Lecture 9-Hematologic System
1/56
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
57 Terms
Hematologic system
blood, blood vessels, organs that produce blood
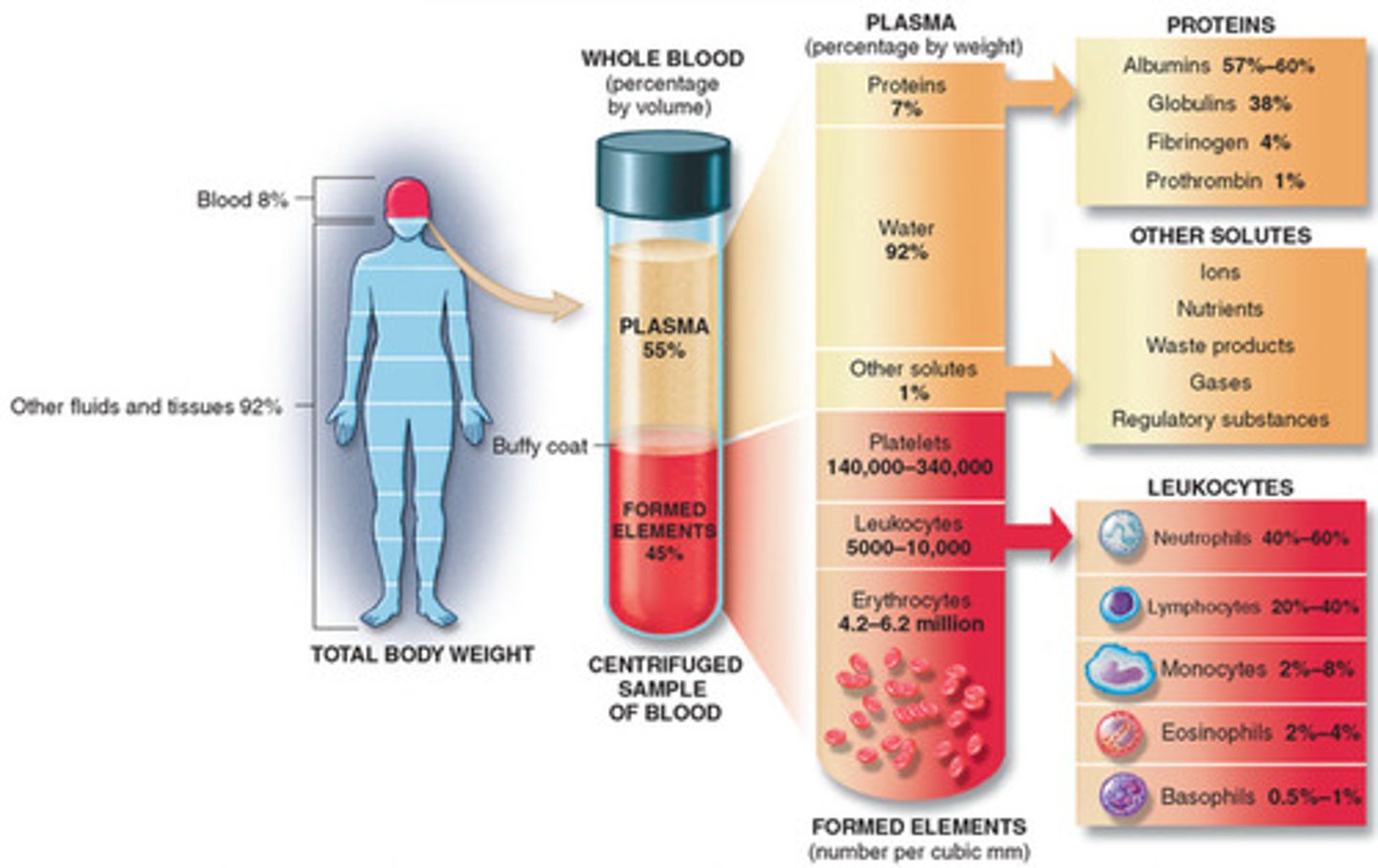
Erthryocytes
red blood cells, carry oxygen
Leukocytes
White blood cells; inflammatory/immune response
Platelets
Control clotting
Plasma
Serous solution of blood
Classification of Hematologic Disorders
1. Erythrocytes (RBC) Disorders
2. Leukocyte (WBC) Disorders
3. Platelet Disorders (platelets help with clots)
4. Coagulation disorders (not every coagulate disorder is a platelet issue)
Erythrocytes (RBC's)
- consists mainly of hemoglobin & supporting framework to carry oxygen & carbon dioxide
- number of RBC's is affected by:
1. gender (Men>Women)
2. fitness level (sedentary individuals have fewer in their bloodstream)
Erythrocyte Disorders: Anemia (more of a disorder/symptom; usually a product of something else)
- reduction in oxygen-carrying capacity of blood due to abnormality of quantity or quality of erythrocytes
- anemia is not truly a disease itself
- can result from conditions that cause excessive blood loss, destruction of erythrocytes, and/or decreased production of erythrocytes.
