27. Head and spinal trauma. Emergency and critical care. Diseases of the peripheral nerves on the fore and hind limbs.
1/66
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
67 Terms
What are the key initial steps in managing an emergency patient?
Ensuring ABCs (Airway, Breathing, Circulation)
Oxygen administration (mask, hyperbaric chamber)
Glucose control (avoid hyperglycaemia → nerve damage)
Anti-oedema drugs (Mannitol, NSAIDs)
How can CNS injuries be classified?
Primary
Secondary
Direct physical damage from the traumatic event (contusion, laceration, haemorrhage, haematoma, vasogenic oedema, unstable fractures)
Complex cascade of biochemical, vascular, and systemic changes occurring minutes to days after the primary injury → depletion of ATP, influx of Na & Ca into cells → increase in excitatory neurotransmitters → cytotoxic oedema, failure of membrane pumps, neuronal damage and death → local tissue acidosis, hypoperfusion, reactive oxygen radicals, inflammatory cytokines activating arachidonic acid & coagulation cascades, thus damaging the blood-brain barrier (BBB)
Release of nitric oxide → excessive vasodilation, loss of pressure autoregulation → neuronal death
Hypotension, hypoxia, inflammation, glucose changes, hyperthermia, electrolyte abnormalities, acid-base abnormalities, hypercapnia/hypocapnia
What are the types of pathogenesis of CNS trauma?
Acute compression
Slow/chronic compression
What is the effect of vasospasm in acute compression?
Activation of AMPA (glutamate) receptors → intracellular Ca build-up, free radicals → lipid peroxidation, fluid/protein/electrolyte/erythrocyte leakage → haemorrhagic necrosis in grey matter.
Chronic mass pressure → increased intraparenchymal pressure → white matter damage: gliosis, demyelination, axonal oedema, vacuolization → impaired proprioception, motor skills, skin sensitivity, deep pain (grey matter is relatively preserved)
What are the pathological changes after brain/head trauma?
Damage to brain tissue or vessels in brain → brain herniation, brain oedema → astrocyte swelling → cytotoxic oedema
Bleeding from nose/ears, confusion, disorientation, lethargy, pale gums, loss of consciousness, head pressing, pupil dilation (mydriasis)/differences (anisocoria), nystagmus, stumbling, seizures, shock, weakness, paralysis, coma, death
History, clinical signs, X-ray, MRI, CT, intracranial pressure measurement
Check reflexes: corneal, pupillary light, palpebral
What are the key treatments for brain/head trauma?
ABC therapy: correct hypoxia and hypotension (>90 mmHg) → supply O2 to maintain pO2 >90%.
IV fluids – lactated ringer (shock dose) +/- glucose (avoid hyperglycemia)
Hypertonic saline – over 10-15 min to expand IV volume + draw fluid from ECS → corrects BP
Mannitol – control brain edema and decrease ICP 0.5-1 mg/kg IV over 15 min
Seizure = diazepam, 0.1-0.5 mg/kg/h (phenobarbital if not effective enough)
Keep head elevated - prevent gravity from causing blood to go to the head.
Craniotomy - opening of skull for decompression - poor prognosis
Why are glucocorticoids and narcotics contraindicated in brain/head trauma?
Glucocorticoids: hyperglycaemia, immunosuppression;
Narcotics: increased intracranial pressure
How can the prognosis of brain/head trauma be monitored?
Repeated neurological examination
Neurological score (0 = normal, 5 = plegia with loss of voluntary function and loss of deep pain)
Progression
Deep pain assessment (may be able to walk with spinal walk - learned behaviour, but not urinate/defecate)
Cranial nerve assessment (more cranial nerves affected → worse prognosis)
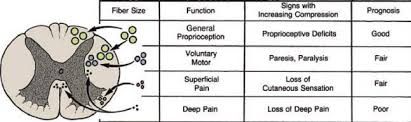
How is prognosis affected according to the size of the fibres effected?
The smaller the fibres, the worse the prognosis. The smallest fibres do not have a myelin sheath → no protection → do not regenerate.
A. Proprioceptive deficits (good)
B. Paresis/paralysis (fair)
C. Loss of cutaneous sensation (fair)
D. Loss of deep pain (poor)
External trauma e.g. concussion, compression, laceration → IVD protrusion, fractures, dislocations, subluxation
Infarction (FibroCartilaginous Embolism)
Pathological luxation of the the spine
Hereditary ligament instability → decreased spinal support
What is the difference between a pathological and traumatic fracture of the spine?
Pathological: bone disease;
Traumatic: force (hyperextension/hyperflexion of vertebral junctions)
How can external traumatic injuries of the spine be divided?
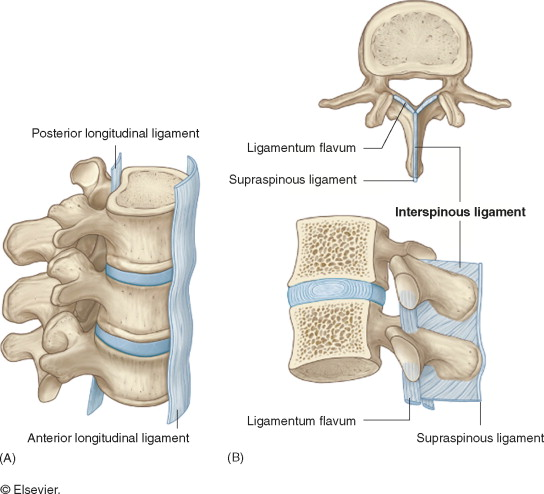
Ventral compartment injuries
Dorsal compartment injuries
Which structures may be affected in ventral compartment injuries?
