Retinal Disorders, Glaucoma, Macular Degeneration
1/93
Earn XP
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
94 Terms
Open angle glaucoma
An increase in intraocular pressure due to a decrease in draining the aqueous fluid through meshwork could be caused by either an obstruction or degeneration that is the leading cause of IRREVERSIBLE blindness and the 2nd leading cause of blindness
glaucoma
A group of optic neuropathies characterized by progressive degeneration of retinal ganglion cells usually, not always, due to an increase in intraocular pressure. Sclera may perforate at the lamina and the optic nerve fibers exit the eye.
closed-angle
What form of glaucoma is the more common in people of Asian descent?
open angle, closed angle, normal tension
Forms of chronic glaucoma
open angle glaucoma
What is the leading cause of blindness in African Americans?
About every 1-2 (for pts 40-54 its 1-3)
For patients with risk factors for glaucoma when does the AAO recommend comprehensive eye examination?
Aqueous humor
a transparent watery fluid secreted from by the ciliary body that fills both the anterior and posterior chambers of the eye
posterior chamber through pupil into anterior chamber, trabecular meshwork, Schlemms canal
Drainage route for the aqueous humor
primary (DM), Secondary (ocular disease, corticosteroid therapy, uveitis, trauma)
Forms of chronic open angle glaucoma (90% of chronic glaucoma cases)
age, black/latino, family history, high intraocular pressure, HTN, DM
Risk factors for open angle glaucoma
patients are usually asymptomatic, usually found during a ophthalmologic exam
How is open-angle glaucoma usually found?
central vision (late stage manifestation)
In open angle glaucoma, there is no vision changes as long as what is preserved?
funsoscopic examination, visual field testing, intraocular pressure (IOP)
What tools can you use to diagnose open angle glaucoma?
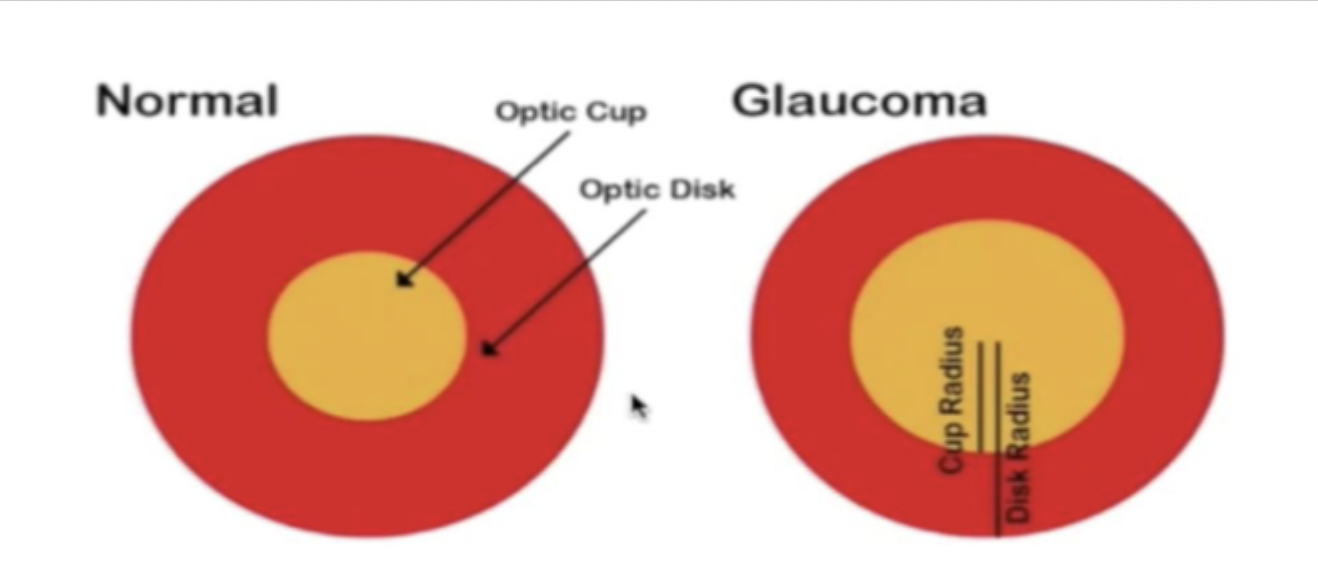
0.5 or less
What is the normal cup-to-disc ratio?