common diseases/causes of anemia
1. iron deficiency associated w/ chronic GI-bleed (often secondary to excessive or prolonged NSAID i.e. non-steroidals use
2. chronic diseases (cancers i.e. leukemia, kidney & liver disease)
3. autoimmune/inflammatory diseases (rheumatoid arthritis, systemic lupus erythematosus, pernicious anemia)
4. infectious diseases (tuberculosis, AIDS)
pernicious anemia
slow onset; body is unable to absorb B12
anemia risk factors
- deficiency in iron, vitamin B12 and folate
- conditions like Crohns, Celiac disease that affects absorption within GI tract
- heavy menstrual periods
- pregnancy
- family hx & genetics
- hx of certain infections, autoimmune conditions, and/or other blood diseases
- excessive alcohol consumption (b/c alcohol thins blood)
- excessive or prolonged use of NSAIDs (GI bleed)
- age >65
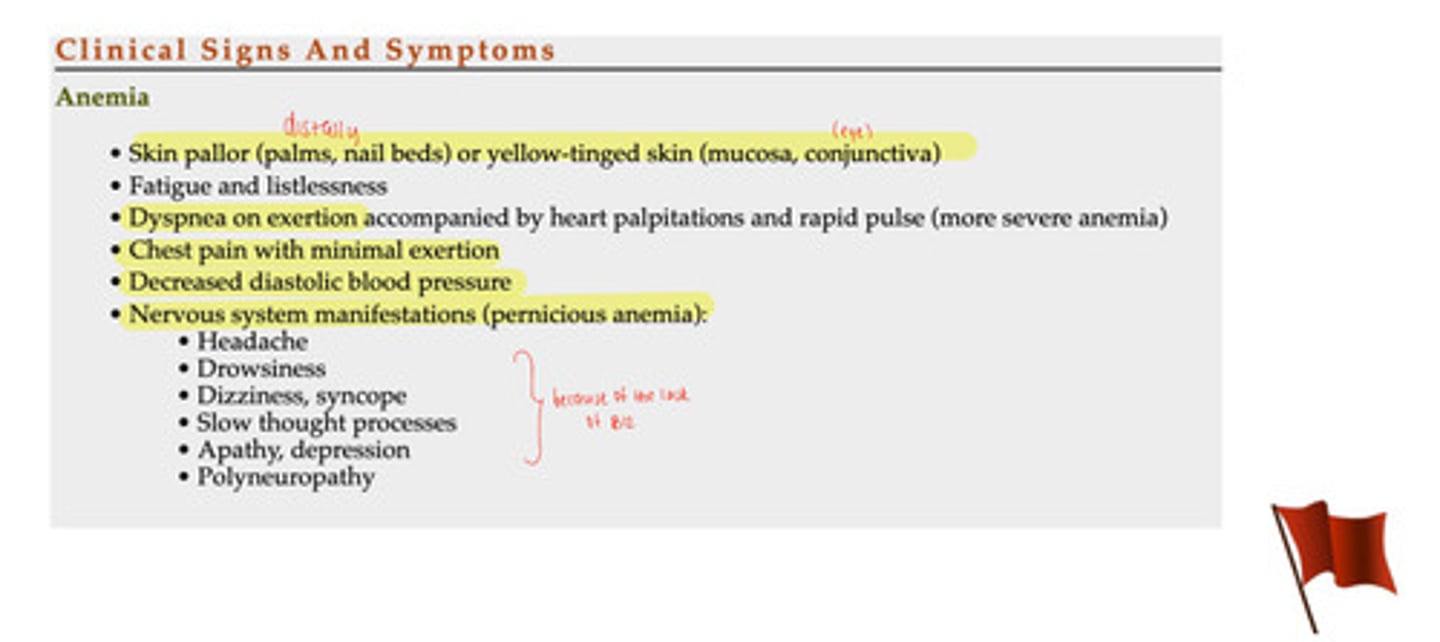
anemia clinical signs & symptoms
- skin pallor (palms, nail beds) or yellow-tinged skin (mucosa, conjuctiva)
- fatigue or listlessness
- dyspnea or exertion accompanied by heart palpitations & rapid pulse (more severe anemia)
- chest pain with minimal exertion
- decreased diastolic BP
- nervous system manifestation (pernicious anemia):
1. headache
2. drowsiness
3. dizziness, syncope
4. slow thought process
5. apathy, depression
6. polyneuropathy
*b/c of lack of B12*
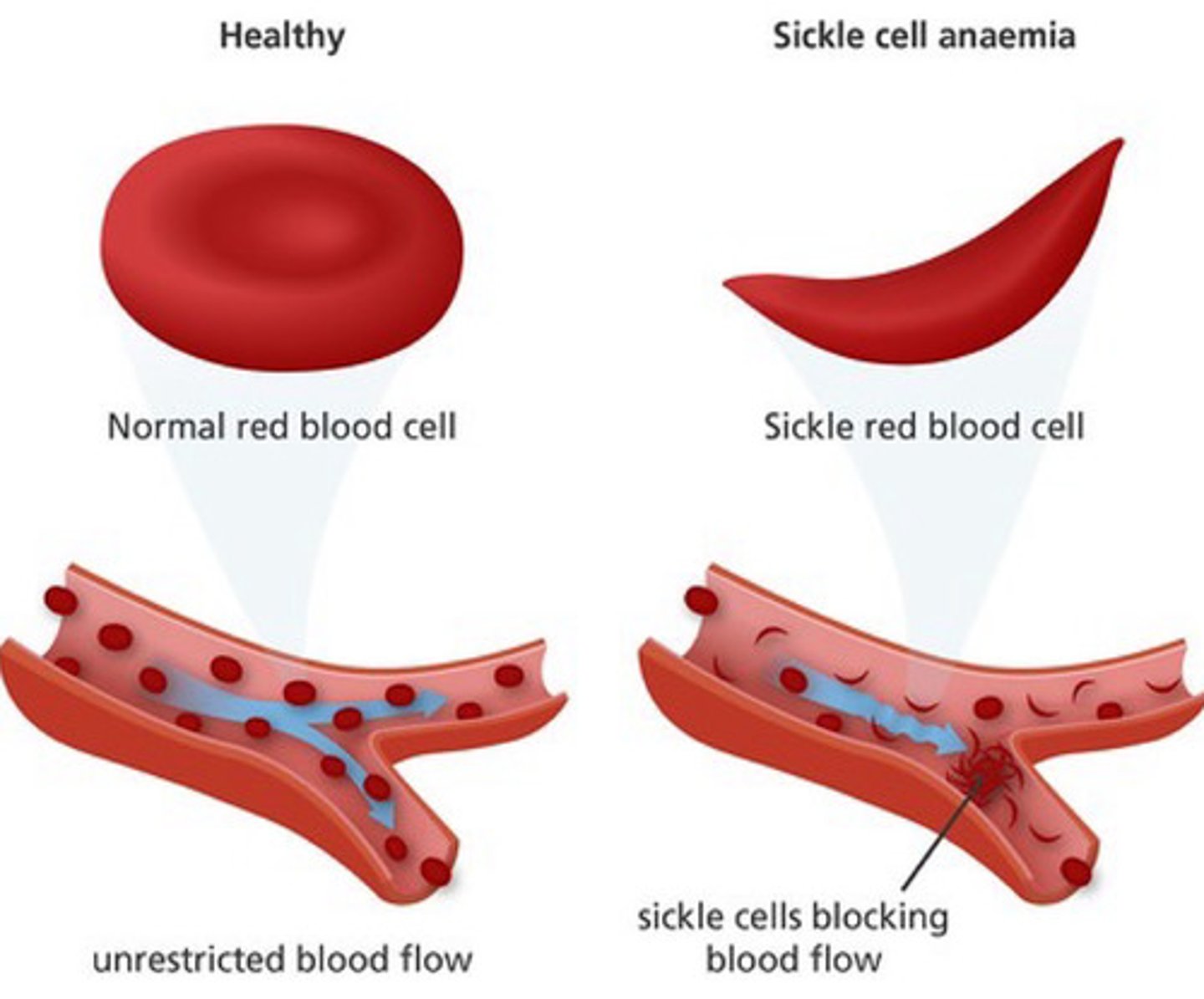
sickle cell anemia
- inherited, autosomal recessive disorder characterized by the presence of abnormal form of hemoglobin
