Caring for Patients with Cardiovascular Disorders
1/235
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
236 Terms
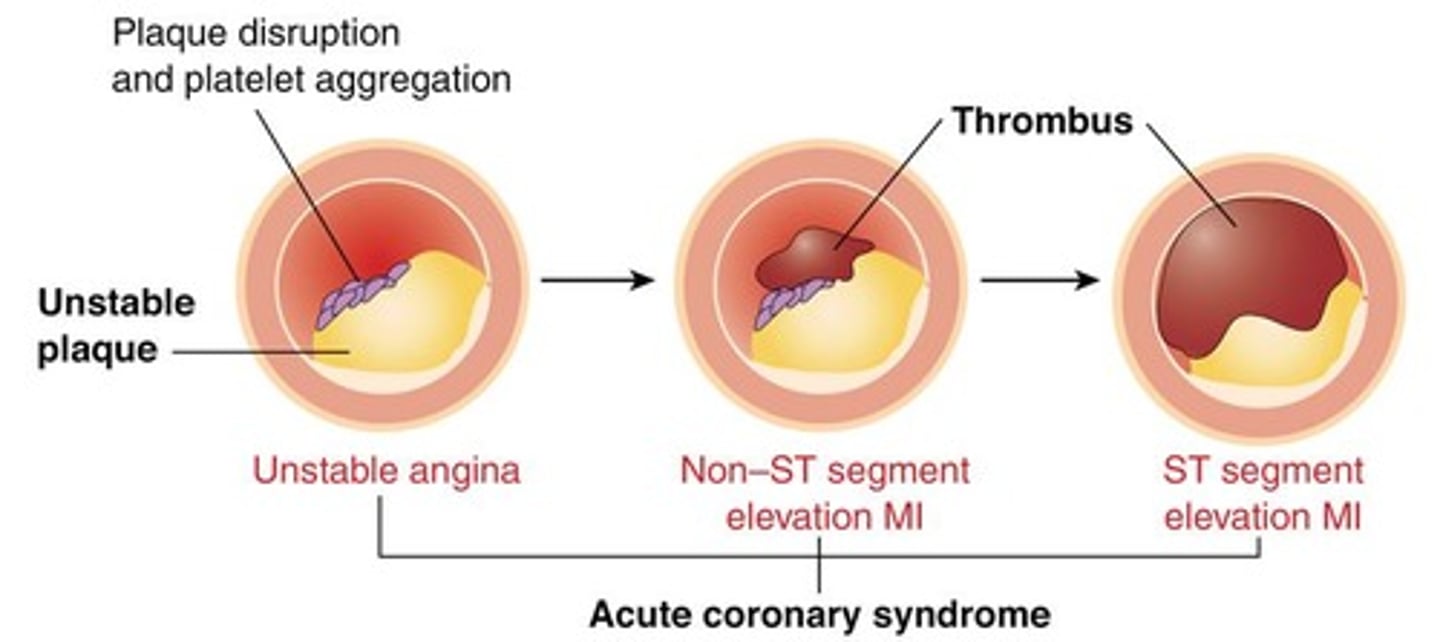
Acute Coronary Syndromes (ACS)
(umbrella term) includes unstable angina, NSTEMI, and STEMI.
Unstable angina
Of the 3- has the most blood flow through the CA.
Non-ST elevation myocardial infarction (NSTEMI)
A heart attack with less blood flow than unstable angina, not blocked off, can become a STEMI patient.
ST elevation myocardial infarction (STEMI)
Most severe form of an MI with no blood flow through the CA, is an emergency.
Heart Failure
(umbrella term) includes acute and chronic heart failure.
Vascular disorders
(umbrella term) includes aortic aneurysm, aortic dissection, and peripheral arterial disease.
Tissue perfusion
Directly related to blood flow and cardiac output (CO).
Coronary artery disease (CAD)
Results from plaques in the arteries.
Diastole
The phase of the heartbeat when the coronary arteries fill.
Tachycardia
Leads to less time in diastole, resulting in less blood flow (O2) to the heart.
