Week 8 (Physiotherapy for the pregnant and post-natal client)
1/34
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
35 Terms
Cardiovascular adaptations during pregnancy
- ↑ blood volume
- ↑ HR & CO
- ↓ systemic vascular resistance (can cause ↓ BP)
Respiratory adaptations during pregnancy
- ↓ thoracic cage expansion & high diaphragm (ribs have expanded & diaphragm lifted due to presence of baby)
- ↓ lung volumes
- ↓ oxygen availability for prolonged strenuous exercise
Biomechanical adaptations during pregnancy
- Weight gain & expanding uterus
- Relaxin: ↑ flexibility & joint mobility
- Shift in COG
- Lumbar lordosis & thoracic kyphosis
- Gait changes: shorter & wider stance, ↑ double support phase
- ↓ balance (↑ falls risk)
causes of PGP and LBP
multifactorial
secondary to postural changes
load on ligaments
hormonal changes (Relaxin)
signs and symptoms of pelvic girdle pain & LBP in pregnancy
- Pelvic pain (front or back)
- One-sided / bilateral or moving
- May have referred pain to the buttock or posterior leg
- Aggravating factors include lying supine (due to load on sacroiliac ligaments), STS, hip abduction, or single leg movements (e.g. stairs)
management of PGP and LBP
- Core stabilisation (i.e. TA activation) with exercise (especially LL): Can ↓ LBP, sick leave & improve functional disability
- note: whole body active exercise required not just core stability (major muscles of LL to provide support for increased load)
- SIJ stability belt
- Advice on lumbopelvic posture, especially in driving, lifting & other ADLs