- genetic mutation that leads to an alteration in RBC shape; looks like a sickle or crescent
- altered shape causes the cell to lose its ability to deform & squeeze through smaller vessels & affects blood flow
sickle cell anemia risk factors
- genetics/family hx
- ethnicity: african, middle eastern, indian, mediterranean, asian, or hispanic-american (central & south america) ancestry
- estimation that 1 in 12 African Americans descent carry at least one sickle cell gene
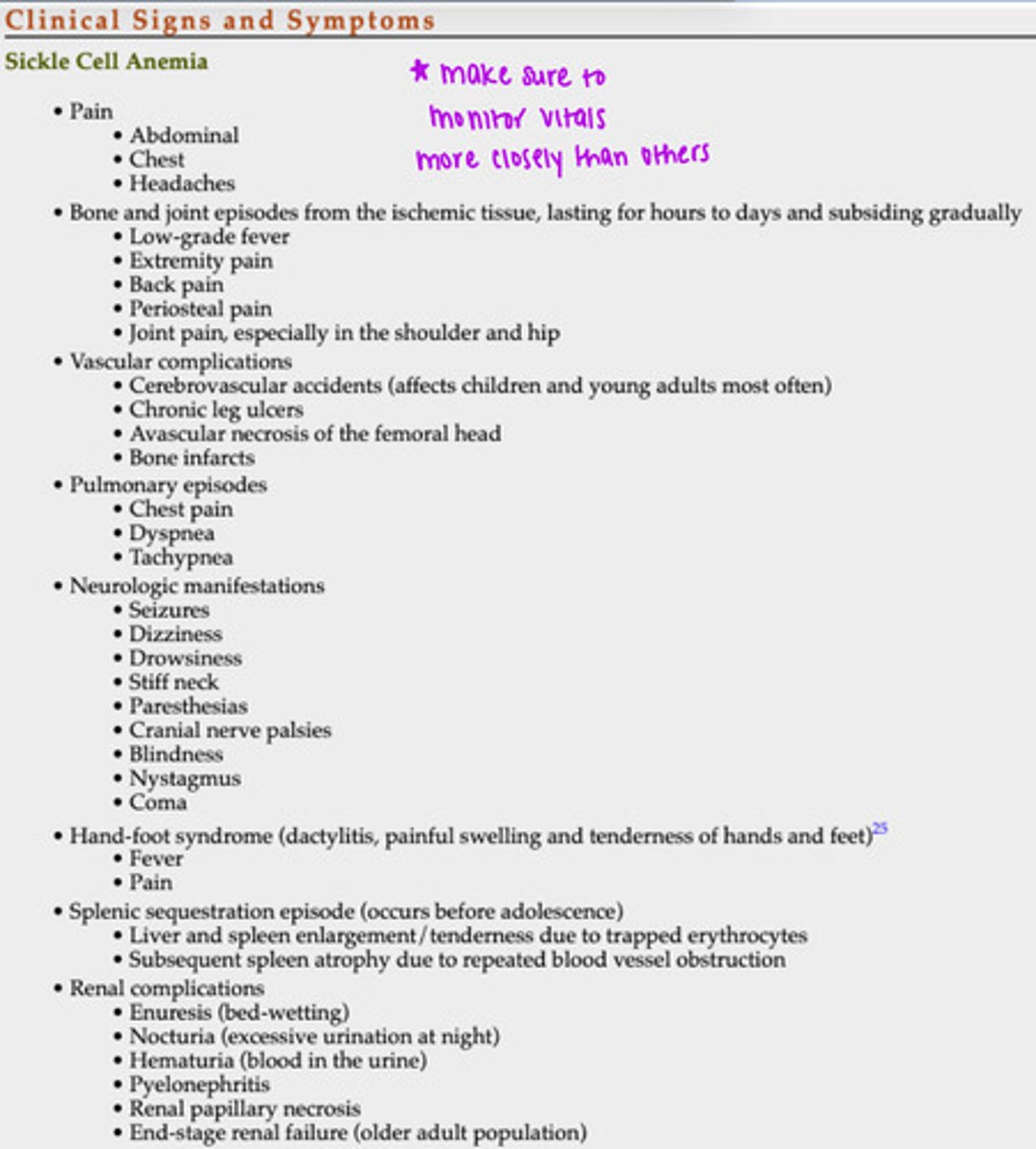
sickle cell anemia clinical signs & symptoms
- pain
- bone & joint episodes from ischemic tissue, lasting for hours to days & subsiding gradually
- vascular complications
- pulmonary episodes
- neurologic manifestations
- hand-foot syndrome
- splenic sequestration episode (occurs before adolescence)
- renal complications
*make sure to monitor vitals more closely than others*
anemia level of urgency
MODERATE; can be a life-threatening situation for some
- depends on level of severity & clinical presentation, presence or absence of medical management, along w. medical hx & other situational risk factors present
- requires caution, especially during planning exercise component of plan of care
polycythemia (erythrocytosis) i.e. general disorder of blood cells; many cells in blood
- elevation in number of RBC's & concentration of hemoglobin
- increases whole blood viscosity & blood volume
- can cause abnormal clotting & reduced flow to brain & other vital organs/structures
what are the 2 forms of polycythemia (erythrocytosis)?
