Clinical biomechanics midterm SG (Davis)
1/64
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
65 Terms
What can a orthosis do?
- Improve function by:
Supporting skeletal system due to weakness
Decrease inappropriate movement
Maintain appropriate movement
Limit motion
Prevent deformities
- Improve Quality of Life
- Decrease pain
When applying an orthoses what should you watch out for?
Discomfort
Pain
Skin irritation
Nerve compression
Muscle weakness that can develop over time
Possible increase in energy expenditure
Psychological effect
Patient must be able to don, doff and want to use it
(Pretty straight forward, Davis emphasis to make sure you read the questions carefully and that sometimes he might put “NOT”)
When developing goals for the orthosis, what are the 4 main things to take into consideration?
What is one thing orthosis can also do?
Assist joint movement when joint movement is insufficient
Stabilize a joint by stopping or limiting motion when joint movement is excessive, abnormal or unwanted
Protect joint or skeletal component from excessive, unwanted or deleterious loading or forces that may cause pain or injury
Assist deformities: in management of joint or skeletal deformities
Can also prevent deformity
Accommodate, balance or support a fixed deformity
Correct a flexible deformity that interferes with function
Basic terminology - joints
Free
Assist
Resist
Stop
Hold
Free: No control is exerted, and the joint is free to move in a designated plane
Assist: Assists motion by applying an external force to increase the range, velocity, or force of a desired motion (IE, a spring, elastic band, motor, pneumatic force, muscle e-stim)
Resist: Resists unwanted motion by applying a force to decrease the velocity or force of an undesirable movement
Stop: Stop or limit motion at a joint. The prescription must indicate the specific motion to be stopped and then the stop is to occur in the rom
Hold: Controls and eliminated all motion at a joint in all planes. The prescription must indicate the specific joint position for the hold
Orthotic materials and properties
Strength
Brittleness
Ductility
Stiffness
Elasticity
Strength
The maximum external load or force that a material can sustain or support before breaking…commonly subjected to compressive, tensile, and bending forces
Brittleness
Materials that when loaded do not deform (change in shape) before breaking are called brittle
Ductility
Materials that yield or deform in response to loading prior to breaking are called ductile
Stiffness
The amount of deformation that occurs when a material is loaded. Materials that do not deform very much in response to loading are very stiff
Elasticity
The ability of materials that deform in response to loading to return to their original dimensions when unloaded. Materials that can return to their pre deformed size and shape have good elastic memory
Orthotic materials and properties
Plasticity
Viscoelasticity
Hardness (and how its measured)
Density
Durability or fatigue resistance
Corrosion resistance
Plasticity
The ability of materials that deform in response to loading to retain the deformation even after the deforming force has been removed
Viscoelasticity
The ability of materials to demonstrate both elasticity and plasticity when deformed in response to loading
Hardness
A material’s resistance to permanent indentation in response to a compression load. Hardness is measured in durometer
Density
A material’s weight per unit of volume. Materials that are lightweight but strong are most desirable
Durability or Fatigue resistance
The ability of material to withstand cyclic loading without breaking or deforming significantly
Corrosion resistance
The degree to which a material is able to resist degradation in response to exposure to chemicals, often exposed to water, perspiration, possibility of urine
(He will not ask a lot of questions directly about the terms on this flashcard and the last 2 cards (maybe 1 or 2) , but have a rough idea what they are and are not, as it makes it easier to understand characteristics of orthotics)
Shoes
Shoes were traditonally designed to?
Shoes are considered to be the _____ of a orthosis and may also be a _____ _____ by design
Shoes can be modified to redistribute what? Not only through the foot and ankle but also alter forces transmitted throughout the?
Well designed shoes can frequently help with?
Improper shoes can cause what?
Traditionally designed to protect feet from injuries and inclement weather. Designed to support feet during activities
Considered the foundation of an orthosis and may also be a corrective device by design
Can be modified to redistribute weight bearing not only throughout the foot and ankle, but also can alter forces transmitted throughout the lower limb
Well designed shoes can frequently promote healing, prevent further injury and provide an adequate foundation for lower limb orthotics
Improper shoes can cause blisters, calluses, ulcers, deformity
(He didnt really say much about this, but i would get a general idea of this)
Therapeutic footwear is designed to do what 5 things? SSDPI
Enhance shock absorption
Reduce shear stresses on the foot
Accommodate and support foot deformities
Accommodate or relieve pressure-sensitive areas
Accommodate shoe inserts and other devices that are worn inside the shoes
View the following image and fill in the red boxes:
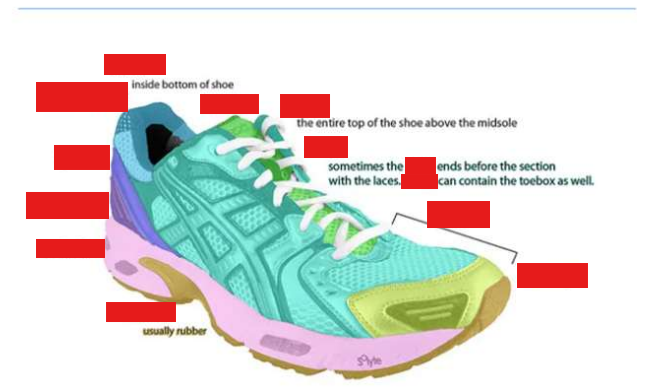
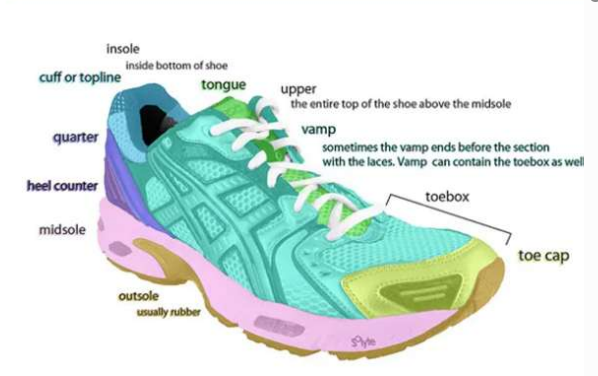
Toe box, Vamp, Insole, Outsole, Midsole
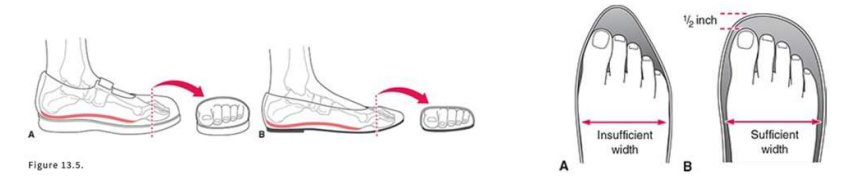
When recommending shoe fits for patients, what should you know/consider?
Try on shoes while wearing?
How much space should be in the toe box?
When should you try on shoes?
Try on shoes with proper socks, braces and orthotics
Leave adequate space in the toe box (1/4 to 1/2 inch rule - Must leave ¼ - ½ inches of space between the edge of the shoe and the largest toe)
Try on shoes in the afternoon or evening, as your feet expand throughout the day
Foot Orthoses (FO)
What are they?
What should you consider when recommending a foot orthoses?
What are the general goals of a foot orthoses? SPSSLDF
Can be custom-made, custom-fit, or modified prefabricated appliances designed to apply forces to a client’s foot to improve function.
Consider the client’s size and weight, how and where the client intends to use the device, and the source of abnormal forces or loads that contribute to complaints
Goals of a foot orthoses:
Provide cushioning to improve shock absorption
Provide relief for pressure-sensitive plantar structures
Reduce shearing forces on the foot
Balance or support the joints of the foot in a neutral position
Limit or restrict excessive or abnormal movements
Correct flexible deformity
Accommodate and support a fixed deformity
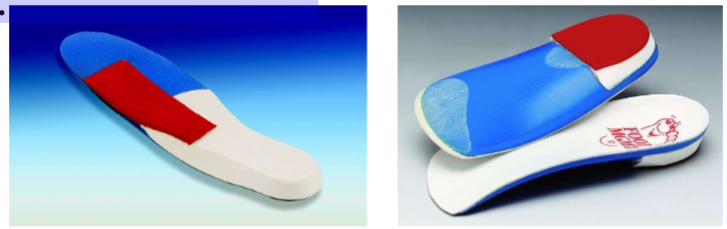
Foot Orthoses (FO)
What are the two categories of FO based on function?
Accommodative orthoses
Designed to provide protection or relief to areas or structures of
the footReduce plantar pressure and improve shock absorption
Reduce shearing forces, relieve painful or pressure-sensitive structures
Prescribed for patients that are diabetic or other forms of neuropathies
Useful for patients with significant rigid or fixed deformities
(moderate to severe OA)
Functional (Biomechanical) orthoses
Designed to support and control the subtalar joint, rearfoot, and forefoot and influence the biomechanical functioning of the foot during walking and running
Include use of wedges or posts that prevent abnormal
compensatory movements
(KNOW THE DIFFERENCES BETWEEN ACCOMODATIVE AND FUNCTIONAL FOOT ORTHOSIS AND WHAT TYPE OF PATIENT CLIENTAL WOULD BE REPRESENT OF THOSE TWO)

