Critical care - test 4
1/105
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
106 Terms
What is shock and why is it a medical emergency?
- Shock - mismatch of oxygenation and blood flow, as well as decreased tissue perfusion where cells/tissue may start to die
- Medical emergency - happens quickly, high rate of mortality, organs shut down, blood shunted to most vital organs
What are the 4 types of shock?
- Cardiogenic
- Hypovolemic
- Distributive Shock
* (neurogenic, anaphylactic, septic)
- Obstructive Shock
Comparison of different types of sock
- Hypovolemic: Hypotension, tachycardia, Weak thready pulse, Cool, pale, moist skin, U/O decreased
* Decreased CO, Increased SVR
- Cardiogenic: Hypotension, tachycardia, Weak thready pulse, Cool, pale, moist skin, U/O < 30 ml/hr, Crackles, tachypnea
* Decreased CO, Increased SVR
- Neurogenic: Hypotension, Bradycardia, Warm Dry Skin
* Decreased CO, Venous & arterial vasodilation, loss sympathetic tone
- Anaphylactic: Hypotension, tachycardia, Cough, dyspnea, Pruritus, urticaria, Restlessness, decreased LOC
* Decreased CO, Decreased SVR
- Septic: Hypotension, Tachycardia Full bounding pulse, tachycardia, pink, warm, flushed skin, Decreased U/O, fever
* Decreased CO, Decreased SVR
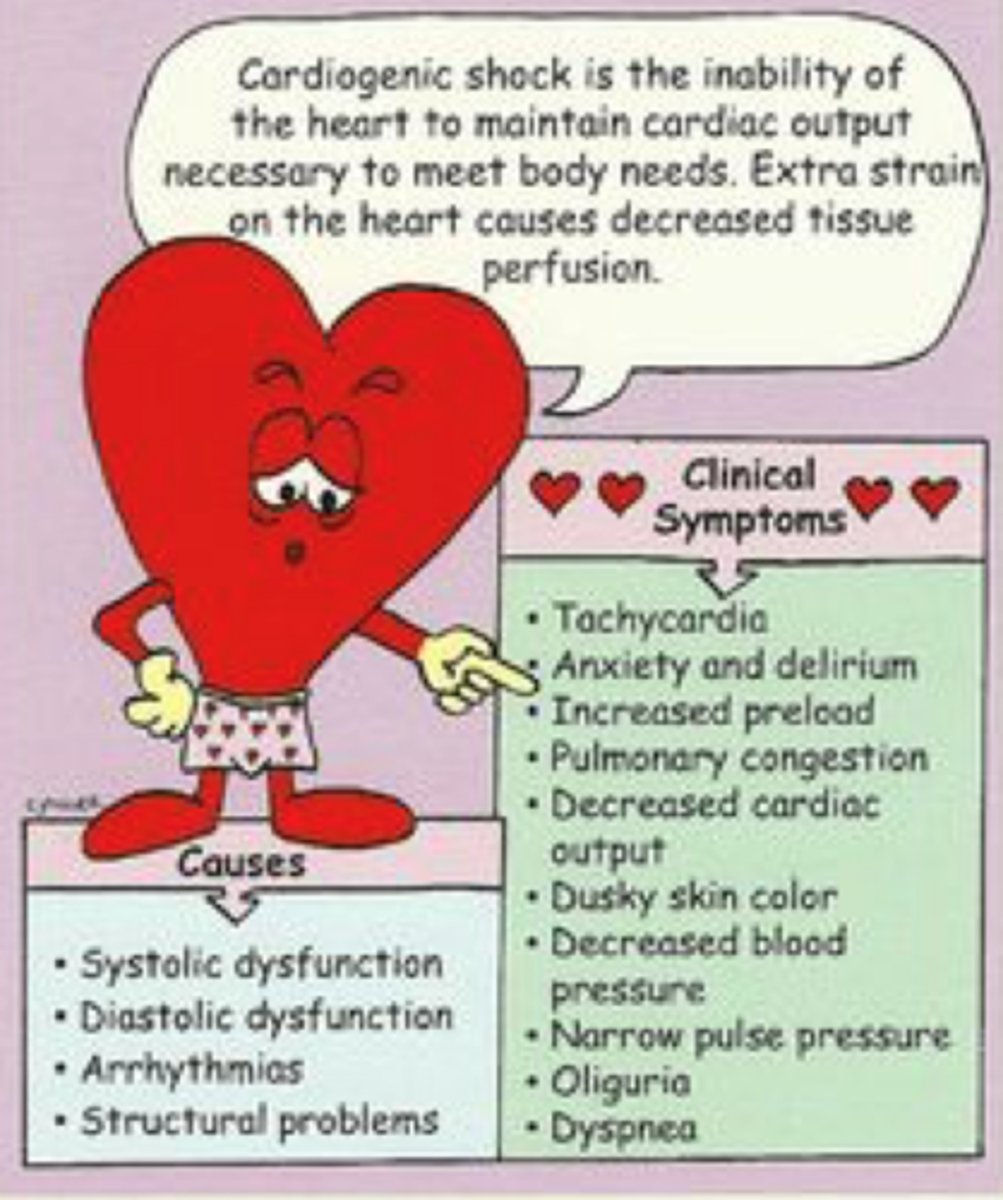
CARDIOGENIC SHOCK
Systolic or diastolic dysfunction of the heart decreases cardiac output
- Causes - MI, cardiomyopathy, blunt injury, pulmonary hypertension, cardiac tamponade, slow heart rhythms, fast heart rhythms, CHF
What are some common assessment findings of cardiogenic shock.