- exercise for posture and reduction of thoracic kyphosis (seated rows, bent over rows)
- Gait aid (if severe pain in SLS)
- Education: most will resolve spontaneously at birth
- Limited evidence: acupuncture, osteomanual therapy, craniosacral therapy
Abdominal diastasis
Midline separation of rectus abdominis along linea alba
associated with weaker abdominal muscles, predisposition to LBP & PGP, pelvic organ prolapse
Assessment for DRAM
- Patient in crook lying, performing a mini-sit up (pt lifts head and shoulders off plinth)
- Distance between borders of rectus abdominis is measured 2cm above and below, and at level of umbilicus
- > 2.3 - 3.3cm is significant
Management of abdominal diastasis
- Abdominal & PFMT exercises commonly used clinically (for return to functional strength)
- note: abdominal exercises must train ALL muscles not just TA and IO (prevent widening of gap as opposed to narrowing)
- May use abdominal compression stockings in first 6 - 12/52
- may require surgical management if conservative not effective
medical conditions to be aware of during pregnancy
gestational diabetes (exercise can help)
cervical incompetence (risk of premature labour)
antepartum haemorrhage
placental abruption
placenta praevia
intrauterine growth restriction
pre-eclampsia/eclampsia (pregnancy induced hypertension)
exercise guidelines during pregnancy
include:
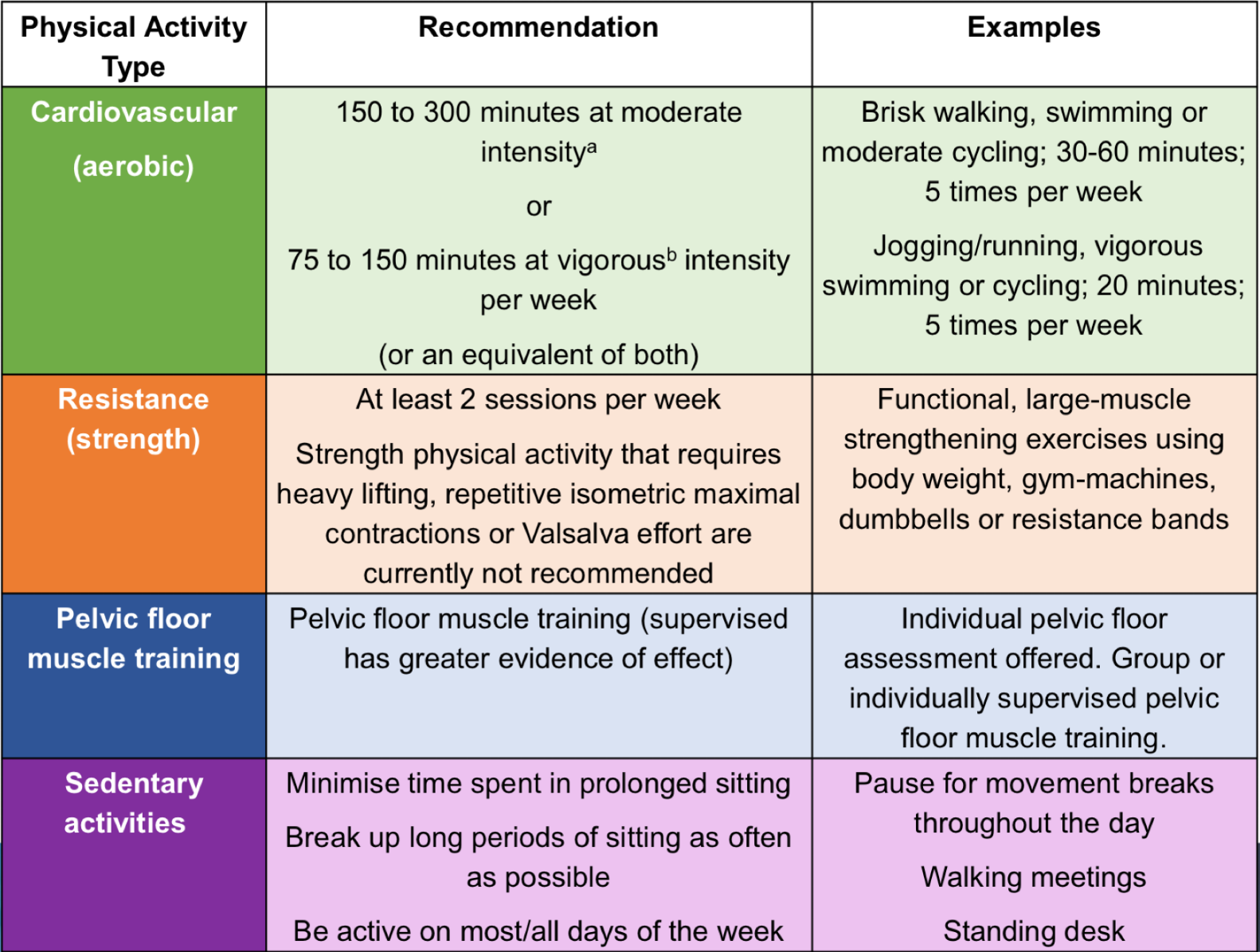
defining physical activity intensity in pregnancy