Foot orthoses (FO): Define the following
Soft
Semi ridged
Ridged
Soft: Flexible foam type materials provide cushioning, improve shock absorption, decrease shear forces
Semirigid: Combination of soft and rigid materials including cork, rubber, or plastics that provide some flexibility and shock absorption
Rigid: Strong, stiff, and durable materials such as plastic and metals used to assist with transfer of weight, stabilize and control abnormal motion
(Know why you would be using a soft material over the other two options or a ridged over the other two options or a semirigid over the other two options)
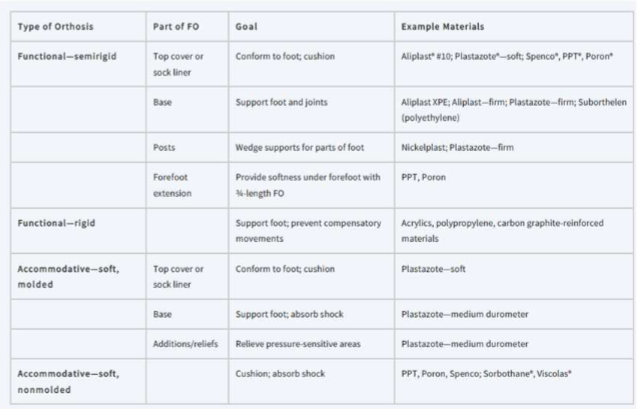
Don’t need to know example materials
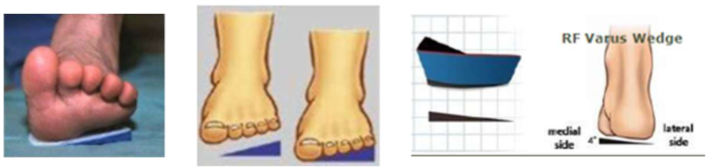
Posts or wedges
What are they? What do they do? Max degrees it can influence?
Material added onto the shell (extrinsic) or the shell itself is made thicker (intrinsic) within the rearfoot and/or forefoot region to either:
• Support in case of limited motion
• Control motion in cases of excessive motion
• Maximum amount is about 3-4 deg
(Do not overthink the question on the exam about this, just know what the purpose is and why you would do it)
Posts or wedges: Supporting limited motion foot deformities
Give examples for pronation and supination
Limited motion into calcaneal eversion (pronation of STJ) will be supported (build
ground up to the foot) with a medial (varus) rearfoot wedge/postLimited motion into forefoot supination, client presents with rigid forefoot valgus,
will be supported (build the ground up to the foot) by a lateral (valgus) forefoot
wedge (post)
(Do not overthink the question on the exam about this, just know what the purpose is and why you would do it)
What are the causes of orthosis failure?
Poorly performed/no biomechanical evaluation
Improper or inappropriate casting
Inappropriate materials used
Inappropriate prescription
Improper shoes/shoe wearing habits
Patient refuses to wear the orthotic
(He mentioned this too for the slide: not being educated about wear times, or how often you should be wearing them, or how you should be slowly adding more time day to day for the first 10 - 15 days. )
What are some Do’s and Dont’s when it comes to healthy foot care?
Do’s
Be aware of food conditions
Alert care providers immediately if
a problem is notedInspect feet after removing shoes
• Wear white socks if at risk for
woundsDaily foot hygiene and lubrication
Regular toenail care
Be fitted with proper footwear
Regularly check shoes/orthotics
for wearSelect appropriate activities
Optimize body weight/BMI
Don'ts
Do not walk barefoot
Do not soak feet in water
Do not walk on hot surfaces (sand)
Do not use chemicals or sharp objects to remove
callusesDo not use nail polish
Do not wear new shoes without frequent checks
Do not wear socks with constricting bands
Do not wear inappropriate shoes
Do not smoke cigarettes or use tobacco products
(Straight forward, easy give away question)
Varus/Valgus corrections - What are:
Medial T-strap
Lateral T-strap
Supramalleolar orthoses (SMO)
Medial T-strap
The leather strap arises from the shoe quarter covering the medial malleolus and buckles to the lateral upright pushing laterally to correct a valgus (eversion) deformity
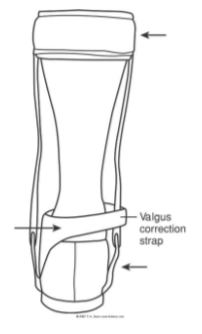
Lateral T-strap: The leather strap arises from the shoe quarter covers the lateral malleolus and buckles to the medial upright pushing medially to correct a varus (inversion) deformity.

