Lecture 23: Traumatic Brain Injury
1/57
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
58 Terms
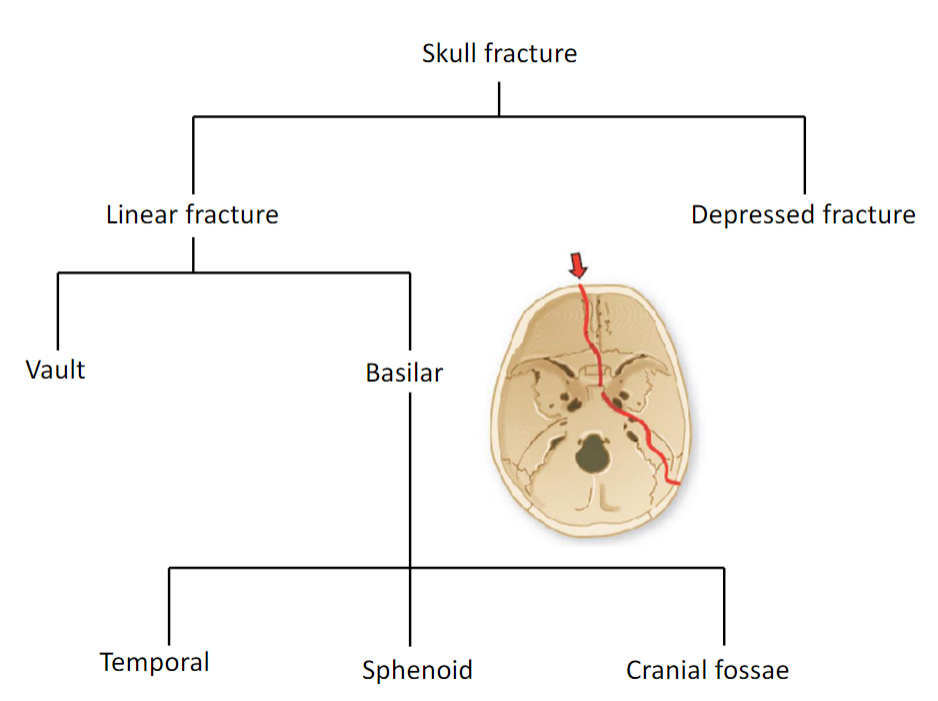
Types of skull fracture
Basal skull fracture
the absence of fracture does not mean the absence of brain injury
basal skull fracture easy to miss on CT
occult signs of basal skull fracture (revealed by PE):
leakage of CSF (otorrhea, rhinorrhea)
signs of cranial nerve damage (esp. I, VII, VIII)
characteristic accumulations of blood:
postauricular ecchymosis (Battle’s sign):
bruising over the mastoid process as a
result of extravasation of blood along the path of the posterior auricular artery or sigmoid sinus; indicative of fracture of middle cranial fossa
periorbital ecchymosis (raccoon eyes):
purplish discoloration around the eyes
following fracture of the frontal portion
of the skull base
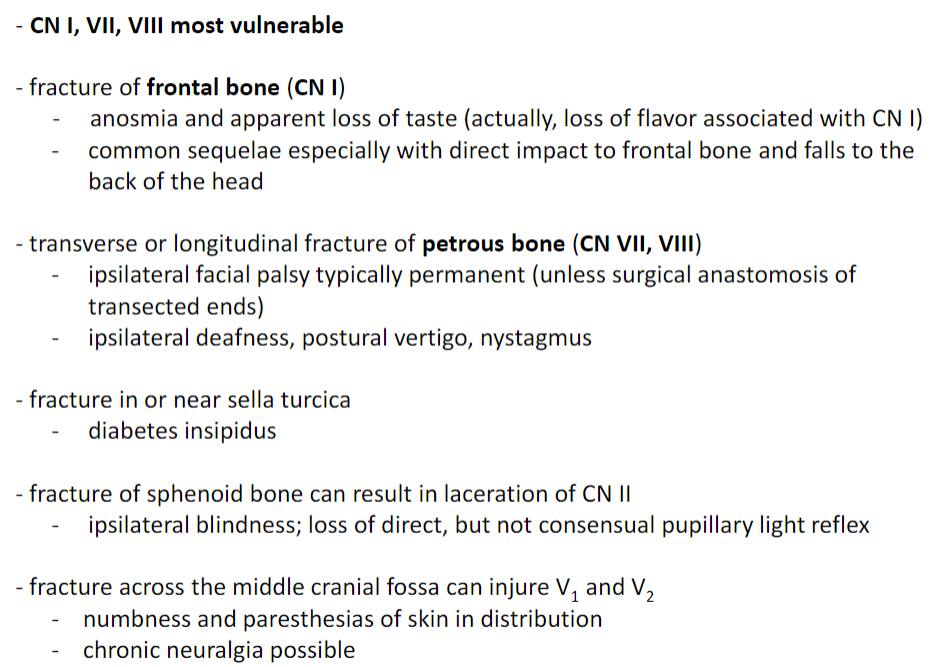
Basal skull fractures and cranial nerve injuries
Contusion Overview
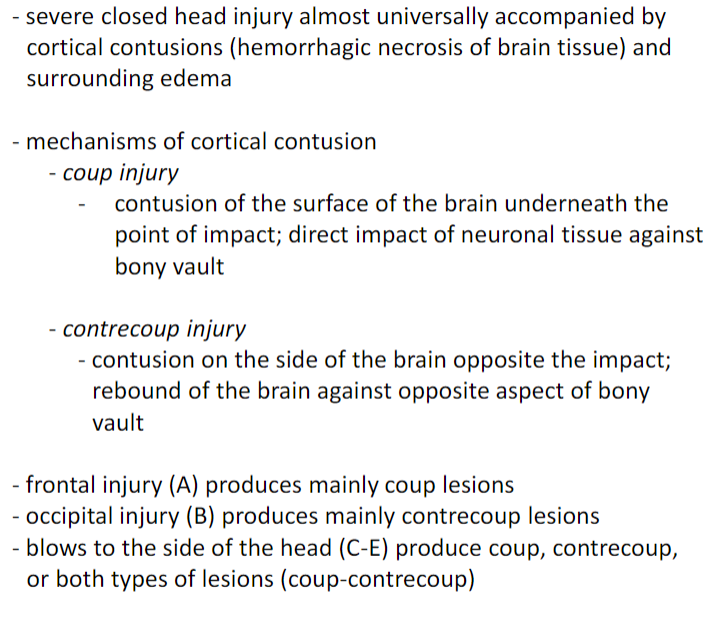

contusion
contusion

contusion
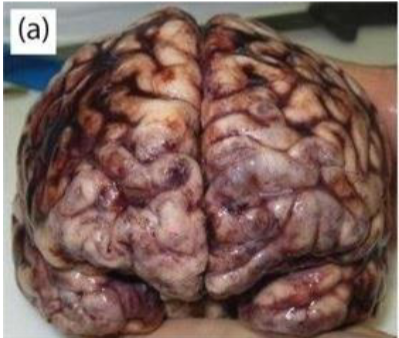
Contusions in gross anatomy
most commonly injured areas are orbitofrontal and anterior temporal lobes
contusion of occipital lobes and cerebellum rare due to smooth inner table of skull posteriorly
focal neurological deficits related to the site of impact
contused cortex diffusely swollen and hemorrhagic
lesions enlarge over several hours as a result of further hemorrhage
contusions typically involve crests of
gyri; often superficial, involving only
