Bone Histology
1/27
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
28 Terms
What is the calcified matrix composed of?
minerals (65%): mostly calcium hydroxyapatite crystals,
organic matter :
type I collagen,
sulphated glycoproteins, and
proteoglycans (including bound water)
What are the functions of bones
Support and protection for the body and its organs.
Reservoir for calcium and phosphate ions.
Plays an important role in hematopoiesis
HOw are bones classified?
according to shape;
location of spongy and compact bone varies with shape
Describe the structure of the long bone
In shaft:
entire thickness of bone tissue = compact, (only small portion = spongy), which faces the marrow cavity.
At ends:
most of the bone is spongy, and only the outer shell of bone is compact.
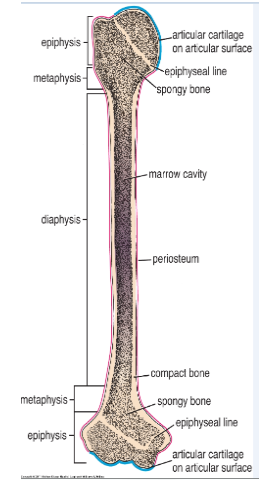
Describe the structure of short, flat, and irregular bones
Short
equal in length and diameter.
carpal bones in hand.
Flat
thin and plate-like,
consist of two layers of thick compact bone; intervening layer of spongy bone.
bones of the skull.
Irregular bones,
contain air sinuses
vertebrae, ethmoid bone
Describe what is on the outer surface of bone? What are the two layers of this? Describe each layer? How is collagen arranged? Exeption?
covered by periosteum (except in areas covered by articular cartilage)
sheath of dense connective tissue consisting of:
outer fibrous layer
inner cellular layer
contains osteoprogenitor cells.
more prominent in growing bone.
/
/
Collagen fibers = parallel to bone surface
except at tendon/ligament’s attachment
here, collagen fibers extend directly into bone tissue
This is called Sharpey’s fibers
What is inside the bone cavity (aka marrow cavity) of both compact/spongy bones? Describe this layer.
How is the marrow cavity different in adults/ kids?
lined by endosteum,
a layer of connective tissue containing
osteoprogenitor cells (can → osteoblasts and bone–lining cells.)
Younger people/kids:
marrow cavity contains red bone marrow → later replaced by yellow bone marrow (fat)
red b/c blood cells in different stages and reticular fiber network
Adults:
red bone marrow is restricted to spaces of spongy bones at a few places in the body,
ex: sternum and the iliac crest
site for taking diagnostic bone marrow samples
What are the five types of cells associate with bone tissues; how are osteoclasts different than the rest of these cell types
Osteoprogenitor cells,
Osteoblasts,
Osteocytes,
Bone lining cells
Osteoclasts.
Similarities (except for OSTEOCLASTS):
differentiates from mesenchymal stem cell
all transform from less mature → more mature form (bone growth)
ONLY OSTEOCLASTS:
originates from granulocyte / monocyte progenitor
responsible for bone resorption , an activity associated with bone remodeling.
What is osteogenesis? Where are Osteoprogenitor found? Describe their cell type/structure
Process of new bone formation
requires osteoprogenitor cells
responsive to molecular stimuli → transformation into bone-forming cells
Osteoprogenitor cells location:
periosteal and endosteal
microvasculature of bone. ( Harversian &
Volkmann's canals)
flattened or squamous-shaped cells with a very lightly staining oval nucleus and a pale cytoplasm. EM reveals rER and free ribosomes
What are osteoblasts and their functions. Describe their cell type. how do they communicate? What receptors do they possess
Differentiated Bone-forming cells
Function:
secrete bone matrix (type I collagen) and bone matrix proteins (BMPs),
constitute the initial unmineralized bone or osteoid.
responsible for the calcification of the bone matrix
communicate with other osteoblasts/ osteocytes by gap junctions.
possess Parathyroid hormone receptors, estrogen, and progesterone on cell membrane
Histology:
Under the light microscope, osteoblasts appear as cuboidal or polygonal in shape and in a single layer lying in apposition to the forming bone.
cytoplasm is intensely basophilic because of an extensive rER.
