Eye Disorders 2: Orbital and Other Infectious/Inflammatory Disorders
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
Orbital Cellulitis
infection involving the contents of the orbit posterior to the orbital septum
-a medical emergency
-must rule this out if suspected

Ethmoid sinuses, perforated, communication
Orbital cellulitis often arises from the paranasal sinuses, specifically the _________ _______. This is because those sinuses are separated from the orbit via the __________ lamina papyracea, allowing easy __________ between the sinus and orbit.
S. pneumoniae, children, veins, cavernous, infection, intracranial
Etiology/Epidemiology/Pathophysiology of Orbital Cellulitis
-Often arises from the paranasal sinuses, specifically the ethmoid sinus
-_.__________ is the most common cause, but H. influenza and Staph. Aureus can cause it too
-More common in ______
-Associated with recent eye surgeries, dental infections, middle ear infections, etc.
-The superior and inferior orbital ________ drain blood directly into the _________ sinus, making it easier for _________ to pass readily from the orbit to ___________ structures
pain, movement, EOMs, edema, fever, acuity
Symptoms of Orbital Cellulitis
-Ocular _______ especially with eye ________
-Restricted mobility of ___
-Proptosis
-Lid erythema/______
-Chemosis
-_______
-Decreased visual ________
-Afferent pupillary defect
-Leukocytosis

CT, culture, broad spectrum, abscess, loss
Diagnosis, Treatment, and Complications of Orbital Cellulitis
-Orbit/sinus __ scan, blood cultures/CBC, _______ of sinus drainage if concomitant sinusitis
-Hospitalize immediately, give _____ _______ IV antibiotics (Nafcillin ± metronidazole, clindamycin (anerobic coverage), Cefazolin or Ceftriaxone (trauma), or vancomycin (MRSA))
-May require surgical drainage if abscess forms
-Complications: subperiosteal ________, orbital abscess, vision ______, cavernous sinus thrombophlebitis, brain abscess
Preseptal Cellulitis
infection of the soft tissues anterior to the orbital septum, far more common than orbital cellulitis
-generally mild

children, trauma, sinusitis
Epidemiology/Etiology/Pathogenesis of Preseptal Cellulitis
-More common in ________ than adults
-Caused by S. aureus, S. pneumonia, beta-hemolytic streptococci
-_____, insect/animal bite, or foreign body of surrounding tissues of the face and eyelids or ________
unilateral, swelling, NOT, bactrim
Symptoms and Treatment of Preseptal Cellulitis
-________ ocular pain, less painful that orbital cellulitis
-Eyelid _________/erythema
-Will ___ cause pain with EOMs, proptosis, or ophthalmoplegia with diplopia
-Treat with _________ or Clindamycin + Amoxicillin-clavulanate or cephalexin

Corneal Ulcer
inflammatory and ulcerative keratitis, small/cloudy infiltrate seen in the cornea
Staph, HSV, A, pain, FB, infiltrate
Etiology and Symptoms of Corneal Ulcer
-Bacterial Causes = _____, Strep, Pseudomonas
-Viruses = ___, adenovirus
-Fungal = rare
-Vitamin _ deficiency
-_____, photophobia, __ sensation, corneal ______ (round, white spot)
-Decreased vision, discharge, conjunctival hyperemia, meiosis, chemosis
Keratitis
inflammation of the cornea, threat to vision due to risk of corneal clouding, scarring, and perforation
-must have a corneal ulcer
A, Staph Aureus, HSV 1, contact lens
Etiology of Keratitis
-Noninfectious (vitamin _ deficiency)
-Bacterial (____ _____, strep, chlamydia, pseudomonas)
-Viruses (___ _)
-Fungus
-Predisposing factors include _______ ___ use, trauma, corneal grafting
Bacterial Keratitis
keratitis caused by a bacterial infection
-caused by improper contact lens wear (greatest risk factor)
-dry ocular surface, breakdown of host defenses
-topical corticosteroid use and/or immunosuppression