gray matter but may extend into
underlying white matter
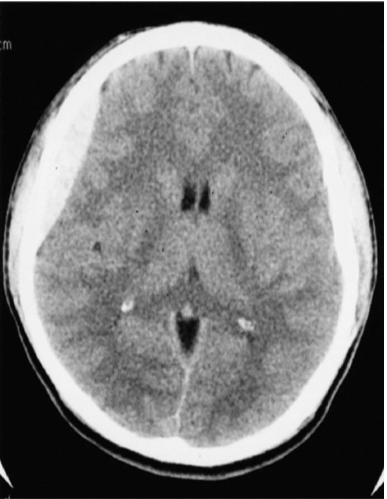
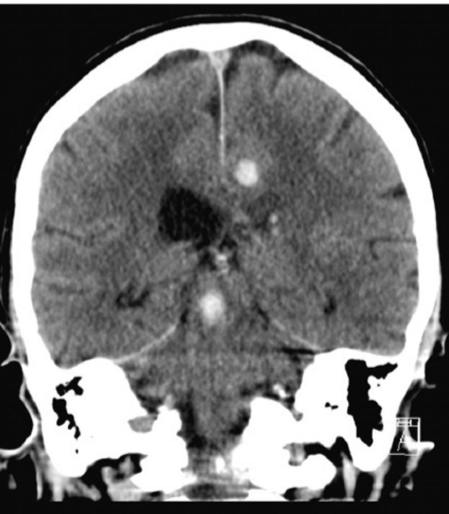
Contusion CT findings
lesions appear as edematous regions of cortex and subcortical white matter admixed with areas of increased density representing leaked blood
early response: within hours post-trauma, bleeding points in the contused area may appear small and innocuous
over time, may coalesce and appear as a single large clot or may appear as multiple contusions adjacent to bony prominences
delayed hematomas and edema are common sequelae that may develop up to days later
the mass effect of contusional swelling, if sufficiently large, becomes a major factor in the genesis of tissue shifts and elevated ICP
craniotomy and decompression of the swollen brain relieves the ICP, but has no effect on the focal neurological deficit
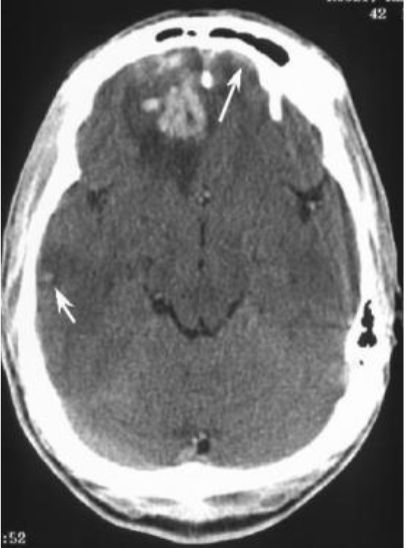
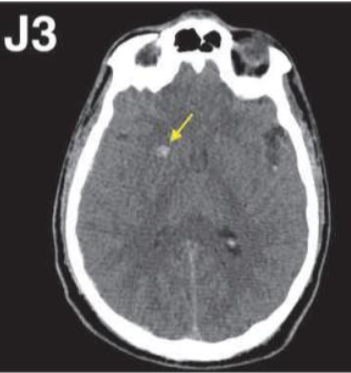
Acute brain contusion
smaller, subtle, right temporal cortical
contusion (short arrow) is noted, as
well as a small, left frontal subdural
hematoma (long arrow)
Acute brain contusion
subacute contusion
subacute contusion

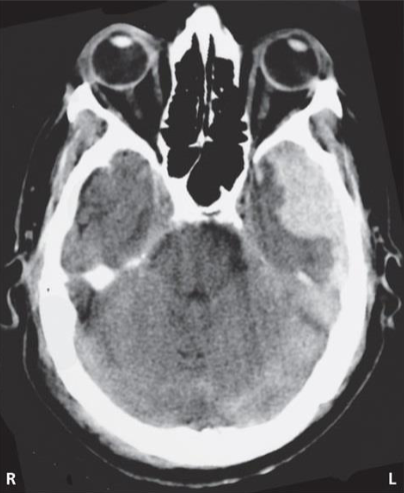
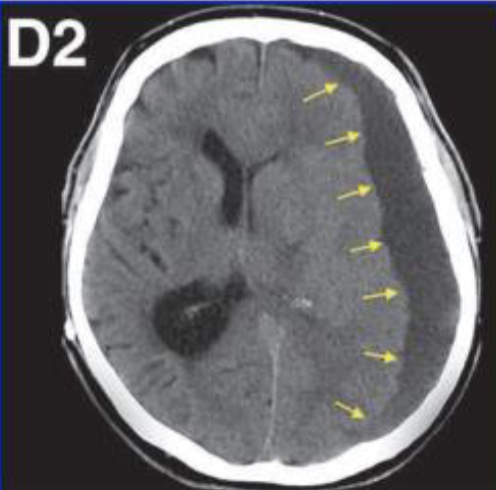
acute subdural hematoma

acute subdural hematoma
acute subdural hematoma
intracranial lesions often associated with intracranial bleeding (typically related to meninges); SDH is the most common post-traumatic bleed; may be unilateral or bilateral
