Pathopharm-Burns, eye and ear
1/68
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
69 Terms
Burns are..
Categorized according to the source that produces injury, such as thermal, chemical, electrical, or radiation energy.
Factors that determine the severity; Burn depth, percentage of body surface are injured, age of patient, extent of associated systemic involvement.
Smoking and open flame are the leading causes of burn injury for older adults.
Scalding is the leading cause of burn injury for children.
Both infants and older adults are at the greatest risk for burn injury.
Burn classification
Depth- superficial, superficial partial thickness, deep partial thickness, full thickness.
Degree from 1 to 6- by tissue layer
Superficial burn Depth
Only damage epidermis. Erythematous, hypersensitive, no blister formation.
Appearance similar to a sunburn
Burn typically heal within 3-5 days and without permanent scarring.
Superficial partial thickness
Damage to epidermis and superfical portion of dermis is damaged minimally; epidermal appendages remain intact.
Portion of dermis may contain sweat, sebaceous glands, hair follicles, sensory nerves, capillary network.
Moist and weepy, pink or red, blisters, blanching hypersensitive.
Burns typically heal within 14 to 21 days, depending depth with minimal to no scarring.
Deep partial thickness
Damage is deep in dermis; epidermis destroyed; underlying dermis damaged; some epidermal appendages remain intact.
Pale; decreased moisture; blanching absent or prolonged; intact sensation to deep pressure but not to pin prink.
Wound is usually white or yellow, dry, and nonblanchable.
Prolonged healing, often more than 21 days; may require skin graft to achieve complete healing with better functional outcome.
Full thickness burn
Damage to epidermis and dermis and subcutaneous tissue. Can also extend through epidermal appendages, fat, muscle, bone causing destruction.
Usually white or black/brown, dry and leathery, and nonblanchable; may note thrombosed vessels or charring; insensate; may have limited extremity movement.
Requires skin grafting and may require amputation if greater depth.
1st degree burn
Damage to the epidermis, like a sunburn
2nd degree burn
Damage to epidermis and dermis
3rd degree burn
Damage to epidermis and dermis that will require skin grafting.
4th degree burn
Same as third degree but extending into fat layer
5th degree burn
Same as third degree but extending into muscle layer
6th degree burn
Same as third degree but extending to the bone.
Thermal burns
Exposure to fire, hot objects, scalding liquids, hot grease, or steam.
Produce damage to and underlying tissues after exposure to temp greater than 111.2 F.
Can range from superficial, affecting only the epidermis, to full thickness, which injures subdermal tissues.
Scald burns occur after exposure to hot liquids, grease, or steam and cause tissue necrosis and cellular death within sec after exposure to temp 158 F
Smoke inhalation
Burns from breathing noxious chemicals or hot air. Damage to respiratory tract. Major mortality predictor in burn victims.
3 types= Upper airway injury, Lower airway injury, and metabolic asphyxiation.
Chemical burns
Generally occurs after industrial accident or ingesting harsh household chemicals, including strong acids, alkalis, and corrosive materials.
Induce protein coagulation of tissues(protein breakdown) as chemical energy is converted into thermal energy. Produces a characteristic gray coloring of skin.
Response is proportional to type, quantity, and concentration of chemical; duration of contract; and degree of penetration of tissues.
Electrical burns
Electrical current generates heat when it meets resistance in body tissues and produces damage as current passes through the body, possibly leaving entrance and exit wounds.
Path of electrical energy commonly causes internal organ injury. Degree of injury depends on amount of voltage, length of contract, and pathway of current.
Nerves and muscles produce less resistance and suffer greater damage than tendons, fat, and bones.
Pathway of current across heart is associated with highest mortality as alternating current of electrical shock disrupts normal cardiac conduction, can produce cardiac arrest.
Three zones of injury
Zone of Coagulation= deepest point of injury, most irreversible damage.
Zone of Stasis= decreased tissue perfusion, potential reversible damage.
Zone of hypermia= outer zone, reddened due to vasodilation, and minimal tissue damage.
Zone of hypermia
outer zone, reddened due to vasodilation, and minimal tissue damage.
Zone of Stasis
decreased tissue perfusion, potential reversible damage.
Zone of Coagulation
deepest point of injury, most irreversible damage.
Labs to monitor in burn injury
CBC, Electrolyte level, urinalysis, arterial blood gas, carboxyhemoglobin level is burn injury occurred is closed space and inhalation injury is suspected.
Myoglobinuria or dark brown urine, signals development of tubular necrosis. Breakdown of plasma proteins and dehydration indicated through spilling protein in urine.
