CH 10- muscle tissue
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
105 Terms
function of muscular system
movement
generate heat
venous return
smooth muscle function
maintain blood pressure
movement within visceral organs encourage transport
cardiac muscle function
pump blood throughout the body
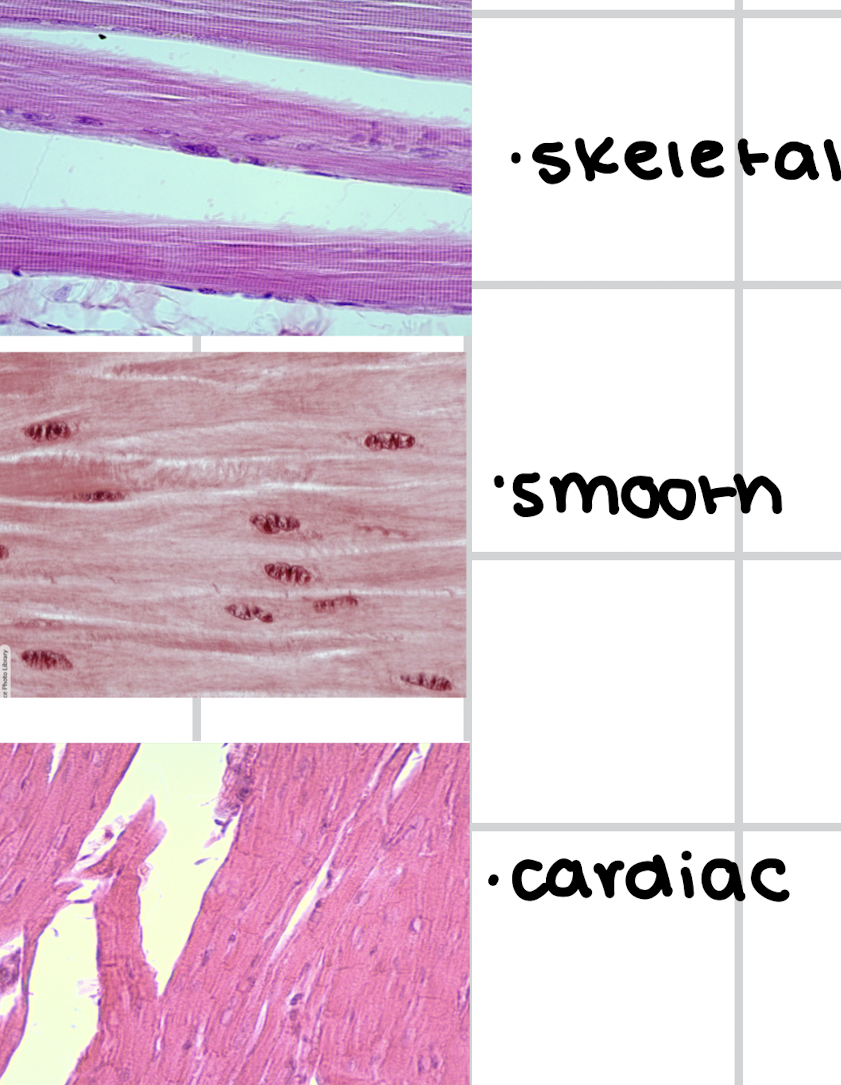
muscle tissue types
smooth
cardiac
skeletal
all muscle tissue characteristics
excitability
contractility
elasticity
extensibility
contractility
muscle contrast to create force by shortening when actin protein pulled by myosin protein
extensibility
muscle can stretch/extend beyond
excitability
muscle need to “depolarize”
undergo change of electrical state of membrane
send electrical wave down membrane
action potential
send electrical wave down membrane
elasticity
muscle can recoil to original length
all muscles require what to contract
calcium
all muscles require what to relax
ATP
cardiac cells
branched and joined by intercalated disc
gap junction allows calcium flow rapidly across cells for entire heart depolarize as one
fiber arrangement skeletal
actin/myosin arranged in parallel bundles
overlapping pattern make it appear stripes
sacromeres
actin and myosin arranged in parallel bundles
striation
overlapping pattern; stripe
epimysium
wrap entire muscle
hold fascicles together and separate muscle from other body structure
muscles nuclei
smooth: uni-nucleated
skeletal: multi-nucleated
cardiac: uni-nucleated
tendon
collagen of 3 Mysia layer melt into collagen of tendon
collagen tendon meld into collagen of periosteum
fascia
connective tissue sheets beneath skin
help anchor and separate muscle
skeletal muscle
muscle tissue proper
epimysium
perimysium
endomysium
muscle tissue proper
delicate and must be protected/separate by connective tissue wrapping
fiber arrangement cardiac
striation similar to skeletal
fiber arrangement smooth
actin/myosin criss-cross (smooth appearance)
aponeurosis
some muscles connect to broad, flat tendons instead directly to bone
embryonic development
tiny, indv myoblast fuse together to form one long component cell for contraction
nuclei remain; muscle fiber is multi-nucleated
perimysium
separate muscle fiber into bundles (fascicles)
fascicles
separate muscle fiber into bundles
endomysium
surround each indv muscle fiber for protection and integrity
sarcolemma
cell membrane of muscle cell
sacroplasm
cytoplasm of muscle cell
sarcoplasmic reticulum
endoplasmic reticulum of muscle cell
store, release, retrieve calcium ions for muscle contraction
sarcomere
functional contractile unit of muscle cell
sarcomere structure
span from one Z disc to next
Z disc
zigzag line that attach actin (thin) filament
A band
dark stripe
actin-myosin overlapped
M line
middle sarcomere
line attach myosin (thick) filament
I band
light color
thin actin
H zone
only myosin
NO overlap of actin
action potential
electrical signal that travel across membrane as wave
70mV
membrane potential
electrical gradient (voltage) across cell membrane
70mV
what does a muscle to contract need to be
excited
stimulate to fire an action potential
neuromuscular junction NMJ
nerve/skeletal muscle to contract
release acetylcholine (ACh)
T-tubules
invagination of cell membrane that connect to sarcoplasmic reticulum
pass action potential all around myofibrils
terminal cisterna
portion of SR; join T-tubules
motor neuron
nerve that originate in spinal cord or brain stem to give signal to muscle
acetylcholine
ACh
diffuse across synaptic cleft
bind to receptor on motor endplate of muscle cell
synaptic cleft
space between nerve/muscle
voltage-gated sodium channel
depolarization triggers it
open along membrane
spread action potential to muscle
ATP in contraction
creatine phosphate
glycolysis
aerobic respiration
triad
TC: terminal cisternae
TT: t-tubules
1 TC + 1 TT 1 TC = 3
excitation-contraction coupling goal