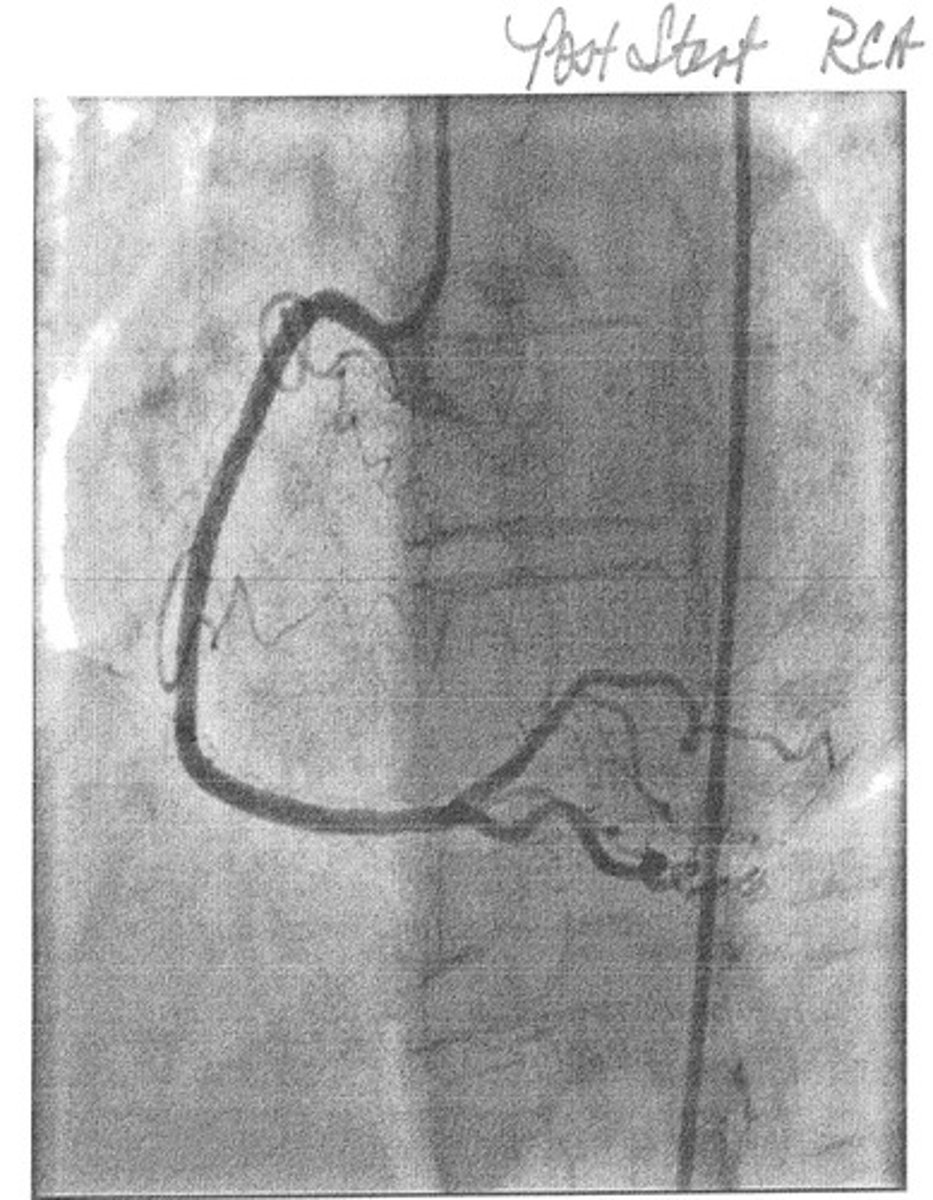
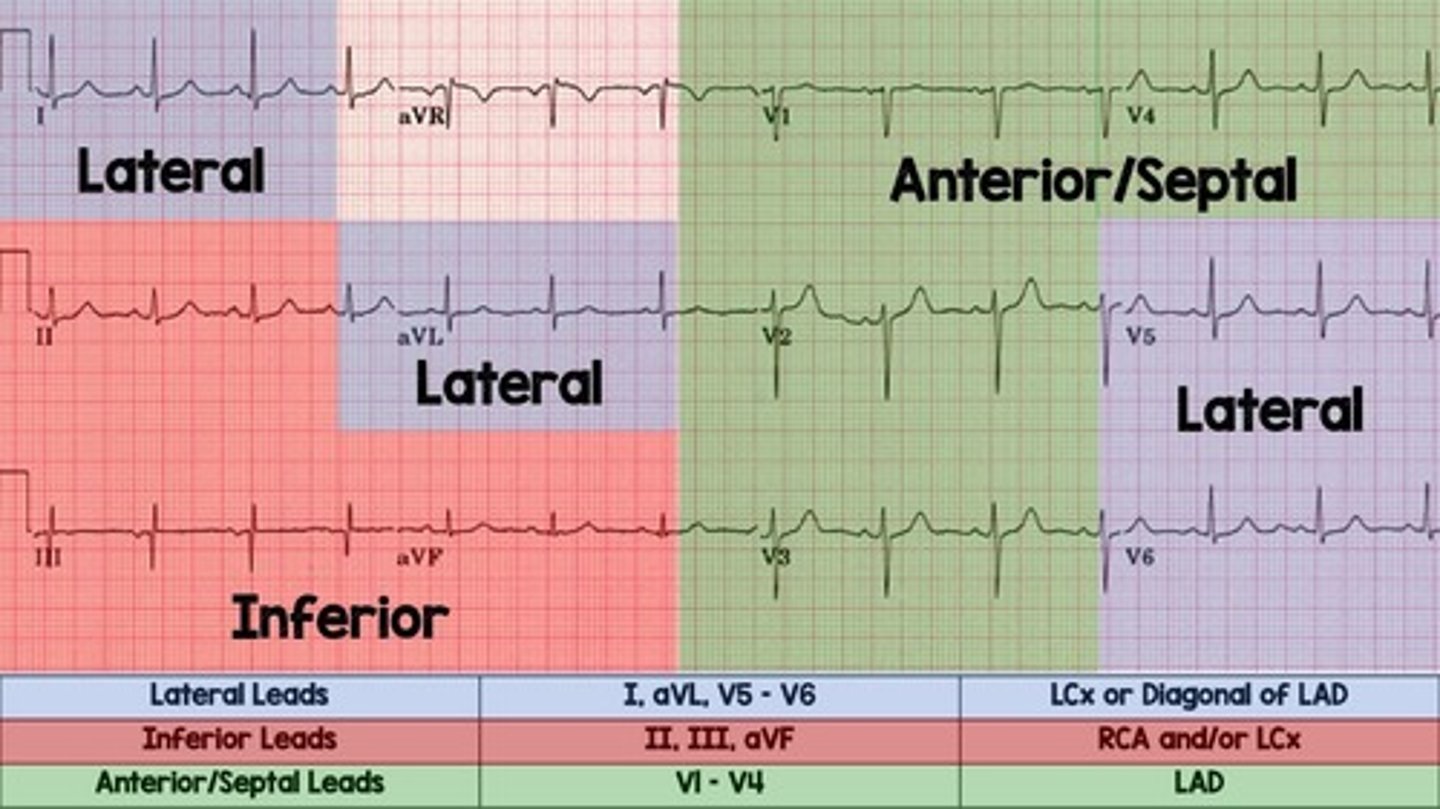
12-lead ECG
Shows different views of the heart corresponding to different coronary arteries.
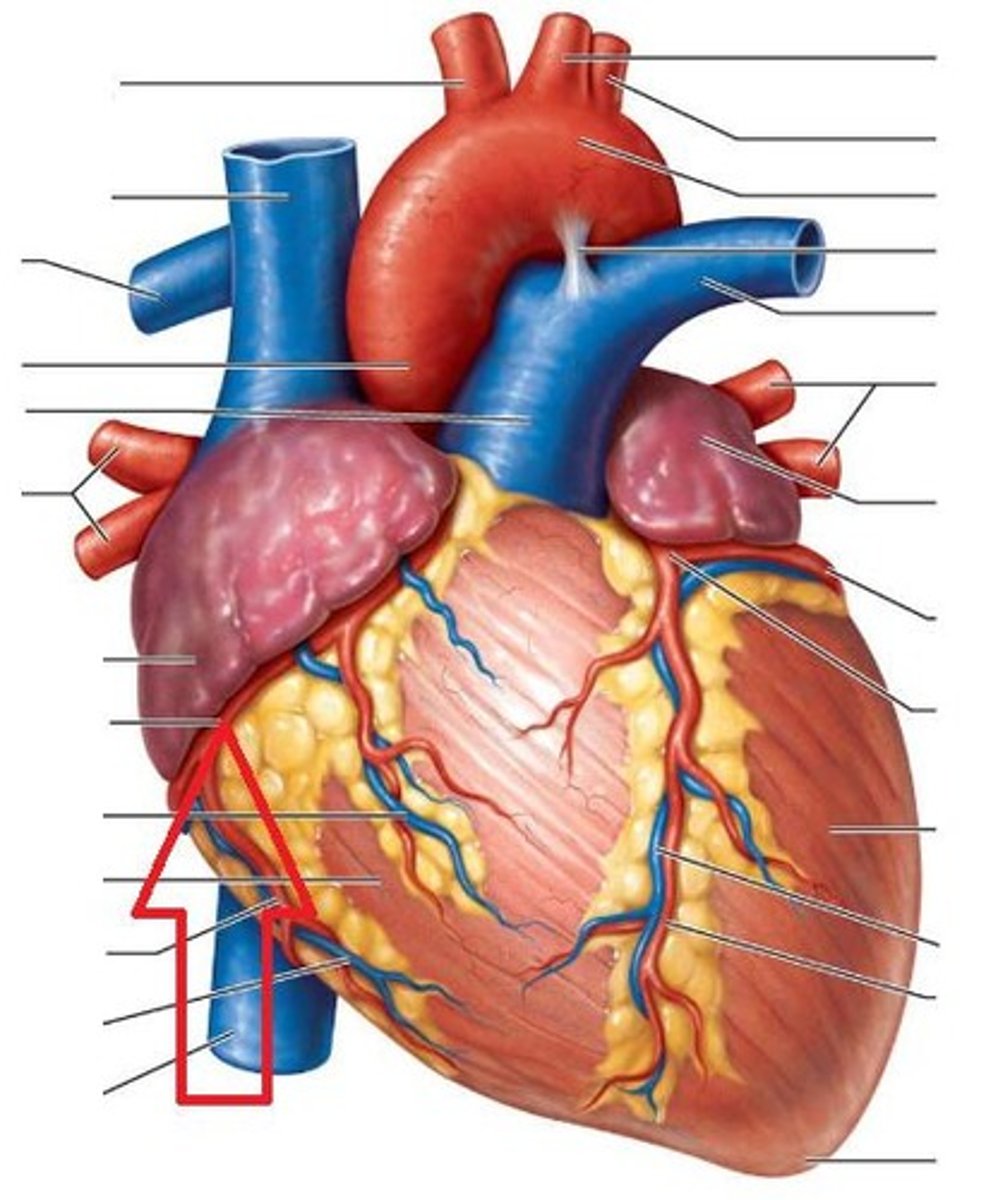
Left Anterior Descending (LAD) Coronary Artery
Supplies blood to the anterior ventricular septum, anterior left ventricle, and ventricular apex.
Circumflex Coronary Artery
Supplies blood to the left atrium, left ventricular lateral wall, and left ventricular posterior wall.
Right Coronary Artery (RCA)
Supplies blood to the right atrium, right ventricle, and inferior and posterior walls of the left ventricle.
Angina Pectoris
Chest pain or discomfort caused by decreased blood flow to the heart.
Stable Angina
Pain that improves with rest; caused by increased demand.
Unstable Angina
Does not improve with rest; requires immediate treatment.
Atypical Angina Symptoms
Common in women, patients over 65, and diabetic patients.
Common Sites for Angina
Presents in different ways, including epigastric pain, heart burn, or fatigue.
Abrupt increase in angina
Increase in frequency, severity, or duration of pre-existing stable angina.
Angina at rest
Angina that is difficult to control with drugs.
Acute Myocardial Infarction
A serious condition where blood flow to the heart is blocked, leading to heart tissue damage.
ST Elevation MI
A type of myocardial infarction characterized by ST segment elevation on an EKG, indicating part of the heart is dying.