typically results from tearing of bridging veins
usually present in combination with other mechanisms of injury (contusions, diffuse axonal injury)
CT findings: hyperdense, crescent-shaped
patients may be stuporous or comatose on admission or they may be alert
if comatose: typically, immediate coma that deepens progressively; high overall mortality
disturbances of consciousness and mentation (inattentiveness, confusion, apathy) are more prominent than focal or lateralizing signs
aphasia possible, but rarely observed
homonymous hemianopia seldom observed because the optic radiation deep and not easily compressed
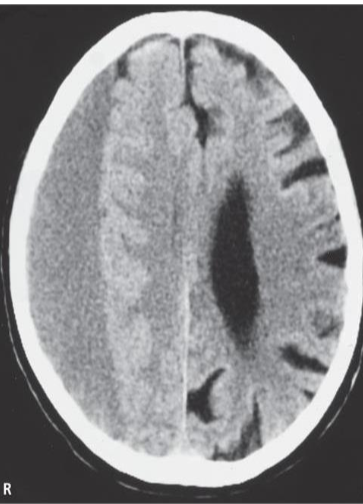
subacute SDH
subacute SDH
lot is initially hyperdense but becomes slowly more isodense after a period of one or more weeks
may be difficult to detect, except by the tissue shift that it causes
CT findings: isodense, clotted blood beginning to liquefy
generally related to mass effects (i.e., tissue shifts)
focal signs, when present, consist of mild hemiparesis (usually not complete paralysis)
dilation of ipsilateral pupil is a fairly reliable indicator of the side of the lesion
if the condition progresses, patient becomes stuporous or comatose
hemiparesis, dilation of I/L pupil, and
depressed consciousness = classic clinical triad of herniation
chronic SDH
chronic SDH
chronic SDH
traumatic etiology often less clear (especially in elderly)
if bilateral, no shift of tissue (effacement) apparent; mass effect can
