(21) Regulation of Reabsorption & Secretion
1/90
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
91 Terms
ability of renal tubules to reabsorb the same relative amount of water and solutes no matter how much is filtered
they increase reabsorption in response to increased glomerular filtration fraction
glomerulotubular balance
In order to maintain glomerulotubular balance, the rate of proximal tubule reabsorption remains at what amount of the glomerular filtration fraction regardless of the volume?
65%
When the glomerular filtration fraction is increased, do tubules (including the loop of Henle) increase reabsorption, decrease it, or keep it constant?
increase
What 2 general types of pressures govern the rate of reabsorption across the peritubular capillaries?
hydrostatic, colloid
What is the direction of flow of reabsorption?
renal tubule to interstitial fluid to peritubular capillary
Is hydrostatic pressure an inward or outward force? (relative to whatever column it is in)
outward
Is colloid pressure an inward or outward force?
inward
What predominantly determines colloid pressure?
plasma proteins
What draws water into a peritubular capillary from the interstitial fluid after it has been partially reabsorbed from the tubules?
pericapillary colloid pressure
Does peritubular capillary hydrostatic pressure favor or oppose capillary reabsorption?
oppose
(pushes fluid out of the capillary)
Does interstitial fluid hydrostatic pressure favor or oppose capillary reabsorption?
favor
(pushes fluid into capillary)
Does capillary colloid pressure favor or oppose capillary reabsorption?
favor
Does interstitial fluid colloid pressure favor or oppose capillary reabsorption?
oppose
What is normal glomerular filtration rate?
125 mL/min
(every minute, 125 mL leaves capillary and enters filtrate)
What is the net filtration pressure (net reabsorptive force) favoring outward movement of fluid from glomerular capillaries into renal tubules?
10 mmHg
(6+32-13-15)
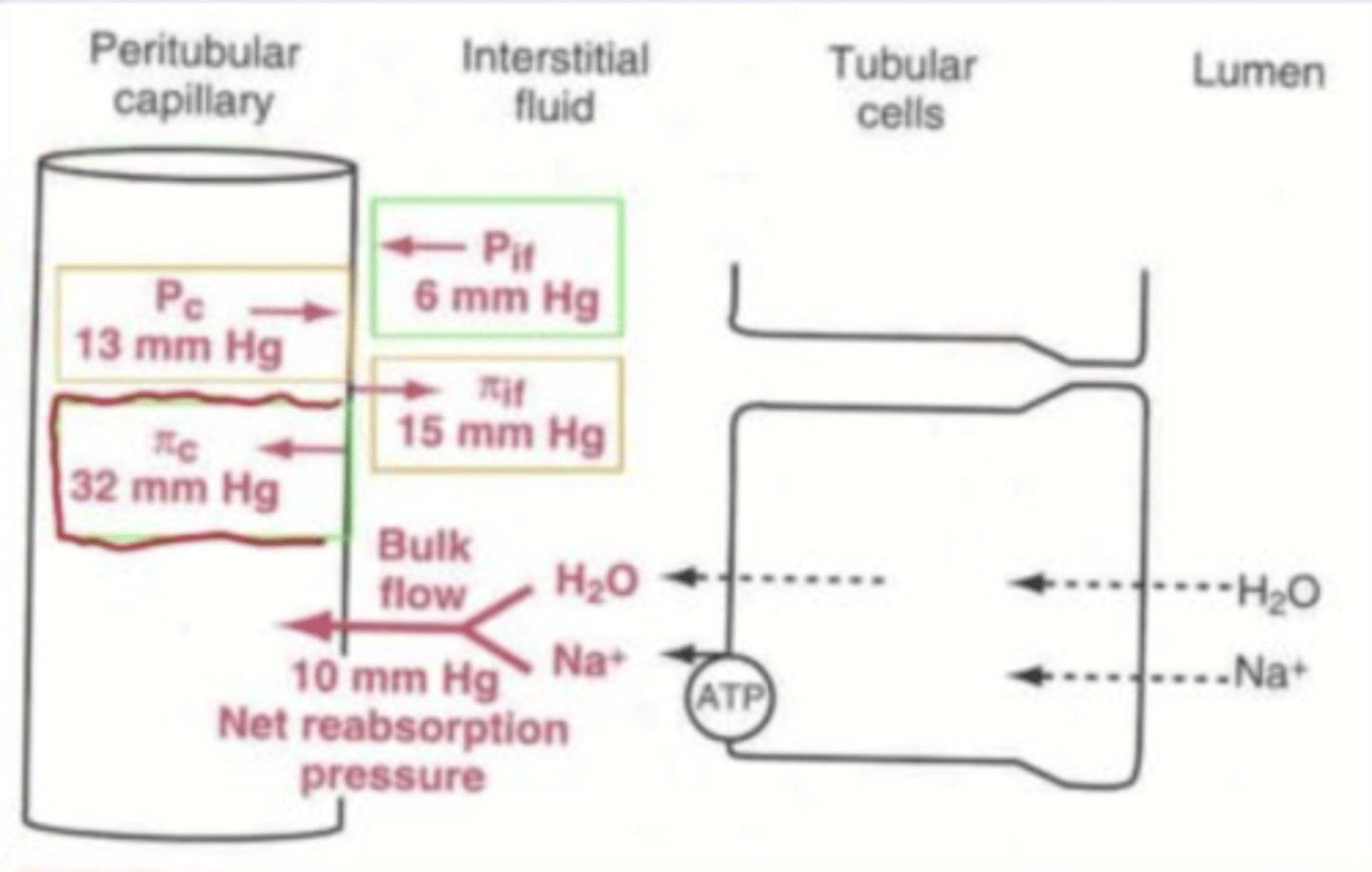
Under normal physiologic circumstances, what is the average filtration coefficient?
12.4 mL/min/mmHg
How can we calculate overall reabsorption rate?
filtration coefficient x net reabsorptive force
What is our average reabsorption rate?
124 mL/min
(since this is filtration coefficient 12.4 x net absorptive force 10)
What are two factors that influence peritubular capillary hydrostatic pressure?