moderate intensity: HR 125-146bpm in those under 29, 121-141bpm in those over 30
vigorous intensity: HR 147-169bpm in those under 29, 142-162 in those over 30
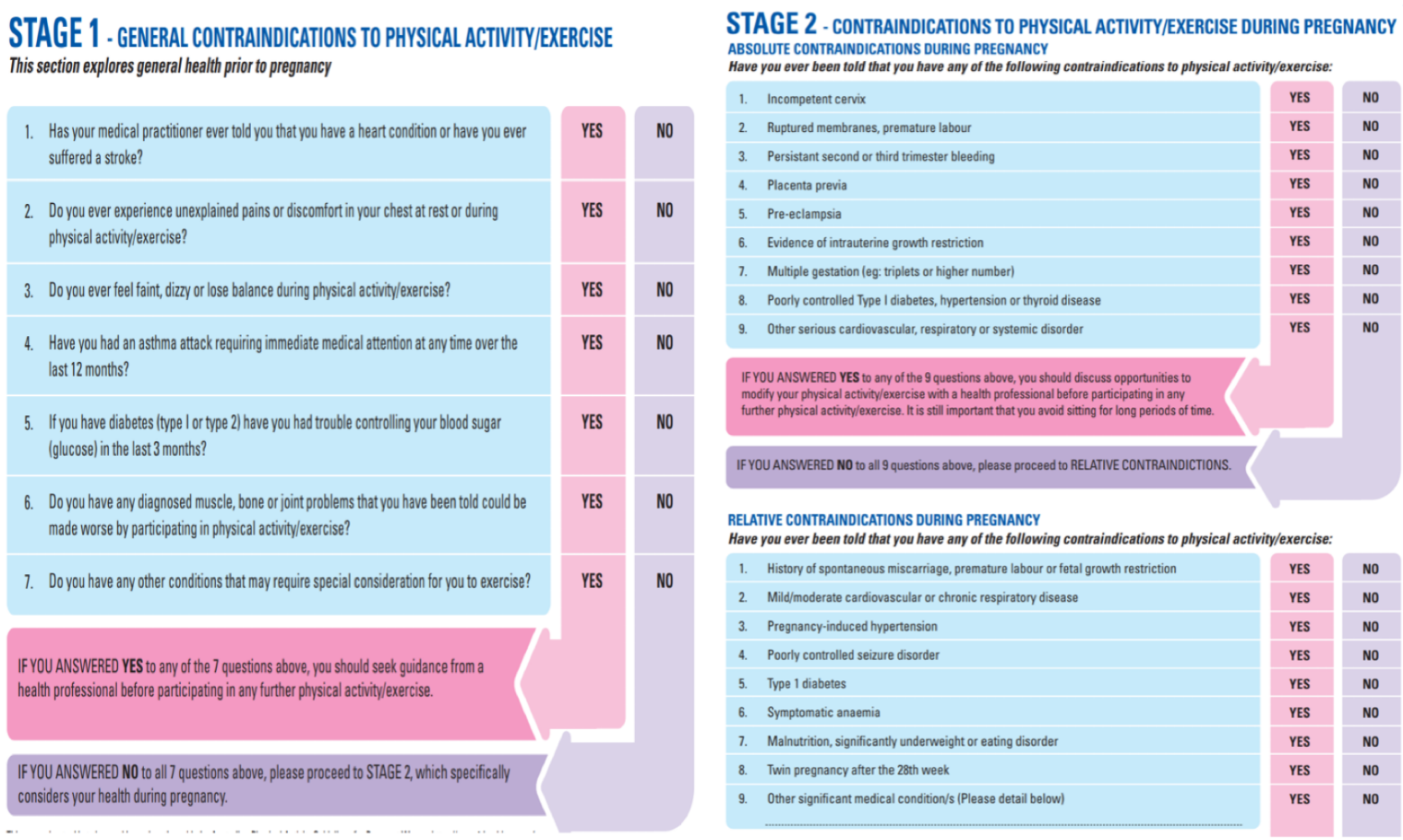
Absolute contraindications for exercise in pregnancy
Can perform ADLs, but may not tolerate exercises
- Poorly controlled T1DM, HT or thyroid disease
- Cervical incompetence (thin / weakened cervix)
- Pre-eclampsia (pregnancy induced hypertension)
- Persistent 2nd / 3rd trimester bleeding
- Placental abruption (separation of placenta before birth)
- Placenta praevia (low placenta, close to or over cervix)
- Intrauterine growth restrictions
Relative contraindications for exercise in pregnant women
- Gestational HT
- Cardiovascular (e.g. anaemia) / chronic respiratory diseases
- T1DM
- Poorly controlled seizure disorder
- Recurring pregnancy loss
- History of spontaneous miscarriage, preterm birth or foetal growth restrictions
Exercise guidelines for pregnant women
- Should all be physically active in absence of contraindications (which they should be aware of)
- 150 - 300/60 moderate intensity PA or 75 - 150/60 vigorous intensity PA weekly (consult OB for risks)
- Appropriate intensity: "Talk test" / Borg 12 - 14
- 2x strength training weekly
- Minimising prolonged sitting periods
Benefits of exercise in pregnancy
- ↑ cardiovascular fitness, muscle strength & endurance
- ↓ risk of gestational diabetes & pre-eclampsia
- ↓ excess weight gain, helping with body image
- Improved pelvic floor function
- May help with management of LBP & PGP?