Supramalleolar Orthoses (SMO): A low-profile supramalleolar design for subtalar joint control to limit varus or valgus within the ankle joint, which also assist with DF during swing

(Just know all this lol also know the patients that would wear a SMO, more on that in the next card)
More on supramalleolar orthosis (SMO)
Where are the trimlines?
Is there a hinge? Y or N
What does it provide compared to FO, and what does it still allow?
When are these commonly used?
Superior trimlines are above malleoli
No hinge
Provide increased medial/ lateral stability compared to FO and still allow DF/PF
Commonly used in pediatrics for those with excessive pronation

What are the differences between SMO, Posterior Leaf Spring, Medial leather t-strap, and Solid Ankle AFO?
Refer to other cards
(Will be a test question with a patient you are working with and you have to choose which one of these 4 you should use on them)
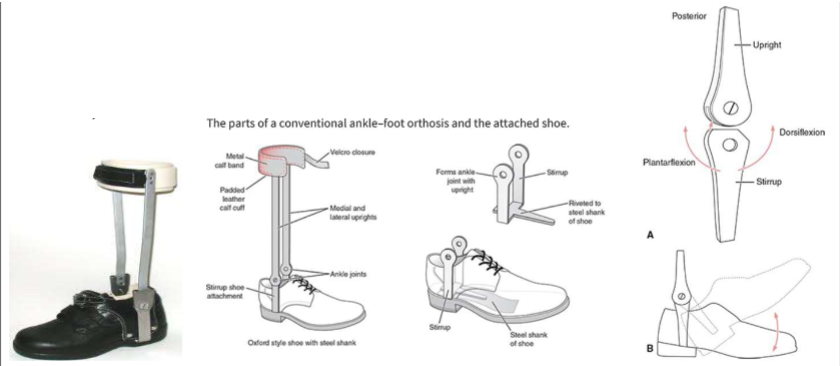
AFO types - Conventional
Made with what and extends from where to where?
Distally attach to?
The mechanical ankle joint must align with?
Can have what two things?
Type of joint and what does it mean?
What is one draw back with this orthosis?
Used mostly when?
Made with metal double uprights extend from ankle joint to leather calf band
Distally attach shoe, often built into the shoe
Mechanical ankle joint must align with the axis of the anatomical joint
Can have ankle stops or ankle assist
Are single axis joints (allow movement only in the sagittal plane)
Heavy, require more energy expenditure
Used mostly when there are skin or swelling issues
(Please understand the differences when talking about the conventional AFO use to look like, how they worked for patients, heavier, leather calf strap, built into the shoe)

More on AFO Conventional
What does it stop?
What does it assist?
Stops: restrict ankle motion at predetermined joint ROM such as 0 degree PF stop; DF stop; Limited motion stop
Assists: produce force to aid a designated joint motion; use of channels on side of AFO and tiny springs; DF assist; DF-PF assist.
AFO types: Posterior Calf Shell AFO
Can vary in?
The farther _____ the medial and lateral trimlines extend and the more the limb is enclosed the more _____ the AFO _____ ______.
When trimlines are located inch or more behind the widest part of the malleoli, what does this cause?
Can vary in rigidity (varies on the type, thickness and shape of material used) and assistance offered to ankle motion
The farther anterior the medial and lateral trimlines extend and the more the limb is enclosed the more rigidly the AFO resists movement
When trimlines are located inch or more behind the widest part of the malleoli, the AFO is more flexible supporting ankle during swing but little effect during stance (Typically called a Posterior Leaf Spring Orthosis)
(He talked more about posterior leaf spring but i would know this info just in case)