arterial pressure, afferent/efferent arteriole resistance
Any increase in systemic arterial pressure will cause peritubular hydrostatic pressure to increase or decrease?
increase
If we have an increase in peritubular capillary hydrostatic pressure, does this result in an increase or decrease in overall reabsorption?
decrease
(greater outward force = reduced inward force)
Any time we have a decrease in resistance of the afferent or efferent renal arterioles (i.e. dilation), will this increase or decrease reabsorption?
increase
(since it increases the amount of fluid entering peritubular capillaries)
What are two factors that influence peritubular capillary colloid osmotic pressure?
systemic plasma colloid osmotic pressure, filtration fraction
If we have a higher filtration fraction, does this lead to an increase or decrease in peritubular capillary colloid osmotic pressure?
increase
(higher concentration of proteins that were left behind)
Does an increased peritubular capillary colloid osmotic pressure lead to an increase or decrease in reabsorption?
increase
(pulls more fluid into peritubular capillaries)
If the filtration fraction somehow increases, does peritubular capillary colloid osmotic pressure increase or decrease?
increase
Peritubular capillary hydrostatic and colloid osmotic pressures influence renal tubule reabsorption by changing what?
pressures in interstitial fluid
(because it's the middle man, changes from the peritubular capillary alters what's going on here, having an effect on reabsorption)
If interstitial fluid hydrostatic pressure increases, does this cause reabsorption to increase or decrease?
decrease
If interstitial fluid hydrostatic pressure decreases, does this cause reabsorption to increase or decrease?
increase
Decreased capillary reabsorption (decreased amount of fluid going from interstitial fluid to peritubular capillary) will lead to an increase or decrease in renal tubule absorption?
decrease
(increases interstitial fluid hydrostatic pressure = decreases reabsorption rate)
Decreased capillary reabsorption leads to a decrease in renal tubule absorption. This is because what happens to interstitial fluid hydrostatic pressure: increase or decrease?
increase
Decreased capillary reabsorption leads to an increase in the interstitial fluid hydrostatic pressure, which leads to a decrease in the rate of reabsorption from the renal tubule.