1. primary polycythemia (i.e. polycythemia vera)
2. secondary "adaptive" polycythemia
primary polycythemia
occurs from a neoplastic (i.e. tumor/cancerous growth) disease of bone marrow w. unknown etiology
secondary "adaptive" polycythemia
results in response to decreased oxygen supply to tissues; commonly from smoking, high altitudes, sleep apnea, chronic arterial hypoxemia, & chronic heart/lung conditions
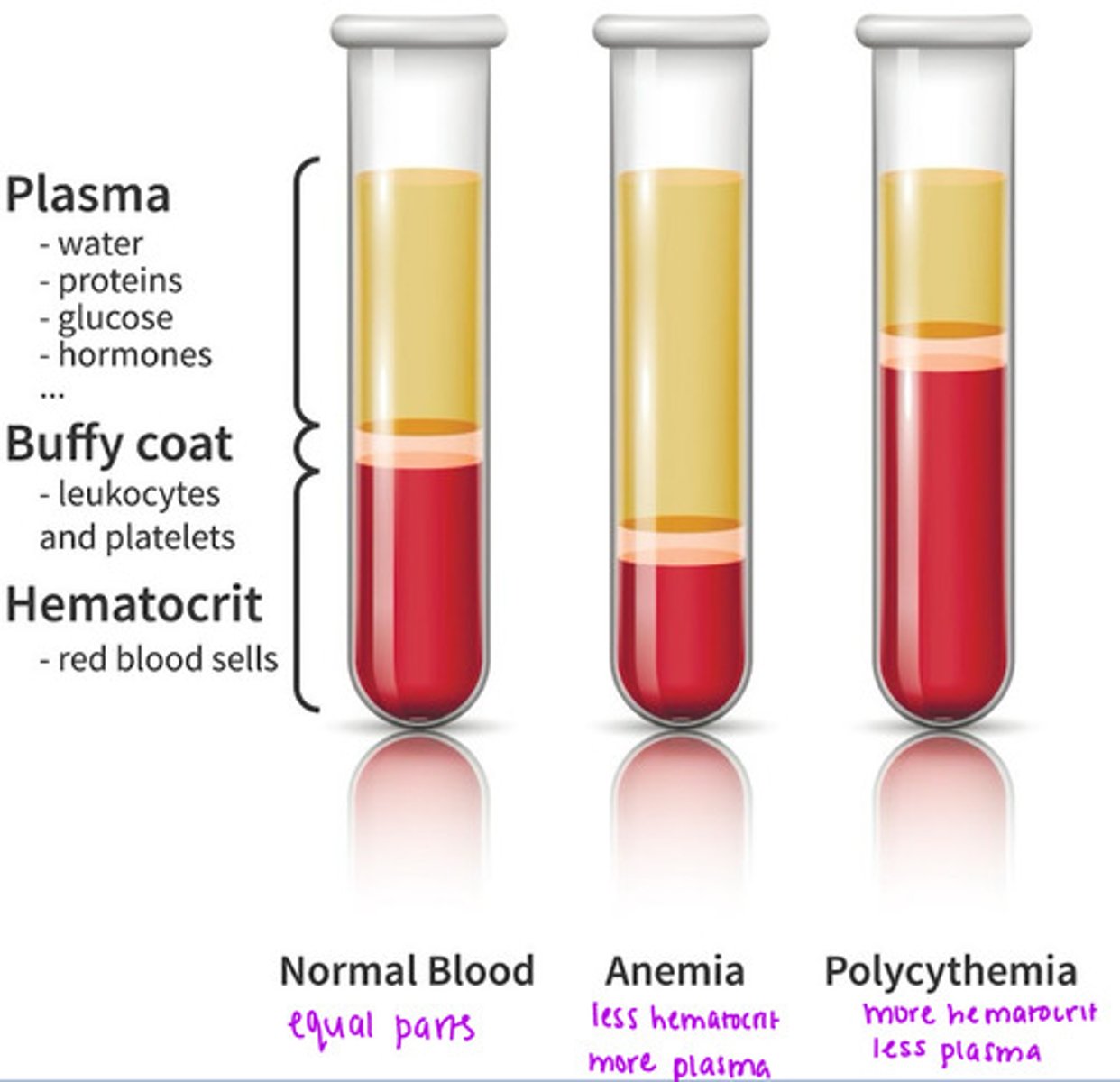
what does normal blood, anemic blood, and polycythemic blood look like?
normal blood: equal parts
anemia: less hematocrit, more plasma
polycythemia: more hematocrit, less plasma
polycythemia clinical signs & symptoms
- general malaise (not tired or exhausted, but doesn't feel right) & fatigue
- SOB
- headache/feeling "fullness" in the head
- dizziness
- irritability
- blurred vision
- syncope (fainting)
- sensory disturbances in hands & feet
- unintentional weight loss
- excessive ecchymosis (bruising easily)
- cyanosis
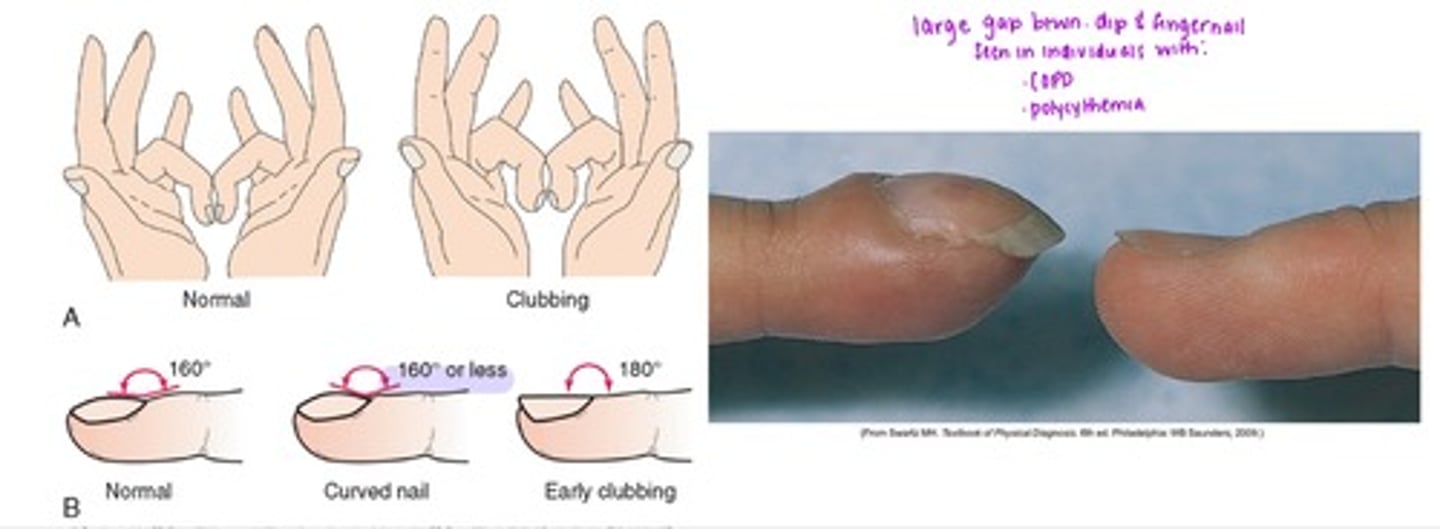
- clubbing of fingers
- elevated BP
