillary beds.
Greatest pressure drop, and greatest resistance to flow, occurs here.
Degree of constriction of arterioles throughout the body determines total peripheral resistance, which itself affects mean arterial blood pressure.
Capillary
Size
Structure
Function
Rate of blood flow
~Size of one RBC (~9 microns).
Wall made of a single layer of endothelial cells (leaky), with an external basement membrane. No smooth muscle (diameter is fixed) and no connective tissue is present.
Plasma leaks through the walls into the tissue fluid, and then exchanges gases, nutrients, and waste with tissue cells. Most of the lost plasma is immediately recovered due to an osmotic gradient.
Slow blood flow in capillaries allows time for this exchange to occur.
Venule
Size
Structure
Function
Smallest vein; Larger than a capillary (~10-30 microns)
Layer of endothelial cells surrounded by a small amount of connective tissue. Some larger venules have a single smooth muscle layer.
Drains deoxygenated blood from capillary beds at low pressure; The site where WBCs leave the blood circulation to attack bacteria in the adjacent tissue (e.g. neutrophil squeezes between endothelial cells to exit venule and attack area with infection/inflammation).
Vein
Size
Structure
Valves
Function
Ranges from the width of a ~pin to a ~pencil.
Thin-walled. Similar structure to muscular arteries, but have much less muscle and connective tissue; Consists of 3 layers (in to out):
Inner ‘Tunica Interna/Intima’.
Middle ‘Tunica Media’ with smooth muscle under control of the autonomic nervous system.
Outer ‘Tunica Externa'/Adventitia’ which attaches to other organs.
Larger veins (especially in limbs) have bicuspid valves preventing backflow and pooling of blood in feet, hands. Must be active as the valves are leaky.
Returning blood to heart; Blood reservoir:
As muscles around the veins contract and relax when moving, they act as a venous pump draining deoxygenated blood back to the right atria** at low pressure.
A small change in venous BP causes a big change in venous volume, so ~64% of blood volume occurs in systemic veins and venules (vs. ~13% in systemic arteries and arterioles).
**Except portal veins, which drain blood to another capillary bed
Coronary Arteries
Location/Structure
Function
Muscular arteries that arise from the aorta, just downstream of the aortic valve. Branch out around the outside of the whole heart, giving up arterioles and capillaries into the heart.
Supply the muscle of the heart (myocardium).
Cardiac veins
Drain deoxygenated blood from the myocardium and return it to the right atrium.
Of NO clinical importance.
Atherosclerosis description and effect on Coronary artery:
Description:
Disease that causes the buildup of fat (atheroma) in arteries, narrowing the artery.
Coronary artery:
If it narrows a Coronary artery to ~20% of its normal cross section, it significantly obstructs blood flow to the myocardium it supplies.
During exercise, this myocardium experiences ischemia (low oxygen), leading to angina (chest pain).
Severe ischemia results in infarction (death) of that local myocardium area*
*Sometimes, anastomoses (artery-to-artery junctions) between small penetrating branches of the main coronary arteries widen slowly so that an ischemic area of muscle can be supplied by a distant artery.
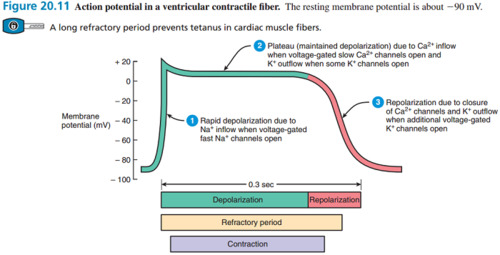
Action Potential in Ventricular Contractile Fibre: Steps (3)
Rapid depolarisation
Plateau (maintained depolarisation)
Repolarisation
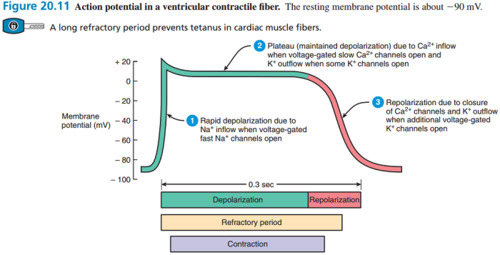
Rapid depolarisation in Action Potential of Ventricular Contractile Fibre
Initiated by specialised cells in the SA node (lying close to the great veins entry in right atrium).
