1. small animal med- lab evaluation of GI/pancreatic disease
1/49
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
50 Terms
what are indications for performing in-depth diagnostics for GI disease?
-depression, weakness
-abdominal distension, anorexia, fever
-marked dehydration
-weight loss
-mucus membrane abnormalities (congestion, pallor, petechiation)
-tachycardia/poor pulse quality/arrhythmias
-melena/severe hematochezia
-abdominal organomegaly or mass, pain
-chronicity
-lack of response to symptomatic therapy
What are the 4 primary goals of diagnosing GI disease?
Determine if in depth testing is indicated (vs symptomatic treatment)
R/O secondary causes of GI signs initially
R/O common causes of GI diseases before ruling out rare causes
Use less invasive and more affordable diagnostic tools before reaching for more invasive and expensive tools
what lab work should be run in cases of GI disease?
-CBC, chem, urinalysis, total T4
-endoparasite tests
-serum folate and cobalamin
-bacterial enteropathogen tests
-trypsin-like immunoreactivity (TLI)
-pancreatic lipase
what CBC changes may be seen with primary GI disease?
-eosinophilia (parasitic, fungal, eosinophilic gastroenteritis)
-anemia

what types of anemia may be seen with primary GI disease?
1. anemia of chronic disease (mild normocytic, normochromic non-regenerative anemia)
2. acute blood loss (parvovirus, acute hemorrhagic diarrhea- regenerative anemia)
3. iron deficiency anemia (chronic blood loss- non-regenerative)
what abnormalities may be seen on the serum chemistry profile with primary GI disease?
-elevated BUN
-hypocholesterolemia
-hypocalcemia
-panhypoproteinemia
what causes elevated BUN in primary GI disease?
overt GI bleeds, dehydration
what causes hypocholesterolemia in primary GI disease?
malabsorption and maldigestion
what causes hypocalcemia in primary GI disease?
vitamin D malabsorption
what causes panhypoproteinemia in primary GI disease?
Hypoalbuminemia and hypoglobulinemia→ protein losing enteropathy (PLE)
what are GI causes of hypochloremia?
-vomiting (loss of Cl)
-diarrhea (secretory diarrhea)
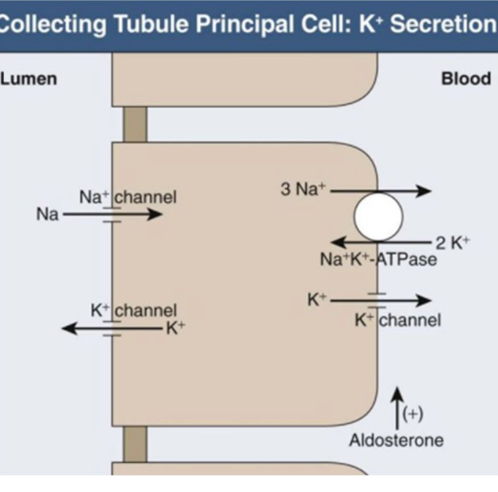
what are GI causes of hypokalemia?
-decreased intake
vomiting and diarrhea--> volume depletion--> increased aldosterone (promotes sodium resorption and potassium secretion)
what is hypochloremic metabolic alkalosis?
loss of hydrogen chloride, and retention of bicarbonate to maintain electroneutrality
what GI diseases result in hypochloremic metabolic alkalosis?
occurs with severe frequent vomiting
-upper GI obstruction
-gastric stasis

what is hyperchloremic metabolic acidosis?
loss of bicarbonate, retention of chloride with hydrogen to maintain electroneutrality
what are GI causes of hyperchloremic metabolic acidosis?
diarrhea (most commonly)
vomiting pancreatic/intestinal secretions rich in bicarbonate

what are the common GI helminth parasites?
roundworms
hookworms
tapeworms
whipworms
what are the common GI protozoa parasites?
giardia
coccidia
tritrichomonas foetus
how are endoparasites detected?
via detection of different life stages depending on parasite:
-helminths: ova
-giardia: cysts
-trichomonas: trophozoite
Testing __ __ fecal sample improves likelihood of detection of endoparasites.
>1 fresh
___ treatment often indicated in cases of diarrhea. Treat with __ for _ days.
Emprical
fenbendazole x 3 days
what parasites can fecal smears (wet mounts) detect?
used to ID protozoan oocysts and trophozoites (giardia, tritrichomonas foetus)
low sensitivity, false negatives 72-90%, cannot exclude infection
what parasites can fecal flotation with centrifugation detect?
most commonly used test
-used to detect giardia cysts wide variety of helminths
-centrifugation and zinc sulfate flotation improves sensitivity

what parasites can fecal sedimentation be used to detect?
preferred test to look for trematode ova (heterobilharzia)
what does the giardia and cryptosporidium ELISA or IFA tests detect?
detects fecal antigen
has high sensitivity and specificity
which animals can visualization of tritrichomonas trophozoites on direct wet mounts be done in?
cats only
must differentiate from giardia
trichotrichomonas progressive motility vs giardia “falling leaf”