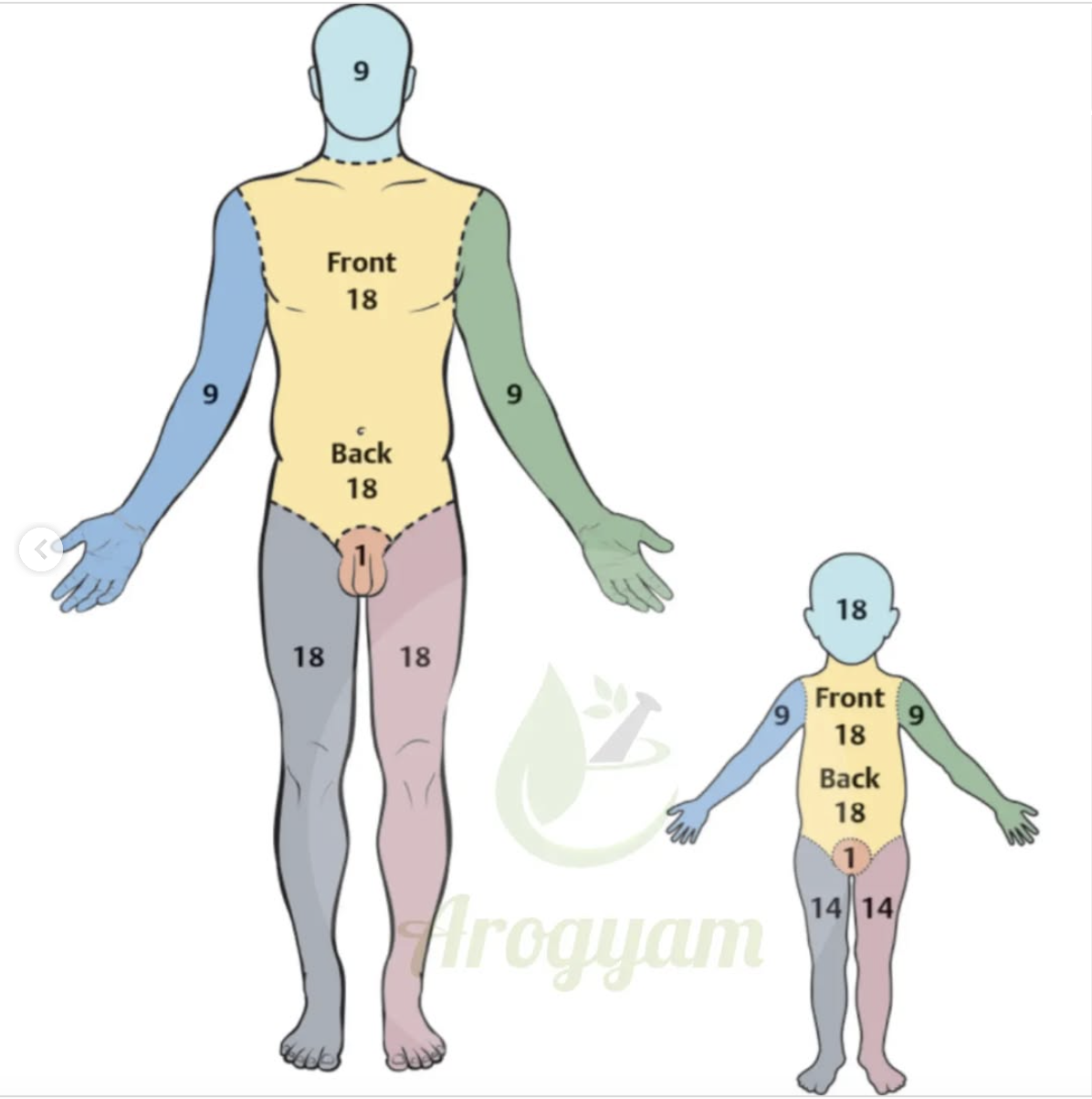
Rules of nines
Rapid method used during prehospital and emergent phase of care. Body divided into regions that present 9% or multiples of nine, with exception of perineum, which is 1% of BSA.
Face and back of head are 4.5% so entire head 9%.
Anterior and posterior portion of arm 9% and total for each leg is 18%. Patient’s total area of burn is estimated by adding percentage of surface area burned.
Lund and Browder method
More accurate estimation of affected body surface. It divides the body into smaller sections of TBSA and evaluates the percentages of these areas.
Patients total area of burn is estimated by adding the percentage of surface area burned.
Acute phase
Begins 48 to 72 hours after burn injury includes start of diuresis (loss of water from body) and ends with closure of burn wound.
Continued assessment of respiratory and circulatory status related to edema, fluid shifts, nutritional support, infection prevention, and burn wound care are priorities during this phase.
Hydrotherapy, excision and early skin grafting (surgical implantation of new skin) of full-thickness wounds are performed as soon as possible after injury.
