CLS 161 UNIT 2 MICROSCOPIC EXAMINATION
1/201
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
202 Terms
what is the purpose for microscopically examining urine?
to detect and identify insoluble materials present in urine
what are the procedural variations for microscopic analysis?
method of how sediment is prepared
volume of sediment actually examined
method and equipment used to obtain visualization
manner in which results are reported
describe the protocol of initiation of microscopic examination based on macroscopic examination
a microscopic examination is only triggered when the specimen meets specific criteria which would be based on physical and chemical results
color, clarity (cloudy urines trigger microscopic examinations), and odor even though it is not reported
presence of blood, protein, nitrite, LE, and possibly glucose
what are the patient populations that must be considered when developing protocols for when a microscopic examination is triggered?
pregnant women
old people
pediatric
diabetics
immunocompromised
what does CLSI recommend when a microscopic examination should be performed?
physical requests
lab-specified population is being tested
abnormal physical or chemical results are obtained
describe the microscopic examination of urine specimens
microscopic examination is used to detect and identify insoluble materials that are present in the urine
blood, kidney, lower genitourinary tract, and external contamination all contribute formed elements
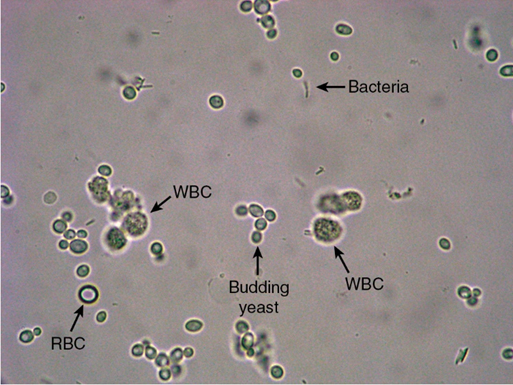
RBCs, WBCs
epithelial cells
casts
bacteria, yeast, parasites, mucus, spermatozoa
crystals
artifacts
some formed elements have no clinical significance and are actually considered normal until they are present in increased amounts
examination of urinary sediment must include both ID and quantitation of elements present
describe the recommended methods for standardizing specimen prep and volume, centrifugation, sediment prep, volume, and examination and reporting of results
regarding specimen prep, specimens should be examined while the urine is fresh or properly preserved as formed elements will disintegrate quickly, especially in dilute alkaline urine.
a clean-catch midstream specimen will have less contamination regarding epithelial cells.
regarding specimen volume, the recommended volume is between 10-15 mL although 12 mL is usually used since reagent strips and capped centrifuged tubes is calibrated to 12 mL.
if 12 mL isnt possible then it needs to be noted onto the report so a physician can make corrections to the results
regarding centrifugation, specimens are centrifuged so the sediment falls to the bottom.
the speed of the centrifuge and the length of time that the specimen is spinning for needs to be consistent.
specimens should be capped to avoid aerosols
centrifuging for 5 mins at 400 RCF or 1000 RPM is optimum for amount of sediment with the least chance of damaging the sediment
regarding sediment prep, a uniform amount of urine and sediment should be present after decantation.
sediment should be gently resuspended through gentle agitation with a pipetted or by tapping the tip of the tube.
there should be a consistent amount of sediment placed on the slide and if commercial systems are used then it must be filled completely
regarding examining the sediment, it should be performed in a consistent manner by observing a minimum of 10 fields under low and high power fields
first, slides are examined under low power to detect casts and to overall determine the general composition of sediment
if the sediment is unstained, the sediments should be viewed under reduced light when using bright field microscopy
regarding reporting the microscopic examination, casts are reported as average number per low power field (lpf), RBCs and WBCs are reported as average number of high power field (hpf), and epithelial cells, crystals, and other elements are reported semiquantitatively.
semiquantitative = rare, few, moderate, and many or +1, +2, +3, +4 followed by per lpf or hpf
MICROSCOPIC RESULTS SHOULD CORRELATE WITH PHYSICAL AND CHEMICAL RESULTS
what formed elements will disintegrate quickly in dilute alkaline urine?
