Microbiology and Immunology Exam 2 Class 3 [The Microbiology of Periodontal Disease]
1/99
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
100 Terms
What is Periodontium
Tissue that surround and support teeth
- Gingiva
- Alveolar bone
- Cementum
- Periodontal ligament
Collar of fibrous soft tissue that invests the cervical region on teeth and is contiguous with its periodontal ligament and lining alveolar mucosa`
Gingiva
Collar-like band of epithelium, which located apical to the base of gingival sulcus. It usually terminates at the CEJ in healthy conditions or close to CEJ
Junctional epithelium
The junctional epithelium function
- attaches to the tooth and provides a secure seal around the tooth surface
- Barrier against plaque bacteria
The junctional epithelium ______ migrates in periodontitis
apically
Form a dense fibrous network to provide the shape of gingiva and attachment to teeth
gingival fibers
Vascular and cellular connective tissue that surround the root and alveolar bone
Rich in: Cellular components and fibers
Periodontal ligament
Functions of the periodontal ligaments
- anchor teeth to the bone
- support and maintenance of gingival tissue
- Transmission of occlusion (chewing) force
- Absorption of occlusion force
Provides osseous support
Alveolar bone
The shallow V-shaped space that is coronal to the attachment of the junctional epithelium and bounded by the tooth on one side and the sulcular epithelium on the other.
Gingival sulcus
Exudate similar to serum, nutrients for bacteria and inflammatory molecules
Found in the gingival sulcus
Gingival crevicular fluid
Most common types of periodontal disease
- Gingivitis
- Periodontitis
Gingivitis
Inflammation that resides in gingiva and has not caused damage to the tooth supporting structures- cementum, PDL, and alveolar bone. No attachment loss so it is reversible
Periodontitis
Inflammation that results in the destruction of tooth supporting structures with bone and attachment loss and thus irreversible
When you put in your probe for a patient with gingivitis what is reason for having a bigger number
This is due to swelling of the tissue not due to a bigger pocket
Gingival Health without clinical attachment loss
When you probe the bottom of the sulcus is coronally positioned to the CEJ and so the junctional epithelium attaches to the enamel as well as a little bit to the root surface
- The root structure is not exposed
- No attachment loss
Periodontitis with clinical attachment loss
When you probe the sulcus is apical to the CEJ. Damage of the junctional epithelium and some bone loss. Junctional epithelium will be detached from the tooth and migrate apically.
- The root structure is now exposed
- Attachment loss
A biofilm-induced inflammatory disease which is the major form of tooth loss
Periodontal disease
Alveolar bone loss occurs when
bacteria are present
No bacteria =
Bacteria =
Minimal bone loss
More bone loss
NHANES studies
National Health and Nutrition Examination Survey
Based on NHANES study Periodontal disease is tightly associated with
flossing (plaque bacteria control practice)
- Non-flossers have more disease activity
We can conclude from the NHANES study that
more bacteria control = less disease activities
Other than bacteria the _______ response is also critical in periodontal disease
host immune
The plaque bacteria can activate a range of
different cells including host immune cells which can produce a lot of inflammatory mediators
If host response is disregulated (for whatever reason)
Inflammation will be more exaggerated and can lead to periodontitis
In oral cavity approximately _____ species most of oral bacteria are ________ under normal circumstances, living in harmoney with other bacteria and a host.