FB, open, red, limbic
Symptoms of Bacterial Keratitis
-___ sensation, painful red eye
-Trouble keeping eye _______ (sign of active corneal process), corneal opacity, infiltrate, ulceration (round white spot)
-____ eye
-Photophobia, +/- mucopurulent discharge
-_________ flushing, could be only part of the limbus

clinical, ophthalmologist, drops, same
Diagnosis and Treatment of Bacterial Keratitis
-Mostly _______, could get corneal scrapings for culture and gram staining (performed by the _____________)
-Antibiotic eye _______ (fluoroquinolones) applied hourly for 24-28 hours x 2 weeks, drops preferred over ointment because of corneal availability
-Cycloplegic gtts
-Don’t patch eye
-Warrants ______ day evaluation by an ophthalmologist
HSV Keratitis
keratitis caused by infection with HSV-1 or HSV-2, viral latency (trigeminal ganglion) can be reactivated by stress, trauma, fever, UV exposure, and other infection
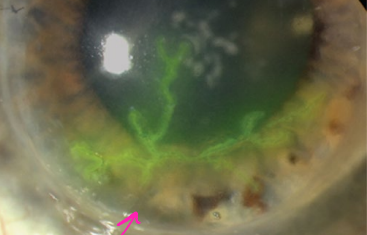
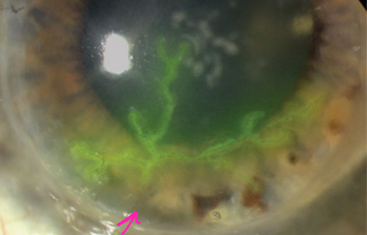
pain, limbus, watery, dendritic, clinical
Symptoms and Diagnosis of HSV Keratitis
-Typically unilateral with visual blurring
-______, photophobia, conjunctival injection near the ________ (ciliary flush)
-________ discharge, ________ lesions
-Diagnosis is usually ______, but there are three types of testing: viral culture, detection of viral antigen, detection of viral DNA (PCR)
topical, oral
Treatment of HSV Keratitis
-______ antiviral agents (Ganciclovir, Acyclovir)
-______ antivirals (Acyclovir, Valacyclovir)
-Sometimes use of topical glucocorticoids are effective but need to be used with caution, best done by ophthalmologist
Herpes Zoster Ophthalmicus
Varicella Zoster reactivation within the trigeminal ganglion/nerve, frontal branch is most frequently involved
-vesicular eruption along the dermatome that never crosses midline
-sight threatening, must not miss

unilateral, dermatome, Hutchinson’s sign, dendrites
Symptoms of Herpes Zoster Opthalmicus
-Headache, malaise, fever
-__________ pain/tingling in the affected eye/forehead/scalp
-Vesicular eruption along the _________, not crossing the midline
-Vesicular lesions on the nose (_________ ______) indicate high risk of HZO
-Conjunctivitis, lid droop
-Corneal involvement (keratitis), corneal __________ seen after staining
-Anterior uveitis, increased IOP, nerve palsies, retinal necrosis, corneal scarring are common

Antivirals, steroid
Treatment for Herpes Zoster Ophthalmicus
-_________ (oral and topical), common to use a combination
-Topical _________ drops
Corneal Ulcer
ulceration found on the cornea
-diagnosed with fluorescein stain and slit lamp exam, may need cultured
small, significant, amphotericin B
Treatment for Corneal Ulcers
-Cycloplegic drops to help with discomfort
-Bacterial: moxifloxacin (______ ulcers) or tobramycin and cefazolin (________ ulcers)
-HSV: ganciclovir, valacyclovir, acyclovir
-Fungal: natamycine or _________ _ (very rare)
-Refer to ophthalmology
Uveitis
inflammation of the uveal tract (choroid, ciliary body, iris)
-can be anterior (ciliary body, iris) or posterior (choroid)
Infections, immune-mediated, Ankylosing spondylitis, hypersensitivity
Etiology of Uveitis
-__________: bacterial, viral, fungal, and parasitic. Viral causes include HSV, CMV, toxoplasmosis, syphilis, West Nile
-Systemic _______-______ disease (40% of cases): inflammatory diseases like __________ __________, reactive arthritis (two most common), and inflammatory bowel disease. Or drug ___________ reactions to fluoroquinolones, bisphosphonates, and immunotherapy
-Syndromes confined to the eye
Anterior Uveitis
uveitis including the iris (iritis), ciliary body (cyclitis), or both (iridocyclitis)

deep, acuity, red, miosis, consensual
Symptoms of Anterior Uveitis
-Unilateral, ________, aching pain
-Decrease in visual _______, ciliary injection or diffusely ___
-Cornea may be slightly cloudy
-Pupils usually small and may become irregular (_______)
-Photophobia (_________), where shining a light in the unaffected eye hurts the affected eye because the iris is trying to move
-Adhesions or scarring in the iris can pull the pupil into an irregular shape