RBC
WBC
hyaline casts
why should you refrain from using the centrifuges braking mechanism to slow down the centrifuge?
disrupts the sediment before decantation
what amount is common after decanting the sediment?
0.5 and 1.0 mL
what is the concentration factor? what does it relate to?
volume of urine centrifuged divided by sediment volume
related to the probability of detecting elements present in low quantities
also used when quantitating the number of elements per mL
what is necessary to quantitate cellular elements per mL of urine?
chamber volume, size of viewing area, and approx. number of low power and high power viewing areas (commercial systems do this) + sediment concentration factor
what does the CLSI recommend regarding commercial systems?
the use of commercial systems and standardization of all phases of the methodology which includes the conventional method
how should the physical and chemical tests correlate when RBCs are seen microscopically? what are the exceptions?
physical
turbidity
red color
chemical
+ blood
+ protein
exceptions
number of them
hemolysis
how should the physical and chemical tests correlate when WBCs are seen microscopically? what are the exceptions?
physical
turbidity
chemical
+ protein
+ nitrite
+ LE
exception
number
lysis
how should the physical and chemical tests correlate when epithelial cells are seen microscopically? what are the exceptions?
physical
turbidity
chemical
none
exceptions
number
how should the physical and chemical tests correlate when casts are seen microscopically? what are the exceptions?
physical
none
chemical
+ protein
exceptions
number
how should the physical and chemical tests correlate when bacteria’s are seen microscopically? what are the exceptions?
physical
turbidity
chemical
pH
+ nitrite
+ leukocyte
exceptions
number
type
how should the physical and chemical tests correlate when crystals are seen microscopically? what are the exceptions
physical
turbidity
color
chemical
pH
+ bilirubin
exceptions
number
type
what are the 4 factors that could affect the appearance of a sediment?
cells and casts in various stages of development and degeneration
distortion of cells and crystals (will reflect light) by the chemical content of the specimen
presence of inclusions in cells and casts
contamination of artifacts
how perfect is it? (nature is not perfect)
how is light being reflected?
when someone is talking about counting the elements found in a sediment, what are they talking about?
talking about the field of view meaning the microscope needs to be moved in 10 unique spots
what does staining do?
increases the overall visibility when using bright field microscopy (use subdued light) by changing the refractive index
what does staining show?
shows identifying characteristics to cellular structures like nuclei, cytoplasm, and inclusions
what are the two stains for supravital stains? explain why each stain is used
Sternheimer-Malbin
WBCs, epithelial cells, and casts absorb this dye well which allows a clear description of its structure and contrasting colors of their nuclei and cytoplasm
0.5% toluidine blue (metachromatic stain)
used to differentiate between WBCs and renal tubular epithelial cells
also used to examine other cells from other body fluids
is the sediment fixed on the slide when using supravital stains? why or why not?
not fixed onto the slide because the cells need to be alive when examining them
what is acetic acid used for? why should it not be used for initial analysis?
enhances the nuclear detail of WBCs and epithelial cells
should not be used for initial analysis as RBCs will lyse
use if you need to see other things that may be present like WBCs, yeast, oil droplets, and crystals
what does the passage of lipids across the glomerular membrane result in?
appearance of free fat droplets and lipid-containing cells and casts in the sediment
what are the two lipid stains? explain their usage. what else is used in conjunction with lipid stains?
two lipid stains → Oil red O and Sudan III
stains triglycerides and neutral fats an orange-red
polarizing microscopy is used in conjunction with lipid stains to confirm the presence of cholesterol
what are gram stains used for?
identification of bacterial casts but can be easily confused with granular casts
what is almost always associated with microbial infections?
polynuclear WBC, neutrophil
what is the hansel stain used for? what is in it? how is it performed?
used to stain eosinophils (preferred)
can use Wright stain and Giemsa stain
contains methylene blue + eosin Y in methanol
performed on a dried smear of centrifuged specimen or a cytocentrifuged prep of sediment
what are the other causes of eosinophils to be present?
