02 - Respiratory Mechanics III&IV
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
28 Terms
breathing pressure changes in spontaneous breathing vs positive pressure ventilation
spontaneous breathing
inspiration → intra-alveolar pressure decreases and then increases to 0, intrapleural decreases to below -5
expiration → intra-alveolar pressure increases then decreases to 0, intrapleural increases to -5
parabolic curve in intra-alveolar pressure due to recoil of lungs
decreased intrapleural pressure pulls on lungs and lowers intra-alveolar pressure to pull air in
positive pressure ventilation
inspiration → intra-alveolar pressure increase, intrapleural pressure increase
expiration → intra-alveolar pressure rapidly decreases, intrapleural pressure rapidly decreases
generates force by raising intra-alveolar pressure
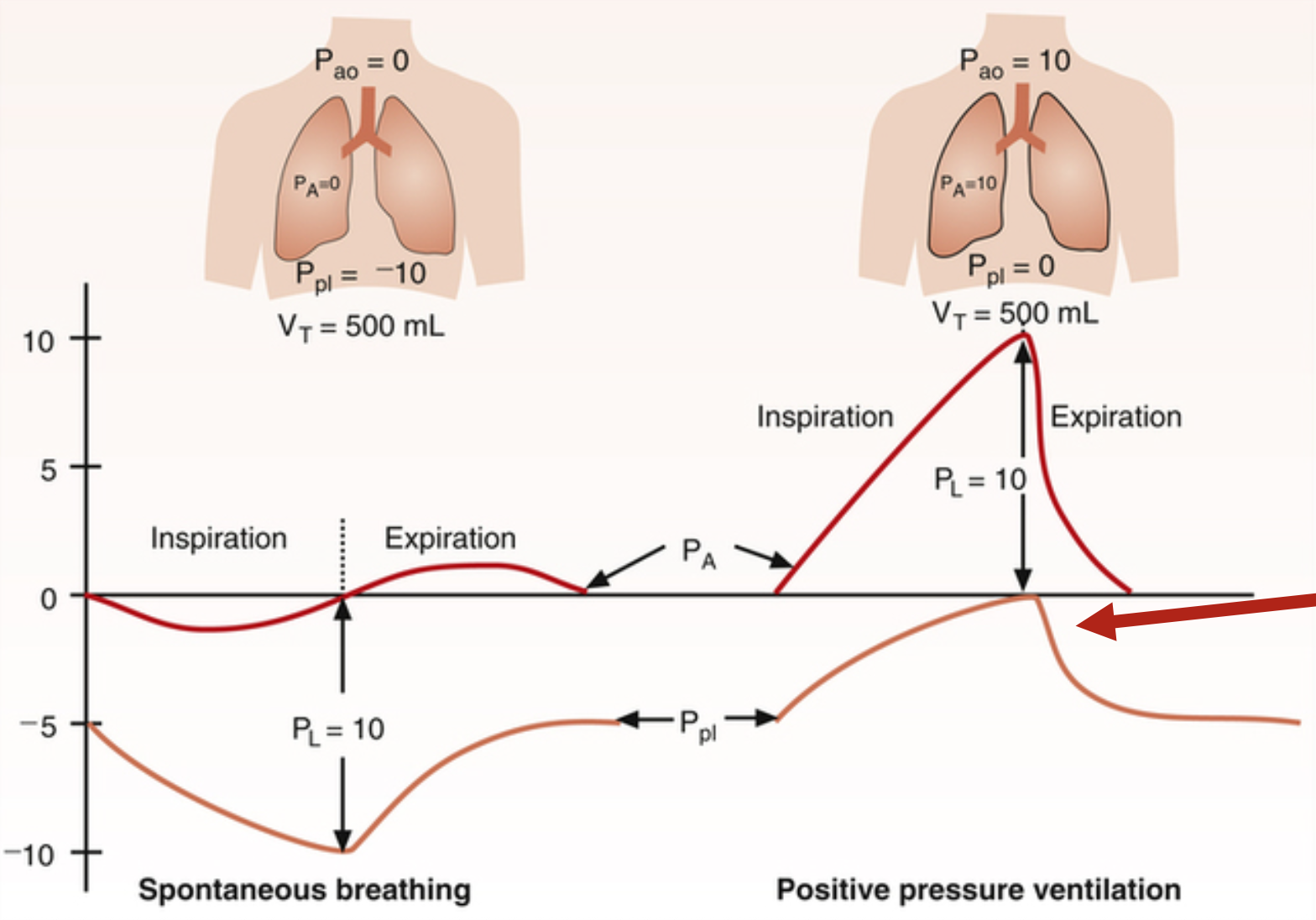
positive intrapleural pressure
during normal respiratory cycle, intrapleural pressure fluctuates solely in the negative range
intrapleural pressure can become positive under special circumstances:
inspiration → positive pressure respiration, where outward movement of lungs compresses intrapleural space to raise its pressure
expiration → active respiration, where respiratory muscles compress intrapleural space so lungs can return to pre-inspiratory level more quickly and forcefully
assisted control mode ventilation (ACMV)
form of positive pressure respiration or mechanical breathing where inspiratory cycle initiated by patient, or automatically if no signal is detected within a specified time window
positive end expiratory pressure (PEEP)
form of positive pressure respiration or mechanical breathing where lung is kept at a larger volume by not allowing intra-alveolar pressure to return to 0 at the end of expiration
starts at positive pressure, which distends conducting airway and decreases resistance to keep airway open with low resistance
lung volume is elevated at end of expiration
functional residual capacity is increased, with larger lung volume at end of expiration
positive pressure ventilation (PPV)
aka mechanical breathing
three forms → assisted control mode ventilation (ACMV), positive end expiratory pressure (PEEP), continuous positive airway pressure (CPAP)
ideally, trans-alveolar pressure should be low as possible during mechanical respiration to minimize development of ventilator-induced lung injury
less than 28-30 cmH2O
if plateau pressure is kept at 28-30 cmH2O, trans-alveolar pressure can never exceed this level
air trapping in mechanical ventilation
air trapping or auto-PEEP occurs when a new breath begins before the lungs have fully expired the previous one, trapping air in the lungs
leads to increased pressure and over-inflation of the lungs
flow never returns to baseline due to increased pressure and resistance
continuous positive airway pressure (CPAP)
form of positive pressure respiration or mechanical breathing that is not a true support-mode of ventilation
breathing is spontaneous but via a circuit that is pressurized
used to maintain airway size and prevent respiratory muscle atrophy
raises pressure in environment to distend airways and start ventilation at a higher pressure, making it easier to breathe
