NS Fundamentals - Skeletal Neuromuscular Junction
1/12
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
13 Terms
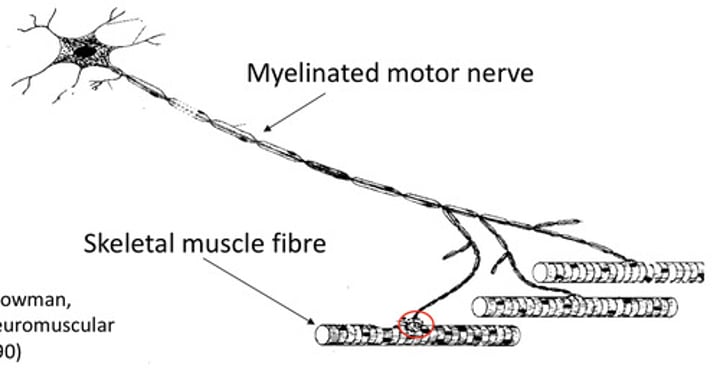
Describe a typical "motor unit".
- The motor unit consists of the motor neurone and the muscle fibres it innervates
- The motor neurone may form synapses at multiple muscle fibres/cells
- The axon of the motor neurone is myelinated for rapid neuronal transmission via saltatory conduction
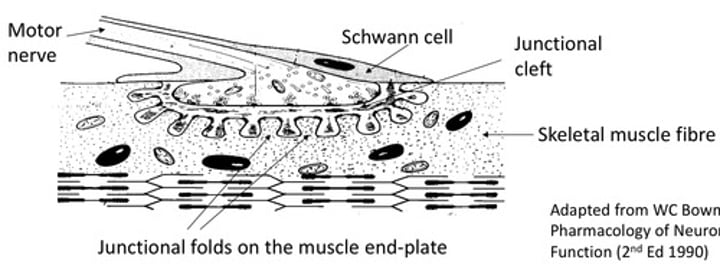
Describe the features of a neuromuscular junction.
- The motor neurone and muscle fibre forms a Junctional Clef, which is an indentation into the muscle where the two join
- There are junctional folds on the muscle end-plate that increases the surface area of the neuromuscular junction for optimal synaptic transmission
- The Junctional Cleft is closed off by Schwann's cells for constant connection to the muscle fibre (poses difficulty for drug diffusion at these sites)
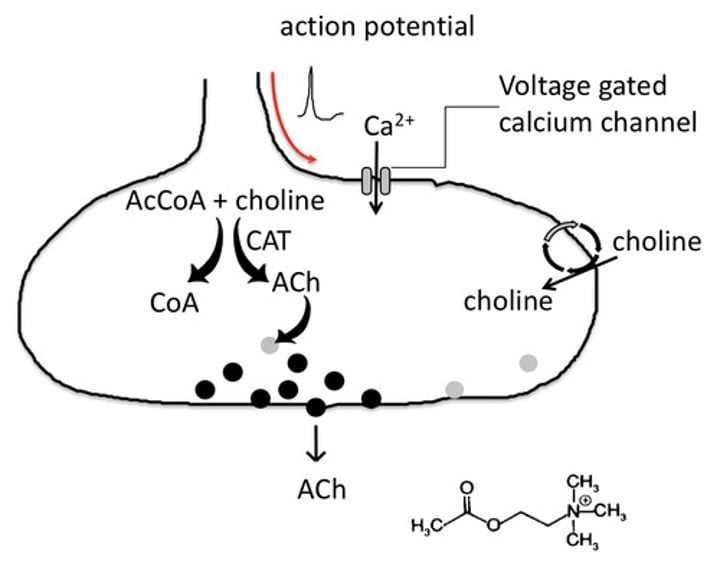
What pre-junctional events occur in neuromuscular transmission?
- Acetylcholine is synthesised from Choline and Acetyl Co-enzyme A, by the enzyme Choline Acetyl Transferase (CAT)
- Choline is taken into the nerve terminal from the extracellular space by a transporter (as it can't be synthesised)
What is Botulinum Toxin and its effects?
- It is a drug that acts of blocking the process of exocytosis for neurotransmitter
- It is only injected in extremely small amounts to site locally due to high potency mean low lethal doses
- It is mainly used in cosmetics to treat abnormally contracted muscles
What post-junctional events occur in neuromuscular junctions?
- The enzyme Acetylcholinesterase (AChE) hydrolyses acetylcholine found in the neuromuscular synaptic cleft, to prevent further synpatic transmission.
- The choline is recycled by the pre-synaptic neurone, while the acetyl is diffused away.
- Most acetylcholine is destroyed before binding to the receptor, in space of 1 millisecond, as fast, single contractions are required
What is EPP?
- This is short for End Plate Potential, and this defines the depolarisation of the muscle fibre membrane produced, following the activation of the Nicotinic Acetylcholine receptor.
What do drugs acting post-junctionally do?
- They inhibit neuromuscular transmission, and are usually reversible competitive antagonists to Nicotinic Acetylcholine receptors
- This means they have zero efficacy but high affinity, preventing acetylcholine from binding and activating the receptor
What are clinical uses of reversible competitive antagonists?
- They are used a muscle relaxants during surgery, allowing lower anaesthetic doses to be administered
- Their effects last 15-40 mins generally, but reversible by the drug Neostigmine, and they cause patients to be artificially ventilated
What is an example of a depolarising muscle relaxant?
- Suxamethonium (aka Succinylcholine) is an agonist of the Nicotinic Acetylcholine receptor and acts very quickly
- Unlike Acetylcholine, Suxamethonium is not broken down by Acetylcholineesterase (due to larger size), leading to prolonged depolarisation
- Voltage Gated Na+ channels become "inactivated" during repolarisation, only reactivating once resting potential is reached
Explain the mechanism of action of Suxamethonium.
- Normally, the EPP produced by Acetylcholine leads to opening of the channels transiently, before closing into an inactivated state
- Once in an inactivated state, the membrane potential must cycle back to resting potential for the channel to reach their resting state also.
- Due to Acetylcholinesterase, action potentials are short lived, so voltage gated Na+ channels recover to resting state very quickly
- Suxamethonium prolongs the depolarisation by trapping the Na+ channels in an inactivated state, so another action potential cannot be fired, causing an initial contraction before continuous relaxation
Why may Suxamethonium be used clinically?
- It has a rapid onset of action, producing short-term muscle relaxation within 60 seconds of intravenous injection
- It is broken down in the blood plasma by butyryl-cholinesterase, so effects last for a few minutes (patients with deficiency in this enzyme have effects that lasts hours)
What are Anticholinesterase drugs?
- They prevent the breakdown of acetylcholine, leading to high concentration in the neuromuscular junction
- An example is Neostigmine which is used clinically to reverse effects of reversible, competitive antagonists, but not able to reverse effects of Suxamethonium
What is Myasthenia Gravis?
- This is an auto-immune condition characterised by neuromuscular weakness, caused by antibodies targeting alpha-subunits on nicotinic acetylcholine receptors
- Anticholinesterase drugs (like Neostigmine) increase acetylcholine concentration in the synapse, reversing the effects of Myasthenia Gravis