700, commensal bacteria
When this harmony is disrupted
dysbiosis disease can occur
Ratio of bacteria to human cell
10:1
TOP HAT: Which of the following statements is correct about facultative vs obligate anaerobes
Both can survive when oxygen is present
Neither can survive when oxygen is present
Both can survive when oxygen is absent
Neither can survive when oxygen is absent
Both can survive when oxygen is absent
TOP HAT: Which of the following statements is correct about Gram negative bacteria
Have a thicker cell wall than Gram positive bacteria
Have an outer lipid membrane
Appear to be purple in Gram staining
Do not produce endotoxins
Have an outer lipid membrane
TOP HAT: Pellicle for biofilm development is produced by
Host
Bacteria
Virus
Host (mainly from saliva)
TOP HAT: Compared to planktonic bacteria, the same bacteria in biofilm or plaque generally grow
Slower
Faster
About the same
Slower
Biofilm grow slower because they are competing for nutrients (his words later in the lecture)
Tooth Deposits: Materia Alba
- White-cheese like accumulation
- Salivary proteins, some bacteria, desquamated epithelial cells, food debris
- Lack organized structure
- Easily displaced with a water spray
Tooth Deposits: Plaque (biofilms)
- Primarily composed of bacteria in a matrix of glycoproteins and extracellular polysaccharides
- Biofilm
- Impossible to remove by rinsing or with the use of sprays
Tooth Deposites: Calculus
- Hard deposit that forms via mineralization of dental plaque
- Generally covered by a layer of unmineralized dental plaque
A structured community of bacterial cells enclosed in a self-produced polymeric matrix and adherent to an inert or living surface
Biofilm
Primary etiology of caries, gingivitis, periodontitis and peri-implantitis
Bacterial plaque
The biofilm is highly structured
This is true
Biofilms: Structured communities
Colonized by a diverse range of bacteria
- Heterogeneous microcolonies
- Efficient metabolic network
- Temporal pattern of colonization
- Communication (quorum sensing)
Adhesion of biofilms
- adhesion to matrix
- adhesion to other bacteria
Components of biofilm
Water: 97%
Microbial cells: 2-5%
Polysaccharides: 1-2%
Proteins: <1-2%
DNA and RNA <1-2%
Process of plaque formation
1. Formation of the acquired pellicle on the tooth surface
2. Initial adhesion/attachment of bacteria
3. Colonization/plaque maturation
The formation of the pellicle on the tooth or soft surface
- Thin layer of organic materia
- From Saliva (proline-rich and histidine-rich proteins, glycoprotein mucin-receptors for bacteria to adhere)
- Forms on tooth surface within minutes
- Bacteria-free, acellular
- Provides a scaffold
The initial adhesion/attachment of bacteria
- Occurs within 2 hours via bacterial movement, sedimentation, nonspecific hydrophobic, electrostatic, and van der waals forces-- reversible
- Strong attachment specific binding between adhesions from bacteria and (mucins) receptors in pellicle-- irreversible
Colonization/ Plaque formation
- Coadhesion: bacteria adhering to other bacteria that are already in the plaque mass (also through specific receptors-adhesins among bacteria)
- Coaggregation: Process by which genetically distinct bacteria become attached to one another via specific molecules in suspension (corncob and bristle brush)
Structural features of biofilm
- Has water channels as circulatory system in the deep layers of the film
- Has heterogeneity in the distribution of different species
- Enhanced tolerance of environmental stress, antimicrobial agents, and the host defenses (protection)
Communication between biofilm bacteria is through