Voltage-gated Na⁺ channels open leading to Na⁺ inflow, thus increasing positive ion concentration.
A wave of depolarisation is then conducted throughout the myocardium; The membrane potential between successive action potentials shows a progressive depolarisation (the Pacemaker).
When threshold is reached, an action potential is triggered to initiate a heartbeat.
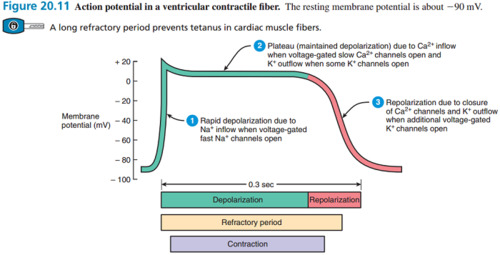
Plateau (maintained depolarisation) in Action Potential of Ventricular Contractile Fibre
Slow voltage-gated Ca²⁺ channels open, leading to Ca²⁺ inflow
Some K⁺ channels open leading to some K⁺ outflow.
Therefore, ion concentration within the fibre stays the same.
*Both the slowness of the calcium channels and the gradual opening of the potassium channels leads to the longer-lasting depolarisation.
Because the muscle is refractory during and after the action potential passage, the long plateau phase ensures the unidirectional depolarisation of the myocardium.
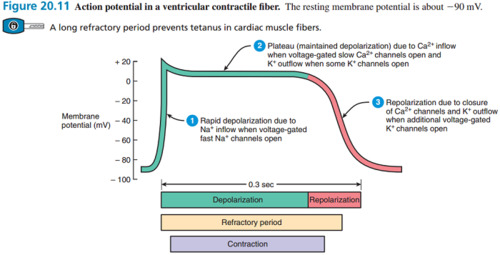
Repolarisation in Action Potential of Ventricular Contractile Fibre
Ca²⁺ channels close.
Voltage-gated K⁺ channels open, leading to additional K⁺ outflow.
This causes the positive ion concentration within the fibre to decrease, thus repolarising it.
Sections of an ElectroCardioGram (ECG):
P wave
PQ interval
QRS complex
ST segment
T wave
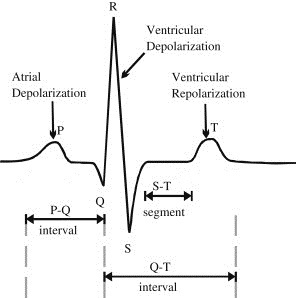
P wave:
ECG correlation with atrial and ventricular systole (contraction)
Depolarisation of atrial contractile fibres at the SA node produces the small P wave.
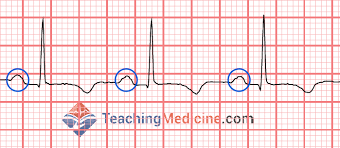
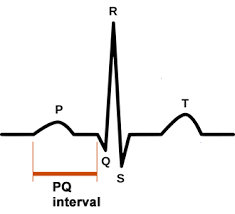
PQ interval:
ECG correlation with atrial and ventricular systole (contraction)
Flat interval showing how fast the action potential is transmitted through the AV node (atrioventricular) from the atria to the ventricles.
QRS complex:
ECG correlation with atrial and ventricular systole (contraction)
Main part of the graph.
Produced by the depolarisation of ventricular contractile fibres.