Posterior leaf spring (PLS):
Trimlines are _____ to malleoli
Motions occurs as the material does what?
When is it indicated to use?
Usually set in small degree of what motion?
Medial and lateral stability?
When is this not a good choice?
Trimlines are posterior to malleoli
Motion occurs as material bends and recoils
Indications: DF weakness
Usually set in small degree of DF
Medial and lateral stability varies but limited
Not a good choice if there is significant PF weakness or spasticity, if this is the case we have to use something much more firm and solid like the solid ankle AFO for example

Solid ankle AFO:
Where do the ankle trimlines extend/anterior to?
What does it not permit?
Very what?
When is it often used?
What is difficult when wearing this and why?
The ankle trimlines extend to or anterior to the malleoli
Doesn’t permit any movement
Very strong and stable
Often used with spasticity or when goal is to manipulate the GRFV and affect the knee during stance
The blocking of PF makes it difficult to rise from chair, go up ramps, squat and eliminates active push off during gait
(Didn’t say much on this slide but know the info)

HAFO - Free motion
Restricts what motions?
Free motion for what two movements?
When is it indicated to use?
Restricts frontal and transverse plane motion
Free motion for ankle DF and PF
Indications: when there is absent or weakness of inv/ever; functional strength of DF/PF

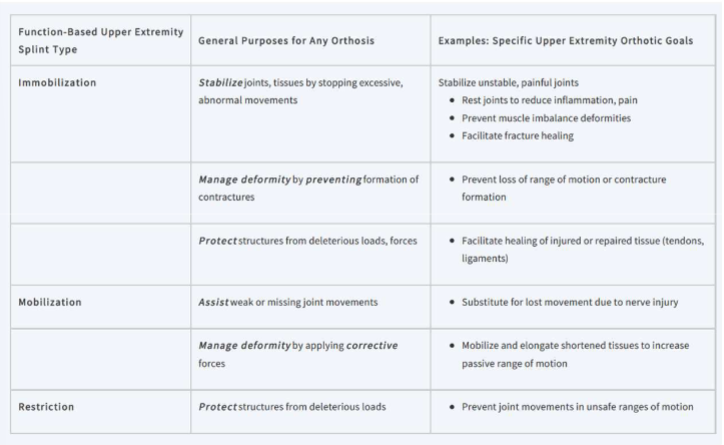
For the following terms what is the general purposes for each for any orthosis?
Immobilization
Mobilization
Restriction
No need to memorize the far right column
Categories of splints
What are static splints (with sub categories)?
What are dynamic splints?
Static Splints: passive supports that hold a joint or body part in a particular stable position (a position of rest or functional position)
Subcategories include serial static and static progressive splints these are used to increase joint ROM. They mobilize shortened tissue.
HAVE NO MOVING PARTS OR COMPONENTS. PROVIDES SUPPORT AND IMMOBILIZATION
Dynamic Splints: Impart forces to target joint to substitute for missing muscle contraction or apply a low load prolonged stresses to increase tissue length. Often use elastic bands, springs, or material that store and release energy.
WILL EMPLOY TRACTION USING RUBBER BANDS OR SPRINGS OR CORDS OR VELCO TO PROVIDE A LOW LOAD PROLONG STRESS
(MAKE SURE YOU KNOW THE DIFFERENCES BETWEEN THESE TWO SPLINTS)
More on static and static progressive splints
What are they used for?
How do they mobilize tissues?
Low load prolonged stress produces and stimulates what?
Specialized splints that are used as part of a program to increase joint ROM by increasing connective tissue length
Mobilize shortened tissues and increase their length by applying low load, but prolonged tensile stresses at the end point of the available passive joint ROM
Low load prolonged stress produces stress relaxation and stimulates the connective tissue cells to increase tissue turnover and remodeling
(He didnt really say anything in particular here but know all)
More on dynamic splints
What are they and what do they do?
Used to provide?
This splint must apply only a certain amount of force, why?
Mobilization devices that apply dynamic forces to the body, usually by using elastic bands, springs, or other materials with elastic memory that store and release energy
Used to provide low load prolonged stress to increase joint ROM, however, the end range force is dynamic and is usually produced by a spring or elastic material
Splint must apply only the amount of force required to hold the end range position, the use of high tensile loads that produce pain and limit total end range time is less effective
(He said to “know all those key terms” so i assume he means know all this)
Shoulder slings
What are they used for? What about patients with hemiplegia?
Should have what and why?
What is commonly made of and what type of designs can it have?
Often used to protect from subluxation, Use to protect and immobilize the shoulder after surgery or fracture. May be used with patients that present with hemiplegia or low tone, worn to prevent subluxation of the shoulder while the arm is flaccid.. Also reduce pain
Ideally should have broad straps and cuffs to help distribute pressure
Commonly made of fabric construction, an assortment of designs
include the figure 8, universal sling, bandanna sling, flail arm sling
(Definitely know when and when not to use a shoulder sling, for instance if patient had a mild shoulder injury and you don’t know what it is its probably best for you to immobilize them and put them in a sling, or a patient is having a lot of subluxation either do to injury or a neurological condition like hemiplegia or low tone you should put them in a sling too. If they have high tone levels its probably not a good idea to try to get them into a sling)
Elbow orthoses
Commonly used to (Static/restrictive and dynamic/mobilize)
Static orthoses or restrictive - No movement, protect healing of repaired structures.
Can be removed for topical ointments and hygiene
As ROM returns, the angle of the splint can be adjusted by reforming the plastic shell
Used with burns, fractures, tendon injury, nerve injury, vascular repairs, and cubital tunnel syndrome

Dynamic orthoses or mobilize - Used to improve contractures that are limiting ROM
Splints used for clients with burns and elbow contractures.