screening tool for exercise during pregnancy
ESSA
Activities to avoid in pregnancy
- exercising in supine (due to compression of inferior vena cava)
- Contact sports / risk of falling or trauma (e.g. footy, water skiing), though can participate in non-contact drills
- Hot, humid or if febrile
- Skydiving / scuba diving
- Valsalva manoeuvre (heavy lifting)
- Ballistic / jerky movements, or taking joints to end of range
Stage 1 of labour
From onset of contractions to full (10cm) cervix dilation
baby moves down into pelvis
Stage 2 of labour
From full cervix dilation to baby delivery
Contractions are less frequent but stronger
Stage 3 of labour
From baby delivery to placenta delivery
Differences between Braxton-Hicks contractures and labour contractures
Braxton Hicks: irregular, painless contractions
Labour: painful and regular (interval shortening) contractions
positioning during labour
stage 1: upright posture, pelvis open
stage 2: posterior pelvis not fixed (not supine)
stage 3: position most comfortable for mother
Pain relief during labour (coping strategies)
- Positions of ease / companionship
- Mobility, breathing
- Relaxation / music / acupuncture
- Massage / warm baths or showers
- Epidural / opiates (Entonox / Pethidine)
conservative pain relief during labour
TENS
acupuncture
hypnosis
pharmacological pain relief during labour
entonox (NO and O2)
pethidine
epidural
levator ani muscle (LAM) defect
due to stretching of LAM to 3x of its normal length
partial or full avulsion from origin near pubic symphysis (may also cause damage to pudendal nerve)
risk factors for LAM defect
large baby (>4kg)
forceps delivery
large fetal head circumference
prolonged second stage labour
3rd/4th degree perineal tear/sphincter rupture
anal sphincter tear
damage to perineal body and anal sphincter
risk factors for anal sphincter tear
episiotomy
instrumental deliveries
posterior presentation
associated with anal incontinence
Postnatal physiotherapy (on ward)
- Postnatal exercise classes
- Assessment of DRAM and PFM contraction
- PFMT exercise prescription
- Advice on posture, back care, breastfeeding positions and warning signs of pelvic floor dysfunction
- Wound care for vaginal & caesarean delivery
- Mastitis management
Postnatal physiotherapy (6 weeks-6 months)
assessment of symptoms of PFD
assess PFM (Strength, endurance, correct contraction etc)
return to sport/exercise advice
management of mastitis
exercise advice
post-natal pelvic floor recovery timeline
includes:
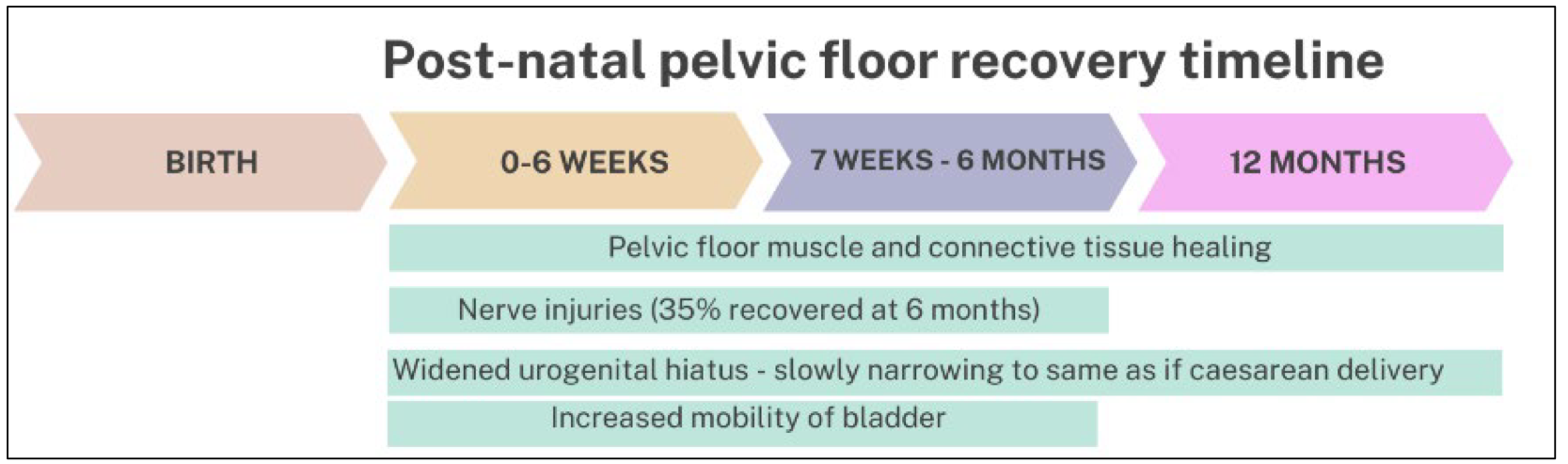
Return to sport / exercise in postnatal periods
0 - 6/52:
- Gentle walking as tolerated (+/- static cycling if able)
- Focus on recovery & PFMT
6/52 +:
- Gradual ↑ in exercise levels (e.g. resistance) to prenatal levels
- Refer to PF physio for return to high-impact sports
- Dependent on PFD & DRAM
considerations for return to sport/exercise
pelvic floor muscle function and passive tissue integrity
pregnancy/birth related complications
exercise load