Endocrine System NoteGuide
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
What are some of the gerontologic considerations for the effects of the aging on the endocrine system?
Decreased production and secretion
Altered metabolism and biologic activity
Decreased responsiveness
Changes in circadian rhythms
Assessment may be difficult
Co-morbid conditions and medications that change body’s usual response
What is Insulin and what does it do?
Insulin is a hormone produced by the cells of pancreases, and it is released into the blood stream to enhance glucose transport from the bloodstream across the cell membrane to the cytoplasm of the cell to be used for energy.
How is glucose stored?
Glucose is stored at glycogen.
Type 1 Diabetes
An autoimmune condition leading to the destruction of insulin-producing beta cells in the pancreas, requiring lifelong insulin. This is commonly diagnosed in childhood or adolescence but can occur at any age.
Type 2 Diabetic
Pancreas continues to produce some endogenous insulin but not enough insulin is produced of the body does not use insulin effectively. This is more common in adults but rising in children due to obesity and sedentary lifestyle.
Type one diabetes genetic link
Strong genetic component linked to HLA types, HLA-DR3 and HLA-DR4 are commonly associated with an increased risk. Additionally some environmental factors such as viral infection can trigger the autoimmune response. Sudden onset
Type 2 Diabetes Genetic link
A family history, an insulin resistance, a decreased production of insulin, an inappropriate glucose production, adipose tissue hormone and metabolic syndrome increase the risk for type 2. Can develop gradually.
What are the classic symptoms of diabetes (1 & 2)?
Polyuria (frequent urination)
Polydipsia (excessive thirst)
Polyphagia (excessive hunger)
What are the clinical manifestations of type one diabetes?
Weight loos, weakness, fatigue and Diabetic ketoacidosis (DKA)
What are the clinical manifestations for type 2?
Fatigue, recurrent infection, recurrent vaginal yeast or candid infection, prolonged wound healing and visual problems
Fasting BG
Blood glucose level after fasting; diagnostic if ≥126 mg/dL on two separate occasions mean type 2 diabetes.
HbA1c
6.5% or high on 2 separate occasion mean types 2 diabetes.
Oral glucose toleranc test
2-hour post OGTT blood glucose 200 mg/dL or higher
Type 1 diabetes drug therapies
Insulin therapy is essential, using short-acting long-acting or continuous pump delivery.
Type 2 diabetes drug therapy
Oral hypoglycemic (metformin, sulfonyureas) and or insulin may also use GLP-1 agonists or SGLT2 inhibitorss.
DKA (Diabetic Ketoacidosis)
A severe complication of diabetes, primarily Type 1, characterized by high blood glucose, ketosis, and acidosis.
Prandial insulin
This is a proactive method of insulin and it is give before meals to cover the rise in blood sugar from eating. It is part of the basal-bolus insulin theraphy.
Insulin storage
Insulin must be stored properly to maintain its effectiveness, typically in a refrigerator; (36-46) however, it can be kept at room temperature for up to 28 days after opening.
Handling Prefilled Syringes (storage)
These can be stored for up to a week and need to be stored in a vertical position with the needle pointing up to prevent insulin from blocking the needle. Additionally the insulin should be rolled with you hands before administering.
Type 1 Insulin Pump
These are continuous subcutaneous infusion of rapid-acting insulin.This is a major advance in keeping the blood glucose in a tighter range. However it is expensive and can increase the risk of infection. (site change every 2-3 days)
What is Lipodystrophy?
This is when there is changes in the fat tissue at the site of repeated insulin injections leading to either hypertrophy (lumps) or lipoatrophy (dents).
What is the Somogyi effect?
This occurs when blood glucose drops too low during the night, and the body responds by releasing stress hormones (like cortisol and adrenaline) to increase blood glucose. The result is that you wake up with high blood sugar levels. Often caused by to much insulin or not enough food.