calcium to filaments of myofibrils; to attach to each other and contract
tail
large protein
rope
head
binding site for actin and ATP
muscle contractions requires
calcium
ATP
thin filament
actin
protein present
actin
small
globular protein chain
troponin
attach tropomyosin to actin
binding site for calcium
trompomyosin
long
thin protein
thin protein
hide binding site on actin
thick filament
myosin
myosin strand intertwined
eccentric contraction
load moved under constant muscle tension and angle joint INCREASE
concentric contraction
load move under constant muscle tension and angle of joint DECREASE
Isotonic
under constant muscle tension, load is moved
concentric contraction
eccentric contraction
isometric
under constant muscle tension
load is NOT moved and angle of joint does NOT change
muscle tension
force generated by shortening sarcomeres
type muscle tension
isotonic
isometric
contraction of muscle fiber
cross-bridge form between actin and myosin head trigger contraction
muscle to shorten
muscle to shorten
calcium ion remain sarcoplasm bind to troponin
ATP always available
creatine phosphate
fast
store extra phosphate for fast transfer back to ATP when needed
muscle fiber relaxation
calcium ion pump back to SR
tropomyosin to reshield binding site on actin strand
muscle STOP contracting when ATP run out/fatigued
glycolysis
slow/anaerobic
break one molecule of sugar down to 2ATP/2 pyruvic acid
myoglobin
store small O2 for absence of sufficient O2
quickly available
aerobic respiration
best way
use oxygen to convert pyruvic acid to ATP
water/CO2 in mitochondria
1 glucose = 36 ATP
myoglobin
rigor mortis
3rd post-mortem stage of death
sarcoplasmic reticulum disintegrate, calcium release into cytosol
muscle contraction occur…
neural stimulus ceases
neural stimulus ceases
release ACh ceases
membrane repolorize
calcium pump return calcium to sarcoplasmic reticulum
skeletal muscle contraction
active site actin exposed (calcium bind to troponin)
myosin bind actin at actin-binding site (cross-bridge)
power stroke
new ATP attach myosin head (cross-bridge detach)
myosin head hydrolyze ATP to ADP/Phosphate
power stroke
phosphate generated in post contraction cycle is released
contraction/relaxation
myosin binds with actin
calcium bind to troponin; troponin pull tropomyosin
myosin head “flexes” to pull actin closer to M-line; sacromere shorten
filament slide
each pull myosin head req. ATP
muscle strength
number of muscle fibers (cells)
disuse
lifestyle or immobility
hypertrophy
muscle growth (Bulk)
atrophy
muscle loss/reduction (disuse)
Duchenne muscular dystrophy DMD
gene mutation on X chromosome
muscle contraction cause sacrolemma to tear and cause accumulated damage/weak
mutation affect protein “dystrophin”
dystrophin
attaches the myofibrils to the sarcolemma
motor unit
motor neuron and all muscle fibers it controls
small
large
small motor unit
each motor neuron only innervate s a few fibers
fine motor
large motor unit
motor unit may innervate thousands of fibers for simple but powerful movement
gross motor
muscles wide range of motor unit size
small motor: light task to elicit small amount of muscle tension
larger motor: recruited for more challenging task
muscle tone
skeletal muscle never relaxed
slight contraction is maintained to keep protein in regulation
flaccid
never relax
hypotonia
decrease muscle tone
hypertonia
increased muscle tone
rigidity or spactic
nervous system control of tension
muscle tone
hypotonia
hypertonia
tetany
tetany
involuntary
sustained muscle contraction, spasms, cramps
overstimulated nerves
calcium issue
tetanus
tetanus
clostridium tetani bacteria
type of muscle fibers
slow oxidative
fast oxidative
fast glycolytic
oxidative
glycolytic
slow oxidative
most myoglobin for oxygen storage
sustain activity for long period of time w/o fatiguing
low tension
fast oxidative
intermediate fibers
less myoglobin
produce powerful, more controlled movement