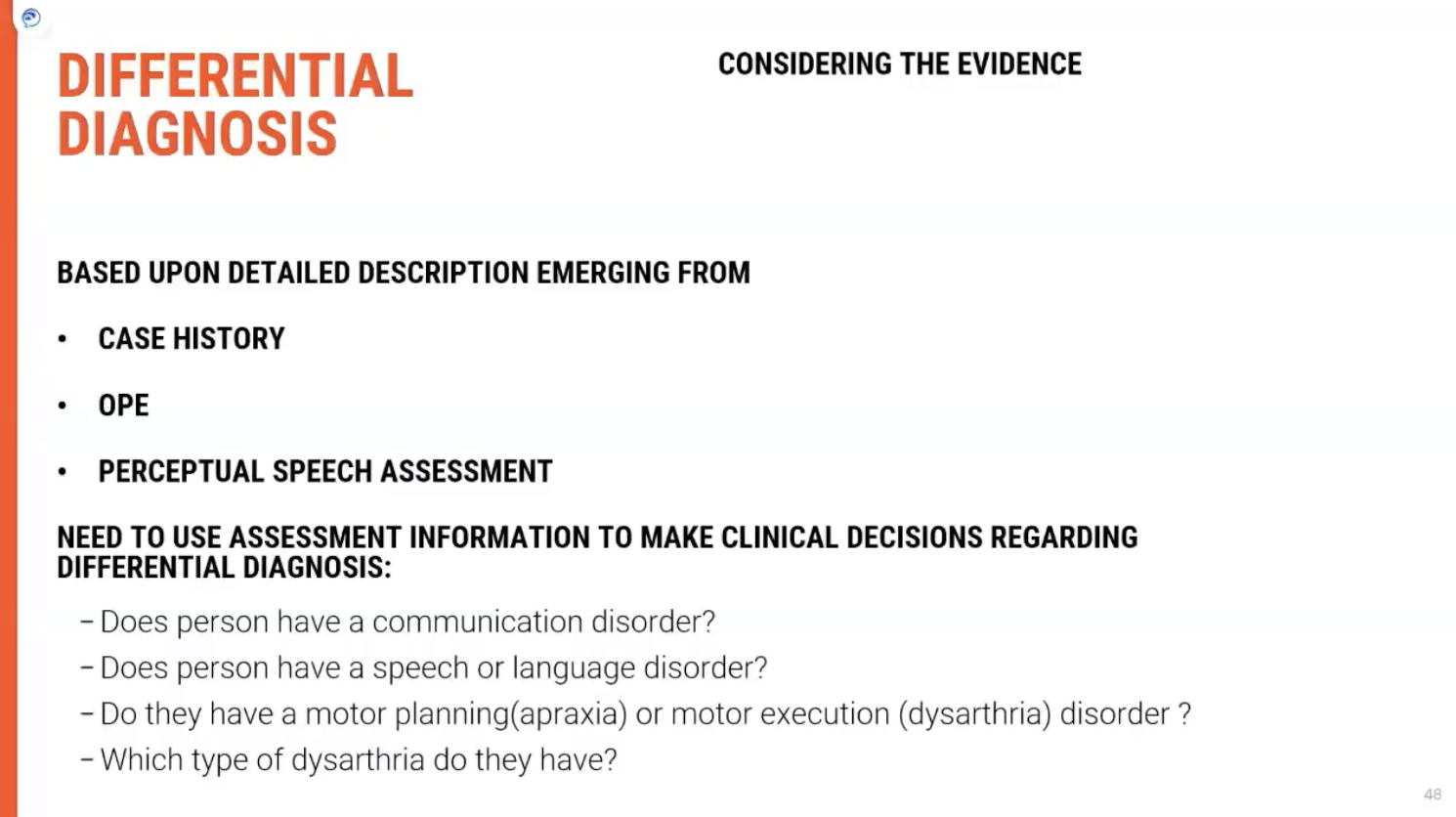
Differential Diagnosis
1/5
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
6 Terms
Comprehensive Diagnosis of Dysarthria
Comprehensive Diagnosis of Dysarthria
Key Features of Dysarthria Diagnosis
Diagnosing dysarthria involves more than a single assessment. A holistic approach is necessary, considering various factors:
Information Gathering: Diagnosis is informed by detailed patient history and clinical information.
Neurological Signs: The presence or absence of additional neurological signs and symptoms plays a crucial role in diagnosis.