This creates the potential for movement of what two things back into the tubule?
sodium, water
(typically only happens in chronic hypertension though)
Increased capillary reabsorption (increased amount of fluid going from interstitial fluid to peritubular capillary) will lead to an increase or decrease in renal tubule absorption?
increase
Increased capillary reabsorption leads to an increase in renal tubule absorption. This is because what happens to interstitial fluid hydrostatic pressure: increase or decrease?
decrease
Increased capillary reabsorption leads to a decrease in interstitial fluid hydrostatic pressure, eventually resulting in net increase in renal tubular reabsorption.
This is because the movement into interstitial fluid of what two things is favored and occurs without a back leak?
water, solutes
If we have a short term high BP, this stimulates what mechanism? How does this affect GFR? Urine output?
myogenic mechanism, slightly increases GFR, same urine output
Does long term elevation of BP result in increased or decreased excretion of sodium?
increased
Does long term elevation of BP result in increased or decreased excretion of water?
increased
refers to increased excretion of sodium (decreased reabsorption) as a result of long term elevated arterial pressure
natriuresis
refers to increased excretion of water (decreased reabsorption) as a result of long term elevated arterial pressure
diuresis
Does long term elevated arterial pressure result in an increase or decrease in the reabsorption of sodium and water?
decrease
Long term elevated arterial pressure results in natriuresis and diuresis. Is this due to an increase or decrease in peritubular capillary hydrostatic pressure?
increase
Does long term elevated arterial pressure result in an increase or decrease in angiotensin II production?
decrease
(since angiotensin II normally elevates BP)
If we have chronic hypertension, do we want our kidneys to increase or decrease urine output?
increase
(reduce blood volume)
A significant decrease in systemic blood pressure would lead to which of the following?
A. no change in renal tubule reabsorption
B. an increase in renal tubule reabsorption
C. a decrease in renal tubule reabsorption
B
hormone that controls tubular reabsorption by increasing Na+ reabsorption and K+ secretion
aldosterone
Does aldosterone increase or decrease Na+ reabsorption?
increase
(decrease secretion)
Does aldosterone increase or decrease K+ secretion?
increase
(decrease absorption)
What kind of cells does aldosterone act upon? (specific kind + location)
principal cells in late distal/collecting tubules
How does aldosterone cause an increase in Na+ reabsorption and decrease in K+ reabsorption (increase in K+ secretion)?
stimulates Na/K ATPase and increases Na+ permeability
What molecule is stimulated by aldosterone to affect Na/K reabsorption and secretion?
Na/K ATPase
(increases amount of these in the membrane)
Does aldosterone increase or decrease Na+ permeability?
increase
(by inserting more Na+ channels into lumenal membrane)
Without aldosterone, such as in Addison's disease, what two conditions result based on the ion concentrations?
hyponatremia, hyperkalemia
condition involving excess aldosterone, associated with hypernatremia (Na+ retention) and hypokalemia (K+ depletion)
Conn's syndrome
With excess aldosterone, such as in Conn's syndrome, what two conditions result based on the ion concentrations?
hypernatremia, hypokalemia
Aldosterone is more important in regulating which ion: Na+ or K+?
K+
Is aldosterone release stimulated when there is increased or decreased plasma K+ concentration?
increased
Is aldosterone release stimulated when there is increased or decreased plasma Na+ concentration?
decreased
Is aldosterone release stimulated when there is increased or decreased extracellular fluid volume?
decreased
(since aldosterone tries to raise blood pressure by reabsorbing Na+ and water)
hormone that controls tubular reabsorption by increasing both Na+ and water reabsorption only
angiotensin II
How does angiotensin II affect sodium reabsorption?
increases it
How does angiotensin II affect water reabsorption?
increases it
How does angiotensin II affect efferent arteriole?
vasoconstriction
(helps increase BP)
How does angiotensin II initially affect GFR: increase or decrease?
increase
Does angiotensin increase or decrease peritubular capillary hydrostatic pressure? What about net tubular absorption?
increases, decreases
Does angiotensin increase or decrease filtration fraction? What about peritubular capillary colloid osmotic pressure?
increases (for both)
Which renal tubule does angiotensin II have its greatest effect on?