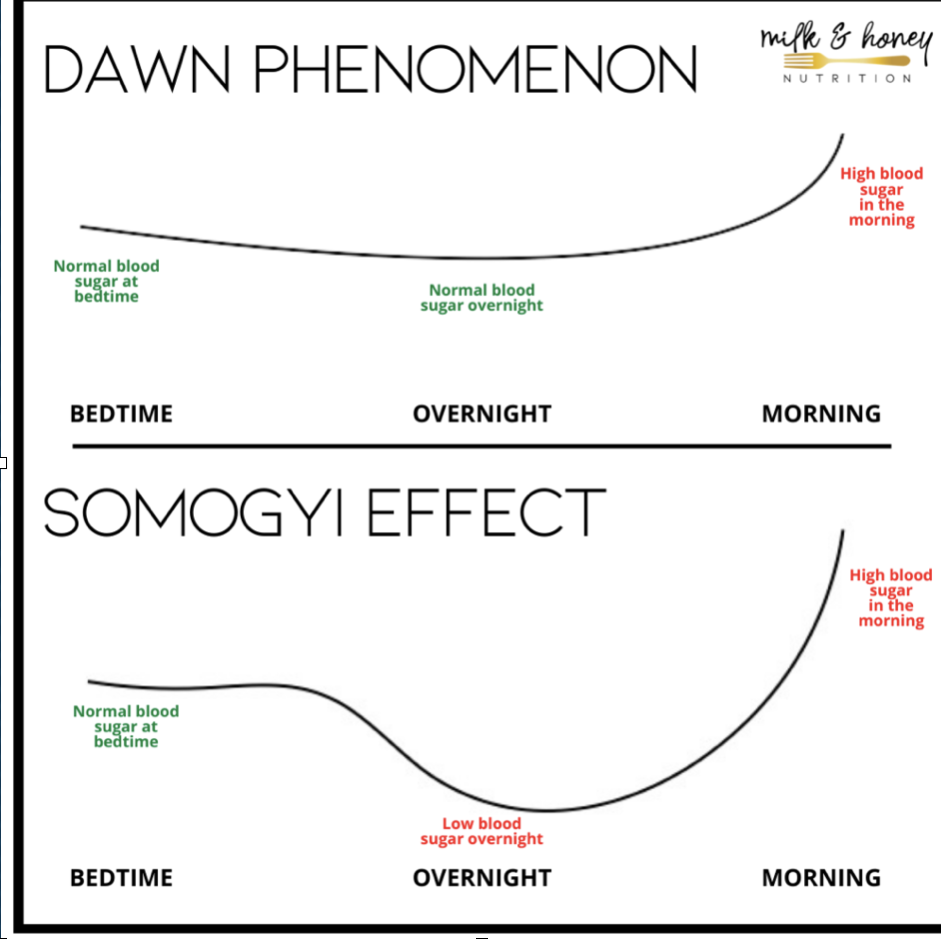
What is the Dawn Phenomenon?
This is a natural rise in blood glucose that occurs in the early morning due to the body releasing growth hormones, cortisol, and other hormones that increase insulin resistance. This is often caused by the natural body rhythms and not necessarily tied to any one behavior or mistake in diabetes management.
Metformin
Function: Increases insulin sensitivity, allowing the body’s cells to use insulin more effectively.
Benefits: Often the first medication prescribed for Type 2 diabetes; can help with weight loss.
Sulfonylureas
Examples: Glipizide, glyburide, glimepiride
Function: Stimulates the pancreas to release more insulin.
Consideration: Can cause hypoglycemia; requires careful monitoring of blood sugar levels.
GLP-1 Agonists
Examples: Liraglutide (Victoza), semaglutide (Ozempic)
Function: Enhance insulin secretion in response to meals, suppress appetite, and slow gastric emptying.
Delivery: Injectable form; some available in daily or weekly doses.
SGLT2 Inhibitors
Examples: Canagliflozin (Invokana), empagliflozin (Jardiance)
Function: Prevents the kidneys from reabsorbing glucose, thus increasing glucose excretion through urine.
Benefits: Also provide cardiovascular benefits in patients with Type 2 diabetes.
Alcohol intake with a diabetic patient
Limit to moderate amount if no risk for other alcohol-related problems
1 drink/day for women; 2 drinks/day for men
Inhibits gluconeogenesis by liver
Can cause severe hypoglycemia (with lots or chronic use of alcohol)
Eat carbohydrates when drinking unless drinks have sweetened mixers
Hyperglycemia causes
Illness, infection
Corticosteroids
Too much food
Too little or no diabetes meds
Inactivity
Emotional or physical stress
Poor absorption of insulin
Emergency Management
First ensure the patients airway is good then administer O2 if needed. Second establish IV access, begin fliu resuscitation until BP stabilized and urine output is at 30mL/hr
Hyperosmolar hyperglycemic state (HHS)
A serious condition characterized by extremely high blood sugar levels and dehydration, often occurring in patients with type 2 diabetes. It may present with confusion, lethargy, and increased urination. Glucose will be more or equal to 600.
