Physical Changes
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
35 Terms
vision - primary aging characteristics
decrease in amount of light passing through (cornea, lens thickening, less flexible)
increased sensitivity to glare
light/dark adaptation declines (Miosis)
lens adaptation declines (presbyopia)
Miosis (primary vision aging)
abnormally constricted pupils, limiting light that comes in too much
Presbyopia (primary vision aging)
decline in ability to focus on nearby objects, time to change focuses increases
→ age-related farsightedness
secondary aging vision changes
cataracts
age-related macular degeneration (AMD)
glaucoma
Cataracts (secondary vision aging)
opaque spots covering/clouding the lens
caused by protein (in lens) breakdown, prolonged UV exposure
leading cause of blindness worldwide
Age-related macular degeneration (AMD) (secondary vision aging)
progressive loss of central vision
caused by accumulation of protein deposit or blood/fluid leak in macula
affects central vision, fovea location (responsible for visual acuity, vivid colour processing)
wet vs dry AMD
dry AMD → protein deposits
wet AMD → protein deposits w/ blood/fluid leak in macula (extension of the disorder)
Glaucoma (secondary vision aging)
damage to optic nerve
high pressure in eyes
loss of peripheral vision
subtle changes to vision, not initially apparent and not noticed until it becomes quite bad
inner ear damage leads to
balance issues
→ fluid in semicircular canals moves around as body/head move
primary aging hearing changes
presbycusis
hearing in noise
Presbycusis (primary hearing aging)
gradual age-related hearing loss
caused by damage/wear to inner ear over time
hearing in noise also affected
functional hearing (hearing sentences/words in noisy environ)
pure tone audiometry
what is Hearing in noise
functional hearing (hearing sentences/words in noisy environ)
typical audiogram
louder volume needed to hear higher frequencies
secondary aging - hearing
as pure tone hearing decreases, so does functional hearing
primary balance aging
vestibular system
proprioception
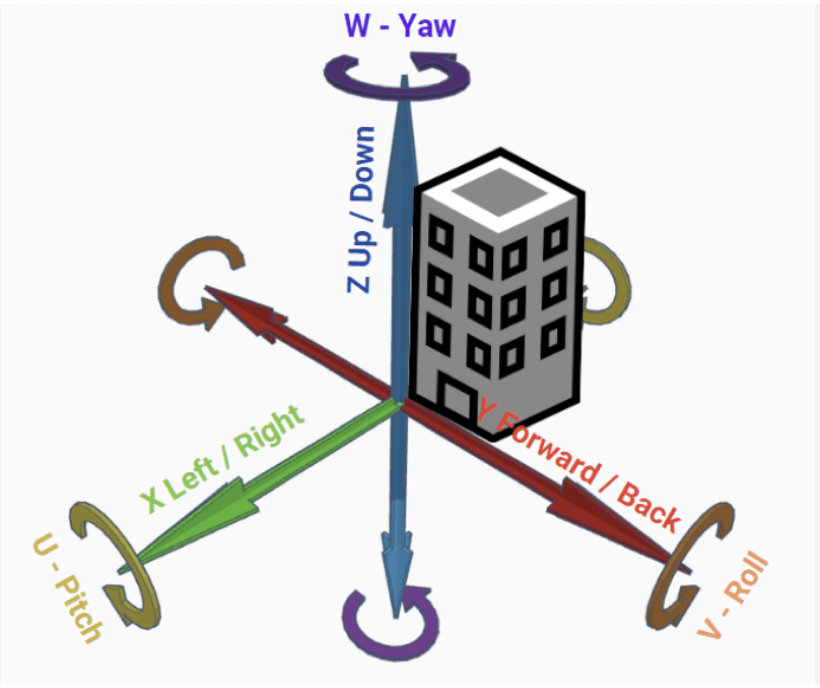
primary balance aging - vestibular system
it declines with age, semicircular canals process movement in 6 degrees of freedom
vest. syst. helps us orient in space & maintain balance
primary aging balance - proprioception
declines with age, perception of joint/body movement in 3D space
vestibular system works with this
secondary balance aging
vertigo/dizziness
secondary balance aging (vertigo/dizziness)
sensation of movement that makes one uneasy
→ multi-factoral causes, puts balance in jeopardy, increase in risk of falls
primary/secondary muscle aging
sarcopenia
primary/secondary muscle aging - sarcopenia
progressive age-related loss of muscle tissue, strength
multi-fact causes (genetic, lifestyle, hormonal) - increased risk of falls, physical disability
prevention → exercise, strength/resistance training
primary joint aging (ligaments)
become less elastic overtime → thick, short, flexible, fibrous connective tissue that connects bones/cartilage, holds joints tgt
prone to damage/tearing
secondary joint aging
osteoarthritis
rheumatoid arthritis
secondary joint aging - osteoarthritis
degeneration of cartilage (cushion for bones) → bone-on-bone contact
inc risk with age, injury, genetics
symp: pain, tender, stiff, swell, loss flexibility
secondary joint aging - rheumatoid arthritis
autoimmune condition
degeneration of cartilage, inflammation around joints
diff pathology/causes than osteo
secondary aging bones - osteoporosis
change in amount of bones, decr quality of tissue
low bone mass (quantity)
deterioration of bone tissue (quality)
low bone mineral density
osteoporosis in women
50% will devel, 1/3 will break a bone bc of it
causes:
less bone mass
low levels of estrogen
greater rate of bone density decreases
insufficient dietary calcium
less weight-bearing activities in devel
what hormone directly impacts intracellular processes that regulate bone/muscle health (and deficiency incr risk for osteoporosis and sarcopenia)
estrogen
osteoporosis in men
1/5 will break a bone
37% who suffer hip fracture will die within 1 yr
general risk factors for osteoporosis
genetic
previous falls and broken bones
smoking
drinking alc >3/day
certain medication
where you live
LBMD in developed countries w/higher pop
prevention of osteoporosis
weight bearing and muscle strengthening exercise
avoid smoking/alc
at 50+ yrs → get assessed
at 65+ yrs → regularly assessed
calcium and vitamin D supplements/intake levels
4 imp (individual) risk factors that can lead to falls
weakness, balance deficit, gait deficit, visual deficit
fear of falling is associated with ___ activity
decreased/less
fear of falling is a ___ problem, why
cyclical problem
→ ppl fear falling, don’t do activities they could fall, not exercising increases risk of falls
fear of falling & sensory impairment/difficulties
FOF higher proportion of sensory difficulties
ppl with FOF report difficulties walking 2km, 3 yrs later
FOF decreased likelihood of exercise, which increases chance of falling