produce herniation; compress upper brainstem
CT findings: uniform hypodense (if no further bleeding)
symptoms and signs develop over weeks and progressively worsen (mainly associated with elevated ICP)
headaches
light-headedness
slowness in thinking
apathy and drowsiness
unsteady gait
occasionally, seizures
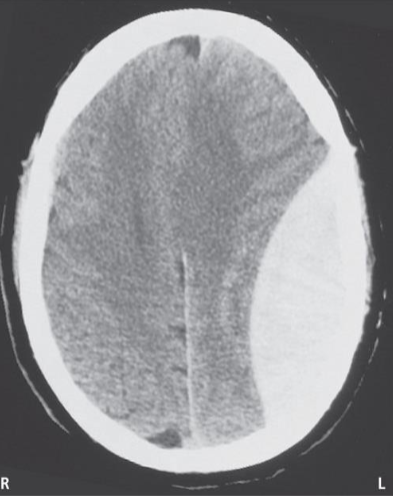
epidural hematoma
epidural hematoma
epidural hematoma
typically arises with a temporal or parietal fracture and laceration of the middle meningeal artery, or, less commonly, a tear in a dural venous sinus
initial loss of consciousness may be brief, followed by a lucid interval before rapid neurological decline
CT findings: hyperdense, lens-shaped with smooth inner margin
signs and symptoms appear over a few hours (increase ICP)
headache of increasing severity
vomiting
drowsiness
confusion
aphasia
seizures (may be unilateral)
hemiparesis with slight hyperreflexia, Babinski
progression of signs indicates herniation and worsening of prognosis:
coma
hemiparesis becomes bilateral with spasticity and Babinski
ipsilateral pupil may dilate and be nonresponsive
decerebrate posturing may appear
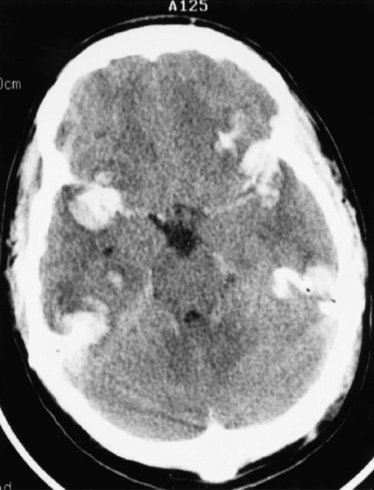
intracerebral hemorrhage
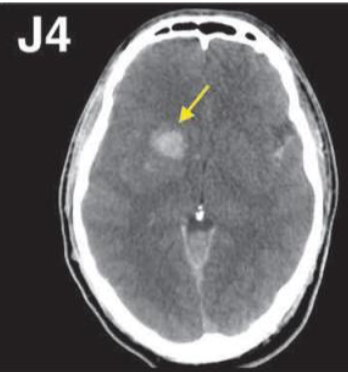
intracerebral hemorrhage
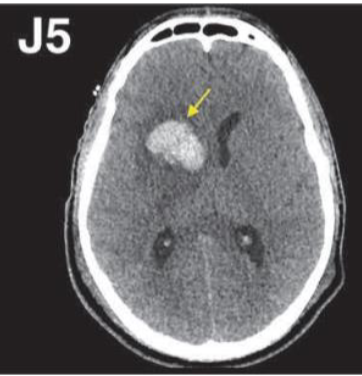
intracerebral hemorrhage
intracerebral hemorrhage
intracerebral (or intraparenchymal) hemorrhage
hemorrhages associated with coup-contrecoup injuries; shearing forces produce bleeding within underlying white matter as well as in gray matter contused areas