Vertebral body
IV disc
Dorsal/ventral longitudinal ligaments
Inter-transverse ligaments
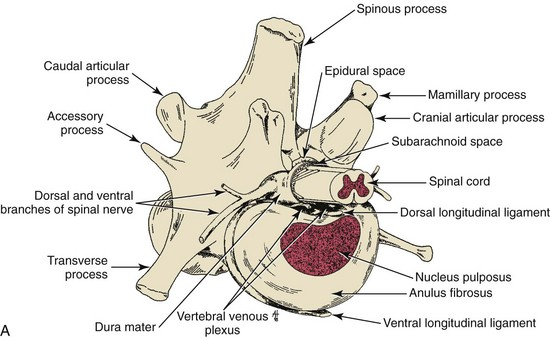
Which structures may be affected in dorsal compartment injuries?
Lamina
Pedicles
Spinal processes
Articular processes
Ligaments (supraspinosus, interspinosus, interarcuate)
Biochemical processes potentiating further damage (can be prevented)
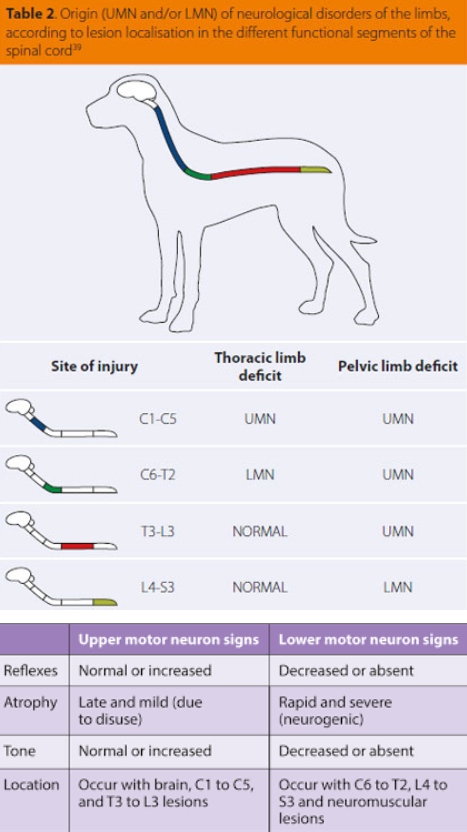
Depends on location of injury.
Loss of function, ataxia, pain/loss of deep pain, neurological deficits, spasms, weakness, paralysis, urinary/faecal incontinence
History, clinical signs, neurological examination, X-ray (2 views), myelography, MRI, CT
What does treatment of spinal injuries depend on?
Location and type of trauma. Non-surgical management is generally recommended for most injuries.
Decompression (laminectomy), removal of compressive disc material (fenestration), stabilisation of vertebrae
Airway: Clear obstruction if present; intubate or perform tracheostomy for oxygen delivery.
Breathing: Monitor breathing pattern; if not breathing, perform CPR. Dull lung sounds indicate fluid/air in pleural space – perform thoracocentesis.
Circulation: Monitor heart rate, mucous membrane colour, capillary refill time, pulse. White gums = possible shock/blood loss. If no heartbeat, start CPR.
Drugs
Adrenaline: ↑BP, peripheral vasodilation, bronchodilation.
Atropine: ↑HR, antispasmodic, avoid bradycardia, mydriatic.
Diazepam: Seizure control.
Dopamine: ↑BP, ↑HR.
Doxapram: Respiratory stimulant.
Cranial nerves
Spinal nerve roots
Dorsal root ganglia
Peripheral nerve trunks
Motor neuron branches
Peripheral autonomic nervous system
How can neuropathies be classified according to lesion severity?
Neuropraxia: mildest form of nerve injury. Interruption of transmission, no atrophy
Axonotmesis: higher degree of injury. Damage to axons, loss of function
Neurotmesis: complete severance of peripheral nerve trunk. All function lost
What types of clinical signs are associated with mononeuropathies?
Lower motor neuron signs: Gait abnormalities, rapid atrophy, dysmetria, ataxia
LMN: Paresis, paralysis, hypotonia, hyperaesthesia, ataxia, loss of tone and reflexes
Autonomic signs (rare): Cranial nerves, bladder control and panniculus reflex usually intact
History, clinical signs, neurological exam, X-ray, biopsy, electromyography
Evaluate muscles innervated by injured nerves by palpation and electromyography (needle inserted into muscles to record electrical impulse).
Evaluate grade of spinal cord weakness – ataxia, arched back, paresis, paralysis, deep pain.
Immediate repair (8-12 hours) for clean, sharp wounds e.g. glass
Does primary or secondary repair of nerve damage have better nerve regeneration, and why?
Secondary because contamination/inflammation has resolved
Brachial plexus (C6-T2)
Suprascapular (C6-T2)
Axillary (C6-C7)
Musculocutaneous (C6-C7)
Radial (C8-T2)
Median and ulnar (C7-T2)
No significant signs. Affects flexors of shoulder (teres major/minor, deltoideus)
Carpal and digital flexor atrophy, absent cutaneous palmar sensation
Which nerves are involved in pelvic limb paralysis?
Lumbosacral plexus (L4-S2)
Obturator (L4-L6)
Femoral (L3-L6)
Sciatic/Ischiatic (L5-S2)
Tibial (L4-S3)
Pudendal (S1-S3)
Plantigrade stance, paw dragging, no withdrawal reflex
Distal polyneuropathy of hindlimbs in Dobermans, causing involuntary flexion