**by stimulating Na/K ATPase and Na/H exchange
proximal tubule
If we have a decrease in arterial pressure, this is sensed by what cells in the kidney? What do they secrete as a result?
juxtaglomerular cells, renin (converted to angiotensin I, then angiotensin II)
After renin stimulates the production of angiotensin I, a converting enzyme in the lung converts it to angiotensin II. What is the biggest difference between these two?
angiotensin I just causes mild vasoconstriction, angiotensin II causes strong response and Na+ reabsorption
What two hormones does angiotensin II stimulate the release of?
aldosterone, ADH
hormone that causes decreased water excretion in the kidneys and mostly increases the water permeability of the late distal/collecting tubules
ADH (vasopressin)
What is the most important function of ADH?
conserve water
(increase water permeability of late distal & collecting tubules so that it doesn't get excreted)
In the absence of ADH, are the late distal and collecting tubules permeable or impermeable to water?
impermeable
(results in water loss in urine)
Does ADH (vasopressin) cause vasodilation or vasoconstriction throughout the body?
vasoconstriction
modified neurons in the hypothalamus that sense the osmolarity of extracellular fluid
osmoreceptors
When the osmolarity of the extracellular fluid is low, the osmoreceptors initiate nerve signals in the hypothalamus and cause an increase or decrease in ADH secretion?
decrease
Does a high osmolarity indicate increased or decreased ADH secretion?
increased
Does alcohol increase or decrease ADH secretion?
decrease
(therefore it functions as a sort of diuretic)
ADH acts upon which cells to increase water permeability?
principal cells
(in the late distal and collecting tubules)
receptor on principal cells in the collecting tubule (their basolateral membrane) that ADH binds to when it diffuses into the interstitial fluid
V2
When the V2 receptor on principal cells in distal or collecting tubules binds ADH, this activates what second messenger pathway? What overall effect?
cAMP cascade, increases water permeability
hormone that decreases Na+ and water reabsorption
atrial natriuretic peptide (ANP)
How does ANP affect sodium reabsorption?
decreases
(increases excretion)
How does ANP affect water reabsorption?
decreases
(increases excretion)
What part of the kidney does ANP mainly act on to reduce water and sodium reabsorption?
collecting tubules
Why would we want ANP to decrease sodium and water reabsorption?
lower BP by lowering blood volume
How does ANP affect renin and aldosterone secretion?
inhibits it
(since ANP decreases blood pressure and renin & aldosterone increase it)
Aldosterone acts on which of the following tubules in the kidney?
A. early distal tubule
B. descending loop of Henle
C. proximal tubule
D. cortical collecting tubules
D
Angiotensin I...
A. is formed as a result of activation of angiotensinogen by renin
B. is transformed into angiotensin II as a result of converting enzyme action in the lungs
C. is the primary stimulus for the release of aldosterone from the adrenal glands
D. is both A and B
E. is both A and C
F. all of the above
D
(angiotensin II is what stimulates aldosterone release, not angiotensin I)
Which of the following is not attributable to atrial natriuretic peptide (ANP)?
A. It is released from the cardiac atria when the ECF volume is reduced.
B. It inhibits Na+ reabsorption in the distal parts of the nephron.
C. It inhibits renin secretion by the kidneys.
D. It inhibits aldosterone secretion by the adrenal cortex.
E. It inhibits sympathetic nervous activity to the heart and blood vessels.
A
The Na+-K+ ATPase transport system that plays a pivotal role in tubular reabsorption is located in the...
A. lumenal membrane of tubular cells
B. basolateral membrane of tubular cells
C. podocytes
D. glomerular capillary membrane
E. basement membrane
B