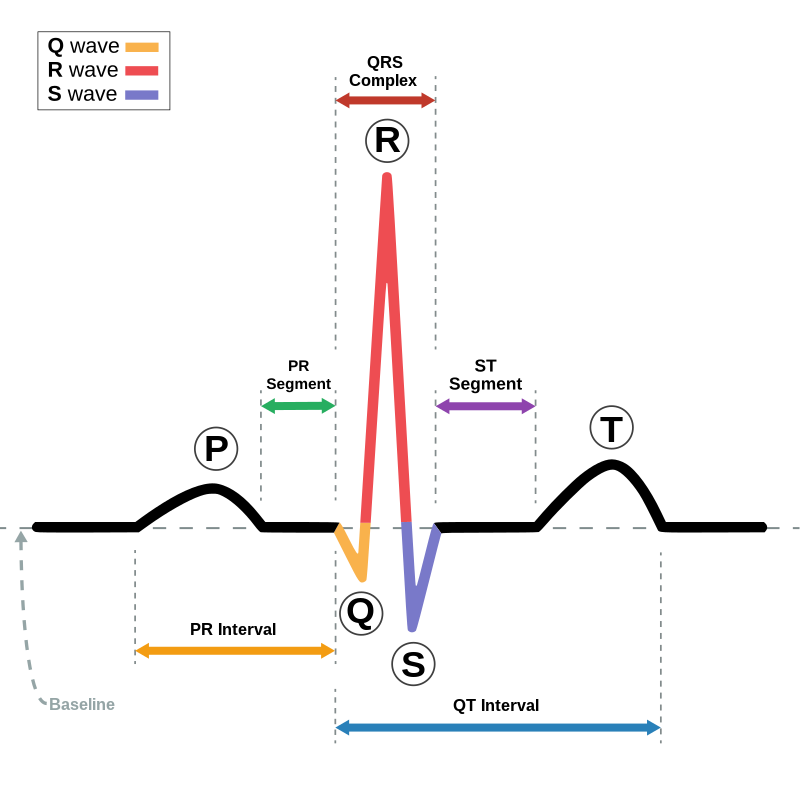
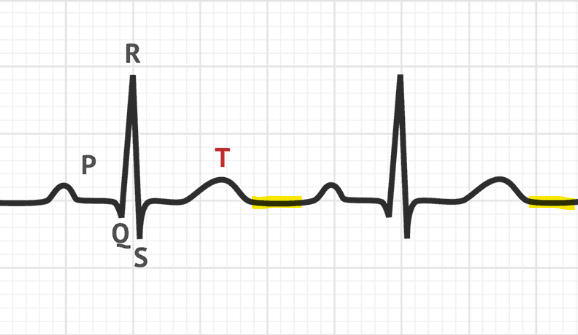
ST segment:
ECG correlation with atrial and ventricular systole (contraction)
Plateau (maintained depolarisation) that occurs during ventricular systole (contraction).
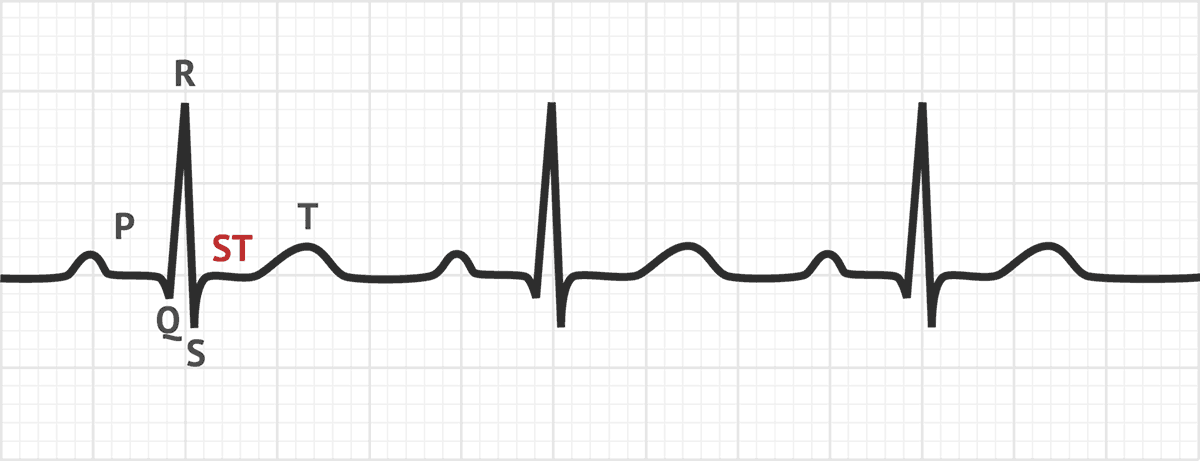
T wave:
ECG correlation with atrial and ventricular systole (contraction)
Produced by repolarisation of ventricular contractile fibres.