Elements Contributing to Diagnosis
Each element must be explored in greater detail to accurately diagnose and differentiate dysarthria subtypes:
Patient History:
Importance: A thorough history helps to identify underlying causes such as stroke, trauma, or neurological diseases (e.g., Parkinson's).
Crossover: History often overlaps with symptoms, providing insights into whether progressive conditionsor acute events are responsible.
Clinical Examination:
Neurological Assessment: The clinician checks for signs of weakness, tone abnormalities, or reflex changes.
Speech Evaluation: Detailed speech assessments look at the dimensions of pitch, loudness, articulation, and resonance.
Presence of Other Symptoms:
Neurological Signs: Symptoms like tremors, muscle weakness, or coordination issues give clues about the type of dysarthria.
Integration: Observing how these signs interact with speech impairments helps refine the diagnosis.
Key Takeaway
A comprehensive diagnosis of dysarthria is based on multiple factors, not just a single assessment. This includes history, clinical examination, and neurological signs, with a focus on identifying the root cause and tailoring interventions accordingly.
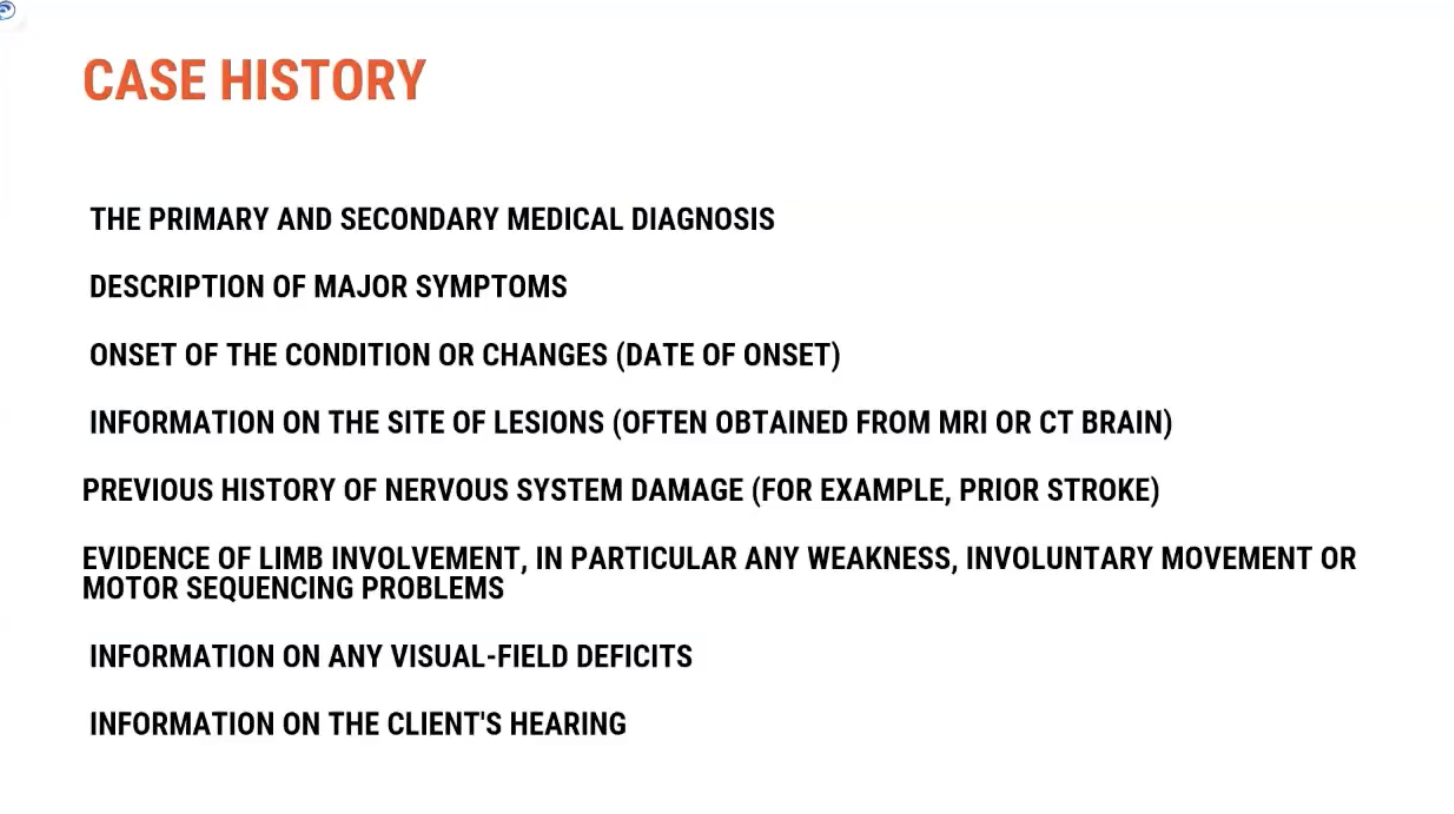
Case History in Dysarthria Diagnosis
Key Information to Collect
The case history is a critical starting point in diagnosing dysarthria. It is typically gathered through discussions with the client, family members, the multi-disciplinary team, and by reviewing medical records.