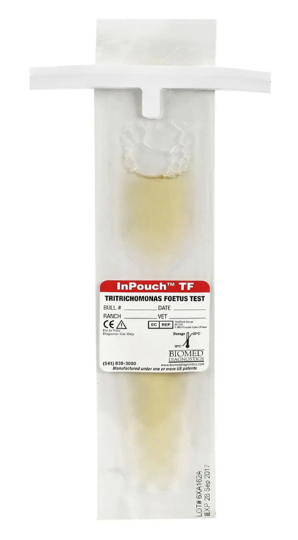
How can tritrichomonas foetus in cats be diagnosed?
visualization of trophozoite on direct wet mount
PouchTF culture
Fecal PCR (North Carolina State)
where is serum folate (vitamin B9) absorbed?
in the proximal intestine by folate carriers
what diseases lead to hypo-folatemia?
chronic duodenal diseases (malabsorption, depletion of folate stores)
what is elevated serum folate concentration be a marker of?
dysbiosis (some bacterial species can synthesize folate)
this finding does not warrant treatment with antibiotics
what are 3 causes of hypocobalaminemia (vitamin B12)?
1. chronic distal small intestinal (ileum) disease
2. surgical removal of ileum
3. exocrine pancreatic insufficiency
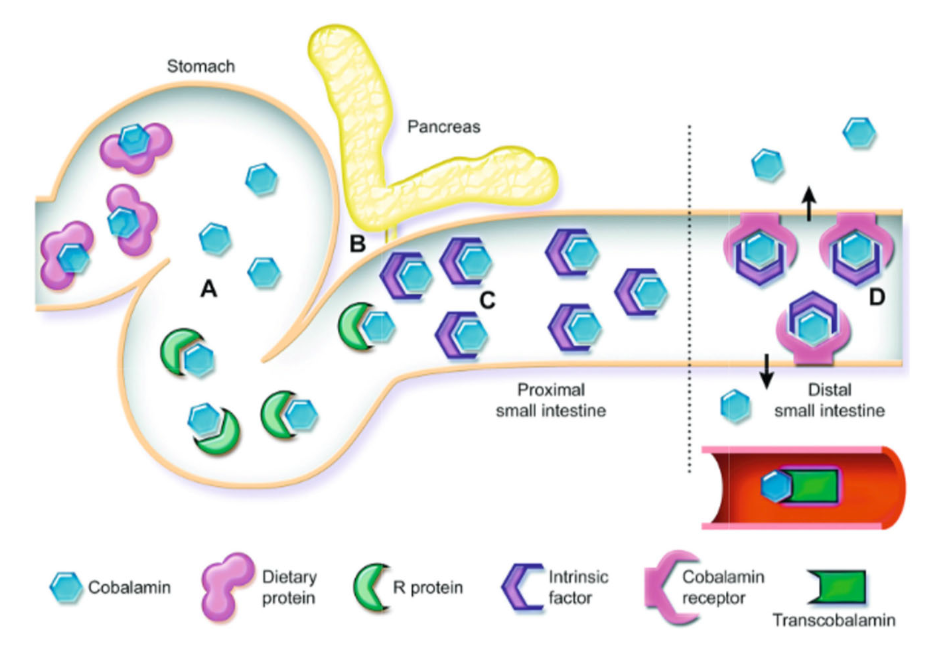
how are serum folate and cobalamin measured?
measured on fasted serum samples
when is supplementation indicated for folate and cobalamin?
for low concentrations
-cobalamin: oral supplementation or parenteral injections
-folate: oral supplementation
do normal serum concentrations of folate and cobalamin exclude gastrointestinal disease?
no
what are the 5 common bacterial enteropathogens of dogs and cats? (found in healthy dogs and cats)
clostridium perfringens
clostridium difficile
campylobacter jejuni
salmonella
escherichia coli
what is the typical clinical presentation of animals with enteropathogens?
often have acute diarrhea:
-mild and self limiting acute hemorrhagic diarrhea
-most commonly large bowel diarrhea (small or mixed possible)
+/- fever, malaise, vomiting
True or False? Only some strains of Clostridium perfringens produce toxins A and B to cause diarrhea.
False. Some strains of C. perfringens produces alpha (CPA), enterotoxin (CPE), netE/F.
Does presence (culture/PCR) of clostridium perfringens alone indicate c. perfringens-associated diarrhea?
no- isolation of c. perfringens alone cannot be used to diagnose c. perf diarrhea (normal flora in 80% of dogs)
diagnosis: PCR detection of c. perfringens toxin genes
is clostridium difficile more commonly isolated in dogs or cats?
dogs
how is clostridium difficile-associated diarrhea diagnosed?
isolation alone cannot be used for diagnosis-
diagnosis requires positive result for both:
-organism detection (culture, antigen ELISA, PCR)
-toxin A and B detection by ELISA/PCR
True or false? Only some strains of campylobacter cause gastroenteritis but all strains of salmonella cause gastroenteritis.
False. Both camplyobacter and salmonella only have some strains that cause gastroenteritis.
what are clinical signs of salmonellosis?
fever
anorexia
abdominal pain
vomiting in addition to diarrhea
which bacterial enteropathogens are zoonotic?
salmonella, campylobacter
Fecal smears were historically used to look for ___ or ___ endospores but have no diagnostic utility for sole diagnosis of bacterial enteropathogens.
campylobacter, clostridium

when should testing for bacterial enteropathogens be considered?
1. dogs and cats with acute onset bloody diarrhea that fails to respond to supportive care
2. dogs and cats with diarrhea and fever
3. diarrhea outbreaks occurring in multiple animals (± people) in densely populated shelter/kennel
when is treatment of bacterial enteropathogens indicated?
most bacterial enteropathogens are associated with self-limiting diarrhea
treat only when animals manifest systemic signs of illness that fail to respond to supportive care
what antibiotics are used to treat bacterial enteropathogen diseases?
metronidazole or amoxicillin (clostridium spp.)
fluoroquinolone (campylobacter)
what may be used to treat clostridium difficile infections?
fecal transplants
what is trypsin-like immunoreactivity (TLI) used to diagnose?
exocrine pancreatic insufficiency
what is pancreatic lipase (cPLI/fPLI) used to support the diagnosis of?
pancreatitis