Tone reducing orthoses
When are they used?
Primary objective? How is the hand placed? How long should it be worn for?
Anti-spasticity splints are prescribed when hypertonicity is present
Primary objective is to reduce flexor tone, reduce the incidence of contractures, and maintain the arches
• Placing hand and fingers in an extended and abducted
position
• Creates firm pressure on the palmer surface of the hand
• Avoid over pressure areas and potential skin irritation
• Worn 2 hours on and 2 hours off


What are the therapeutic benefits for orthosis for trunk and cervical regions?
Intra-abdominal pressure
Considered controversial
Pressure exerted on the abdomen by the corset or rigid orthosis creates a cylinder effect, which in turn raises the intracavitary pressure
Believed to reduce the intradiscal pressure during forward bending
Muscle relaxation
Reduces the need for abdominal contractions as the cylinder effect to support the vertebral column is created passively, thus relaxing the abdominal and erector spinae muscles
Decreasing the need for contractile support of the vertebral column may relax the muscles and reduce existing pain
Restriction of motion
Primary method employed for motion control is the three-point pressure system
Amount of limitation varies between the designs, however, a reduction in the
motion at retrospective intervertebral segments has been linked to a reduction in
pain and spinal instability
Postural realignment
Increased IAP, relaxation of muscle in spasm, and restriction of movement can assist in facilitating improved posture and reduce compensatory postures related to pain
(He didn’t really go over each individual section, i would know the general bullet points for sure. The information under each one is probably good to know too)
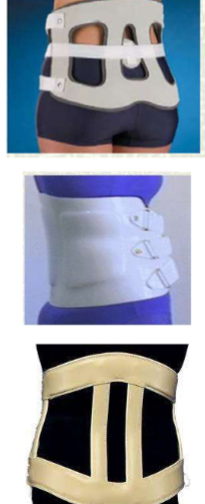
Throacolumbosacral orthoses - Soft
Example of these?
What does it limit?
What does it help with?
Inserts (stays) can be used for?
How can it affect breathing?
Corsets
Limit thoracic flexion
Offer flex/ext control. May provide some control for side-
bending and rotationInserts (stays) can be used to increase the control provided
Can alter breathing patterns of normal patients by reducing the tidal volume and increasing the respiratory rate (may be appropriate for patient with spinal cord injury or muscular dystrophy)
(He said to know the information on thoracolumbar orthoses when they are soft VS Lumbar belts)

Lumbar belts
What does it restrict and increase?
May prevent what?
Prolonged use can cause?
What can it remind the user of?
NIOSH concluded that?
Thought to restrict motion and increase IAP
Little evidence that they prevent low back injury
Some thought that prolonged use may lead to muscle weakness
May provide a kinesthetic reminder
NIOSH has concluded that because of the limitations of the studies analyzing workplace use of back belts the results cannot be used to support or refute their effectiveness in injury reduction
((He said to know the information on thoracolumbar orthoses when they are soft VS Lumbar belts. Lumbar belts for people who are doing weightlifting or factory workers or warehouse workers where they are doing a lot of movements and are trying to reduce levels of injury)

Sacroiliac belt
Used for?
Where is it located?
When is it commonly used?
Use for back pain that is attributed to SIJ hypo or hypermobility
Locate between the iliac crests and greater trochanter
Commonly used during pregnancy of female patients, decrease SIJ mobility, and reduce pain during symptoms associated with functional activities that may be linked to SIJ instability

Rigid Lumbosacral Orthoses
What system does it employ and what does it limit? Also help with?
What is it typically made from?
Worn over or under clothes?
When wearing one, what should you watch out for? What is commonly done to avoid it?
How does it affect lordosis? Limits what motion?
What does it not limit? This means you can permit what exercise?
Employ 3-point counterforce system to limit motion in the lumbar spine and make sure you have upright posture.
Typical make today from molded plastic
Worn under clothing
Watch for rubbing or skin irritation, often use a T-shirt or body sock between skin and brace
Lordosis is decreased to limit lumbar extension while the pelvic and thoracic bands exert a medial force that tends to limit lateral trunk motions
There is no limitation of trunk flexion, therefore permitting light flexion exercises to increase abdominal strength while wearing the orthosis
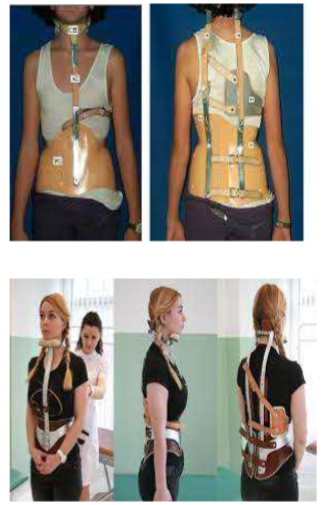
Thoracolumbosacral Orthoses- TLSO
Controls motions in what planes?
What type of material is it made from?
Commonly used to?
Stabilizes what levels of of the spine?
Taylor device (limits what motions? Pelvic band connects with? Terminating at? What pressure system is used?)
Control movement in all planes
Thermoplastic (body jacket)
- Have total contact except over bony prominences
- Typically bivalved “clamshell” deviceCommon use
- Restrict spinal movement after surgery
- Limit thoracic flexion
- Prevent progression of scoliotic curvesTypical effective range of stabilization T5-L 4
Also called a Taylor Device
- Limits flexion/extension
- Pelvic band connects with 2 posterior uprights terminating at the mid-scapular level of the thoracic region
- 2 three-point pressure systems are coupled together to limit both flexion and extension of the lumbar and thoracic spine

TLSO- Jewett Hyper-extension Brace
Limits what motion? Provides?
What type of counterforce system? What does this provide and why?
Fabricated or Prefabricated? Easy or difficult to put on or off?
Limits forward bending of spine, provides stabilization
3 point counterforce system, applies anterior and posterior forces through sternal and suprapubic pads opposed by a central posterior to anterior force, thus providing a hyperextension force to unload healing vertebral compression fractures
Prefabricated and easy to put on and off