Important Aspects of Case History
Secondary Medical Diagnosis:
Medical Background: Collect information on any previous diagnoses, especially neurological conditions (e.g., stroke, Parkinson's).
Onset of Symptoms: Note the date of onset and any changes in symptoms over time. 📅
Site of Lesion: Understanding the location of brain damage (e.g., brainstem, motor cortex) helps refine the diagnosis.
Details on Symptoms:
Primary Symptoms: Ask questions to understand the nature of the speech problem, such as "Tell me about how your speech is going?"
Changes in Speech: Clients might report slurring, thick tongue, or mumbling, which indicate specific issues:
"My tongue feels really thick": Suggests weakness in tongue movement, possibly indicating flaccid dysarthria or lower motor neuron damage.
"People tell me I'm mumbling": May point to rigidity or reduced motor movement, a hypokinetic presentation like in Parkinson’s disease.
"My jaw feels tight": Suggests increased tone and spasticity, often linked to bilateral upper motor neuron damage. 🔥
Clinical Observations
The descriptions provided by clients can lead to preliminary hypotheses about the type of dysarthria and its underlying cause:
Weakness in Speech: Indicative of flaccid dysarthria, potentially linked to lower motor neuron issues.
Rigidity and Reduced Movement: Common in hypokinetic dysarthria, often due to basal ganglia dysfunction(e.g., Parkinson’s).
Increased Tone: A sign of spastic dysarthria, related to upper motor neuron damage.
Key Takeaway
Gathering a comprehensive case history is crucial for identifying the type of dysarthria and its underlying cause. Client reports on speech changes, combined with neurological signs, help clinicians form a preliminary diagnosis to guide further assessments.
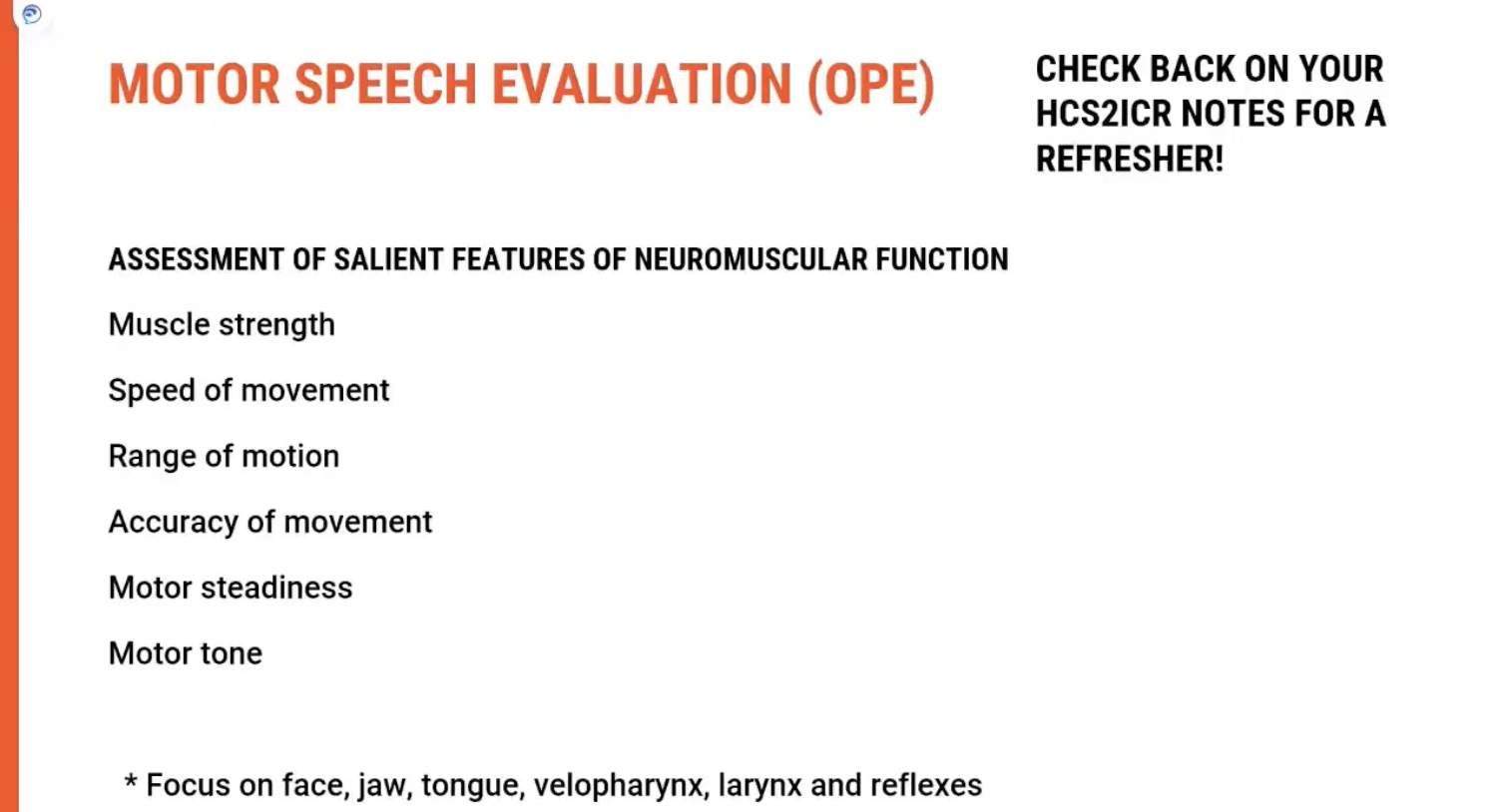
Motor Speech Evaluation
Purpose of the Evaluation