- decreased mental acuity
clubbing of fingers
- large gap btwn. DIP & fingernail i.e. 160 degrees or less; seen in individuals with COPD, polycythemia
polycythemia/erythrocytosis level of urgency
MODERATE; depends on level of severity & clinical presentation, presence or absence of medical management, along w. medical hx & other situational risk factors present
- requires caution, especially during planning exercise component of plan of care i.e. will not have patient do kettle bell snatches b/c of potential bruising from kettle bells
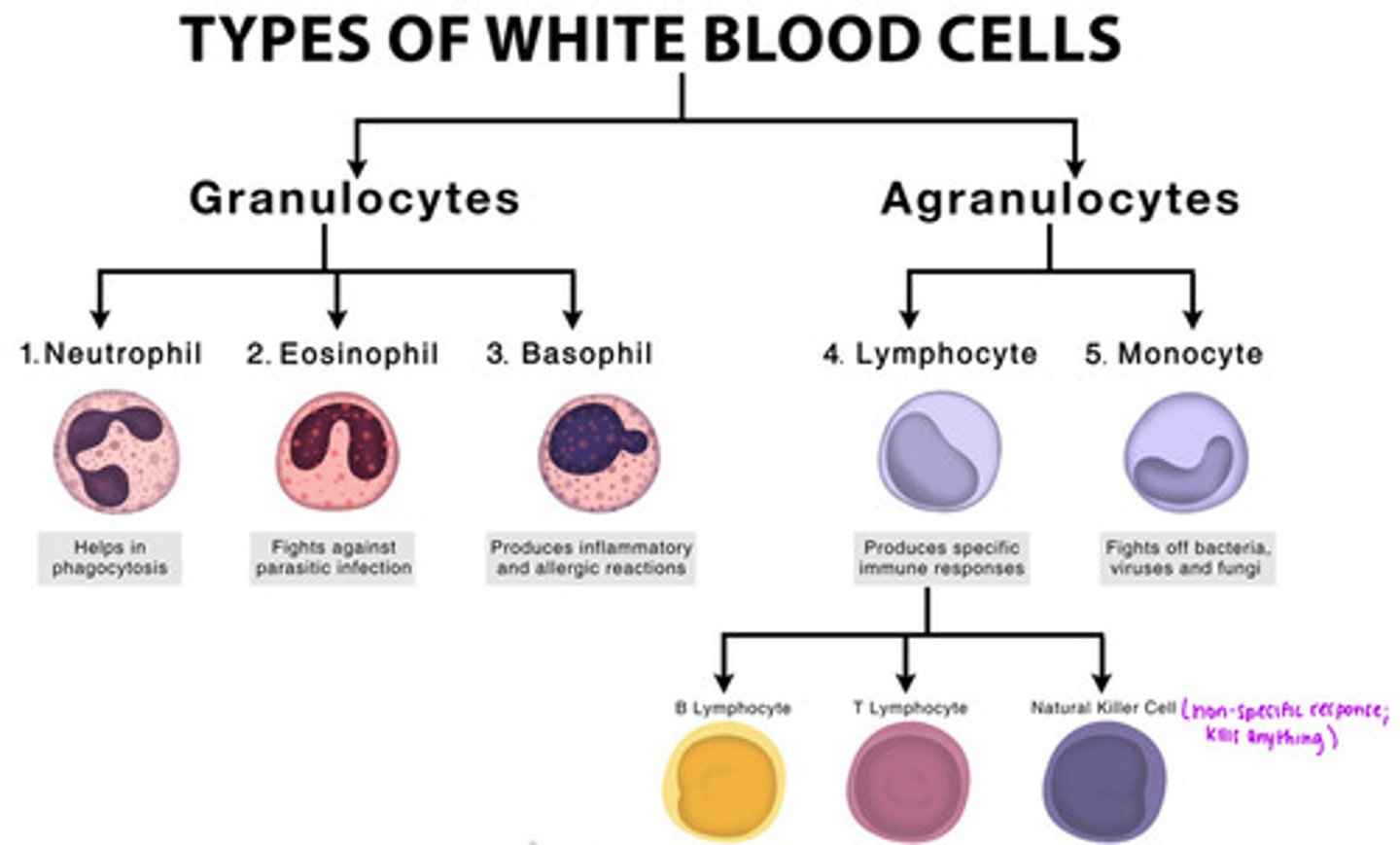
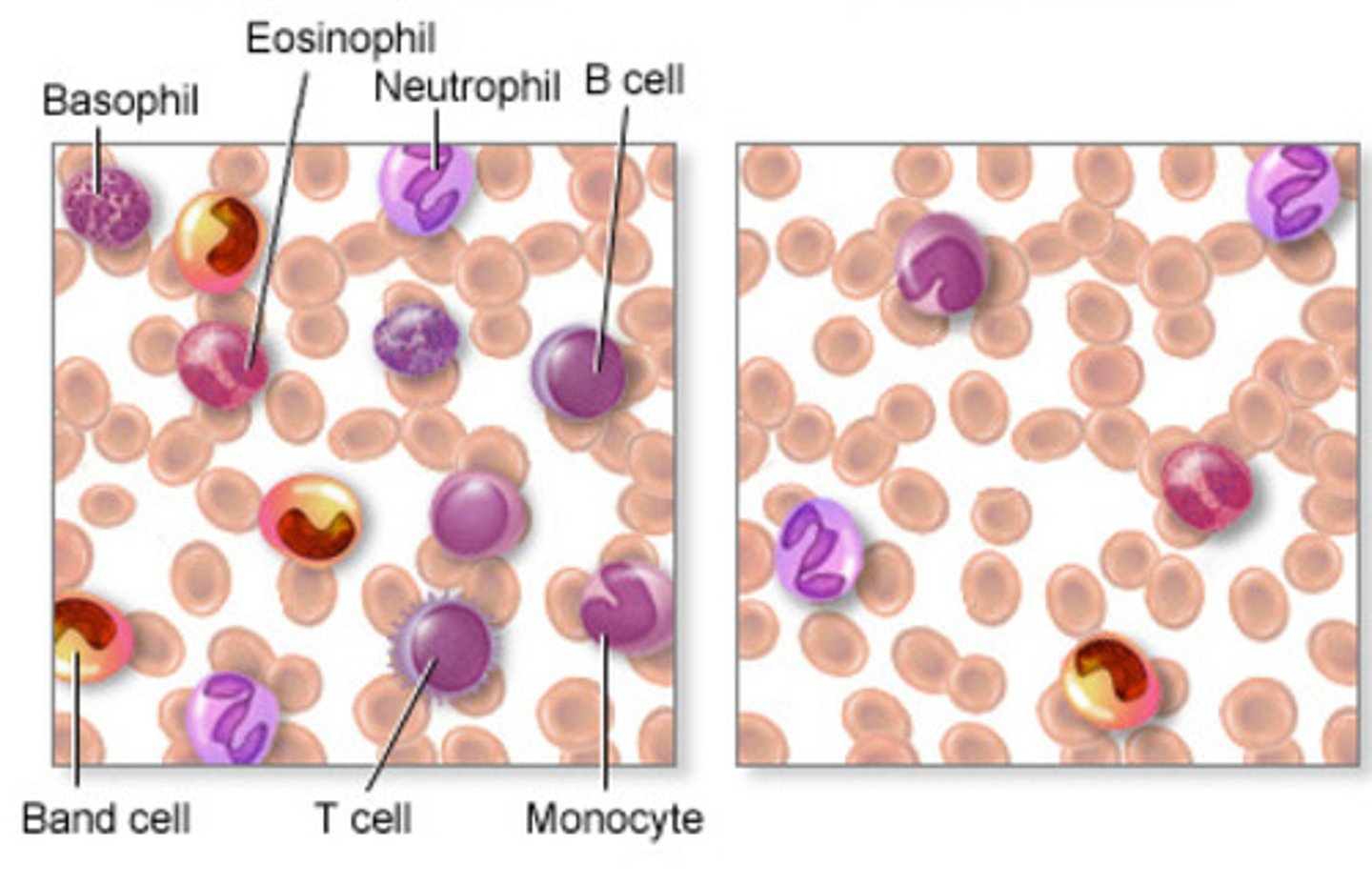
Leukocytes (WBC's) 3 primary types:
1. Lymphoid cells
2. Monocytes
3. Granulocytes
lymphoid cells
produce antibodies & react w. antigens
monocytes
largest circulating blood cell that eventually form macrophages
granulocytes
- contain lysing agents (breaks something down) that can ingest foreign material
- defend by phagocytosing (injects/envelops) bacteria & infectious agents
what are the 2 types of white blood cells?