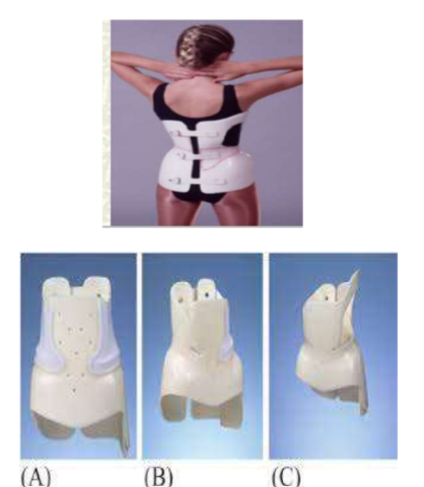
TLSO- Plastic Body Jacket
Limits what motions?
Fabricated with?
Anterior and lateral trunk containment elevate what? Decreases demand of the?
Frequently used when?
Limits Flexion, Extension, and Lateral-Rotary Movements. Well-fitted body jacket that is designed to restrict motion in all planes
Typically fabricated with high temp copolymer plastics
Anterior and lateral trunk containment elevate intracavity pressure, and decrease demands of the vertebral discs
Frequently used post surgically or during acute trauma

CASH (Cruciform anterior sternal hyperextension) orthosis
Limits what motion
Similar to what orthosis?
Has also been used in what retraining and why?
Issues with?
Limit flexion
Similar to the Jewett
Has also been used in postural retraining to increase thoracic extension
Issues with it migrating or rotating during functional activities
(He is not as concerned about the CASH but know what the design looks like, might use it as an alternative test answer

Milwaukee Brace
Used for what condition?
Describe the lay out of the brace.
Positives?
Negatives?
Why is it not used much anymore?
Used for scoliosis
A CTLSO with one anterior and 2 posterior uprights that extend from the pelvic mold and connected to the cervical spine with a neck ring
(+) are that each component of the pelvic, thoracic, and cervical region can be molded or adjusted to slow or even correct scoliotic curve
(-) are that the brace must be worn for 12-18 months, 23 hours a day
Not used much anymore due to poor psychological concerns, and poor acceptance by children and teens
(KNOW THE DIFFERENCES BETWEEN A MILWAKEE VS BOSTON VS PROVIDENCE VS WELLINGTON VS CHARLSTON. ANY PATIENT THAT HAS A CERVICAL COMPONENTRY OF SCOLIOSIS YOU USE MILWAKEE)
More on scoliosis orthoses
Used to treat?
How long are they worn daily and at night?
Most effective when the curve is how many degrees?
Goal of the brace?
Types of force application? (passive and active uses what to apply pressure to where, passive uses what counterforce couple to support and correct what? )
To treat adolescent idiopathic scoliosis
Worn for prolonged periods of time
- Daily for 16-23 hrs (Milwaukee, Boston, Wilmington) (Also worn for a longer time over a year to two years)
- At night: 5-7 days a week (Charleston, Providence)Most effective when the curve is 20-45 degrees
Goals of the brace:
- Support the trunk and stop or minimize the progression of the curvature
- Decrease pain
- Improve appearance
- Allow for growth of the spineTypes of force application
- Passive and active: use pads to apply pressure at the apex of curve
- Passive: use 3 point counterforce couple to support and correct the
curve
Boston Brace
Passive or Active?
Applies pressure where and why?
As curve reduces, what is added?
Generally used for? Easy or difficult to take on or off? Taken and put off in the anterior or posterior?
Passive and active brace
Applies pressure at the spinal convexity to “push” the spine
As curve reduces more pads are added
Generally used for lower thoracic and/or lumbar curves. Worn well and easily taken on a off, taken and put off in the posterior
Wilmington brace
Passive or active? What is it made from?
Is this custom made or pre made?
Where was this developed
Worn for up to how many hours a day?
Taken and put off in the anterior or posterior?
Passive appliance fabricated from thermoplastic material
Custom made from individual cast
Developed at DuPont Hospital for Children in Wilmington DE
Worn for up to 23 hours a day
Generally put on through the anterior

Nighttime Orthoses
Why are these considered ‘more acceptable’ ?
Providence brace (Passive or active? Applies controlled direct _____ and _____ forces on trunk)
Charleston bending brace (Applies ____ ____ forces towards ______ of the curve to overcorrect it. Most effective when the curve is below what level?)
These may be more acceptable due to wear time and cosmesis issues
Providence Brace
- Passive brace employs overcorrection in a
molded plastic appliance.
- Applies controlled direct lateral and
rotational forces on trunk.Charleston Bending Brace
- Molded plastic TLSO formed over a cast
of child’s trunk.
- Applies side- bending forces toward the
convexity of the curve to overcorrect it.
- Most effective with SMALL SINGULAR THORACOLUMBAR CURVATURES (single curve only one movement of the curvature) with apices below T7 (somewhere between the thoracolumbar spine)
T7