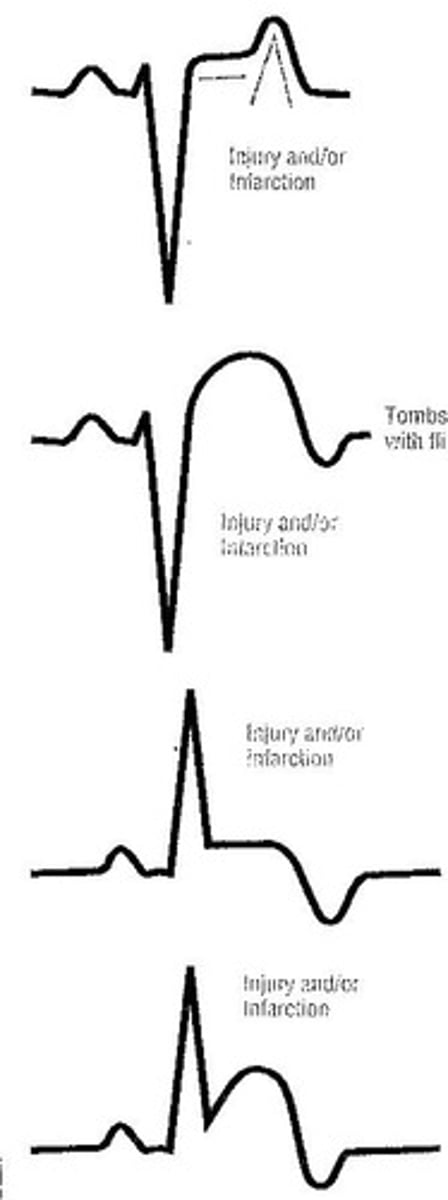
12 Lead Echocardiogram
The GOLD standard for MI diagnosis, used to identify ST segment changes indicative of myocardial infarction.
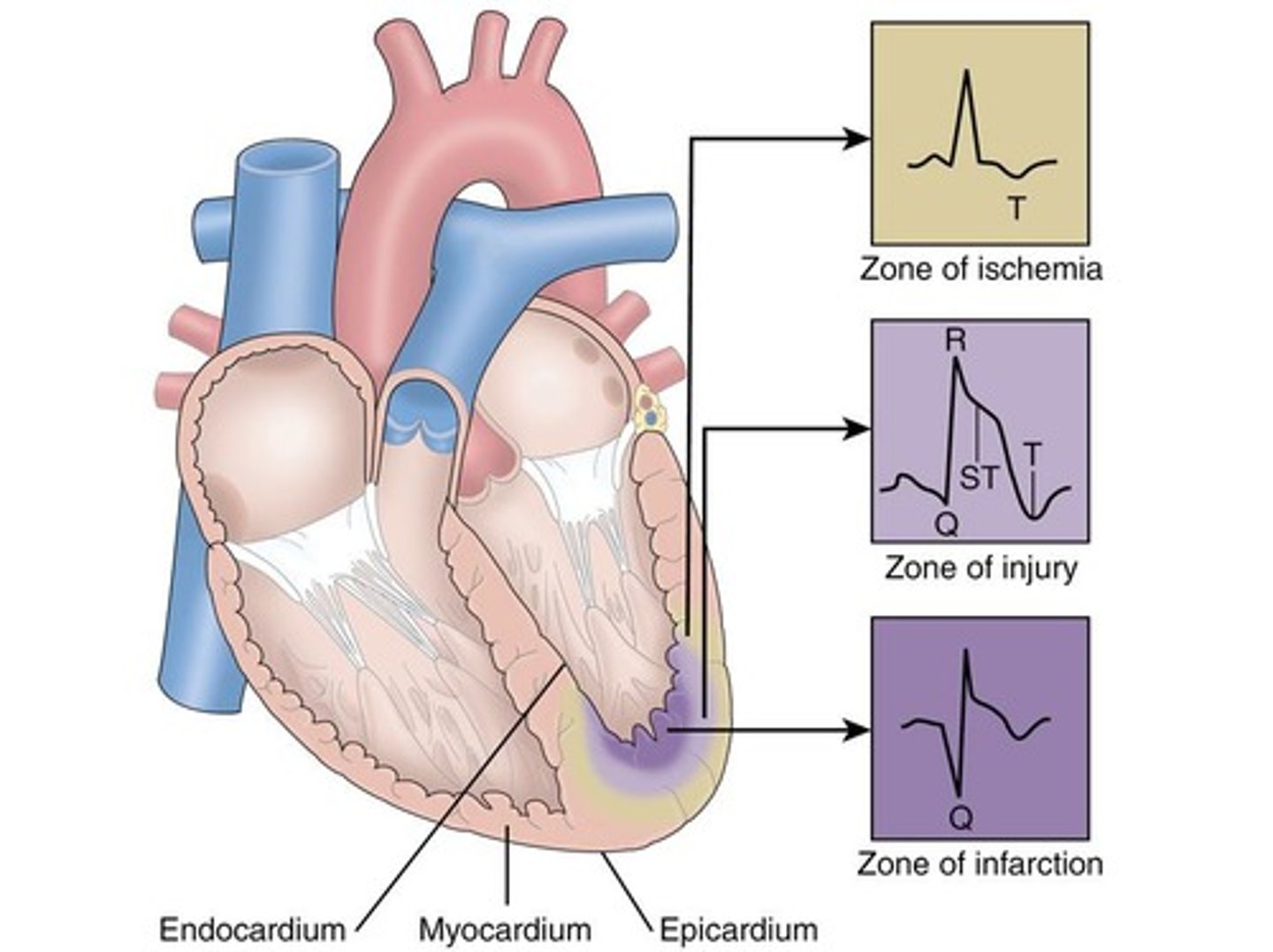
ST Segment Elevation
Indicates that part of the heart is dying; seen in STEMI.