What is hypglycemia?
This is when the blood sugar is less than 70 and the body will not have enough energy, this is caused by to much insulin, skipping meals, alcohol intake without food or to much exercise.
Angiopathy
Damage to blood vessels secondary to chronic hyperglycemia. This is the leading cause of diabetes-related death with 68% CVD and 16% stroke age 65 and older
Macrovascular Angiopathy
Diseases of large and medium-sized blood vessels
Cerebrovascular disease
Cardiovascular disease
Peripheral vascular disease
Women are 4-6X risk for CVD while men are 2-3X risk for CVD
Diabetic Retinopathy
High blood sugar damages tiny blood vessels in the eyes. This is caused by long-term high blood sugar levels. This can lead to blurry vision, dark spots and potential blindness.
Diabetic Neuropathy
This is when high blood sugar damages the hand and feet.
Risk for Infection
High blood sugar weakness the immune systems.
Foot and Lower Extremity
Microvascular and macrovascular diseases increases risk for injury and infection (Fig. 48-16 in the textbook)
Sensory neuropathy may cause loss of protective sensation (LOPS) prevents awareness of injury; major risk factor for amputation
Peripheral artery disease (PAD)
Diabetic Dermopathy
This is the most common diabetic complication and it is a red-brown, round or oval patched. Scaly then flat and indented shins.
Acanthuses nigricans
This is a clinical manifestation of insulin resistance. The skin will become velvety, light brown to black and think arounf the flexures, axillae and neck.
What is the thyroid gland?
This is the gland that releases the vital hormone which plays major roles in metabolism, growth and developing. This gland helps to regulate the body by constantly releasing a steady amount of thyroid hormones into the bloodstream.
What do the thyroid hormones regulate?
Regulates the body's metabolic rate controlling heart, muscle and digestive function, brain development, and bone maintenance.
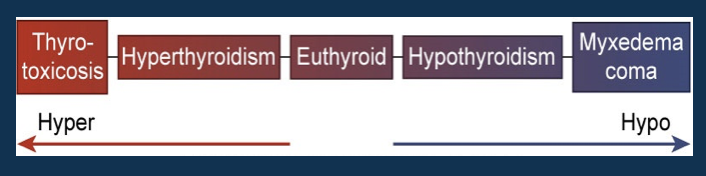
What is the scale for thyroid dysfucntion?
Thyrotoxicosis: Extreme
Hyperthyroidism: Increased
Euthyroid: Normal
Hypothyroidism: Decreased
Myxedema coma: Minimal to none
Hyperthyroidism
A condition characterized by excess production of thyroid hormones,(T3 & T4) leading to increased metabolism. This is often caused by grave disease which is an autoimmune condition which causes the thyroid to enlarge)
Hyperthyroid clinical manifestations
Tremors, hyperrelfexia, anxiety, dyspnea, increase RR, HR, BP, palpitation, murmurs, angina, increased metabolism, fatigue, muscle wasting, increased appetite, diarrhea, warm, fine hair, brittle nails, menstrual changes, decreased libido, bruit possibly heard.
What is exophthalmos and goiter?
Exophthalmos: eyeballs protrude due to an increase in thyroid hormones
Goiter: an enlargement of thyroid gland.
Hyperthyroid Implementation
If exophthalmos present:
Apply artificial tears
Restrict salt
Elevate head of bed
Dark glasses
Tape eyelids closed if needed for sleep
ROM of intraocular muscles
High Calorie diet (4000 to 5000 cal/day)
6 full meals/day with snacks in between
High Protein
High Carbohydrate
Avoid highly seasoned and high-fiber foods
Avoid caffeine products.
What are the three medications for hyperthyroid?
Antithyroid, iodine therapy, B-Adrenergic Blocker
Antithyroid Drug
Propylthiouracil and methimazole (Tapazole)
Inhibit thyroid hormone synthesis
Improvement in 1 to 2 weeks
**Results usually seen within 4 to 8 weeks
Therapy for 6 to 15 months
Iodine Therapy
Potassium iodine (SSKI) and Lugol’s solution
Inhibit synthesis of T3 and T4 and block their release into circulation
Decreases vascularity of thyroid gland, making surgery safer and easier
Maximal effect within 1 to 2 weeks
Iodine is mixed with water or juice and sipped through a straw to decrease teeth staining.