1. Granulocytes
2. Agranulocytes
leukocyte disorder: leukocytosis
defined by an elevated WBC count >10,000 leukocytes mm^3
- process is normal, but only to a point
is not a disease, but a response to, or sign of:
- bacterial/viral infection
- inflammation or tissue necrosis
- metabolic toxicity
- neoplasm
- acute hemorrhage
- pneumonia
- chemical toxicity
leukocytosis clinical signs & symptoms
- symptoms systemic infection/inflammation:
constitutional symptoms (i.e. general malaise, excessive fatigue, etc); especially fever
symptoms of localized inflammation or trauma; localized:
-warmth
-redness
-pain/tenderness
-visible tissue damage
leukocytosis risk factors
- excessive emotional stress
- notable physical stress (e.g. illness, injury, burns, or surgery)
- immune system disorders (lupus or rheumatoid arthritis)
- current or past hx of cancer
- thyroid problems
- certain medications (lithium, corticosteroids, beta-agonists i.e. albuterol aka inhaler)
- allergies
- hx of splenectomy (b/c spleen isn't properly filtering out WBCs; short term response so liver takes over for the spleen)
- smoking
- obesity
leukocytosis level of urgency
MODERATE; depends on level of severity & clinical presentation, presence or absence of medical management, along w. medical hx & other situational risk factors present
- concern is more for what this can indicate, rather than the condition itself
Leukocyte Disorders: Leukopenia
- reduction in the # of leukocytes below 5000mL
- in contrast to leukocytosis, leukopenia is NEVER BENEFICIAL
- these are immunosuppressed individuals & infection of any type can be exceptionally dangerous
- importance of good hand washing & hygiene practices when working w. this population
leukopenia clinical signs & symptoms
- constitutional symptoms include cough, fever, chills, diaphoresis, nausea, fatigue, malaise, etc.
- ulceration of mucous membranes (mouth, rectum, vagina)
- frequent or painful UTI (especially if chronic)
- persistent infections
leukopenia level of urgency
MODERATE; depends on level of severity & clinical presentation, presence or absence of medical management, along w. medical hx & other situational risk factors present
- concern is more for what this can indicate, rather than the condition itself
platelets (thrombocytes)
- have a high turnover rate & survive approx. 8-10 days in circulation
- platelet levels & function can be affected by intrinsic factors as well as extrinsic factors like medication, foods, & exercise
platelets primary function
hemostasis (stopping blood movement); serve in coagulation by creating hemostatic plugs in ruptured blood vessels or any injured blood vessel lining
Platelet Disorders: Thrombocytosis
- increase in platelet count (>450,000 platelets/mm^3, but usually asymptomatic until >1,000,000 platelets/mm^3)
- categories include:
1. primary (essential)
2. secondary (reactive)
primary (essential) thrombocytosis
bone marrow generates excessive platelets; usually a genetic mutation or inherited condition