obstructive sleep apnea
occurs due to critical negative pressure during inspiration
due to sleep reducing tone of muscles of oropharynx, obesity reducing airway size, alcohol depressing muscle activity, and increased nasopharynx resistance that reduces downstream pressure
clinical consequences → cognitive and behavioral deficits like excessive daytime sleepiness, mood swings, poor decision making
major risk factor for cardiovascular diseases like endothelial dysfunction, hypertension, arrhythmias, ventricular hypertrophy
pressure change with forced expiration
transmural pressure is responsible for lung movement and is the difference between intra-alveolar pressure and intrapleural pressure
pre-inspiration → IAP and atmospheric pressure are equal
during inspiration → lowered IPP pulls alveolus open to increase alveolus volume and lower IAP, creating a gradient of low pressure in alveolus compared to atmosphere
end-inspiration → intrapleural pressure remains negative, and air rushes into alveolus to approach atmospheric pressure
forced expiration → increased IPP due to thoracic muscle contraction compresses on lungs and increases IAP to push air out of lungs, but alveolar elastic recoil opposes dynamic compression from lung collapse
expiration is effort-dependent at high lung volumes and effort-independent at low lung volumes
regional variation in intrapleural pressure
due to gravity, intrapleural pressure varies with the position of the thorax
apex → intrapleural volume is higher due to stretch from gravity pulling lung down, where change in volume at apex when taking a breath is less than change in volume at base due to greater distension and being stiffer at apex
base → intrapleural tension is less due to gravity pulling lung down, creating intrapleural pressure gradient from apex to base
less IPP at apex, more IPP at base of thoracic cavity
lung compliance on alveolar ventilation
due to gravity, there is more IPP at the base of thoracic cavity than at the apex
alveoli at apex are more distended at apex than at the base, causing respiratory cycle to start higher on the compliance curve
change in volume with each breath is greater at the base because they are more compliant
ventilation-perfusion ratio (V/Q)
since blood flow is affected more by gravitational forces than air flow, the V/Q ratio increases as one moves up the lung towards the apex
gas exchange is greater at the apex of the lung than the base
pneumothorax
perforation of the chest wall or lung that causes air to move into the intrapleural space because IPP is negative
presence of air in the intrapleural space breaks the liquid seal that attaches the lungs to the best wall, causing that region of the lung to collapse while chest wall expands at the same time
if volume of air in intrapleural space is small, it will be absorbed into venous blood
if volume of air in intrapleural space is large, it must be drained using a chest tube
traumatic or spontaneous
traumatic pneumothorax
wound to chest moves air from environment to IPS
rupture of alveolus by barotrauma moves air from intra-alveolar space to IPS
spontaneous pneumothorax
spontaneous rupture of alveolus moves air from intra-alveolar space to IPS