β-Adrenergic Blockers
Symptomatic relief of thyrotoxicosis
Block effects of sympathetic nervous stimulation
Decreases tachycardia, nervousness, irritability, tremors
Propranolol (Inderal)
Atenolol (Tenormin)
Radioactive Iodine theraphy
Swallowed in a single dose, in pill or liquid form
Treatment of choice for most nonpregnant adults
Damages or destroys thyroid tissue
Delayed response of up to 3 months
Treated with antithyroid drugs and β-blocker before and during first 3 months of RAI
Thyroidectomy Post-Op
Thyroid Hormone Replacement: If the entire thyroid gland was removed, educate the patient on the lifelong need for thyroid hormone replacement therapy (e.g., levothyroxine). Emphasize the importance of regular follow-up to adjust dosage as needed.
Calcium Supplements: Instruct the patient on the importance of taking calcium and possibly vitamin D supplements if prescribed.
Thyroid Storm (Thyrotoxicosis) Definition and causes
A severe, life-threatening exacerbation of hyperthyroidism with symptoms like fever and tachycardia, this is often triggered by stressors like infection, trauma and surgery. Common in patients with hyperthyroidism or post thyroidectomy.
Thyroid Storm (Thyrotoxicosis) Manifestations
Severe tachycardia, heart failure, shock
Hyperthermia (up to 106°F / 41.1°C)
Agitation, delirium, seizures, coma
GI symptoms: abdominal pain, vomiting, diarrhea
What is the difference between primary hypothyroidism and secondary hypothyroidism?
Primary hypothyroidism is caused by dysfunction of the thyroid gland itself, leading to insufficient hormone production.
Secondary hypothyroidism occurs when there is inadequate stimulation from the pituitary gland or hypothalamus, often due to a deficiency in thyroid-stimulating hormone (TSH).
Nursing Interventions
Aggressive treatment required
Medications: Block thyroid hormone production & SNS
Monitor for dysrhythmias
Ensure oxygenation, fluid/electrolyte replacement
Promote rest, establish trust, assist with exercise
Provide a calm, non-stimulating environment
Hypothyroidism
Deficiency of thyroid hormone → slows metabolic rate
Primary: thyroid tissue destruction or hormone synthesis defect
Secondary: pituitary (↓TSH) or hypothalamic (↓TRH) dysfunction
Hypothyroidism Etiology
Iodine deficiency
Chronic inflammation (e.g., Hashimoto’s, Graves’)
Post-treatment for hyperthyroidism
Certain drugs
Diagnostics for Hypothyroidism
History & physical exam
TSH: ↑ in primary, ↓ in secondary
T3, T4 low
Thyroid antibodies → autoimmune cause
Labs:
•↑ Cholesterol
•↑ Triglycerides
•↑ Creatine kinase
•↓ RBCs (anemia)
Hypothyroid clinical manifestation
Neuro: Fatigue, mood/personality changes, impaired memory, slowed speech.
Respiratory: Low exercise tolerance, exertional dyspnea.
Cardiac: ↓ Cardiac output/contractility, ↑ cholesterol/triglycerides, anemia.
Metabolism: Cold intolerance, weight gain, slowed metabolism.
Musculoskeletal: Fatigue, weakness, muscle/joint pain.
GI: ↓ Appetite, N/V, constipation, abdominal distention, possible celiac disease.
Skin/Hair/Nails: Dry/thick/cold skin, coarse hair, brittle nails, puffy face, pallor, ↓ sweating.
Reproductive: Irregular or absent periods, ↓ libido, infertility.
Other: ↑ Infection risk, ↑ sensitivity to opioids/anesthetics, ↓ hearing, possible goiter.
Levothyroxine (Synthroid)
A synthetic thyroid hormone used to treat hypothyroidism.
Hypothyroid Complication, triggers Symptoms and treatment
Complication: Myxedema Coma
Triggers: Infection, cold, trauma, drugs
S/S:
Impaired consciousness, mental sluggishness
Subnormal temp, hypotension, hypoventilation
Cardiovascular collapse, puffiness, masklike affect
Treatment:
IV thyroid hormone, respiratory support, cardiac monitoring
Monitor core temperature