renal transplant rejection
pyelonephritis
prostatitis
cystitis
what is the prussian blue stain?
stains structures containing iron which will stain hemosiderin in cases of hemoglobinuria blue
what is cytodiagnostic urine testing? what is it used in combination with?
performed independently but is used for detection of malignancies of lower urinary tract
used with the Papanicolaou stain to detect:
renal tubular changes associated with transplant rejection
viral, fungal, and parasitic infections
cellular inclusions
pathological casts
inflammatory conditions
when is microscopy best performed?
when the laboratorian is knowledgeable about the types of microscopes, primary characteristics of them, and the properly use and maintenance of them
what does the type of microscopy depend on?
specimen type
refractive index of object
ability to image unstained living cells
what is bright field microscopy?
objects appear dark against light background and is the most common type of microscopy used but can present issues if the light is too bright
what is phase difference influenced by?
thickness of object
refractive index
other light-absorbance properties
what is phase-contrast microscopy useful for?
ID of low refractive index hyaline casts or mixed cellular casts and mucous threads by forming a halo of light around the specimen
what does polarizing microscopy used for? (two things)
used to confirm the identification of fat droplets, oval fat bodies, and fatty casts that produce the maltese cross pattern characteristic
can also help differentiate birefringent uric acid crystals from:
cystine crystals and monohydrate calcium oxalate crystals from nonpolarizing RBCs
calcium phosphate crystals from nonpolarizing bacteria
what is interference-contrast microscopy?
provides 3D image that shows very fine structure detail by splitting the light ray so the beam passes through different areas of the specimen
what is dark field microscopy used for?
to enhance the visualization of specimen (usually unstained) that cannot be easily with a bright-field microscopy
what does fluorescence microscopy detect?
bacteria and viruses within cells and tissues through immunofluorescence
what can cause cellular elements to be easily distorted?
concentration that can vary
pH
presence of metabolities in urine
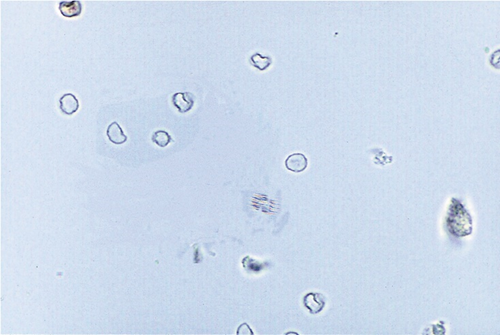
what would normal red blood cells look like in urine?
appear smooth, nonnucleated, biconcave disk that is ~7 μm in diameter
what power should RBCs be ID’d with? what are they reported as?
ID using high power
reported as average number seen in 10 hpfs
what happens to RBCs in concentrated (hypersthenuric, high SG) urine?
cells will shrink due to loss of water and may appear crenated or irregularly shaped
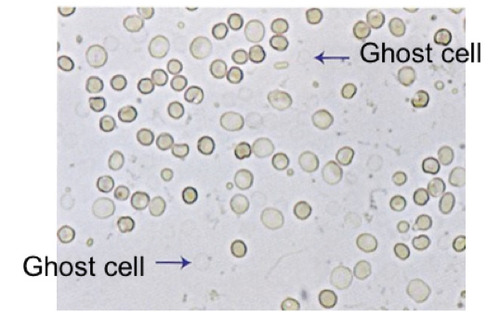
what happens to RBCs in dilute (hyposthenuric, low SG) urine?
cells will absorb water and swell which will lyse rapidly causing them to release their hemoglobin and leaving their cell membrane behind → ghost cell is the result
what are the reasons for RBCs being difficult to identify?
lack of characteristics structure
variations in size
close resemblance to other constituents
what are the five things that can easily be confused with RBCs?
yeasts (usually exhibits budding and should expect to see glucose)
oil droplets (highly refractile)
air bubbles (highly refractile)
starch (highly refractile)
may resemble granules seen in WBCs if RBCs are roughly crenated but smaller
what should be done if identification is still doubtful with RBCs?