Quorum sensing
Quorum sensing
bacteria secrete a signaling molecule that accumulates in the local environment and triggers a response such as a change in the expression of specific genes once they reach a critical threshold concentration
Quorum sensing is a method to control bacteria growth due to
Sense of pressure on the population of bacteria
Quorum sensing can modulate the
drug resistance genes
Colonization is not a random process
This is true
Early colonizers are
Streptococcus species
or other facultative anaerobes
- Gram positive
Secondary colonizers common features
All gram negative strict anaerobic bacteria
Subgingival Microbial Complexes study
Found:
- Associations among species analyzed via cluster analysis
- Yellow (strepptococci species)
- Orange complex (late colonizers): bridges the early colonizers and red complex
- Red complex: is closely associated with periodontal disease
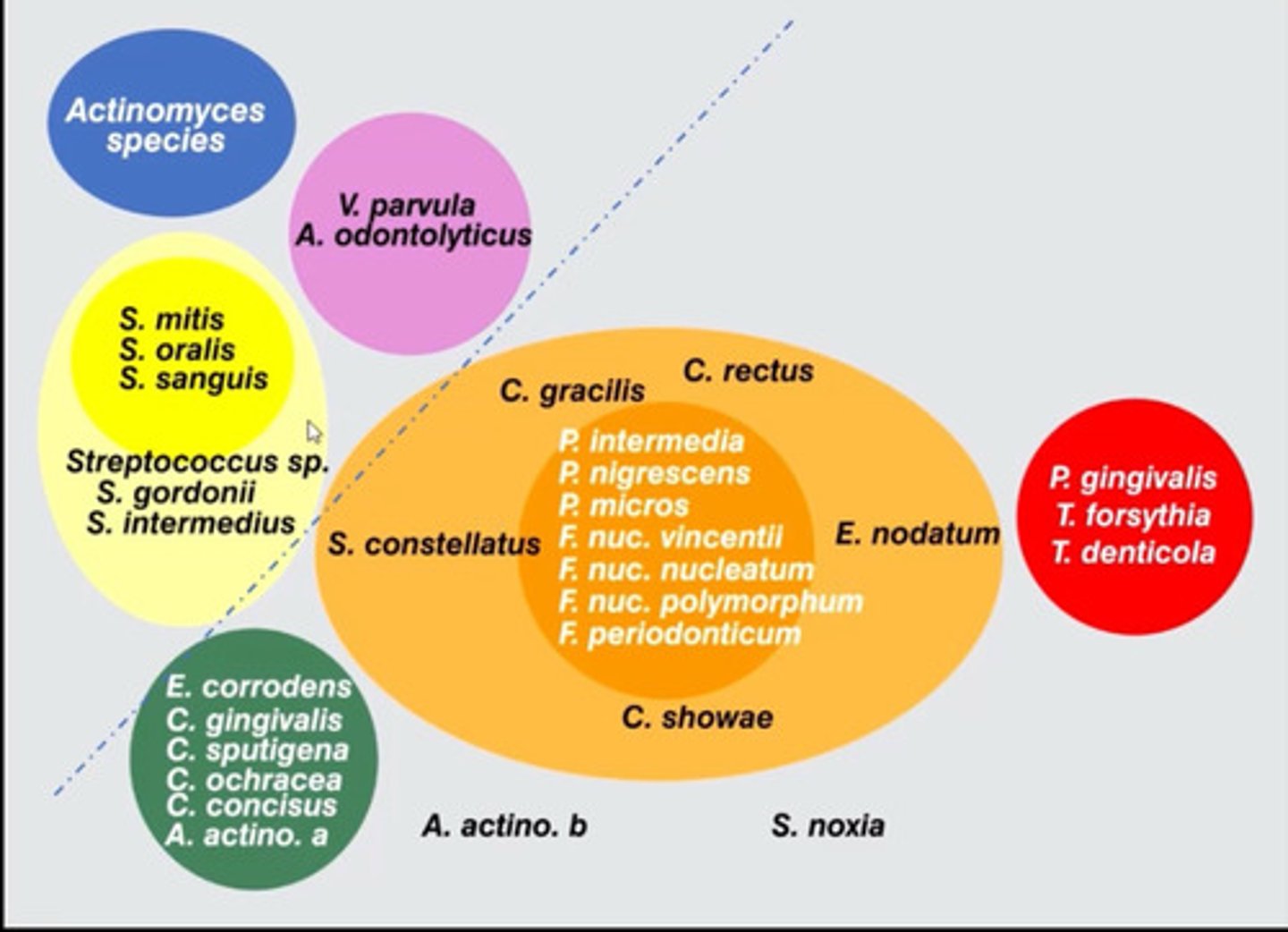
Bacteria closely related to periodontal disease
P. gingivalis
T. forsythia
T. denticola
Where are biofilms found
Supragingival
Subgingival
Supragingival
At or coronal to the gingival margin
Subgingivial
Apical to the gingival margin
Subgingivial plaque
1. Tooth attached
2. Unattached, loosely adherent, planktonic
3. Epithelial-associated
4. Connective tissue-associated (tissue invasion)
5. Alveolar-associated
Subgingival Biofilms compared to Supragingival Biofilms
- Limited access to oral cavity (anerobiosis)
- Increased gingival crevicular fluid
- Minimal mechanical removal by GCF flow due to presence of pocket wall
- Bacteria without adhesion may colonize
- Saliva is a limited source of new organisms
The bacteria within biofilms are _____-______ times more resistant to antimicrobial agents than their planktonic counterparts
1000-1500
Lacking transport system for an antibiotic; lacks the target of the antibiotic molecule; or outer membrane that covers cell wall of Gram negative bacteria
Inherent (natural) resistance
Acquired by means of mutation in its own DNA or acquisition of resistance-conferring DNA from another source; vertical gene transfer and horizontal gene transfer
Acquired resistance
Acquired resistance to antibiotic via:
- Vertical gene transfer
--spontaneous mutation in Bacterial DNA that is directly transferred to all progeny
- Horizontal gene transfer
-- Conjugation
-- Transformation
-- Transduction
Biofilm: why are the bacteria so resistant to antibiotic
- Slow growth in biofilm (nutrient limitation, stress)
- Failure of the antimicrobial to penetrate the biofilm (glycocalyx and exopolysacharide matrix)
- heterogeneity of biofilm structure
- Quorum sensing
- Exchange of genetic materials
Antibiotics used in periodontics
Amoxicillin: inhibition of bacterial cell wall formation
Metronidazole: Interference with bacterial DNA
Ciprofloxacin: Interference with DNA replication
Clindamycin: Inhibition of protein synthesis (50s rRNA)
Doxycycline: Inhibition of protein synthesis (30s rRNA)
Azithromycin: Inhibition of protein synthesis (23 rRNA)
For antibiotics to work they require the bacteria to be in the ____ phase
Log (exponential)
- Bacteria in biofilms are not in the Log phase (they are growing slowly)
Etiology of Periodontal Diseases 4 main hypothesis
1. Non-specific plaque hypothesis
2. Specific plaque hypothesis
3. Ecologic plaque hypothesis
4. Key stone pathogen hypothesis
Non specific plaque hypothesis (1950-1970)
- This theory correlated both age and the amount of plaque with evidence of periodontitis
- Large amounts of plaque would cause a higher production of noxious products, which would overwhelm the host's defense