secondary (reactive) thrombocytosis
increase in platelet production in response to surgery or injury, conditions like iron deficiency, or neoplasm, etc. ; is appropriate to a certain point
thrombocytosis clinical signs & symptoms
- cold, numb, painful hands/feet (related to clot formation & occlusion of smaller more distal peripheral vessels)
- bruising easily
- potential abdominal pain, & referred pain to the left shoulder (related to splenomegaly i.e. enlarged spleen due to compression of central portion of diaphragm)
Platelet Disorders: Thrombocytopenia
- decrease in number of platelets <150,000 platelets mm^3
- results from reduced platelet production or increased/premature platelet destruction
- primary bleeding sites (bone marrow or spleen)
- secondary sites (from small blood vessels in skin, nose, uterus, GI tract, urinary tract, respiratory tract, and brain i.e. intracranial hemorrhage)
thrombocytopenia risk factors
- known disease/dysfunction of bone marrow (leukemia)
- other cancers
- recent radiation (where it was done can affect thrombocytes)
- use of certain medications that have a cytotoxic effect:
- warfarin (coumadin) or other blood thinners
- NSAIDs
- methrotrexate (immunosuppressant that reduces inflammatory response)
thrombocytopenia clinical signs & symptoms
excessive bleeding after minor trauma
- spontaneous bleeding:
1. petechiae (<4mm; little tiny hemorrhages or red dots on skin)
2. purpura spots (4-10 mm; bigger & more purple petechiae; looks like bruises but isn't)
3. ecchymoses (bruising; >1 cm)
4. epistaxis (nose bleeds)
- menorrhagia (menstrual bleeding >7 days)
- gingival (gums) bleeding
- melena (black, tarry colored stools developed from GI bleeds)
Coagulation Disorders: Hemophilia
- hereditary clotting disorder
- caused by abnormality of clotting factors VII and IX: functional plasma clotting proteins; they assist platelets in clotting mechanism
- NOT characterized by altered function or amount of platelets
*affects other clotting factors within blood*
Hemophilia clinical signs & symptoms
- bleeding into joint spaces (hemarthrosis)
- hemophiliac arthropathy
- mild pain & swelling to severe pain w. greater swelling
- muscle hemorrhages
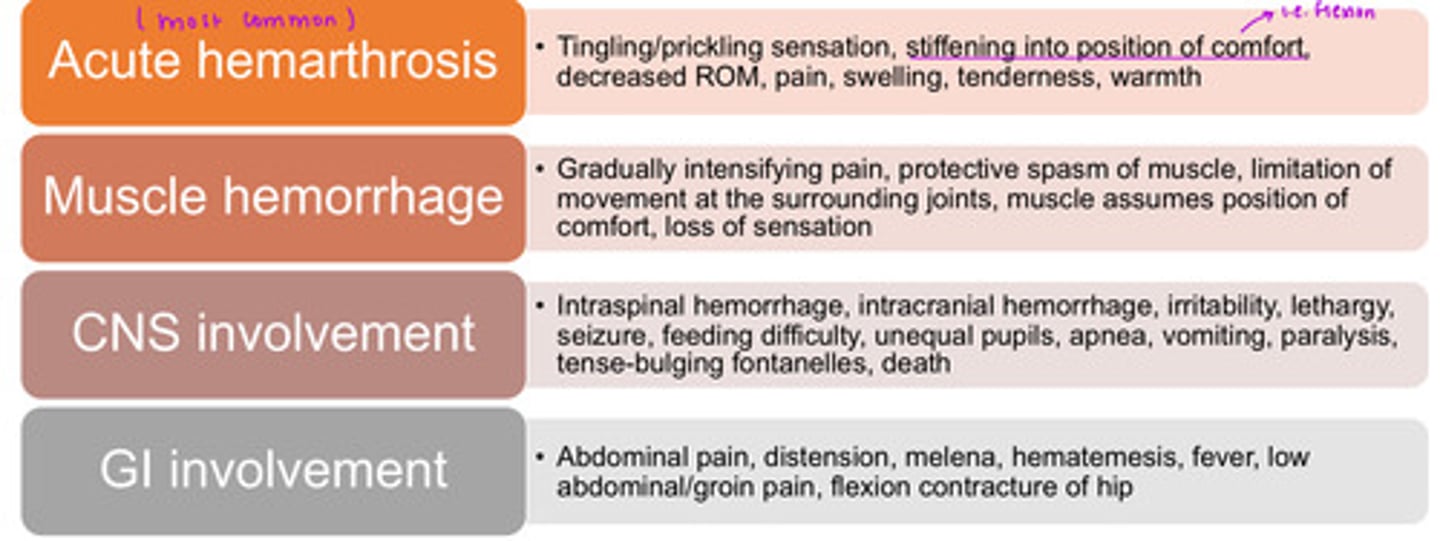
what are the hemorrhage types related to hemophilia?
1. acute hemarthrosis (most common)
2. muscle hemorrhage
3. CNS involvement
4. GI involvement
acute hemarthrosis
tingling/prickling sensation, stiffening into position of comfort i.e. flexion, decreased ROM, pain, swelling, tenderness, warmth
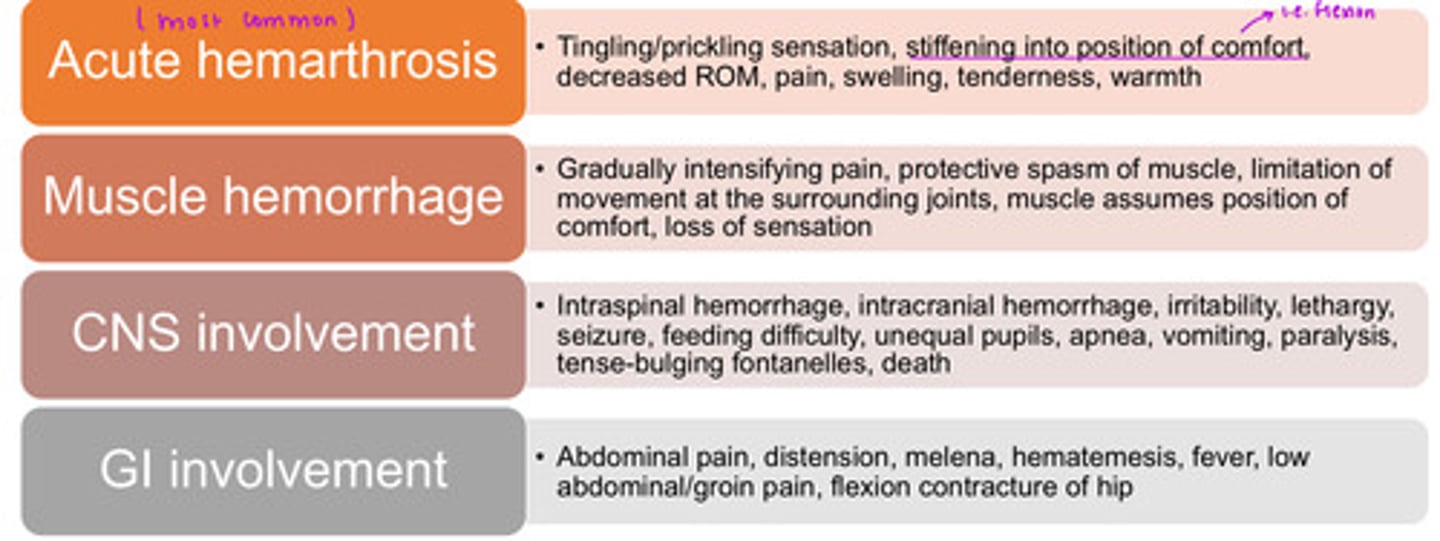
muscle hemorrhage
Gradually intensifying pain, protective spasm of muscle, limitation of movement at surrounding joints, muscle assumes position of comfort, loss of sensation
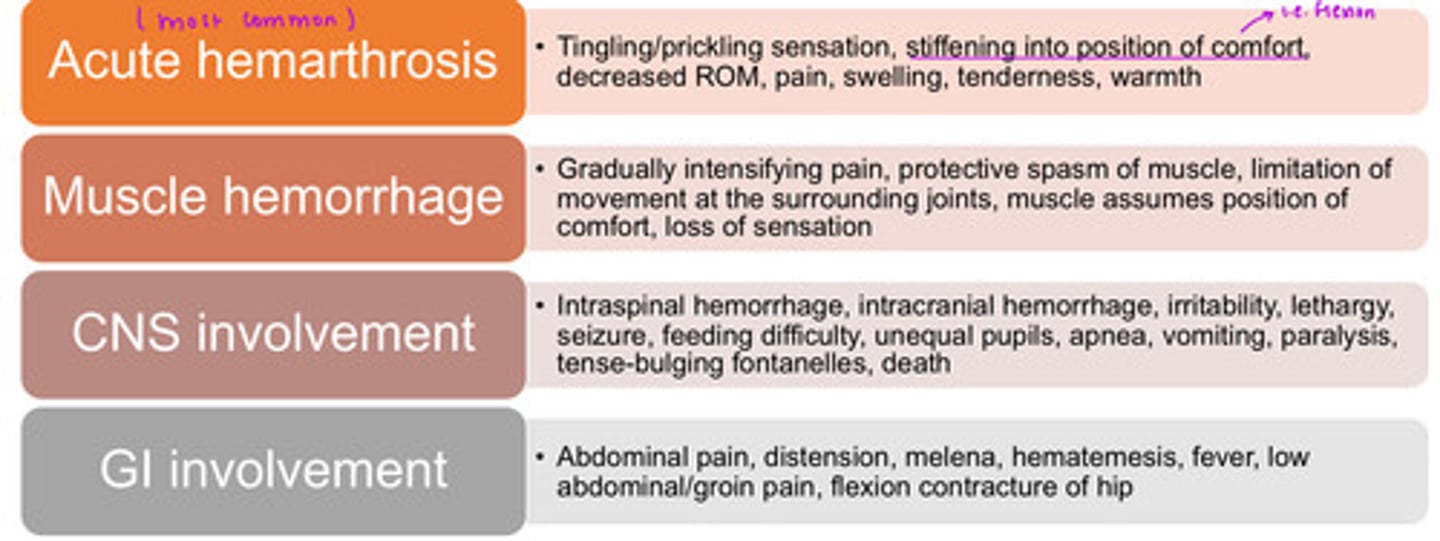
CNS involvement
intraspinal hemorrhage, intracranial hemorrhage, irritability, lethargy, seizure, feeding difficulty, unequal pupils, apnea, vomiting, paralysis, tense-bulging fontanelles, death
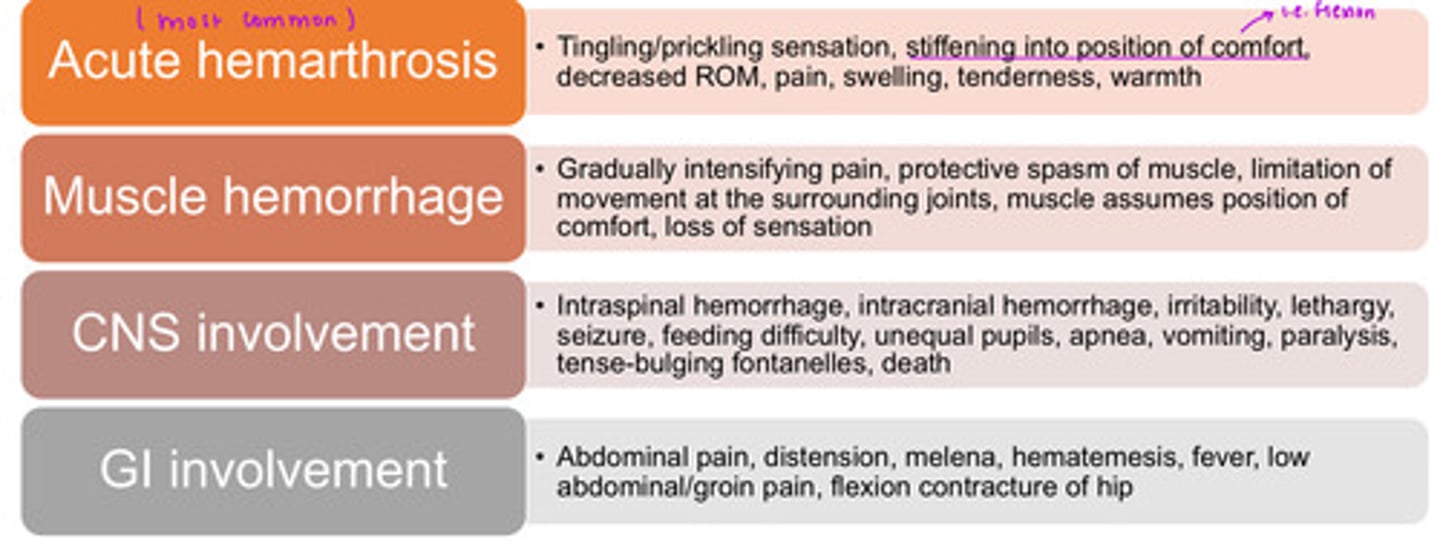
GI involvement