may include petechial hemorrhages or larger confluent areas of hemorrhage
bleeding occurs in subcortical white matter of one lobe of the brain or in deeper structures such as basal nuclei or thalamus
similar to hypertensive brain hemorrhage (hemorrhagic stroke)
altered consciousness: stupor progressing to coma
hemiplegia, Babinski (unilateral or bilateral)
dilated pupil
stertorous and irregular respirations
stertor: noisy inspiration occurring in
coma or deep sleep (i.e., snoring)
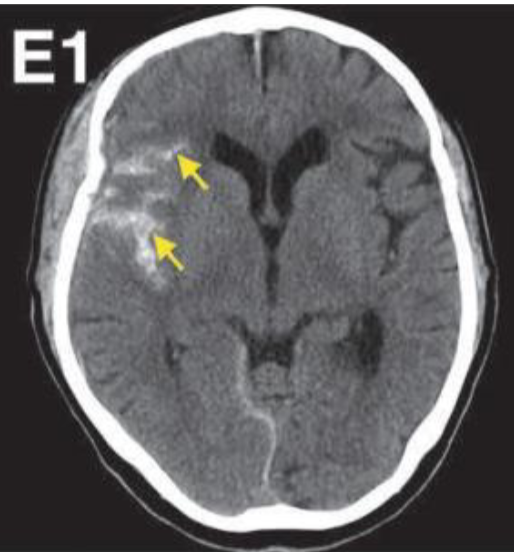
traumatic subarachnoid hemorrhage
traumatic subarachnoid hemorrhage
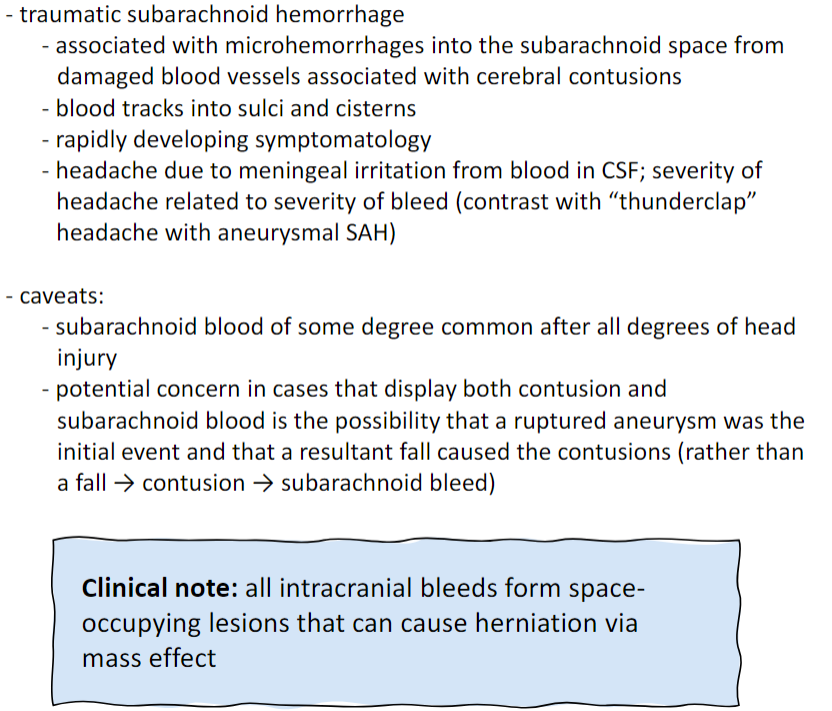
Acute subdural hematoma
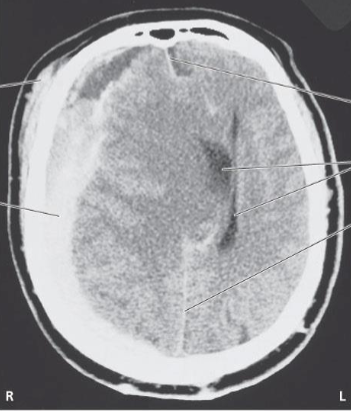
Subfalcine herniation
expanding supratentorial lesion presses the cerebral hemisphere
medially against the falx cerebri
particularly prominent in acute SDH; associated with midline shift
compression of cingulate gyrus, pericallosal, and callosomarginal
arteries
midline hemorrhage with cingulate
gyrus necrosis secondary to ACA infarct
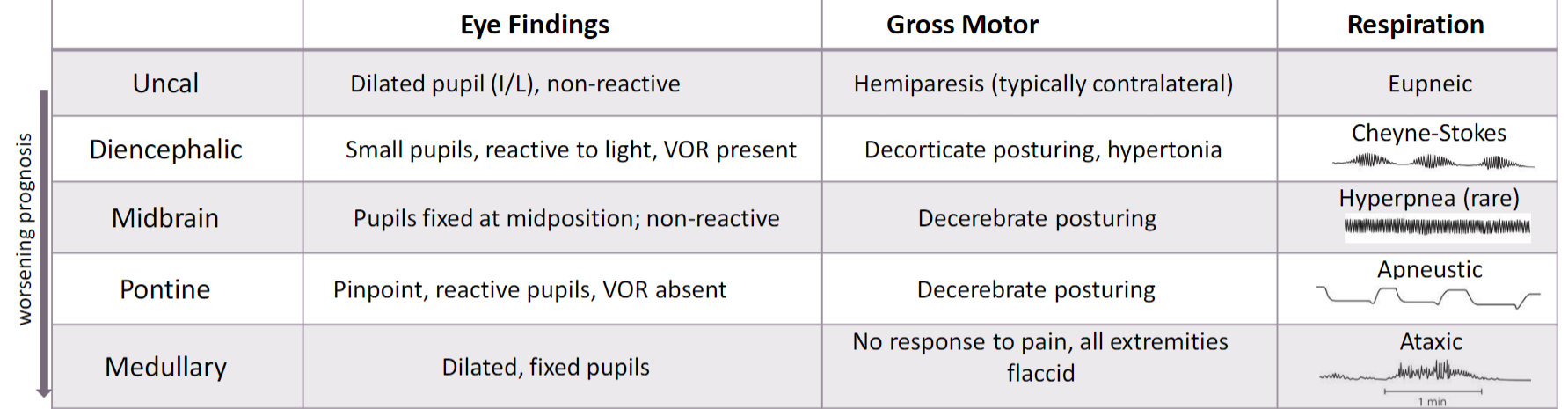
Central herniation
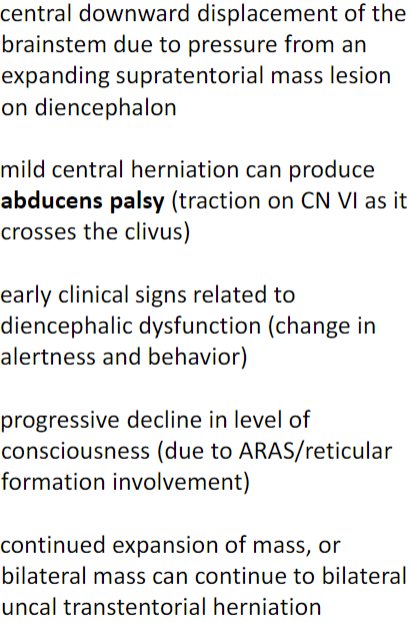

CN Vi
Clivus
Uncus
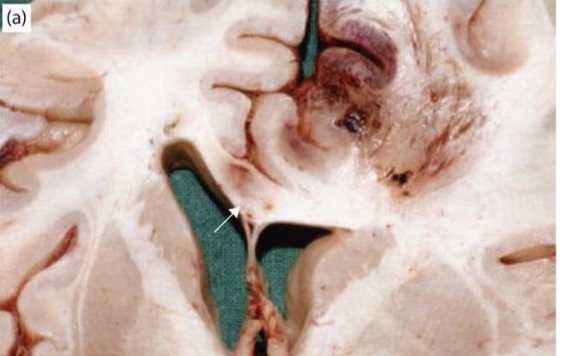
Uncal herniation
expanding mass lesion located laterally in one cerebral hemisphere forces the medial edge of the temporal lobe to herniate over the free tentorial edge into the tentorial notch
PCA compressed between uncus and tentorium