Once the case history is completed, the next step is to conduct a motor speech evaluation to assess the neuromuscular function of the client. The goal is to get an overall picture of the motor speech system, considering various factors such as muscle function, strength, and coordination.
Key Areas to Assess
Muscle Function:
Strength: Evaluate the strength of muscles involved in speech production (e.g., tongue, lips, and jaw).
Speed of Movement: Assess how quickly muscles move, as slow or laboured movements may indicate motor issues.
Range of Motion: Look at how well muscles move through their full range, especially in areas like the lips, tongue, and jaw.
Accuracy of Movement: Determine if movements are precise and controlled, which is critical for articulation.
Steadiness:
Assess muscle steadiness to check for tremors or involuntary movements that might impact speech.
Timing of Muscular Movements:
Evaluate whether muscles can contract and relax at the appropriate times to create smooth, coordinated speech. Timing issues can affect the flow of speech.
Neuromuscular Function Focus
Key Muscles to Evaluate:
Face: Includes the lips and jaw.
Tongue: Look for issues with movement or strength.
Velum (Soft Palate): Check for velopharyngeal function (important for resonance).
Pharynx: Evaluate for swallow-related issues that may also impact speech.
Larynx: Important for voice production (pitch, volume, quality).
Reflexes:
Check for gag reflex or cough reflex, as abnormalities can point to neurological impairments.
Key Takeaway
A motor speech evaluation provides a comprehensive overview of the neuromuscular system involved in speech. By assessing factors like strength, range of motion, and timing, clinicians can identify impairments that may be affecting speech production. Any impairment in these areas will directly impact the motor speech system.