precipitates, flare, ophthalmology
Diagnosis and Treatment of Anterior Uveitis
-Slit lamp and dilated fundus exam: reveals keratitic ____________ (white cells on endothelium) and inflammatory cells and _______ within the aqueous of anterior chamber
-Refer to ____________
-Infectious: treat with antiviral agents or antibiotics
-Noninfectious: topical glucocorticoid (prednisolone), cycloplegic agent (cyclopentolate and atropine)
Posterior Uveitis
uveitis that includes the choroid/retina (choroiditis, chorioretinitis, retinitis, vitritis)
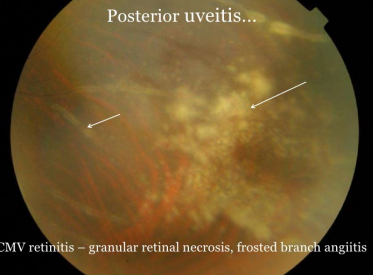
loss, deep, inflamed, fundus
Symptoms and Diagnosis of Posterior Uveitis
-Gradual vision _______
-_______ aching pain, some redness
-Minimally _______ eye, floaters
-Commonly bilateral
-Diagnosed via a slit lamp and dilated _______ exam, revealing inflammatory cells in the vitreous humor and active chorioretinal inflammation
antiviral, dilation
Treatment of Posterior Uveitis
-Treat the cause
-Infectious: _________ agents, antibiotics
-Noninfectious: systemic/periocular/intravitreal corticosteroid therapy
-Pupil ________ usually not necessary
Panuveitis
uveitis where you have simultaneous inflammation of the entire uveal tract and usually the retina
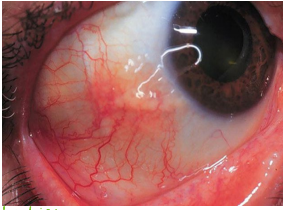
Scleritis
painful, destructive, and potentially blinding inflammatory disorder of sclera
-must not miss
-quick diagnosis and quick treatment

RA, SLE, immune complex, necrosis, occlusion
Etiology and Pathophysiology of Scleritis
-Autoimmune conditions (namely __ and ___), syphilis, and gout. Vasculitis from these disorders can cause scleritis
-Inflammatory invasion and ________ _______ deposition in vessels > fibrinoid ________ (Death of eye tissue that can be caused by clots from stenosis or occlusion), thrombotic ___________ of vessels and inflammatory response in the sclera

redness, boring, scleral, night, morning, therapy
Symptoms and Treatment of Scleritis
-Diffuse _______ or violaceous discoloration
-Vascular engorgement and severe, ________ eye pain
-Tenderness of globe and photophobia
-________ thickening is the hallmark
-Pain is constant and worse at _____/first thing in the ______
-Refer to ophthalmology
-Systemic _______: oral NSAIDs or corticosteroids (first line) and immunosuppressive drugs (second line, Methotrexate)

Oral NSAIDs, corticosteroids
What is the first line treatment for scleritis? What about if necrosis is involved?
Methotrexate (Immunosuppressive drugs)
What drug is the second line treatment for scleritis?
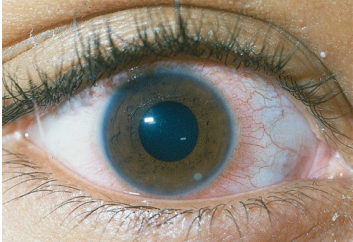
Episcleritis
inflammation of the episclera, which is the thin, highly vascular connective tissue between the conjunctiva and the sclera
-probably not an emergency
hypersensitivity, females
Pathogenesis and Epidemiology of Episcleritis
-Usually a ___________ response that causes vasodilation, edema, and lymphocytic infiltration (nonimmune and immune)
-Present more often in _________ and middle-aged adults
Simple
What type of episcleritis is sectoral, confined to a portion of the episclera? It can also be diffuse
Nodular
What type of episcleritis is raised and usually limited to just one area of the eyeball?
bilateral, mild, vision, tears, NSAIDs
Symptoms and Treatment of Episcleritis
-Acute, 50% ________
-Redness vasodilation of episcleral vessels
-Irritation, watering
-Pain is unusual or very ______
-________ is preserved
-Most resolve within 3 weeks
-Symptomatic relief: artificial _______ (first line), oral and topical ________ (if persistent discomfort despite lubricants), and topical glucocorticoids (if failure of lubricants and topical NSAIDs)