key clinical presentation: CN III dysfunction (ipsilateral pupil fixed and
dilated); decreased level of consciousness; hemiplegia (may be
ipsilateral or contralateral)
Clinical triad: “blown” pupil hemiplegia coma
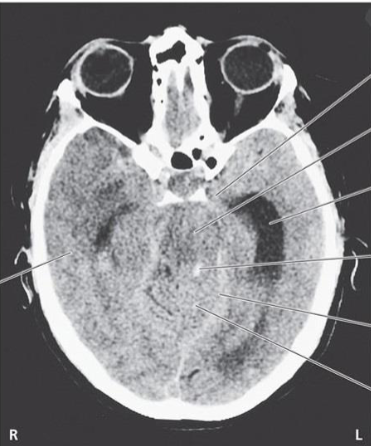
herniation syndromes summary
diffuse axonal injury
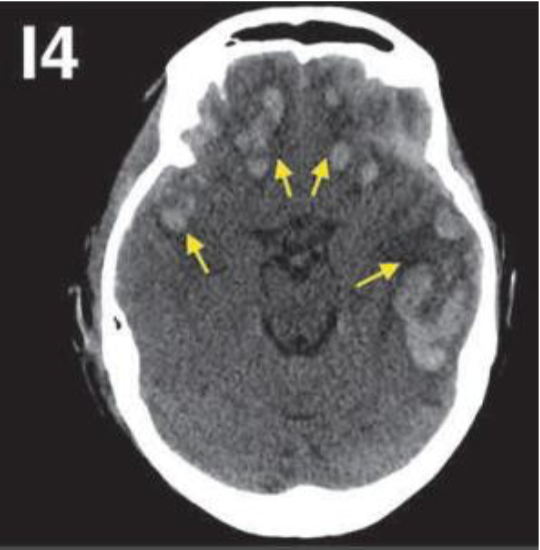
CT: widespread or patchy damage to the white matter and cranial nerves
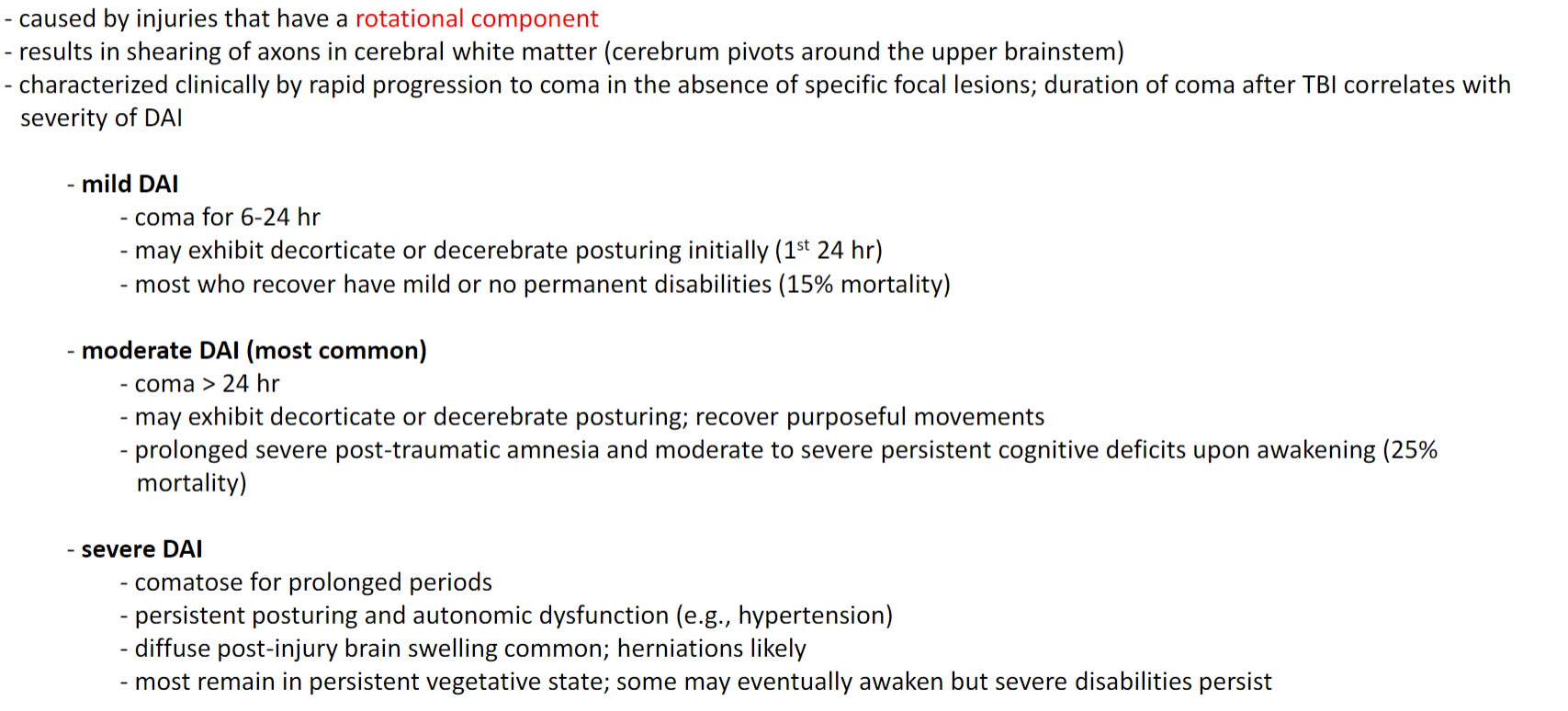
Acute gliding brain contusion
gliding contusion is caused by displacement of cortical gray matter during angular acceleration of the head
most of the damage at junction between gray and white matter (account for ~2/3 of DAI lesions)
acute DAI

acute DAI

acute DAI

acute DAI
acute DAI
the brain is either normal or shows petechial hemorrhages in the corpus callosum (most vulnerable area because of falx cerebri) or brainstem due to tearing of blood vessels
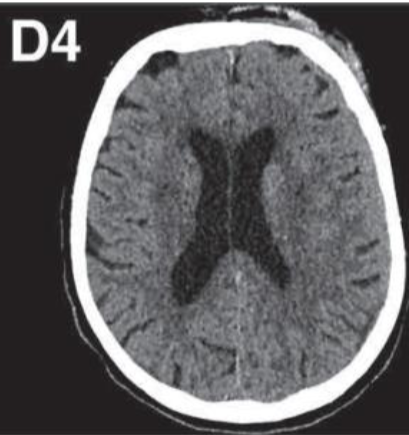
Diffuse axonal injury
overall decrease in gross brain weight due to:
decreased volume of white matter
atrophy of the corpus callosum
compensatory dilation of the lateral ventricles
Microscopic changes: axonal swellings (retraction bulbs; particularly common in
corpus callosum, fornix, internal capsule, and brainstem)
Concussion
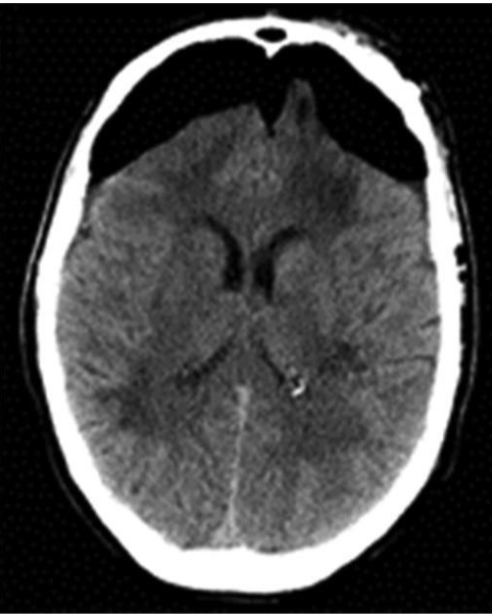
Pneumocephalus
Pneumocephalus
pneumocephalus: air within intracranial cavity
due to trauma or neurosurgical procedure (e.g., decompression)
