Unit 5 - Venous Insufficiency Wounds
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
34 Terms
Venous System — Normal Pathology
Venous flow
Valves prevent retrograde flow
Return of blood flow is facilitated by muscle pump
Interstitial Spaces —> Venous Capillaries —> Superficial Veins —> Deep Veins
Venous Hypertension — Pathophysiology
Weak, “leaky” valves
Varicose veins
Hemosiderin staining/deposits
Edema
Edema below the lower leg =
venous insufficiency
Edema extending to the thigh =
lymphedema
Theories of venous Insufficiency Ulceration
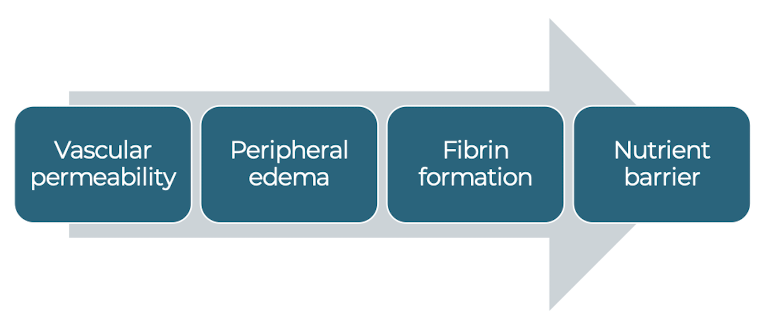
Fibrin Cuff Theory
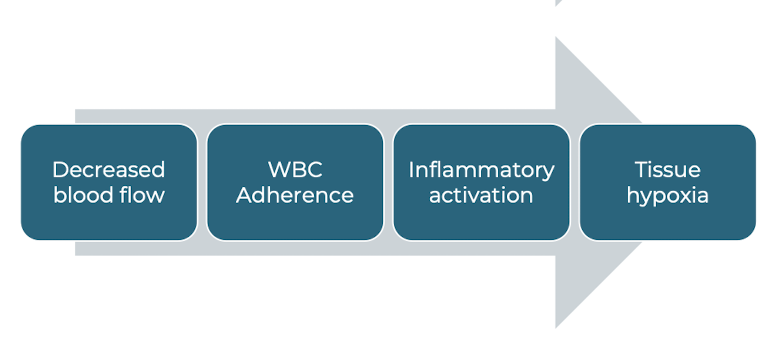
White Blood Cell Trapping Theory
Fibrin Cuff Theory
White Blood Cell Trapping Theory
Risk Factors for Venous Wound Development
Vein Dysfunction
Muscle pump failure
Trauma
Previous wound
Advanced age
Obesity
Diabetes
Venous Insufficiency — Examination
Non-Invasive
Supine and standing
Ankle Brachial Index as needed
Trendelenburg test
Venous Duplex ultrasound
Photoplethysmography
Venous filling time
Venous Insufficiency — Examination
Invasive
Phlebography/venography, ambulatory venous pressure, intravenous ultrasound
Clinical Signs and Symptoms
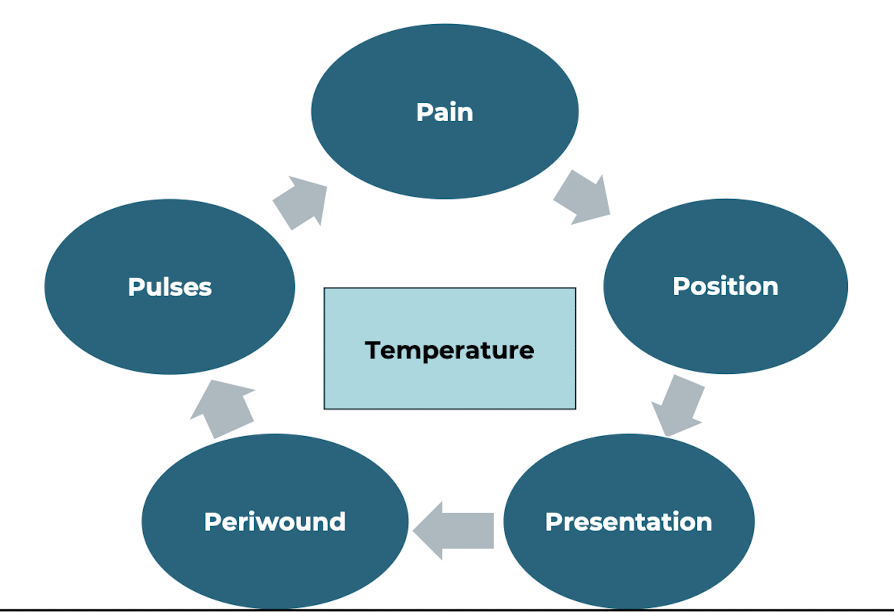
Pain
No Pain/General Aching
Elevated = Good
*NOTE: Contraindication with Active CHF
Position
Gaiter Region (medial lower leg)
Presentation
Insidious onset
Shallow/Superficial
Little to no Eschar
Irregular shape
Periwound
Hemosiderin Staining
Pulses
Palpable without deficits
Temperature
Mild increases
Better Prognosis
smaller
acute / subacute
fast healing
low comorbid factors
adherence
Worse Prognosis
larger
chronic
slow healing
older age
higher BMI
concurrent arterial deficits
General Interventions
Patient Education
Wound etiology
Lifestyle modifications
Adherence to interventions
Compression (Gold Standard)
Absorptive dressings
General skin care
Precautions/Contraindications to Treatment
Arterial Disease
Compression should NOT be used with ABI < 0.5
Consultation required with ABI between 0.5-0.7
Allergic Reactions
Whirlpool
General Intervention Guidelines
control edema
protection
healthy living
follow up with physician
Gold Standard Treatment - Compression
Non-elastic vs Elastic bandages
Enhances calf muscle pump
Graded distal to proximal
Mild-Moderate: 30-40 mm hg (ankle)
Severe: 40-50 mmhg (ankle)
Shifts blood from superficial —> deep veins
Decreases pain
Compression Contraindications
ABI < 0.7
Acute Infection
Pulmonary edema
Active CHF
Active DVT
Compression Types
Unna boot
short stretch wraps
long stretch / elastic wraps
multilayer systems
compression stockings
Unna Boot
Zinc Oxide that hardens after application
Worn for ~ 1 week
May shape the limb into a “wineglass” after use
Short stretch wraps
Ideal
Avoid tourniquet effect
Consistent distal —> proximal pressure
Increasing width =
Long stretch / elastic wraps
Not safe for coexisting arterial disease
Multilayer Systems
Decreased slippage
Increased compression
Bulky
Manual wrapping techniques
short/long stretch procedure
multilayer procedure
Short/Long Stretch Procedure
Prepare Wound/limb
Protect skin/Add padding as needed
Apply wrap
Pt in supine
Foot in DF
Anchor with Fig 8
Continue with spiral or Fig 8 at 50% overlap
No more than 50% stretch
End at popliteal space
Secure with tape
Multi-layer Procedure
Prepare Wound/limb
Protect skin
Apply wrap
Pt in supine
Foot in DF
Apply initial padding layer (no tension/spiral)
Apply light layer
Apply light compression layer – FIG 8
Apply flexible bandage - No more than 50% stretch
End at popliteal space
Secure with tape
Double check the wrapping
No gaps
No wrinkles
Coban
Metatarsal heads
Top of lower limb at popliteal space
Capillary refill!!
Types of wrapping
spiral
figure 8