occurs mostly at apex where more negative IPP is suspected of imposing large stress on alveolar wall
flaps of ruptured wall usually reseal and limit volume of air that accumulates
leads to tension pneumothorax → lung collapse due to air accumulation, compromising both gas exchange and cardiac mechanics
lung elasticity
elasticity resists distortion, where elastic tissues return to its original shape after having been deformed
elasticity = P / V = 1 / compliance
tells how “stiff” a lung is
more elastic = more stiff = more work to get a set volume
work of breathing = P x V
lung compliance
elastance is non-linear
P-V relationship for normal lung → fall in IPP is required to obtain a change in lung volume
at small starting volume, a small change in pressure elicits large volume change
slope of the curve (V/P) → measure of compliance, where compliance is inverse of elasticity
elastic limit is reached at higher volumes, where more stretch makes it harder to stretch even more
P-V curve is non-linear and becomes flat at high expanding pressures
compliance in diseased lungs
affects work of breathing, functional residual capacity, and expiration
emphysema → damage to alveoli, causing more compliant and non-elastic lungs
obstructive disease
very small pressure changes cause large volume changes
fibrosis → scarring of lung, causing less compliant and more elastic lungs
restrictive disease that makes lung stiff
large pressure changes cause small volume changes
surfactant
reduces surface tension to increase lung compliance and greatly reduce work of respiration by sitting between water molecules at air-water interface to disrupt cohesive forces of water
surface tension develops at air-water interface due to water particles interacting with air and pulling in to cause lung collapse
surfactant normalizes surface tension to prevent lung collapse
in absence → surface tension of film lining inside of alveolus is at a high constant
P = 2 ST / r
the smaller the radius, the greater the pressure
small alveoli would inflate larger alveoli if connected
in presence → lung compliance is increased because lung stability is promoted
no inter-alveolar pressure gradient
pressure of small alveoli and large alveoli are equal
compliance at air-water interface
it takes more work to inflate a lung with air than a lung with saline
air forms surface tension when in contact with water
effect of surface tension is less with surfactant
water-water interaction counteracts itself, so there is no developed surface tension
respiratory distress syndrome (RDS) of newborns
infants with respiratory distress syndrome (RDS) have high surface tension that shows little variation in surface tension with area
lungs are very elastic and difficult to inflate
premature birth and maternal diabetes are risk factors
gestational age of 34 weeks divides incidence/mortality from disorder-free
interdependence → alveoli share septa and do not exist as independent units
effects on functional residual capacity (FRC)
functional residual capacity is the volume of air remaining in lungs after passive expiration, achieved when respiratory muscles are relaxed and inward recoil of lungs is balanced by outward elastic recoil of thorax