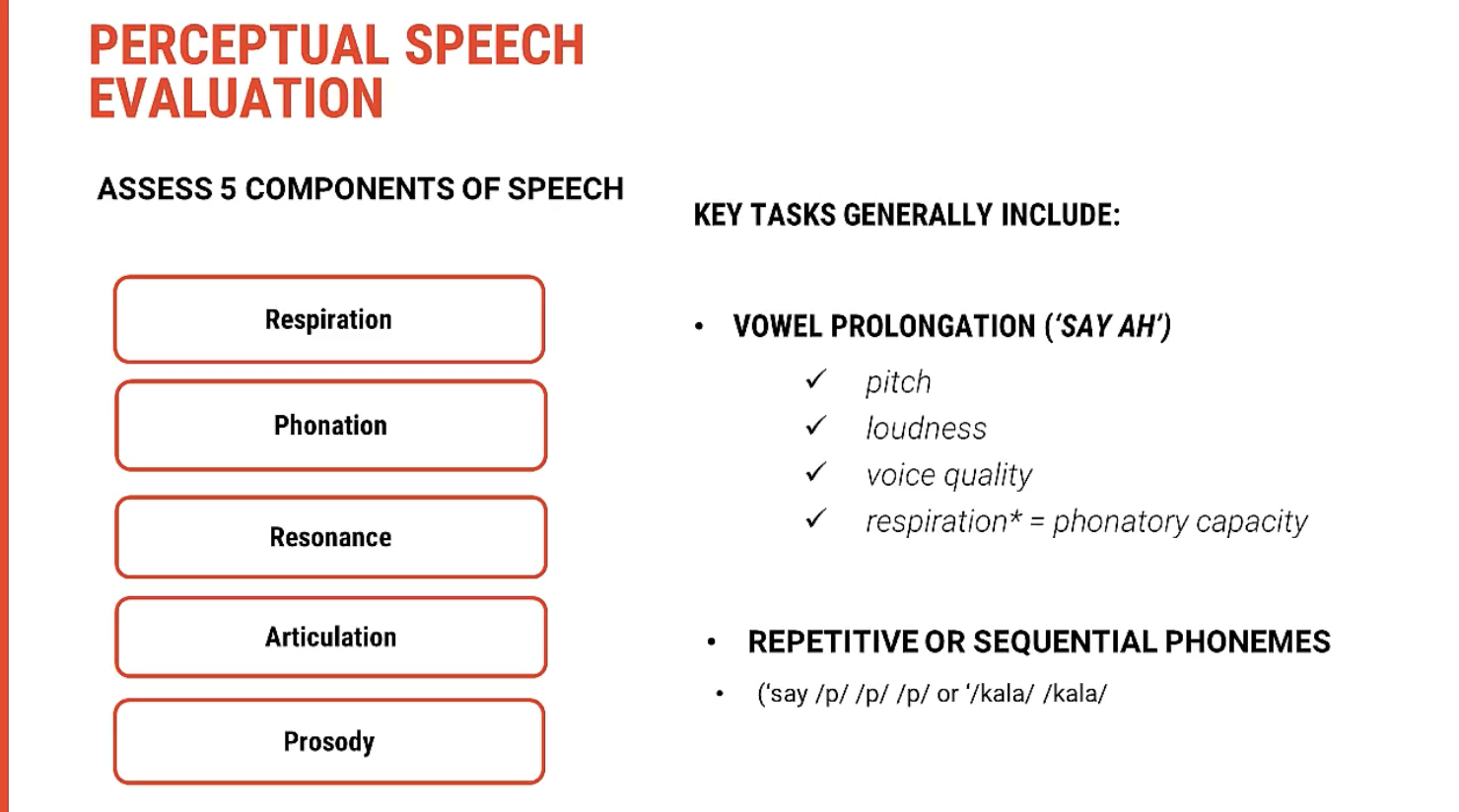
Perceptual Assessment in Dysarthria Diagnosis
What is Perceptual Assessment?
Perceptual assessment involves the systematic observation and listening to the client’s speech to identify distinctive features across different motor speech subsystems. These subsystems include:
Respiration
Phonation
Resonance
Articulation
This approach is often referred to as perceptual centering, and it's essential for evaluating the speech production system from a clinical perspective.
Primary Focus Areas in Perceptual Assessment
Respiration:
Breathing Patterns: Observe the client’s ability to initiate and maintain steady breath support for speech.
Speech-Related Breathing: Look for shallow breathing or shortness of breath, which could affect speech duration and clarity.
Phonation:
Voice Quality: Listen for abnormalities in the pitch, loudness, and quality of the voice.
Harshness or Breathiness: These could signal issues with the larynx (vocal fold dysfunction).
Monotony: In hypokinetic dysarthria, clients might exhibit a flat, monotone voice.
Resonance:
Hypernasality or Hyponasality: Evaluate whether there is excessive nasality in the voice, often associated with velopharyngeal insufficiency.
Normal Resonance: Ensure that the voice is resonating in the correct oral and nasal cavities.