can be acute (< 72 hours post-trauma) or delayed (> 72 hours post-trauma)
potential route for entry of bacteria into the cranium
tension pneumocephalus: when pneumocephalus results in increased ICP that leads to neurological deterioration (through mass effect)
headaches, nausea, vomiting, irritability, dizziness, seizures;
diminished level of consciousness; altered sensorium (inability to concentrate or think clearly) and CSF rhinorrhea or otorrhea
CT: subdural hypodensity of frontal area most common; followed by occipital and temporal areas
Mount Fuji sign: bi-frontal subdural collections that separate the frontal lobes
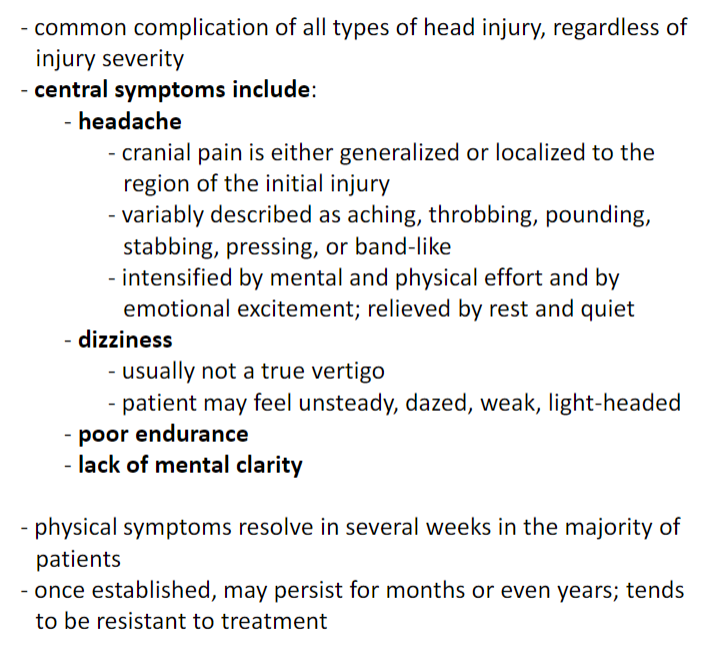
Post-concussion syndrome
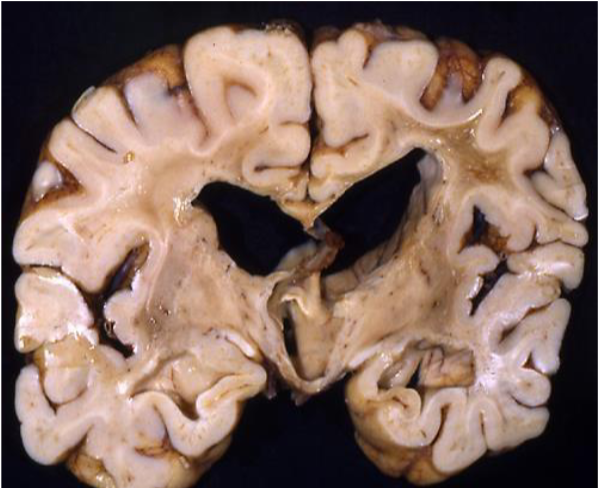
Chronic traumatic encephalopathy
neurodegenerative disorder resulting from cumulative effects of repeated cerebral injuries
clinical features (progressive):
early deteriorations in attention, concentration, memory
disorientation and confusion
progresses to lack of insight, poor judgement, and overt dementia
dysarthric speech, dysphagia, ocular abnormalities (ptosis)
movements are slow, still, and uncertain, especially involving the legs
wide-based, shuffling gait
plantar reflexes may be extensor unilaterally or bilaterall
Chronic traumatic encephalopathy Imaging
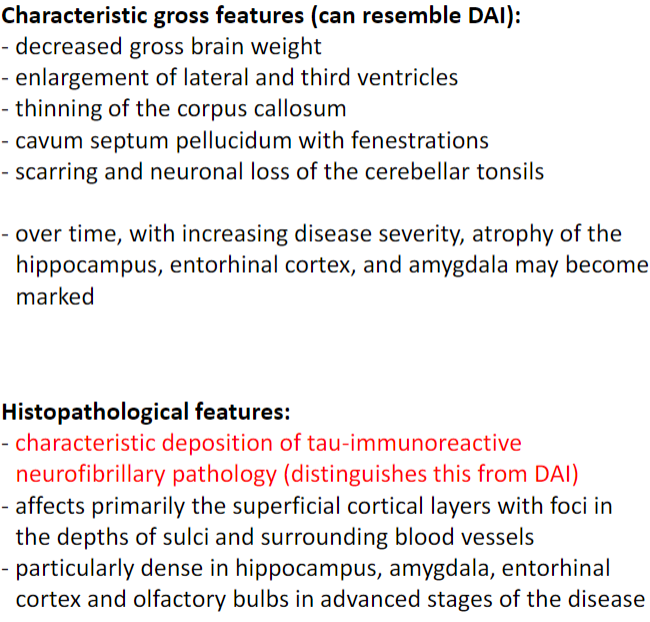
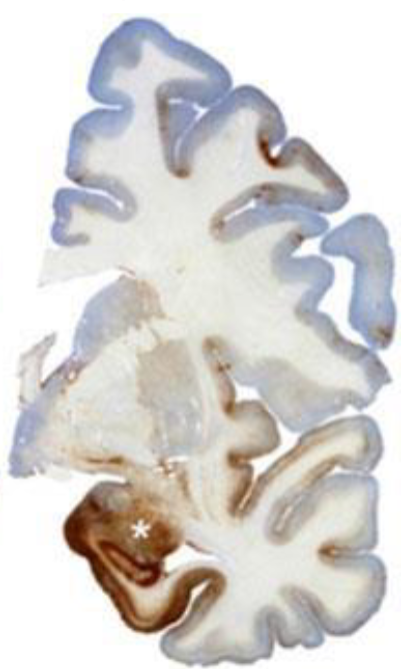
Chronic traumatic encephalopathy
brown staining indicates tau pathology
Axotomy Overview