add acetic acid to lyse the RBCs which would leave the yeasts, oil droplets, and WBCs intact
what does the morphology of urinary RBCs help with?
determining the site of renal bleeding
what can cause dysmorphic RBCs?
primarily associated with glomerular bleeding
strenuous exercise → indicates glomerular origin
what would a dysmorphic RBC that is related to glomerular bleeding look like?
acanthocytic (abnormal RBCs with thorn like protrusions) with multiple protrusions and is not as uniform
what would the dysmorphic cells look like if a wright stain is used to further analyze them?
shows the cells to be hypochromatic and would show a better description of the presence of cellular blebs and protrustions
what is the clinical significance of RBCs in urine sediment? what do the number of cells present indicate?
associated with damage to glomerular membrane or vascular injury within genitourinary tract
the number of cells present indicate the extend of the damage or injury
what would the macroscopic hematuria determine with RBCs in urinary sediment?
cloudy red or brown urine
associated w/ advanced glomerular damage
also seen with damage to vascular integrity of urinary tract caused by trauma, coagulant disorders, and acute infection or inflammation
what would the microscopic hematuria determine with RBCs in urinary sediment?
helps with the early diagnosis of glomerular disorders and malignancies of the urinary tract
confirms the presence of renal calculi
can be transient if pt participated in strenuous exercise which is nonpathological
what would cause a positive for blood with a chemical test but would be absent in microscopic hematuria?
hemoglobin that has been filtered by glomerulus
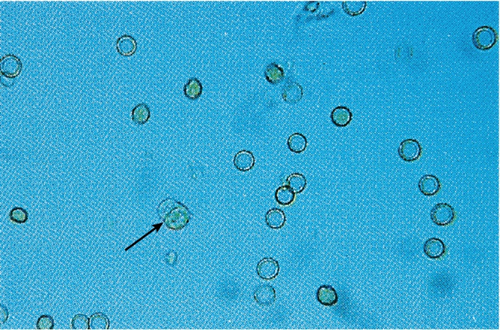
how big are WBCs? what power are they identified under?
12 μm
reported as average number seen in 10 hpfs
what would neutrophils look like under a microscope?
is the predominant WBCs and contains granules and multilobed nuclei
what happens to neutrophils when they are exposed to dilute alkaline urine?
lyses rapidly and begins to lose nuclear detail
what happens to neutrophils when exposed to hypotonic urine?
absorbs water and begins to swell which causes brownian movement and forms a glitter cell (NONPATHOLOGICAL)
when would you see eosinophils in urinary sediment?
drug induced interstitial nephritis
small number would be seen in UTI and renal transplant rejection
finding more than 1% is significant
how is an eosinophil test performed? what is determined for the percentage?
performed on a concentrated, stained (Hansel) urine sediment
can concentrate by centrifugation or cytocentrifugation
percentage per 100 to 500 cells
what would the mononuclear cells look like under a microscope?
lymphocytes are the smallest WBC and may look like RBCs
seen in increased numbers in early stages of renal transplant rejection
monocytes, macrophages, and histiocytes are larger and may appear vacuolated or contain inclusions
mononuclear cells are rare
what is the primary concern with the ID of WBCs?
differentiating between WBCs and disintegrated neutrophils from round renal tubular epithelial cells (RTE)
what is considered normal when seeing WBCs in urinary sediment?
<5 leukocytes per hpf but more in females
how can leukocytes enter urine?
through glomerular or capillary trauma but also through ameboid migration (can be hard to differentiate from epithelial cells) through the tissue to the site of infection or inflammation
what bacterial infections would be associated with an increased of WBCs in the urine (pyuria)?
pyelonephritis
cystitis
prostatitis
urethritis
what nonbacterial infections would be associated with pyuria?
glomerulonephritis
lupus erythematosus
interstitial nephritis
tumors
what are the three types of epithelial cells?