What are osteocytes and their function; what happens when they die; what space do they occupy? What do they possess
Osteocyte = osteoblasts surrounded by osteoid or bone matrix
Function:
Maintain bone matrix via synthesizing or degrading
Death (like fracture):
resorption of bone by osteoclasts → repair or remodeling by osteoblast activity
occupies a space or lacuna that conforms to the shape of the cell.
has cytoplasmic processes, → extend through canaliculi → contact processes of neighboring osteocytes and bone lining cells by means of gap junctions.
what are bone-lining cells derived from? Function? What are they called when on the external/internal side
from osteoblasts
cover bone that is not remodeling.
external = periosteal cells,
internal = endosteal cells
What are osteoclasts responsible for? Where are they found? what happens to the location that osteoclasts occupy? How are they created? What are their three zones? Whats on their cell membrane
responsible for for bone resorption.
large multinucleated cells, found at sites where bone is being removed.
rest directly on the bone tissue where
resorption is taking place.result of activity = shallow bay called a resorption bay or Howship’s lacuna forms under osteoclasts
exhibit 3 specialized zones: ruffled border, clear zone, basolateral region
created by fusion of mononuclear hemopoietic progenitor cells under influence of cytokines.
Newly formed osteoclasts undergo an activation
process to become bone–resorbing cells.
has calcitonin receptors
histology: marked acidophilia and exhibits a strong histochemical reaction with acid phosphatase because of the numerous
What are the three functions of osteoclasts
Bone remodeling by the process of bone turnover.
Proper shaping of the bone.
Enlargement of the medullary spaces to enable hematopoiesis
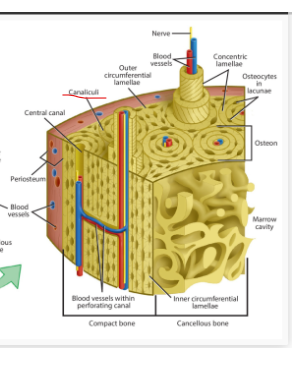
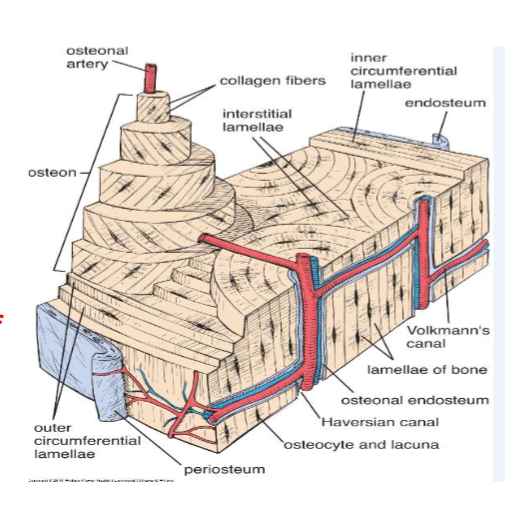
What is the fundamental units of mature compact bone? Describe the parts of this unit
(composed of? Between ___ =? What mature bone also called?
composed of cylindrical structural units called osteons (Haversian systems).
consists of concentric lamellae of
bone matrix surrounding a central canal, called
the osteonal (Haversian ) canalcontains blood vessels/ nerves of osteon.
Between osteons = interstitial lamellae.
Remnants of previous concentric lamellae
Because of the lamellar arrangement, mature
bone is also called lamellar bone.
NOTE: Lamellae: a thin layer, membrane, or plate of tissue, especially in bone.
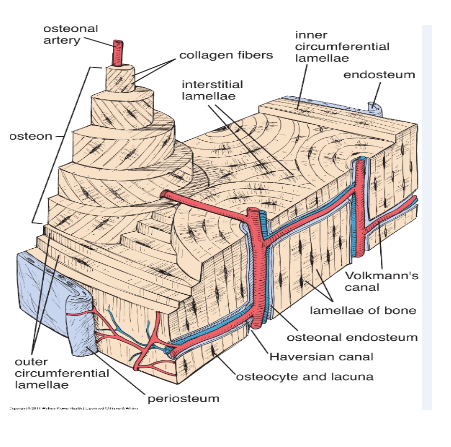
What and where are canaliculi; function?
Canaliculi:
contain processes of osteocytes
arranged in radial pattern around Haversian canal
serves for the passage of substances
between osteocytes and blood vessels.
Describe the orientation of osteons? Orientation of collagen fibers on osteon? What benefit does this arrangement give?
Orientation:
long axis of osteon parallel to long axis of bone.
Collagen fibers in osteon parallel to one another but in different directions from adjacent lamellae.
arrangement gives the cut surface of lamellar bone the appearance of plywood and imparts
great strength to the osteon
where could lamellar bone also could be found? WHat is the orientation of this?
Circumferential lamellae also follow the entire inner and outer circumference of the shaft of a long bone, appearing much like the growth rings of a tree.
What are vokmann’s channels? What do they connect? What is a key histological feature of these channels
channels in lamellar bone through which neurovasculars travel from periosteal/endosteal → haversian canal.
connect Haversian canal and run at right angle to long axis of osteon/bone.