abdominal pain, distension, melena, hematemesis, fever, low abdominal/groin pain, flexion contracture of hip
what are the locations of hemarthrosis?
*typically bilateral*
- knees (most common)
- elbows
- ankles
- hips
- shoulders

clues to screening hematologic disease:
- increased level of concern for hematologic conditions with:
o History of, or undergoing chemotherapy or radiation therapy
o Chronic or long-term use of aspirin or NSAIDs
o History of spontaneous bleeding of any kind
o Recent major surgery or history of organ transplantation
o Rapid onset of dyspnea, chest pain, weakness, and fatigue with palpitations, especially associated with environmental changes (especially significant increases in altitude)
o Observed changes in hands/feet and nail-beds i.e. cyanosis or clubbing
probing hematologic past medical hx questions
- Have you recently been told you are anemic? • Have you recently had any serious blood loss (possibly requiring transfusion)? (Anemia)
• Have you ever been told that you have a congenital heart defect? (Polycythemia)
• Do you have a history of bruising easily, nosebleeds, or excessive blood loss?(Polycythemia, hemophilia, thrombocytopenia)
o For example, do you bleed or bruise easily after minor trauma, surgery, or dental procedures? o Has any previous bleeding been severe enough to require a blood transfusion?
probing hematologic associated signs & symptoms questions
• Do you experience shortness of breath, heart palpitations, or chest pain with slight exertion (e.g., climbing stairs) or even just at rest? (Anemia)
• Do you ever have trouble catching your breath? • Are there any activities you have had to stop doing because you do not have enough energy or breath?
o Be aware of the clients who stop doing certain activities because they become short of breath. For example, they no longer go up and down stairs in their homes and choose to avoid this activity...or the client who cannot complete all of his or her shopping at one time. They may not report being short of breath because they have decreased their activity level to accommodate for the change in their pulmonary capacity.
probing hematologic associated signs & symptoms questions continued
• For persons at elevations above 3500 feet: Have you recently moved to this geographic location? (Polycythemia)
• Do you ever have episodes of dizziness, blurred vision, headaches, fainting, or a feeling of
fullness in your head? (Polycythemia)
• Do you have recurrent infections and low-grade fevers, such as colds, influenza-like symptoms, or other upper respiratory infections? (Abnormal leukocytes)
• Do you have black, tarry stools (bleeding into the GI tract)
• Do you have blood in your urine? (Genitourinary tract)
o For women: Do you frequently have prolonged or excessive bleeding in association with your menstrual flow? [Excessive may be considered to be measured by the use of more than four tampons each day; prolonged menstruation usually refers to more than 5 days] (anemia, thrombocytopenia).