elastic properties of lungs and chest wall determines FRC
elastic lungs (fibrosis) → FRC is decreased and patient appears sunken-chested due to balance happening at less stretch of lungs
non-elastic lungs (emphysema) → FRC is increased due to narrowed airway, where there is less flow out of lungs that results in air trapping
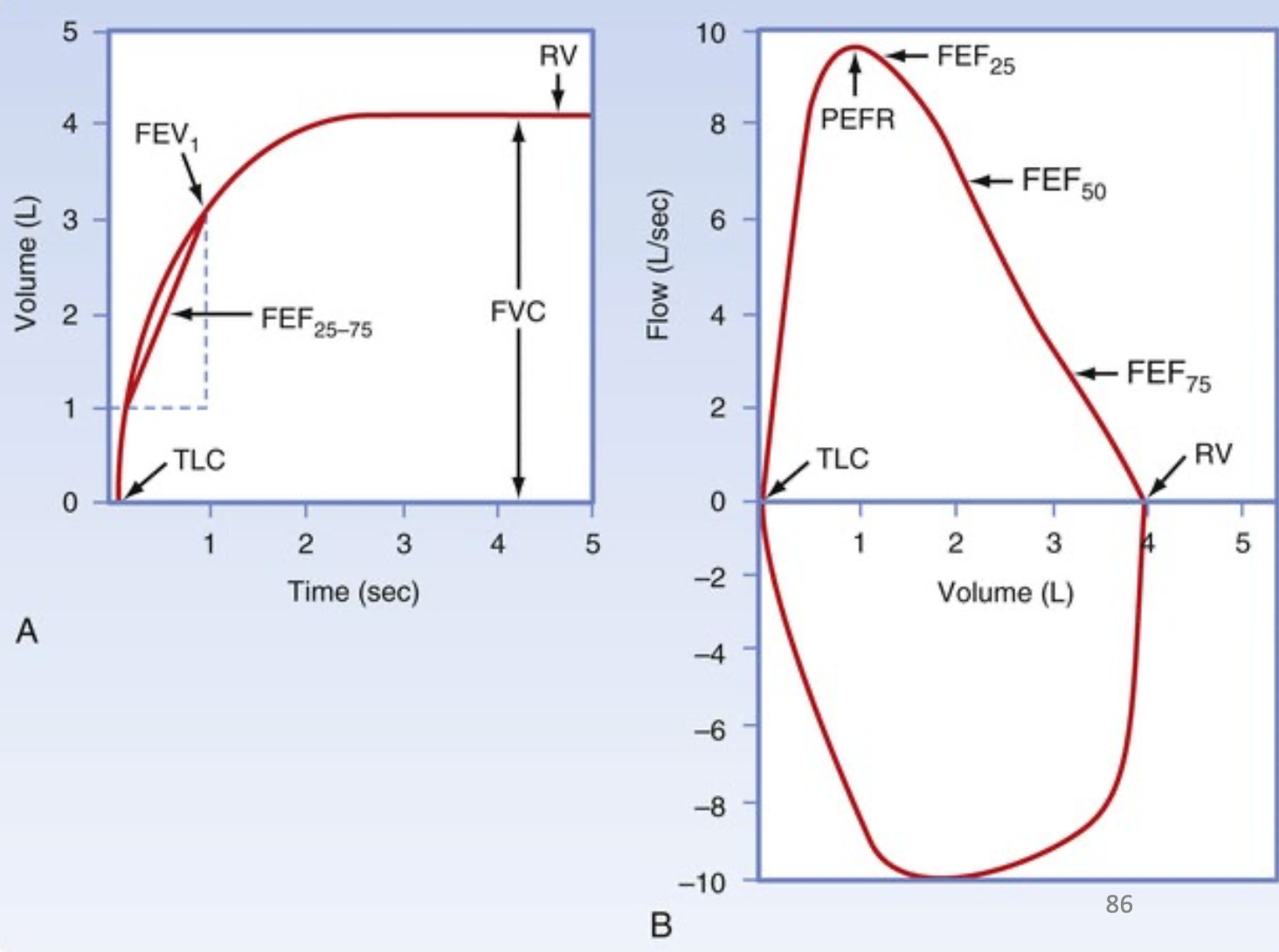
pulmonary function tests
pulmonary function tests should be compared for age and gender
vital capacity (VC) or forced vital capacity (FVC) → maximum volume of air that individual can move in single breath as quickly and forcefully as possible
forced expiratory volume1sec (FEV1sec) → volume of air exhaled in first second of FVC maneuver
normal ratio of FEV1sec to FVC → value of 80% when IPP becomes positive and airways are compressed and effort-independent
peak expiratory flow rate (PEF) → maximum flow rate achieved during FVC
forced expiratory volume25-75 (FEV25-75) → volume of air exhaled in mid-portion of FVC, between 25-75% of VC exhaled
flow-time and flow-volume relationship
flow time curve→ forced vital capacity (FVC), FEV1sec, FEF25-75
shows flow change over time during each breath
flow-volume loop → shows peak expiration flow (PEF) and measures forced vital capacity (FVC), developed from total lung capacity (TLC) to residual volume (RV)
shape of loop reveals lung problems
obstructive lung → lung volume is big because it is stretched at rest
restrictive lung → lung volume is lower due to its elasticity, with higher flow rate because lungs don’t collapse
obstructive pulmonary disease
characterized by increase in airway resistance, and is measured as a decrease in expiratory flow rates
chronic bronchitis → hypertrophied smooth muscle and muscle glands with increased mucus secretions, leading to narrow airways
asthma → hyperreactive airways and inflammation, leading to narrow airways
emphysema → loss of tissue elasticity and loss of support for small airways, leading to easily distorted airways
results in reduced vital capacity → FEV1sec is 50%, when normal is 80%
flow-volume relationship in obstructive diseases
flow-volume loop may begin and end at abnormally high lung volumes and expiratory flow rate is lower than normal, but inspiratory flow rate remains relatively normal
pulmonary function tests
FVC → decreased or same
FEV1sec → decreased
FEV1sec / FVC → decreased
FEF25-75 → decreased
lung volumes
FRC → increased (due to increased resistance that traps air in lungs from previous cycle)
RV → increased or normal
TLC → increased or normal
restrictive lung disease
characterized by an increase in elasticity that is measured as a decrease in all lung volumes
respiratory distress syndrome of the newborn
fibrotic lung disease
pulmonary vascular congestion (congestive heart failure)
pulmonary edema (ARDS, pneumonia)
flow-volume relationship in restrictive diseases
flow-volume loop begins and ends at unusually small lung volumes, where expiratory flow rates in restrictive disease is greater than normal
pulmonary function tests
FVC → decreased
FEV1sec → decreased
FEV1sec / FVC → increased or normal
FEF25-75 → increased or normal
lung volumes
FRC → decreased (due to inability of lung to expand normally)
RV → decreased
TLC → decreased