Enteral (tube feedings) or total parenteral nutrition feedings will be initiated as necessary to meet caloric needs for healing and hypermetabolic state of patient with burns.
Pain management continues to be priority in plan of care for patient with burns, especially before procedures such as dressing changes and wound debridement.
Rehabilitation phase
May extend for years after injury and actually begins during the emergent phase with the application of splints and initiation of physical therapy.
Active and passive range of motion exercises are initiated as soon as possible to prevent development of contractures
Scar tissue formation can be modified with pressure dressings, such as Ace wraps over burn dressing, especially when patients are ambulating
As burn wounds are grafted, specialized tubular support bandages are applied to supply an equal amount of pressure to wounds to prevent or decrease amount of scar formation.
Infection and Sepsis
Infection is the most common complication after burn injury, causing 60% of burn victims.
After burn injury, major barrier to environmental pathogens, the skin, is lost.
There is also immunosuppression with deficient T cells and macrophage-mediated defenses.
Because circulation is diminished in burn region, there is a deficient number of white blood cells reaching the area of injury.
Sepsis is an extensive infection in bloodstream. Several criteria are used to diagnose sepsis.
Compartment syndrome
Full-thickness circumferential and near-circumferential skin burns result in formation of tough, inelastic, dead, burned tissue called eschar.
Eschar cause burn-induced __, which is bulidup of pressure within an area of body so restrictive that it suppresses circulation to region.
Eschar around the torso can cause chest wall restriction and hinder ventilation. Treatment consists of surgical escharotomy or fasciotomy, which is excision of restrictive eschar tissue.
Acute respiratory distress syndrome
Leading cause of death in severe burn injuries.
Can occur when there is large area of burn injury, direct lung injury, inhalation injury or sepsis. The risk of ARDS increases when the burn is greater than 40% TBSA or full-thickness burn is greater than 20%.
Contractures
Deep dermal and full-thickness burns with formation of fibrotic tissue that causes scarring.
Epithelial replacement is not possible if skin is burned below a certain level called stratum reticulare.
_ often form around joints, which pull the two bones close together so the joint cannot fully open.
After healing is complete, surgical reduction of the fibrous tissue and surgical reconstruction using skin grafts can reverse some _.
Hypertrophic scarring
Also called keloids, can occur as burns heal in some patients.
This growth of skin forms hyperemic, raised areas of firm skin.
Compression dressing and garments can be worn to prevent the development of _.
Glaucoma Clinical presentations
Patient history- age, use of lenses, family history, anticholinergic meds.
Patient complaints= eye pain, eye redness, halos around lights, vision loss.
Fundoscopic exam is necessary or central vision.
S/S= Rapid in PACG, and Progressive in POAG
What is tonometry?
a medical test used to measure the pressure inside the eye, known as intraocular pressure (IOP). It is an important part of an eye exam and is used to detect and monitor conditions that affect eye pressure, such as glaucoma
What is the cause of Glaucoma?
Elevated IOP
Silent thief of sight- Gradual progession, increased pressure on optic nerve= may result in blindness.
Risk factors= age greater than 40 years, ethnicity, history of migraine headaches, and cardiovascular disease.
What is Age-related macular degeneration?
Macula- area of retina providing central vision. Can deteriorate leading to blind spot and loss of vision.
-Wet and Dry, both types have failure to remove cellular debris from retina.
Drusen deposits= appear as yellow-white accumulation in macula.
Diagnosis- Amsler grid to measure central vision.
Treatment= antioxidant consumption, low fat diet, smoking cessation, wrap-around sunglasses.
Amsler grid
test used to detect early signs of vision problems, particularly those affecting the central part of the retina (macula), such as macular degeneration.
macular degeneration, the lines may appear wavy or curved, or you may see a blank or dark area in the middle of the grid
Age-related macular degeneration causes
The exact causes of AMD are not fully understood, but several factors are believed to contribute to its development.
Combination of genes and other factors, including smoking, obesity and diet. The condition develops as the eye ages. Dry macular degeneration affects the macula.
Age-related macular degeneration wet
10%; exudative; more severe
Age-related macular degeneration dry
90%; nonexudative
What is Papilledema?
Increase ICP causes swelling of optic nerve.- Sign of life-threatening intracranial HN.
S/S= Headache, nausea, double vision.
Eye examination= border of optic disc, unclear/undefined.
What does Papilledema indicate?
indicates increased pressure inside the skull (intracranial pressure), which can be a sign of serious underlying conditions like brain tumors, bleeding in the brain, or inflammation. Sign of life-threatening intracranial HN.
Signs and symptoms of Papilledema
Headache, nausea, double vision.