After T wave:
ECG correlation with atrial and ventricular systole (contraction)
Flat interval showing ventricular diastole (relaxation).
Nervous system control of the heart - Locations.
Input: From higher brain centres and sensory receptors (to CV centre in medulla oblongata)
Output: (From CV centre in medulla oblongata) To Effectors in heart.
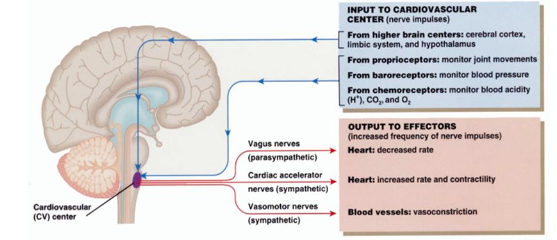
INPUT: Nervous system control of the heart:
From higher brain centres (cerebral cortex, limbic system, and hypothalamus).
From sensory receptors (Proprioceptors, baroreceptors, chemoreceptors)
To CV centre in medulla oblogata
Higher brain centre input: Heart nervous control:
Cerebral cortex, limbic system, hypothalamus; Inputs to CV centre in medulla oblongata.
Thinking can influence heart rate (eg. thinking about exercising can raise heart rate).
Proprioceptor input: Heart nervous control.
Description
Function
Sensory receptor; Inputs to the CV centre in medulla oblongata.
Monitors joint movements
Baroreceptor input: Heart nervous control.
Description
Function
Sensory receptor; Inputs to the CV centre in medulla oblongata.
Monitors blood pressure.
Baroreceptor reflexes: Negative feedback regulation of blood pressure
Stimulus (eg. haemorrhage (extreme example), sudden standing up) changes (typically decreases) blood pressure, thus disrupting homeostasis.
The decrease in blood pressure causes the vessels to stretch less, decreasing the rate of nerve impulses.
Baroreceptors in the carotid sinus and aortic arch register this reduction in nerve impulses.
The baroreceptors therefore input into the CV centre and adrenal medulla.
These output onto the effectors (heart and blood vessels).
CV centre causes increased sympathetic, decreased parasympathetic stimulation.
Adrenal medulla causes increased (nor)epinephrine secretion.
Effectors give a response.
Heart increases HR and SV → increases CO.
Blood vessels constrict → increases systemic vascular resistance (SVR).
Blood pressure increases.
This feeds back into the negative feedback loop, stopping the effectors from continuing (preventing overcompensation).
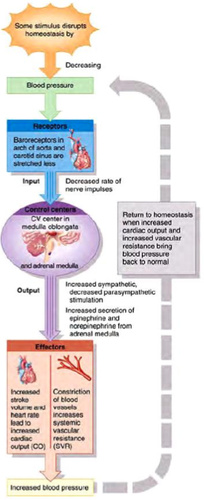
Systemic vascular resistance (SVR)
Resistance to blood flow by all systemic vessels.
Chemoreceptor input: Heart nervous control.
Description
Function
Sensory receptor; Inputs to the CV centre in the medulla oblongata.
Monitors blood chemistry (acidity (H⁺); CO₂; O₂)
OUTPUT: Nervous system control of the heart:
From CV centre in the medulla oblongata to effectors:
To vagus nerves (parasympathetic).
To cardiac accelerator nerves (sympathetic).
To vasomotor nerves (sympathetic).
Vagus nerve output: Heart nervous control.
Description
Function
Parasympathetic Effector ; Outputs from CV centre in the medulla oblongata.
Decreased heart rate due to:
Decreased rate of spontaneous depolarisation in SA node (and AV node)*
*Dominates SA node pace-making at REST
Cardiac accelerator nerve output: Heart nervous control.
Description
Function
Sympathetic Effector; Outputs from CV centre in the medulla oblongata.
Increases heart rate due to:
Increased rate of spontaneous depolarisation in SA node (and AV node).
Increased contractility of atria and ventricles increasing stroke volume.