Histological identification: Volkmann’s canals are not surrounded by concentric lamellae
Describe mature spongy bone
(AKA? Example? Surrounded by? Similar? Except? Matrix?)
AKA: cancellous bone
e.g., present inside the epiphyses of long bones
surrounded by compact bone.
structurally similar to mature compact bone EXCEPT:
tissue is arranged as trabeculae or spicules, and numerous interconnecting marrow spaces of various sizes are present between the bone tissue.
The matrix of the bone is lamellated.
how does immature bone differ from a mature bone? Where is immature bone found in adults?
does not display an organized lamellated appearance (AKA: non-lamellar bone)
AKA: bundle bone or woven bone b/c interlacing arrangement of the collagen fibers.
contains more cells per unit area
Cells in immature bone = randomly organized,
matrix has more ground substance
Mature bone = main type in adult
immature bone in adults = where bone is being remodeled
at insertion of tendons
in alveolar sockets of the teeth .(orthodontic corrections)
HIstological Differences:
matrix in immature bone stains more intensely with hematoxylin
Immature bone forms more readily than mature bone
matrix of compact bone stains more intensely with eosin.
What are the two types of bone development
endochondral (cartilage precursor)
bones of extremities and parts of the axial skeleton
intramembranous ossification (without cartilage model).
flat bones of the skull & face, mandible, and clavicle
Describe the mechanism of intramembranous ossification
(when? Formation of? Mechanism? as process continues?)
begins at 8th week of gestation.
bone formation by mesenchymal cells → osteoblasts
Mesenchymal cells migrate and aggregate at
specific areas →condensation of mesenchymal cells (ossification centers) → starts intramembranous ossification.
as process continues:
site = vascularized
aggregated mesenchymal = larger /rounder
osteoprogenitor cells’ cytoplasm = more basophilic, golgi areas = more evident
these changes result in a differentiated osteoblast
secretes type I collagen/ other comparments of bone matrix
Histology: Newly formed bone matrix appears in histologic sections as small, irregularly shaped spicules and trabeculae.
how does intramembranous ossificaiton lead to appositional growth
(matrix? osteocyets? spicules? cells that does not undergo this?)
With time:
matrix is calcified
osteoblasts → osteocytes w/ their cytoplasmic
processes connecting with neighboring osteocytes.bony spicules increase in size and forms woven bone or intramembranous bone.
Mesenchymal regions that do not undergo ossification give rise to endosteum and periosteum.
describe the mechanism of enchondral ossification
(relies on? Forms? center chondrocytes? osteoblasts/osteoclasts?)
relies on hyaline cartilage model,
template within which the bone is made.
forms bony subperiosteal collar around midriff of template → increases in length/width
chondrocytes in center of template:
hypertrophy and resorb matrix
enlarges their lacunae → become confluent.
hypertrophied chondrocytes → assist in calcification of cartilage → later dies
newly formed spaces are invaded by the periosteal bud
composed of blood vessels, mesenchymal cells, and osteoprogenitor cells
osteoprogenitor → osteoblasts → lay a bony matrix on the surface of calcified cartilage.
As subperiosteal bone collar increases in thickness and length: osteoclasts resorb the calcified cartilage–calcified bone complex
leaves an enlarged space → future marrow cavity
describe the growth of endochondral bone:
(occur? spread? what happens to cartilage template? zonation?
occurs in the 2nd trimester of pregnancy → early adulthood.
process will spread away from the primary ossification center
most of cartilage template will be replaced by bone → diaphysis of long bone
distinct zonation in cartilage at both ends of the marrow cavity could be seen as the diaphyseal marrow cavity enlarges → Epiphyseal cartilage
describe the different zones of Epiphyseal cartilage
Describe the secondary ossification center (when? where? Only cartilage remaining?)
Zone of reserve cartilage ( R)
Zone of proliferation (P)
Zone of maturation (M)
Zone of hypertrophy and calcification ( H)
Zone of cartilage degeneration (CD)
Osteogenic zone (O)
Secondary Ossification Center
Shortly after birth, develops in proximal epiphysis.
only cartilage = articular cartilage at end of long bones and as transverse disc of cartilage known as the epiphyseal growth plate
responsible for maintaining the growth process

describe bone remodeling
(what happens? Epiphyseal closure?)
bone = continuously being remodeled.
Harversian canal systems = modified by osteoclastic resorption and osteoblastic bone formation.
epiphyseal closure: When an individual achieves maximal growth, proliferation of new cartilage
within the epiphyseal plate terminates