Clinical manifestations of Papilledema
headaches, nausea, vomiting, and pulsatile tinnitus, along with visual disturbances like transient visual obscurations, blurred vision, and double vision
Conjunctivitis
Occurs when conjunctiva of eye becomes infected or inflamed. Viral, bacterial and allergic causes of _. Bacterial or viral commonly called pink eye, very contagious.
Person can spread bacteria or virus by touching eye and then touching hands of another individual.
Contaminated objects or bedding can transmit microorganism as well.
Conjunctivitis manifestations
Red, swollen and eye feels itchy. Purulent or watery discharge from eye.
Myringotomy tubes
small, cylindrical devices inserted into the eardrum (tympanic membrane) to improve ventilation and drainage of the middle ear
Hearing loss
The inability to either detect or understand sound.
• Described as mild, moderate, severe, or profound.
• These categories are based on the range of sounds that cannot be heard in terms of dB hearing levels.
• Hearing loss may be congenital and present in infancy or acquired in later life.
• It can be described as genetic, acquired, sudden,
progressive, unilateral, bilateral, partial, complete,
reversible, or irreversible.
• Most types of hearing loss fit into the categories of conductive, sensorineural, or mixed deficiencies
• Noise levels of greater than 85 dB are associated with injury to the cochlea.
Hearing loss- mild
Lower than 26-40 dB. Difficulty following conversations.
Hearing loss- moderate
Lower than 41-55 dB. Hearing aids to hear normal conversation.
Hearing loss- severe
Lower than 60-90 dB. Can hear speaking, but cannot make out words (unless watching lips and mouth). Hearing aid needed.
Hearing loss- profound
Lower than 90 dB. Hearing aids. Lip reading and sign language.
Otosclerosis
a condition that causes progressive hearing loss by affecting the bones in the middle ear.
exact cause of otosclerosis is unknown, but it is believed to be a genetic disorder. It is more common in women than men and usually develops in young adulthood.
abnormal bone growth in the middle ear, specifically around the stapes bone. This growth prevents the stapes from vibrating properly, which is necessary for transmitting sound waves to the inner ear.
Meniere’s disease
Disorder of inner ear. Symptoms are result of changes in fluid volume of both bony and membrane labyrinth of inner ear.
Over time disorder is associated with progressive hearing loss and tinnitus. Although head trauma is one of major causes of this disorder, Unknown etiology.
Most common affects person 40 to 50 years old. Clinical presentations= episodic vertigo, fluctuating SNHL, tinnitus, feeling of pressure within ear.
Cataracts Treatment
Removal of cataract and replace with artificial lens. Manual small incision cataract surgery (MSICS), newest technique.
Cataracts causes
Excessive growth of epithelial layer of lens.
Senile cataracts- advance age, smoking, obesity, diabetes, UV light.
Congenital- develop due to infection; Rubella, syphilis, CMV.
Gradual vision loss and seeing halos at night. Eyes may have opacity covering.
Cataracts manifestations
Gradual vision loss and seeing halos at night.
cloudy or blurry vision, difficulty seeing at night, sensitivity to light, faded colors, and halos or glare around lights
Myopia
Nearsightedness, objects focus in front of retina, see near objects better
Hyperopia
Farsightedness, objects focused behind retina, see for objects better.
Presbyopia
Aging adults, decreased elasticity of the lens.
Astigmatism
Abnormal shape to lens or cornea, may be asymptomatic or present with blurred vision, eye strain.
Amblyopia
AKA= Lazy eye.
Usually present in children, visual cortex will neglect images from amblyopic eye, unless trained not to, use of eye patch on unaffected eye or atropine drops.
Entropion
Eyelid turns inward and irritates the eye
Ectropion
Eyelid turns outward
Pinguecula
Benign growths, yellowish growth that forms on conjunctiva
Pterygium
Benign growths that encroaches on corneal surface.
Exophthalmos
AKA- Proptosis, bulging of eye. Hyperthyroidism or ocular tumor= Thyroid eye disease- Graves’ disease.
Dryness and irritation, corneal inflammation, optic nerve compression. Corticosteroid drops, artificial tears, ophthalmic lubricants. Teprotumumab.
Enophthalmos
Recession of eyeball within socket. Surgery may be necessary
Blepharitis
Inflammation of the eyelids. Symptoms of _ include= red, watery eyes; dry, gritty sensation of eyes; burning sensation in eye; itchy eyelids; erythematous, swollen eyelids; flaking of skin around eyes; crusted eyelashes upon awakening; photophobia; excessive tearing; abnormal eyelash growth and loss of eyelashes.
Eyelids may also appear greasy and crusted with scales that cling to lashes.
Acne rosacea and seborrheic dermatitis are skin disorders associated with _ of eyelids
Smoking and open flame are the leading causes of burn injury for ____?
Older adults
Scalding is the leading cause of burn injury for ___?
Children