squamous
transitional (urothelial)
renal tubular
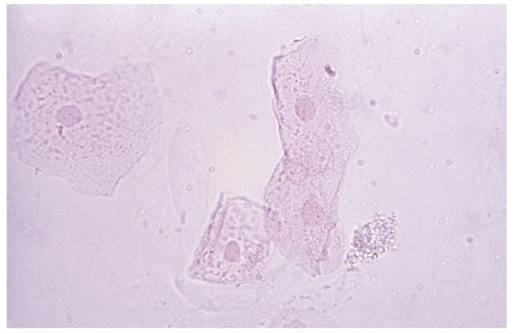
what would squamous epithelial cells look like under a microscope? what are they good for?
is the largest cell and contains abundant, irregular cytoplasm and has a prominent nucleus as big as RBC (~7 μm)
often the first structure observed and is a good reference point
what do squamous epithelial cells originate from? what do they represent? what are they reported as?
originate from linings of vagina, female urethra, and lower portions of male urethra
represents normal sloughing of cells and have no pathological significance
increased amounts are seen in female patients
reported as rare, few, moderate, or many (semiquantitative) and lpf or hpf depending on the lab
why would someone have difficulty identifying an epithelial cell on the rare occasion?
may appear folded which would resemble a cast
begins to disintegrate in unfresh urine
urine with large amounts of epithelial cells can clump which can make it difficult to see smaller pathological elements like RBCs and WBCs
what is a clue cell? what determines a clue cell? what is used to examine a clue cell?
a pathologically significant squamous epithelial cell and is indicative of a vaginal infection by Gardnerella vaginalis
bacteria covers 70% of cell surface and extends beyond the edges of the squamous cell which gives it a granular, irregular appearance
a vagina wet prep (saline) is used to examine a clue cell

what are transitional epithelial (urothelial) cells? where do they originate from? what are they reported as?
smaller than squamous cell with a centrally located nucleus and has three forms
spherical = absorb water in bladder and become large and round
can be difficult to differentiate from RTE cells
polyhedral = multiple sides
caudate = has a tail
originates from lining of renal pelvis, calyces, ureters, bladder, and upper portion of male urethra
appears in small numbers and represent normal cellular sloughing
ID’d in high power and reported as rare, few, moderate (semiquantitative)
what can increased numbers of transitional epithelial cells come in? what would an increase of transitional epithelial cells with abnormal morphology indicate?
singles, pairs, clumps (syncytia) which is present after invasive urological procedures and have no clinical significance
indicative of malignancy or viral infections which should be referred to a pathologist
why do renal tubular epithelial cells vary in size and shape? what areas would they come from and describe them
depends on the area of renal tubules from where they originated from
proximal convoluted tubule (PCT) = larger, rectangular, cytoplasm is coarsely granular
referred to as columnar or convoluted (coiled) cells
distal convoluted tube (DCT) = smaller than PCT and are round or oval with an eccentrically placed nuclei
can be mistaken for WBCs and spherical transitional epithelial cells
collecting duct = cuboidal, never round, has at least one straight edge with an eccentrically placed nucleus
appears in groups of three or more called renal fragments which is seen as large sheets of cells (not seen with PCT and DCT)
indication of severe tubular injury w/ basement membrane distruption
how are RTE’s ID’d and reported? what does their presence indicate?
reported either semiquantitatively (rare, few, moderate, or many) or quantitatively (actual number per hpf)
presence of two or more per hpf → indicative of tubular injury
what is the clinical significance of RTEs?
presence of increased amounts of RTEs is indicative of necrosis of renal tubules which could possible overall affect renal function
what are the 8 conditions that could produce tubular necrosis?
exposure to heavy metals
drug-induced toxicity
hemoglobin and myoglobin toxicity
viral infections (hep b)
seen with bilirubin
pyelonephritis
allergic rxns
malignant infiltrations
salicylate poisoning
single cuboidal cells are noticeable with salicylate poisoning
acute allogenic (donor to host) transplant rejection
what is one of the functions of RTE? based on one of its functions, why can it be clinically significant?
reabsorption of glomerular filtrate so seeing substance from the filtrate is not unusual
may be clinically significant because hemosiderin can be seen in episodes of hemoglobinuria
use prussian blue to stain hemosiderin blue
RTE cells also absorb bilirubin present in filtrate → due to liver damage
often occurs in viral hepatitis and appear deep yellow color
what are oval fat bodies? what are oval fat bodies reported as? how would you know oval fat bodies are present?