Comprehensive eye exam w/in 24 hours
A 64 y/o patient presents to the clinic for a check-up. Patients medical history is positive for DM type II. While checking their eyes, you note cupping appearance of the optic nerve and a thinning of disc rim, bilaterally. Peripheral vision has also decreased. The intraocular pressure of the both eyes are 37 for the right and 33 for the left. What do we need to refer for?
emergent referral
If IOP is greater than 40 mmHg
eval within a week
IOP 25-29
repeat measure to confirm or refer
IOP of 23-24
evidence of optic nerve damage (disc or retinal nerve structural abnormalities ie cupping/thinning/notching), visual field abnormalities, adult onset, open normal appearing anterior chamber angles, absence of known causes of open-angle glaucoma
What are the open angle glaucoma diagnostic criteria put out by the American Academy of Ophthalmology?
Prostaglandins (latanoprost, bimatoprost), alpha adrenergic, cholinergic agonists
What topical medications can be used to increase aqueous outflow?
increase sclera’s permeability to aqueous fluid or lead to ciliary muscle relaxation
How do prostaglandins help in open angle glaucoma?
Beta blockers (timolol, betaxolol), carbonic anhydrase inhibitors, alpha adrenergic agonist
What topical medications can be used to decrease aqueous production?
decreases formation of aqueous humor
Mechanism of action for timolol
2 readings of IOP >25 (maybe 22), IOP 18 + cupping + vision loss
When should we consider treating open angle glaucoma?
Trabeculoplasty (laser therapy)
What other therapies (not meds) can we use to increase aqueous flow in open-angle glaucoma?
Surgery (shunt/filtration bleb)
What therapies for open-angle glaucoma should we consider for advanced diagnoses that were unresponsive to meds or lasers?
25 years
On average, once open glaucoma starts how long does it take you to become blind
acute angle closure glaucoma
A condition characterized by the narrowing or closure of anterior chamber angle due to the lens being too far forward, leading to inadequate draining of aqueous humor leading to increase IOP (usually > 30 mmHg) and damage to CN II.
primary angle closure
The type of acute angle closure glaucoma that is due to an anatomical variation and has no identifiable secondary cause
Secondary angle closure
The type of acute angle closure glaucoma that results from something causing the narrowing or closure of the anterior chamber angle such as neovascular glaucoma, mass/hemorrhage, fibrovascular membrane overgrowth
family hx, 60+, female, hyperiopia, pseudoexfoliation, Inuit/Asian
Risk factors for acute angle closure glaucoma
Ophthalmology EMERGENT UNDER AN HOUR
Patient presents to the clinic with a migraine. She reports halos around lights, severe eye pain with decreased vision in her right eye, and bouts of nausea/vomiting. While conducting a physical exam you note conjunctival redness, corneal edema and cloudiness as well as a shallow anterior chamber. Her pupils are 4-6 mm dilated and slow to respond to light. Who do we need to call?
visual acuity, pupil evaluation, IOP, slit-lamp to view anterior segments, gonioscopy, undilated fundus exam, visual field testing
What is included in an ophthalmic evaluation of acute angle closure glaucoma?
gonioscopy because you can visual the angle
What is the gold standard in diagnosing acute angle closure glaucoma and why?
May exacerbate symptoms
Why is a dilated fundus exam excluded from a acute-angle closure glaucoma workup?
iritis, traumatic hyphema, conjunctivitis, episcleritis, subconjunctival hemorrhage, corneal abrasion, and infectious keratitis
Differential diagnoses for acute angle closure glaucoma
Timolol maleate (0.5%), apraclonidine (1%), pilocarpine (2%), Acetazolamide (500 mg oral/IV)
If we can’t get our acute angle glaucoma patient seen in an hour, what can we start to decrease IOP?
Carbonic anhydrase inhibitor (increase ion secretion, lower bp, lower IOP)
Mechanism of action for acetazolaminde
acts on the ciliary muscle to get it to contract opening the trabecular meshwork through increased tension on scleral spur increasing the rate at which aqueous humor flows out
Mechanism of action for pilocarpine
Laser peripheral iridotomy (creates hole in iris for aqueous humor to flow)
What is the treatment of choice for acute angle glaucoma?
inflammation, laser burns, repeated treatment if hole closes, Increased IOP
Possible complications with laser peripheral iridotomy
Iridotomy if narrow angle is present
If we find acute angle glaucoma in one eye, what do we need to do to the other eye?
2-5
With acute angle closure glaucoma severe and permanent visual loss occurs within ______ days after symptoms onset
retinal artery occlusion
What condition of the eye is rare but emergent if it occurs and is more common in men 60-65 y/o?