ST Segment Depression
Indicates ischemia, where the heart is receiving inadequate oxygen.
T Wave Inversion
A sign of ischemia on an EKG.
Pathological Q Wave
A widened Q wave that indicates a past STEMI; does not resolve after the event.
Troponins
Cardiac biomarkers released when the heart is injured; elevated levels indicate myocardial injury.
Troponin I
A contractile protein not present in healthy individuals; appears within 3-12 hours after symptoms, peaks at 24 hours, and remains elevated for 5-10 days after AMI.
Troponin T
An isoenzyme released due to myocardial injury; appears within 3-12 hours after injury, peaks at 12-48 hours, and remains elevated for 5-14 days after AMI.
Maintain Cardiac Output
A treatment goal to ensure vital organ and tissue perfusion.
Minimize Cardiac Workload
A treatment goal to restore myocardial oxygen supply-demand imbalance and decrease oxygen demand.
Prevent Complications Associated with AMI
A treatment goal focusing on avoiding dysrhythmias as the primary complication.
Patient and Family Education
Survival teaching provided in the first 24 hours to alert to symptoms.
ST-elevation myocardial infarction (STEMI)
The most serious acute coronary syndrome requiring immediate intervention due to risk of myocardial infarction.
Pain Assessment
An important initial intervention in the ED using a more in-depth pain scale.
Oxygen Therapy
Administered if patient is hypoxemic (O2 sat <90% or in respiratory distress).
Aspirin (160-325 mg)
Administered to diminish mortality rate by reducing platelet aggregation.
Dual Anti-Platelet Therapy (DAPT)
Combination of clopidogrel and ticagrelor to prevent platelets from clumping.
Nitroglycerin
Administered sublingual, spray, or IV to relieve chest pain.
Morphine IV
Administered if pain is not relieved by Nitroglycerin; pain must be zero to indicate no cardiac tissue is dying.
Initial Cardiac Biomarkers
Tests obtained to assess heart injury in the ED.
Portable Chest X-ray
Used to rule out pulmonary embolism or pericarditis.
Dysrhythmias
Common side effect associated with AMI that requires monitoring.
Fibrinolytic Checklist
A review completed in the ED to determine eligibility for thrombolytic therapy.
Cardiac Output
Cardiac Output = Stroke Volume x Heart Rate
Stroke Volume
Stroke Volume is determined by: Preload, Afterload, and Contractility.
Preload
Preload refers to the volume of blood returning to the heart.
Afterload
Afterload refers to the resistance the heart must overcome to eject blood, determined by arterial constriction or dilation.
Contractility
Contractility is the strength of the heart's contraction.
Oxygen Therapy Initiation
Oxygen therapy is initiated if patient is hypoxemic (SpO2 less than 90%), in respiratory distress, or has heart failure.
Hypoxemic
Hypoxemic refers to a condition where oxygen saturation (SpO2) is less than 90%.
Subjective Pain Assessment
Subjective pain assessment includes N: normal, O: onset, P: precipitating/aggravating/relieving factors, Q: quality, R: region/radiation, S: severity/other symptoms, T: timing, U: understanding/perception.
Initial Treatment Measures
Initial treatment measures include bedrest, patient positioning, and avoiding Valsalva maneuver.
Nitrates/Nitroglycerine
Nitroglycerine is a vasodilator that primarily dilates veins and decreases preload.