Articulation:
Precision of Speech Sounds: Listen for clear and precise articulation of consonants and vowels.
Slurred or Imprecise Speech: Ataxic dysarthria might cause a lack of coordination in articulation.
How Perceptual Assessment Works
During the perceptual assessment, clinicians will typically listen to the client's speech, observing key aspects of speech production across the subsystems. Speech tasks (e.g., reading passages, repeating sentences) help identify areas of impairment. By listening and observing, clinicians can gather qualitative data on:
Speech patterns
Motor function (movement and coordination)
Impairments in speech subsystems
Key Takeaway
Perceptual assessment is a vital tool in understanding a client’s speech and motor speech subsystems. By evaluating features like breathing, phonation, resonance, and articulation, clinicians can diagnose dysarthria more effectively. This listening and observing process provides clinically valuable insights into the neuromuscular function underlying speech production.
Role of Additional Conventions in Differential Diagnosis
Why Additional Conventions Are Important
Along with the motor speech evaluation and perceptual assessment, additional conventions or methods are used to make a more accurate differential diagnosis. These conventions help identify specific neurological conditions or diseases that may be contributing to the dysarthria.
What Are Additional Conventions?
Physical Inspection:
Non-Specific Muscle Weakness: A physical inspection can reveal muscle weakness, which may not be directly noticeable in speech but is evident upon examination.
Muscle Atrophy: Visible signs of muscle wasting or reduced size could indicate lower motor neuron damage or peripheral nerve issues.
Facial Muscles: Observing the strength and movement of facial muscles can help detect issues in cranial nerve function that affect speech articulation.
Reflex Testing:
Reflex testing helps identify neurological dysfunction. Abnormal reflexes can provide additional clues about the site of the lesion (e.g., brainstem, spinal cord, or motor cortex).
Gag Reflex: The presence or absence of a gag reflex can indicate issues with cranial nerve function, particularly the glossopharyngeal (IX) and vagus (X) nerves.
Jaw Jerk Reflex: Hyperactivity of this reflex might suggest upper motor neuron lesions or conditions like spasticity.
Non-Speech Tasks:
Non-speech oral movements (e.g., blowing, puckering lips, smiling) help assess muscle strength and coordination beyond just speech.
Tongue Movements: Observing protrusion and lateralization of the tongue can help pinpoint issues like weakness or incoordination.
Key Takeaway