Central retinal artery occlusion (CRAO), Branch retinal artery occlusion (BRAO)
Types of retinal artery occlusion
inner retina, surface of optic nerve
What does the central retinal artery supply?
atherosclerotic disease of the ipsilateral carotid artery
What is the most common cause of a retinal artery occlusion?
HTN, smoking, DM, hyperlipidemia
What are the risk factors for atherosclerotic disease of the ipsilateral carotid artery?
cardiogenic embolism, small artery disease, vascular disease, hematologic disease (sickle cell, hypercoaguative states), vasculitis
Other causes of retinal artery occlusion
CRAO, tPA and emergency ophthalmology consult
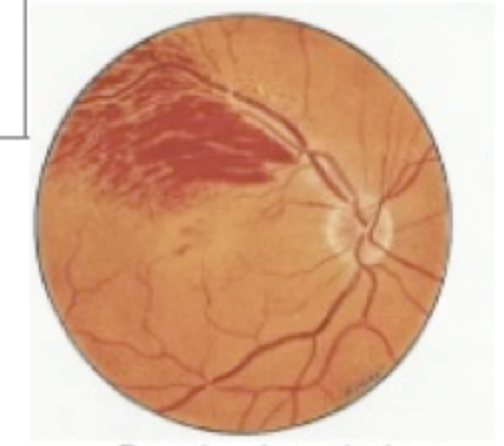
63 y/o male patient presents to the ER with vision loss in his right eye. He states that this started over the last hour and reports no pain. He states that as it was starting his vision would flutter in and out. During your physical exam you note that he can see you hands moving but can’t count fingers. A fundoscopic exam shows a whitening of the retina with a “cherry” spot on the macula. What are we thinking team and what do we need to order?
BRAO
A monocular vision loss (usually just part of the visual field) in which less than 50% of patients have impaired visual acuity that is characterized by a sectoral pattern of retinal ischemia on a fundoscope exam
fluorescein angiography
What other diagnostic tool can we use for retinal artery occlusion though it is barely needed?
recover the vision in the affected eye (damage is irreversible at the 4 hour mark)
What is step one in treating retinal artery occlusion?
ocular massage, anterior chamber para, vasodilators, hyperbaric oxygen, IV acetazolaminde/mannitol, topical pressure lowering drops
Conservative treatments of retinal artery occlusion that aim to decrease IOP and increase perfusion
Pressure is applied to the eye, aqueous outflow increases, once pressure is removed retinal perfusion should improve
Mechanism of action for intermittent ocular massage
prevent recurrent events (blood thinners)
Long term management of retinal artery occlusion
focus on underlying etiology
Treatment plan for BRAO
retinal vein occlusion
The second leading cause of vision loss from retinal vascular disease (follows diabetic retinopathy) with no significant difference between men and women
Branched retinal vein occlusion (BRVO), Hemi Retinal Vein Occlusion (HRVO), Central retinal vein occlusion (CRVO)
Types of retinal vein occlusions
BRVO
A retinal vein occlusion where a vein in the distal venous system is occluded which leads to a hemorrhage along the distribution of the small vessel of the retina. Related to the compression of the branch vein by the retinal arterioles at the arteriovenous crossing point
Refer to ophthalmology for a complete eye exam
Patient reports to the clinic stating she is seeing a dark spot in her left eye and that everything looks burry and grey. She reports no pain, just the blurred vision in the left eye. You see this during the physical exam. What do we need to do next?
HRVO
A retinal vein occlusion that occurs when the superior and inferior retinal drainage does not merge into a single central retinal vein and one of the two trunks is occluded leading to involvement of one half of the retina
CRVO
A retinal vein occlusion that is usually a result of a primary thrombus within the central retinal vein most of the time presents as an acute onset of painless blurred vision in 1 eye
age, HTN, DM, smoking, obesity, hypercoaguable state, glaucoma, retinal arteriolar abnormalities
Retinal vein occlusion risk factors
Patient’s history, complete ophthalomolgic exam (extraocular motility, IOP, pupillary function, external/internal eye structures, slit-lamp exam, visual acuity, dilated fundoscope exam)
How do you diagnose retinal vein occlusion?
monthly observation
In patients with a retinal vein occlusion WITHOUT macular edema or neovascularization what is our treatment plan?