axotomy (damage to the axon) causes the neuronal cell body to undergo chromatolysis, characterized by:
cell swelling
nucleus moves to an eccentric position
fragmentation of RER (“loss” of Nissl substance)
increase in protein and RNA synthesis (e.g., GAP-43)
chromatolysis is reversible if successful regeneration occurs; if successful regeneration does not occur, the neuron will die because the cell body is deprived of target-derived trophic factors
if the injury damages the neuron cell body directly, the cell will die
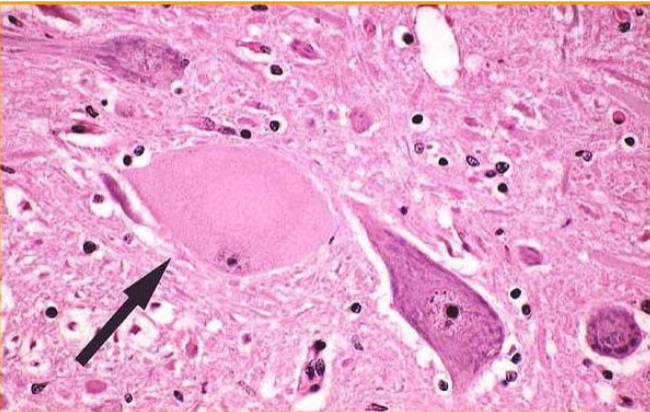
Axotomy and chromatolysis
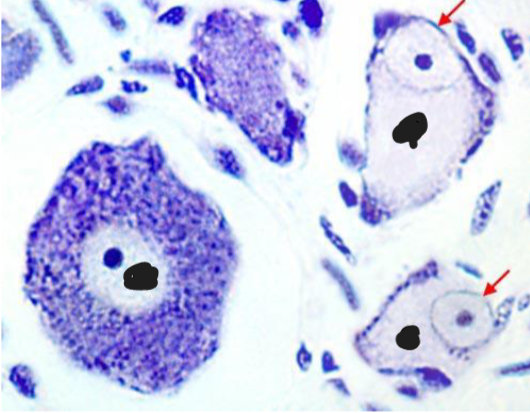
Axotomy and chromatolysis
Axotomy
results in division of the axon into two segments
proximal stump: remains attached to cell body
remains attached to the cell body; attempted growth and formation of retraction bulbs (characteristic histological feature of DAI)
distal stump: becomes disconnected from cell body; becomes detached from the cell body; undergoes Wallerian degeneration:
axon terminal degeneration
myelin fragmentation
phagocytosis of cellular debris (neutrophils, macrophages)
transneuronal degeneration
of pre- and post-synaptic neurons
synaptic stripping: retraction of presynaptic axon terminals from the dendrites or cell body of chromatolytic neurons; replaced by glial cells (microglia or astrocytes); decreases synaptic activity and impairs functional recovery
functional effect on post-synaptic neuron depends on the importance of the lost input to that cell; target cell may atrophy and die