Additional conventions such as physical inspection, reflex testing, and non-speech tasks provide valuable insight into the neurological condition affecting speech. These methods complement motor speech evaluations and perceptual assessments by identifying specific muscle weaknesses, nerve involvement, and reflex abnormalities, which are essential for making a differential diagnosis.
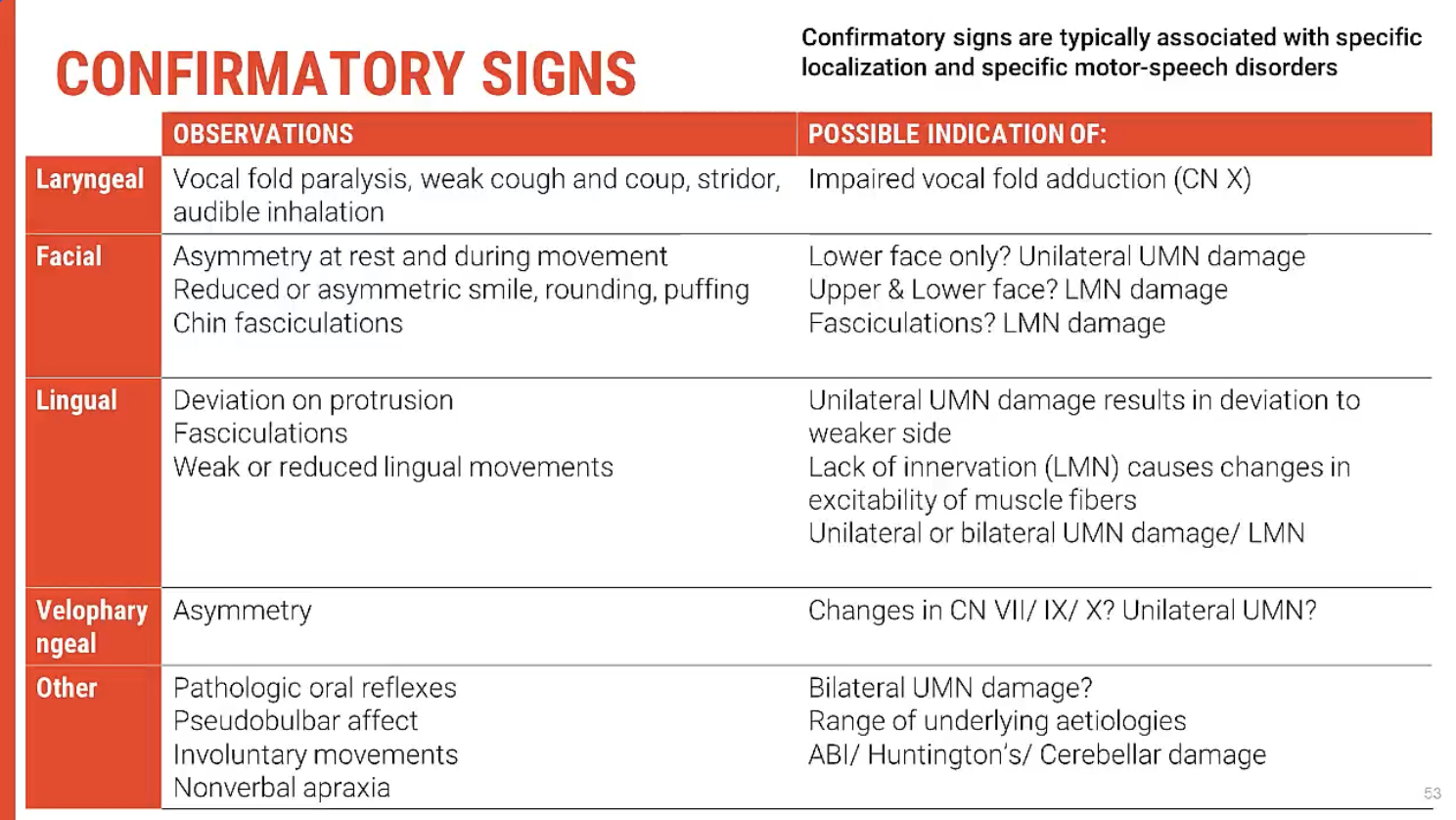
Additional Conventions for Diagnosing Motor Speech Disorders
Key Signs to Look for in Speech System
When conducting a more thorough evaluation, clinicians will observe specific signs in the speech system that may indicate underlying neurological disorders. These signs help in refining the diagnosis and pinpointing the type of motor speech disorder:
Atrophy or Muscle Weakness:
Facial Muscle Atrophy: Visible loss of muscle bulk, especially around the face, jaw, or tongue, which may suggest lower motor neuron damage.
Tongue Weakness: Difficulty moving the tongue may be indicative of flaccid dysarthria or cranial nerve damage.
Fasciculations:
Muscle Twitching: Fasciculations or involuntary muscle twitching can be a sign of lower motor neurondisorders like amyotrophic lateral sclerosis (ALS).
Inappropriate Emotional Responses:
Pseudobulbar Affect: Poorly controlled laughing or crying that is out of context can indicate damage to the corticobulbar pathways. This often appears in conditions like ALS or Parkinson's disease.
Signs from Non-Speech Systems
In addition to observing the speech system, it is important to assess non-speech motor functions. These visual signs or reflex responses can provide further diagnostic clues:
Muscle Stretch Reflexes:
Hyperactive Reflexes: Overactive reflexes, especially in the limbs, can indicate upper motor neuron involvement.
Superficial and Plantar Reflexes:
Abnormal Reflexes: Babinski's sign (toes fanning out when the sole is stroked) could suggest upper motor neuron damage.
Hyperactive Limb Reflexes:
Exaggerated Responses: Increased reflexes may point to conditions such as spasticity or corticospinal tract damage.
Limb Atrophy:
Loss of Muscle Mass: This could suggest lower motor neuron damage or conditions like polio or peripheral neuropathy.
Fasciculations in Limbs:
Involuntary Muscle Twitching in the limbs, much like in the speech system, may indicate motor neuron disease.
Key Takeaway
By observing signs and symptoms such as atrophy, fasciculations, and abnormal reflexes, clinicians can gain confidence in their differential diagnosis of motor speech disorders. These nonspeech system observations help identify specific neurological manifestations, improving diagnostic accuracy and assisting in selecting the most appropriate treatment.