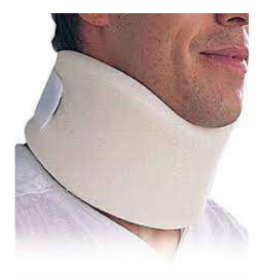
Cervical collars
Encases what part of the body?
Soft collars: Fabricated or prefabricated foam?
How is it secured?
Where can you get these?
Describe how its laid out.
How do they vary
Does not significantly limit what?
Encase the neck
Soft Collars: prefabricated foam (different degrees of firmness)
Secured with VelcroOver the counter devices
Slightly wider posteriorly with anterior “cut-out” to accommodate the chin
Vary in lengths and widths
Do not significantly limit cervical spine motion
(Know the differences between a soft collar vs semi rigid)
Cervical orthosis
Are these rigid, semirigid, or not rigid?
Prefabricated or fabricated?
Slightly more _______ than the soft cervical collar
Better what?
Use with what conditions?
Semirigid collars
Prefabricated with molded chin and occiput
Slightly more unweighting than the soft cervical collar
Better motion control
Use with minor muscle strain and as
extrication orthosis following trauma
(Know the differences between a soft collar vs semi rigid. He’s not really concerned about us knowing the differences between the Miami J and the Philadelphia)
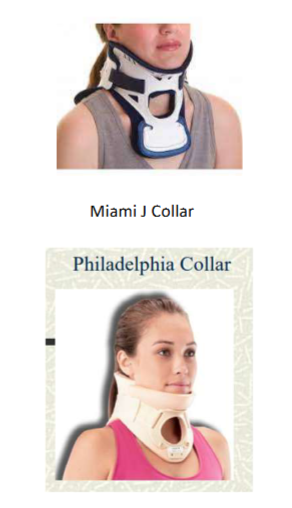
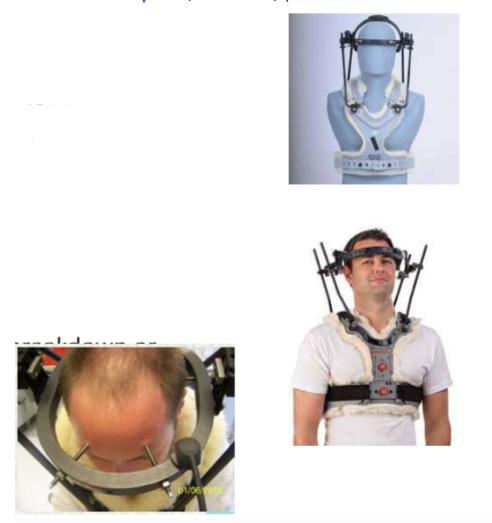
Halo vest
Describe the layout of this.
What does is immobilize?
Since its top heavy what can it cause?
Due to the pins, what does the patient have to do?
What should the patient watch out for due to the vest and pins?
When is it used?
Four posts connect anterior and posterior to chest plate. Invasive, metal ring (halo) is secured into the skull.
Immobilization of cervical and upper thoracic spine
Top heavy: can impair balance and increase fall risk so do a lot of balance and proprioceptive training like walking up and down steps or going through doorways
Need to have pin care
Need to watch for skin breakdown or irritation under the vest or at pins
used in stabilizing after spinal cord injury
Legg-Calve-Pethes disease
What is it and what is the goal if someone has this?
What orthosis and bar is good for this condition and why?
Due to loss of circulation to the femoral head (avascular necrosis) followed by period of revascularization which results in the bone being soft and vulnerable to forces. Goal to maintain the femoral head in the acetabulum during gait and control forces to avoid permanent deformity and OA
Orthosis
Scottish Rite – allows flex and extension but hip held in abduction.
Abduction bar

Clubfoot
What brace is ideal for this condition and what does it do?
When is the bracing applied?
Why is this bracing important to use for the condition?
Foot held in abducted and DF in a foot abduction brace with two shoes connected by a bar. Ponseti brace
Brace applied after clubfoot has been corrected by
manipulation, serial casting, Achilles tenotomyBracing important in preventing clubfoot relapse
(Know what type of patient would need this aka club foot patients)

Developmental hip dysplasia
What is it?
What can be expected when a baby has this condition
What is the treatment for baby under 6 months (what is used to correct it) , how does it work, and how long the treatment is?
The hip not formed well so the joint is partly or completely out of the acetabulum (shallow socket)
See baby hip make a popping or clicking sound, legs are not same length, skin folds under buttocks are not symmetrical. Typically, not painful.
Treatment: babies under 6 months is often Pavlik Harness. Has a shoulder harness attached to foot stirrups to keep legs in abducted flexed position to keep femoral head in acetabulum. Treatment lasts 6-12 weeks
(He will probably give an exam question where we have a pavlik harness, a ponseti brace, a Scottish rite, and an abduction bar. Which one would be most appropriate for the patient for whatever device it is. Straight forward)

Pressure garments
What does it help with?
What are the negative to wearing this?
Is it fabricated, pre-fabricated, or custom?
Help to minimize hypertrophic scarring (either major scar tissue issues and/or significant levels of burn)
- Pressure reduces blood flow slowing the influx of collagen
- Encourages reorientation of collagen
- Minimize pain and itching
- Provide cosmetic cover and protects against secondary
traumaCan be difficult to don and doff, Can be hot and uncomfortable
Pre-fabricated or custom