- Control of the disease depends on the reduction of the total amount of plaque
Specific plaque hypothesis (1960-)
- The pathogenicity of dental plaque depends on the presence of or an increase in specific microorganisms
- Improvements in sampling and detection of bacteria
-- recognition of A. actinomycetemcomitans in aggressive periodontitis
-- Association of "Socransky's red-complex" in periodontitis
Ecologic plaque hypothesis ( 1994)
- Both the total amount of dental plaque and the specific microbial composition of plaque may contribute to the transition from health to disease
- The health-associated dental plaque = microbial homeostasis
- The host response may be brought by an excessive accumulation of nonspecific dental plaque, by plaque independent host factors or by environmental factors
- Microenvironment changes (host response) lead to dysbiosis
Keystone Pathogen Hypothesis (2011-)
- Certain low-abundance microbial pathogens can orchestrate inflammatory disease by remodeling a normally benign microbiota into a dysbiotic one
- P. gingivalis in specific pathogen-free mice can cause periodontal bone loss even when the proportion of P.g is very small in the total microbiota
- Interspecies communication between keystone pathogens and other members of the community is one of the key factors that leads to overgrowth of the more pathogenic microbiota
For disease to happen we need
1. Host susceptibility
2. Pathogenic bacteria
Pathogenic Bacteria
- T. forsythis
- T. denticola
- P. gingivalis
- A. actinomycetemcomitans
Socransky's Criteria for Microorganisms to be judged to be potential pathogens
- Be associated with disease, as evidenced by increases in the number of organisms at diseased sites
- Be eliminated or decreased in sites that demonstrate the clinical resolution of disease with treatment
- Induce a host response in the form of an alteration in the host cellular or humoral immune response
- Be capable of causing disease in experimental animal models
- Produce demonstrable virulence factors that are responsible for enabling the microorganism to cause the destruction of the periodontal tissues
The transition from health to Disease Bacterial profiles:
Health:
- G+ facultative species
- Streptococci, Actinomyces species
Gingivitis:
- Similar portions of G+/G- and facultative/anaerobic
- Increased Actinomyces, decreased Streptococci
Periodontitis:
- High % of G- anaerobes
- Rods, spirohcetes
Microbial shifting from health to periodontitis
From G+ to G-
From cocci to rods
From nonmotile to motile organisms
From facultative anaerobes to obligate anaerobes
From carbohydrate fermenting to proteolytic species
Certain bacterial species are protective or beneficial to the host
S. sanguinis
Veillonella parvula
C. ochraces
Bacteria associated with Gingivitis
Equal proportion of G+ and G- species
Equal proportion of facultative and anaerobic
Periodontal pathogens begin to be present (P. gingivalis, T forsythia, P. intermedia, C. rectus, Treponema spp) but in smaller amounts then periodontitis
Bacteria associated with Periodontitis
Plaque from sites with periodontitis showed elevated proportions of spirochetes
High percentage of anaerobic G- bacterial species
P. gingivalis and A. actinomycetemcomitants can invade host tissue cells
Qualifying bacteria based on Socransky's Periodontopathogen Criteria: P. gingivalis, A. actinomycetemcomitans, T. forsythia
Virulence factors
1. Factors that promote colonization (adhesins)
2. Toxins and enzymes that degrade host tissue
3. Mechanisms that protect pathogenic bacteria from the host
Virulence factors: Adhesion