RTE cells absorb lipids that are present in the glomerular filtrate and appears highly refractile
seen in conjunction with free-floating fat droplets
may float on top of the specimen
reported quantitative as average number per hpf
confirmation = droplets containing cholesterol would have maltese cross formation with polarized light
droplets would stain orange red with Oil Red O and Sudan III with triglycerides and neutral fats
what should be considered when observing free-floating fat droplets?
specimens that are contaminated due to vaginal preparations and lubricants
what is lipiduria? what are they most associated with? what can they also be seen with?
presence of free lipids in urine
associated most often with damage to glomerulus caused by nephrotic syndrome
also seen with severe tubular necrosis, diabetes mellitus, and trauma cases that cause the release of bone marrow fat from long bones
what would be present in lipid-storage disease?
large-fat laden histiocytes which can be differentiated from oval fat bodies due to their large size
what could also be seen in cases of acute tubular necrosis? what are they referred to?
RTE cells that have large, nonlipid-filled vacuoles can be seen along with normal renal tubule cells and oval fat bodies
referred to as “bubble cells”
represents injured cells with the ER has dilated before apoptosis
what are the nonpathological reasons for bacteria to be in urine sediment?
specimen is contaminated from urethra, vagina, external genitalia, collection container
specimen was left unpreserved at room temp for longer than 2 hours
increases pH to 8
may cause positive nitrite
cause amount of glucose and ketone to decrease
not actually representative of urine
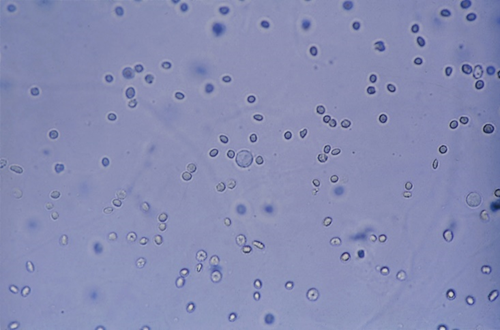
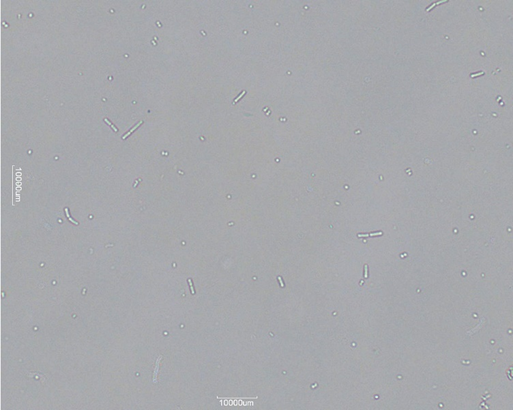
what is bacteria reported as and what will it look like under a microscope?
reported as few, moderate, or many per hpf
small and may be present in cocci or bacilli
what is needed for bacteria to be considered significant?
must be accompanied by WBCs and some labs only report bacteria when it is observed in fresh specimens with WBCs
what would correlate well with a positive urine culture?
the presence of motile organisms in a drop of fresh urine that was collected under sterile conditions
motility is also useful in differentiating them from amorphous phosphates and urates which look similar
what does the presence of bacteria indicate? what cause a follow up with a urine culture? what bacteria is associated with UTIs?