Knee joints - Axis type
What are the three types of axis? What does each type do and used for?
Axis alignment? Why is it aligned this way?
Axis Types
Single
- Designed to behave like a hinge, preventing movement in the coronal plane, providing
medial/lateral stability
- Free motion joints allow full knee flexion and extension, yet prevent hyperextension
- Recommended for genu varum and genu valgumOffset
- A single axis joint design with the axis set further posterior from the weight line than the
standard single axis joint
- Promotes maximal knee extension during WB without having to use a mechanical lock
- Recommended for patients with needs of higher levels of stabilityPolycentric (allow the axis to translate during joint rotation see fig 15.3)
- Designed to mimic the instantaneous center of rotation present in the anatomical knee
- The gliding and rolling motion emulated with polycentric is intended to reduce excessive
motion, slippage, and to provide greater comfort than conventional single axis joints
Axis alignment
Inline or posterior offset relative to the uprights (this enhances knee extension during stance by keeping GRFV anterior to the mechanical axis)
(He didn’t really say anything particularly here so just know all of it)
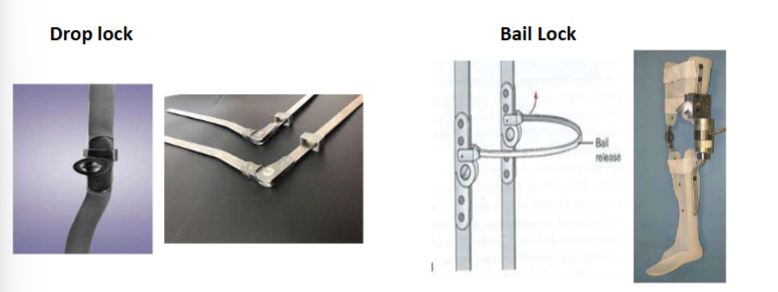
Knee joints - Knee lock types
What are the types of knee locks and what does each do?
What are adjustable locks and subtypes?
Knee Lock Types
Drop lock: (metal ring that slides down over the knee joint in extension; move up to release)
Spring-load pull rod: (spring system with control rod that can be extended to a height for convenient reach, permits easier release of locking mechanism)
Cam (Pawl) lock with Bail Release: (curved metal extends around back of knee, raising it releases lock – can use back of chair to push it up)
Adjustable locks (permit you to reduce joint ROM restrictions as rehab progresses)
• Fan lock
• Dial lock
• Ratchet lock
(Know differences between these)

Knee orthoses (KO)
Where is it enclosed on the body?
Where should you NOT attach it to?
Can be categorized as what three things?
Difference between soft and rigid knee orthoses?
Knee Orthoses (KO)
Enclose the knee joint (mid thigh to mid calf)
DO NOT ATTACH TO THE ANKLE OR HIP
Can be categorized as functional, rehabilitative or
supportive
Soft:
Elastic fabric or neoprene
Typically, over the counter prefabricated
Apply compression forces
Little biomechanical control
Rigid:
Rigid framework of double or single uprights (metal, plastic or
composite material)Articulation at knee joint that allow free flex/ext around single or
polycentric axis while restricting frontal plane movementThigh and calf bands, straps
(Know differences between soft vs rigid)

Post operative or rehabilitative KO
How long is it used for and what does it do?
When and how is it used and why?
Adjustable or non adjustable?
Usually require what type of training?
Short term use to control motion. KNEE IMMOBILIZER
Used after orthopedic surgery to protect structurally incompetent tissues from negative forces during healing
Adjustable (DIAL LOCKS). 2 metal inserts on med/lat side. Adjustable Knee ROM
Usually require gait training with crutches or a walker for safety
(Know what type of patient would be appropriate for immobilizer brace vs functional brace)

Functional KO
Are they rigid or soft? Differences between this and rehab devices?
Joints or no joints?
What does it provide support for?
What movements does it allow?
What motions does it limit? Most designs implements what counterforce system?
Rigid, they are shorter than rehab devices (extending no farther than mid-thigh and mid-calf, less bulky)
Can have joints or no joints
Provide support for ligament laxity or instability
Usually allow for free flexion/extension
Most designed to employ 3 or 4 point counterforce systems to limit excessive movements, including varus/valgus stress and knee hyperextension.
(Know what type of patient would be appropriate for immobilizer brace vs functional brace)

Swedish knee cage (Functional KO)
This brace is known as the _____ of functional knee braces.
This brace is moving or no moving parts?
How is this brace laid out?
Prevents what?
Employs what forces to where countered by what forces where?
Fabricated or prefabricated?
What does it often do that can be an issue?
The “OG” of functional knee braces
No moving parts
Anterior thigh and tibial band and a posterior band
Prevents knee from hyperextending
Employs a posterior to anterior force applied in popliteal fossa countered by anterior to posterior force at the distal thigh and proximal tibia
Prefabricated device
Often migrates down during limb use

Patellofemoral knee orthoses
Primary goal of this orthoses?
Soft or rigid? Made from what material?
What can be seen around the patella when applying this orthoses?
Primary goals of these braces are to minimize patella compression, assist in guiding patella tracking, and prevent excessive lateral shift
Most patellofemoral orthoses are soft appliances made from elastic material as a “pull-on sleeve”
May have a “C” or “O” shaped built up around the patellar window or pull straps that wrap around the lateral side of the patellar window to apply medially directed force. Helps with patella tracing.

Supportive knee orthoses
What does this provide?
When should it be used?
What is it made from?
Provides support
Indications: Patellofemoral syndrome; patellar subluxation; infra-patellar tendonitis
Made from fabrics, elastic or neoprene
Sleeves
Infra-patellar straps (support the patella and facilitate accurate tracking, dissipate tensile forces)

Off-loading (unloading) Knee orthoses KO
When is it used (what condition)?
What does it do?
What is the most common form of the condition its used for?
Goal of the orthoses?
Used with patients that have OA of the knee that affects only one compartment of the tibiofemoral joint
Reduce loads on the involved joint surfaces and may decrease pain to improve function
Most common unicompartment OA is the medial compartment of the tibiofemoral joint with a varus deformity
Goal is to apply a valgus force using 3-point counterforce system

Hip abduction brace
What is it used for? Most frequently used after?
Used post-op or with a femoral neck fracture. Frequently used following labrum repairs.

SAMPLE QUESTIONS FROM REVIEW
Which term is commonly used in orthotics which means limited motion at the joint often with indication of specific motion taking place?
The process of adding material to an FO either intrinsically or extrinsically within the rearfoot or forefoot to control excessive motion, provide support and bring the floor to the foot is called what?
Type of UE splint known for its low load prolonged stress to increase tissue is known as?
Pt presents with mild - moderate ankle and quad weakness. Pt is able to ambulate but experiences knee buckling. This happens a 1-2 times every 25 feet. What is the best orthotic to give this pt?
ANSWERS
STOP
POSTS
DYNAMIC SPLINT
GRAFO