Fimbriae or pili: polymeric fibrils that provide the points of contact on the host cells and tissues
Highly immunogenic
Virulence factors: Tissue destruction-promoting factors
Bacterial proteases activate the host enzymes
Trypsin-like protease activity
Example: Gingipain (cysteine protease) from P. gingivalis multifunctional proteins that play important roles in adhesion, tissue degradation, and the evasion of host responses
Virulence factors: Strategies for evading host immunity
Production of an extracellular capsule
Proteolytic degradation of host innate or acquire immunity components
Modulation of host responses by avoiding binding serum components on the bacterial cell surface
Invasion of gingival epithelial cells
P. gingivalis
G- obligate anaerobic, rod
nonmotile
Black pigment on blood agar (requires heme to grow)
Tissue invader/intragingival
Increased in active periodontal disease sites
Produces virulence factors
P. gingivalis main Virulence factors
- LPS: affects inflammatory response
- Capsule: evasion of phagocytosis
- Fimbriae: adhesion and biofilm formation
- Gingipains: degradation of protein immune molecules
- Hemolysis and hemagglutinins: adhesion, and heme acquisition and supply
A. actinomycetemcomitans
G- facultative anaerobic coccobacillus
nonmotile
Tissue invader/ intragingival
Increased in active periodontal sites
Major pathogen for molar-incisor patter periodontitis
A. actinomycetemcomitans main virulence factors
Leukotoxin: (kills all the below)
- PMNs (neutrophils) cell death, degranulation with massive lysosome enzymes
- Monocytes/macrophages: activation of inflammasome complex to secrete IL-1beta
- Lymphocytes: apoptosis
Cytolethal distending toxin (CDT):
- Causes DNA damage, cell cycle arrest, and apoptosis of affected cells (gingival epithelial cells, gingival fibroblasts and periodontal ligament fibroblasts)
- Stimulates pro-inflammatory and osteolytic cytokine production
A. actinomycetemcomitans cause localized aggressive periodontitis
This is true
Virulence factors that promote colonization: P. gingivalis
Fimbriae
Pili
Exoploysaccharide
Outer membrane proteins
Virulence factors that are toxins and enzymes that degrade host tissue: P. gingivalis
Collagenase
Trypsin-like protease
Gelatinase
Gingipain
Hemolysin
Hemagglutanins
Virulence factors mechanisms that protect pathogenic bacteria from host: P. gingivalis
Enzymes
Gingipain
Capsules
LPS
Virulence factors that promote colonization: A. actinomycetemcominats
Adhesins
Invasins
Bacterocins
Virulence factors that are toxins and enzymes that degrade host tissue: A. actinomycetemcominats
Cytotoxins
Heat shock proteins (HSPs)
Collagenase
Bone resporption agents
Virulence factors mechanisms that protect pathogenic bacteria from the host: A. actinomycetemcominats
Leukotoxin
LPS
Chemotactic inhibitors
Cytolethal distending toxin (CDT)
Immunosuppressive proteins
Fc-binding proteins
Oral/periodontal microbiome can be translocated extraoraly by
1. Enteral (GI) route
2. Circulation (bacteremia)
- Tooth extraction >80% incidence
- Toothbrushing 28% incidence
- Professional cleaning ~70% incidence
- Transient (40-60 min) in healthy individuals
-- Association not causation--
Necrotizing periodontal disease
- Painful acute lesions
- Severe inflammation
- Necrosis of the gingival tissue
- Increased bleeding tendency
Bacteria associated with with Necrotizing periodontal disease (not specific from periodontitis)
- Fusobacterium nucleatum
- Spirochetes (treponema)
- Prevotella intermedia
In necrotizing periodontal disease we have not
identified a specific bacteria causing the disease