Net Effect of Nitroglycerine
The net effect of Nitroglycerine includes decreasing preload, decreasing afterload, enhancing coronary artery perfusion, and decreasing myocardial oxygen demand.
Nursing Responsibilities with Nitroglycerine
Nursing responsibilities include monitoring BP, and not giving nitroglycerine if systolic BP is below 90.
Morphine Sulfate
Morphine Sulfate is used for pain relief and preload reduction after nitroglycerine.
ACEIs
ACE inhibitors block the conversion of angiotensin I to angiotensin II, which is a potent vasoconstrictor.
ARBs
ARBs block the receptor site for angiotensin II outside the lungs, thus not causing a cough.
Vasodilation Effect of ACEIs and ARBs
The vasodilation effect due to blockage of angiotensin II results in afterload reduction, lowering systemic vascular resistance (SVR) and blood pressure (BP).
ACEI Administration Timing
An ACEI should be given within 24 hours of admission for an acute MI unless contraindicated.
Contraindications for ACEIs
Contraindications for ACEIs include renal dysfunction, angioedema, or hypotension.
Right Ventricular Infarct
Right ventricular infarct should not receive nitroglycerine as it requires an increase in preload.
Valsalva Maneuver
The Valsalva maneuver stimulates the vagus nerve, leading to decreased heart rate and blood pressure.
Patient Positioning
Patient positioning in semi or high fowlers helps decrease preload.
Sildenafil Interaction
Nitroglycerine is contraindicated with phosphodiesterase inhibitors like sildenafil within 24-48 hours due to the risk of lethal hypotension.
Initial Bedrest
Initial bedrest is recommended until the patient is pain/symptom free to avoid increased demand on the heart.
Pain Relief with Morphine
Morphine provides pain relief and reduces myocardial oxygen demand and workload.
Inhibits secretion of renin
A mechanism that reduces blood pressure by decreasing the formation of angiotensin I.
Inhibits secretion of aldosterone
A process that leads to reduced sodium and water retention, affecting blood volume.
Limits sodium and water reabsorption
A function that decreases blood volume and pressure.
Decrease in preload
Reduction of central venous pressure (CVP) and pulmonary capillary wedge pressure (PCWP).
Decrease in afterload
Reduction in systemic vascular resistance (SVR) and blood pressure (BP).
Selective Beta-Blocker Therapy
Therapy that targets beta-1 receptors primarily, with nonselective blockers also affecting beta-2 receptors.
Blocks beta 1 receptor sites
Action of selective beta-blockers like metoprolol and labetalol that reduces myocardial oxygen demand.
Decreases dromotropic action
Slowing conduction through the AV node, allowing for better ventricular filling.
Decreases chronotropic action
Slowing down heart rate.
Decreases inotropic action
Reducing contractility of the heart.
Calcium Channel Blockers
Medications that decrease myocardial oxygen demand, such as diltiazem and verapamil.
First line treatment for ACS
Pharmacologic treatment aimed at decreasing workload on the heart.
Morphine
Analgesic used in acute coronary syndrome, typically administered after nitroglycerin.
Nitroglycerin
Vasodilator used to increase blood flow to coronary arteries.
ACE-I / ARBs
Medications that help manage blood pressure and heart workload.
Patient with chest pain
Scenario involving a patient with 10/10 chest pain and specific vital signs.
Nitroglycerin and sildenafil interaction
Combination can cause irreversible hypotension.
Primary benefit of metoprolol
Reduces myocardial workload after a non-ST elevation myocardial infarction (MI).
Anti-thrombotic therapy
Treatment that affects the clotting cascade in one area.
Fibrinolytic therapy
Treatment that affects the clotting cascade in a different area.
Anti-Thrombotic Therapy
To prevent further thrombus/clot formation
Anti-platelet agents
Aspirin
Anticoagulant agents
Heparin
Fibrinolytic Therapy
Lyse/destroy clots
Fibrinolytic agents
Only ever used with STEMI patients
P2Y12 Receptor Inhibitor
If stopped for surgery, it takes 3-7 days for platelets to return to normal so bleeding is a risk
ADP receptor antagonists
Often given in addition to aspirin treatment
Clopidogrel
Also known as Plavix
Ticagrelor
Also known as Brilinta
DATP
When Aspirin and P2Y12 are given together, it is referred to as dual anti-platelet therapy