indicative of upper or lower UTI
specimens with increased bacteria and leukocytes are followed up with specimen urine culture
bacteria that is associated with UTI would be Enterobacteriaceae (gram-negative)
Staphylococcus and Enterococcus can also cause UTIs but are gram-positive which would be negative for nitrites but positive for LE
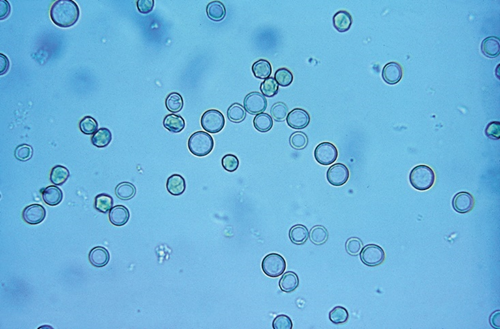
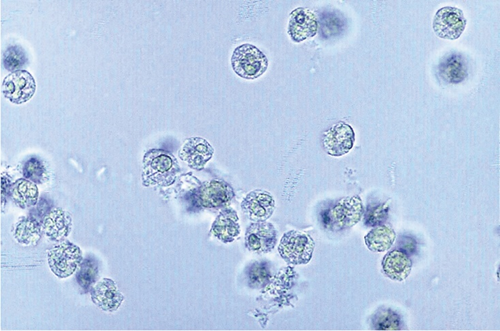
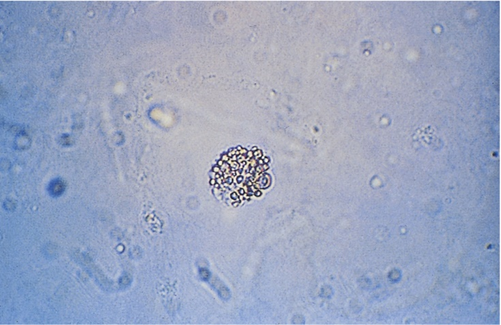
what would yeast look like under a microscope?
appears as small, refractile oval structures that may or may not contain a bud
may also appear branched, mycelial forms in severe infections
what are yeasts reported as?
rare, few, moderate, or many per hpf
where would yeast cells be seen in?
diabetics
acidic, glucose containing urine is an ideal medium for yeast to grow
immunocompromised
women with vaginal moniliasis
what should be accompanied with a true yeast infection?
presence of WBCs
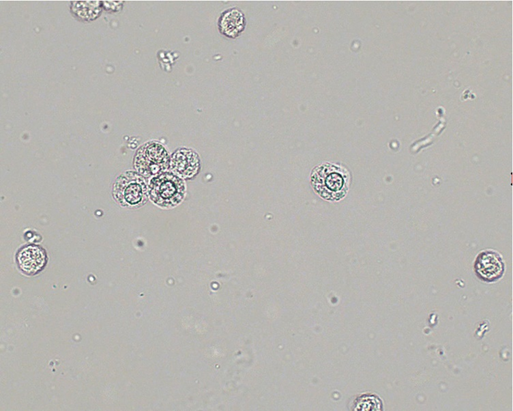
what is the most common parasite encountered and describe it
Trichomonas vaginalis
pear-shaped flagellate with an undulating membrane
easily ID’d in a wet prep due to its rapid, darting movement but when it isn’t moving it could look like a WBC, transitional, or RTE cell
sexually transmitted and primarily associated with vaginal inflammation
males are asymptomatic → infections of male urethra and prostate are asymptomatic
reported as rare, few, moderate, or many per hpf
related to parasites, what could also appear in the urine sediment other than Trichomonas vaginalis?
ova (eggs) of the pinworm Enterobius vermicularis is commonly seen
ova (eggs) of the bladder parasite, Schistosoma haematobium is seldom seen
fecal contamination in the urine specimen can result in the presence of ova from intestinal parasites
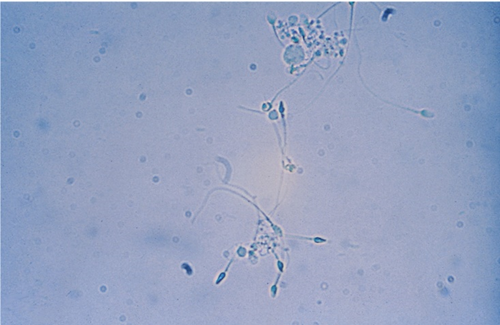
what would spermatozoa look like under a microscope?
oval, slightly taped heads, long flagella like tails and will rarely exhibit motility