Macular degeneration
What condition of the eyes is a degenerative disease of the central portion of the retina (AKA the macula) leading to the loss of central vision and is known as the leading cause of blindness in industrialized countries?
fovea centralis
What is the small, central pit composed of closely packed cones in the eye and is located in the center of the macula lutea of the retina. Responsible for sharp central vision which is needed for reading and driving
Rods
What is responsible for low light vision, no color, and low spatial acuity
cones
What part of the eye are active at higher light levels (photopic vision)
Dry (atrophic, chronic), wet (neovascular, exudative, acute)
Types of macular degeneration
dry
The type of macular degeneration the usually causes some degree of visual impairment and may progress to severe blindness as a result of insoluble extracellular aggregates (drusen) that accumulate in the retina. Late stage includes degeneration of retinal pigment epithelium and overlying light-sensing retinal photoreceptors.
wet
The macular degeneration that occurs in 10-15% of patients that rapidly progresses to blindness if untreated and will only start after dry. Characterized by choroidal neovascularization. Can cause the macula to bulge or lift → destroying/distorting central vision
age (starting at 50), caucasian, smoking, heavy alcohol use, cataract surgery
Risk factors for macular degeneration
dry macular dengeration
65 y/o patient presents to the clinic due to vision loss in both eyes that makes it difficult to read or drive. Patient reports blind spots in her vision and that she needs to be in bright rooms to be able to see well. A dilated fundoscope exam shows oval patches on the retina and increased pigmentation with mottling. What are we thinking team?
wet macular degeneration
77 y/o female presents to the clinic with acute visual distortion she states, “I feel like I’m on a boat, the horizon is moving like waves.” She also reports central vision loss. During your physical you note metamorphopsia while using an Amsler grid. A dilated fundoscopic exam shows hemorrhage and neovascularization. Macula looks greyish green. Thoughts?
Rate of vision loss (if acute call opthalmology), one/both eye involvement, distance/near/total vision loss
While evaluating a patient for macular degeneration what do we need to determine in the history
physical activity, healthy diet, nutritional/vitamin supplements, stop smoking
How do you prevent macular degeneration? NOTE: No real evidence to support any benefit
daily oral eye vitamin supplement (AREDS2), stop smoking
What’s our treatment plan for dry macular degeneration? NOTE: no proven effective treatment
Vitamin C, E, zinc, copper, lutein, zeaxanthin
What’s in the AREDS2 vitamin?
intravitreous injection of vascular endothelial growth factor (VEGF) inhibitor (bevacizumab, ranibizumab, aflibercept), AREDS2 vitamin, low vision rehab, limit progression and stabilize/reverse vision loss
How are we treating wet macular degeneration?
dilated eye exam using a slit lamp
A clinical diagnosis of macular degeneration is made by an ophthalmologist after a
retinal detachment
A condition of the eye characterized by the separation of the retina from the RPE and choroid usually as a result of an accumulation of fluid between layers
Rhegmatogenous
The most common type of retinal detachment that is caused by a full thickness retinal hole tear usually due to vitreous traction on retina that can be asymptomatic or symtomatic
Posteror vitreous detachment (PVD)
Most common site of Rhegmatogenous retinal detachment which is an age-related process where the vitreous fluid separates from the innermost retinal surface layer
Nonrhegmatogenous
A form of retinal detachment caused by leaks or exudate under the retina or vitreous traction without a tear or hole
visual acuity exam, confrontational evaluation of visual fields
Patient presents to the clinic with a increase in floaters in her eyes, she states, “It looks like I’ve got cobwebs in here.” She also notes periodic flashes of light and a dark curtain slowly moving. She also reports that she has loss the ability to read. What do you need to do in your initial eval?
hours to days
Concerning large horseshoe retinal tears symptoms may progress over
1-4 weeks
Concerning small retinal tears symptoms may progress over
central/visual field loss
While conducting an exam testing for retinal detachment, when would we need an URGENT ophthalmology consults, slit-lamp microscopy, and dilated retinal exam?
High risk features (visual field loss, subjective/objective decreased vision, vitreous hemorrhage/vitreous pigment on slit-lamp)
While conducting an exam testing for retinal detachment, when would we need an elective ophthalmology exam?
delimitating laser photocoagulation, cryoretinopexy barrier
How are we treating a full-thickness retinal break with small retinal detachment?
Reattachment of retina (pneumatic retinopexy, scleral buckle placement, pars plana vitrectomy)
How are we treating an obvious retinal detachment?
Nothing just educate your patients on when to come in
What can you prevent a posterior vitreous detachment with?