- sharp decrease in cardiac output, vasodilation, tachycardia, hypotension, crackles, tachypnea, delayed cap refill, narrowing pulse pressure, weak peripheral pulses, cool, clammy skin, decreased urine output, anxiety
- Want to restore heart function, oxygen, nitrates, diuretics (worry about potassium)
- 50% morality rate
Cardiogenic shock lab values
BNP, Troponin, ABG, CMP, KK-MB, BUN, Creatinine
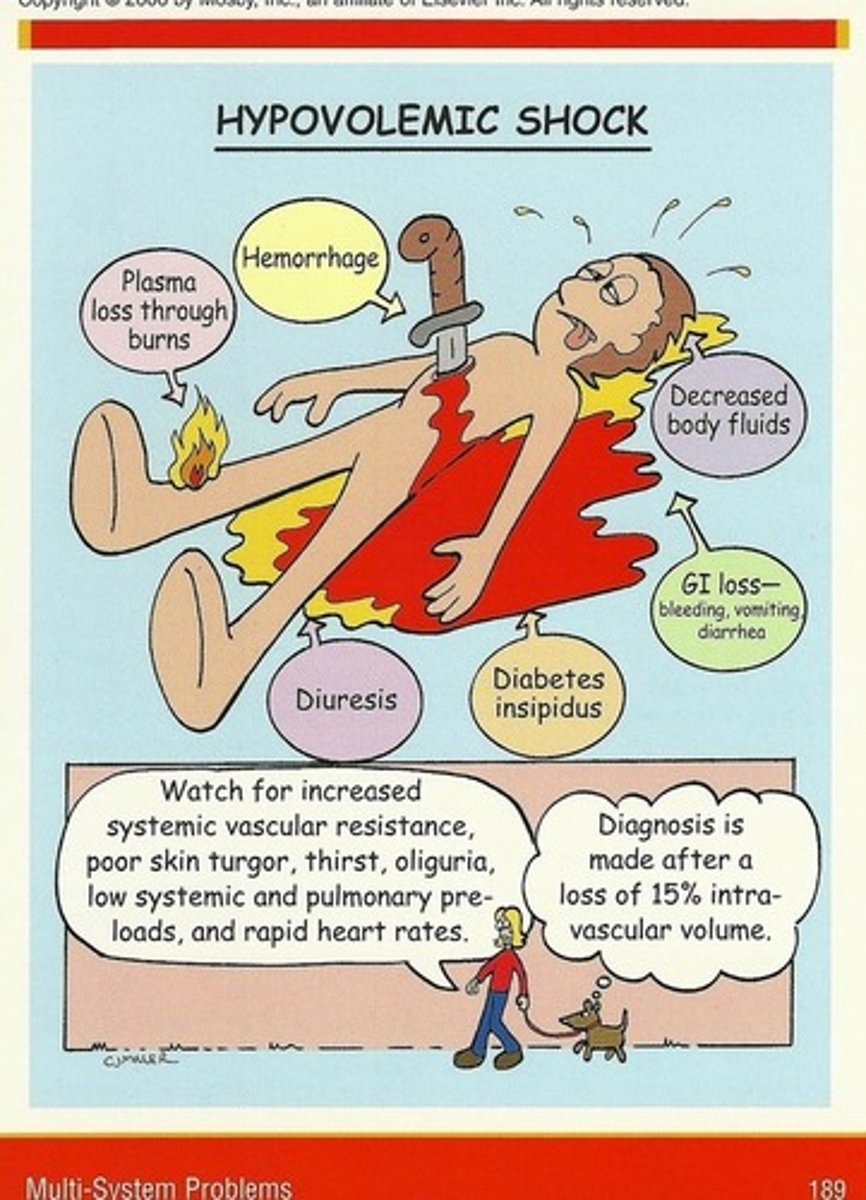
HYPOVOLEMIC SHOCK
Loss of intravascular fluid volume. (Bleeding, 3rd spacing, vomiting, diarrhea)
Causes: bleeding, trauma, surgery, Vomiting, diarrhea, loss of lots of fluids
Assessment findings: tachycardia, hypotension, cool clammy skin, decreased Urinary output, confusion
Interventions: blood and fluid replacement, Normal Saline: 3 ml of isotonic solution for 1 ml of blood loss
- want to know why happened and don't want to give to much fluid
Hypovolemic shock lab values
HGB, HCT, RBC, BUN, Creatinine, CMP, Vitals
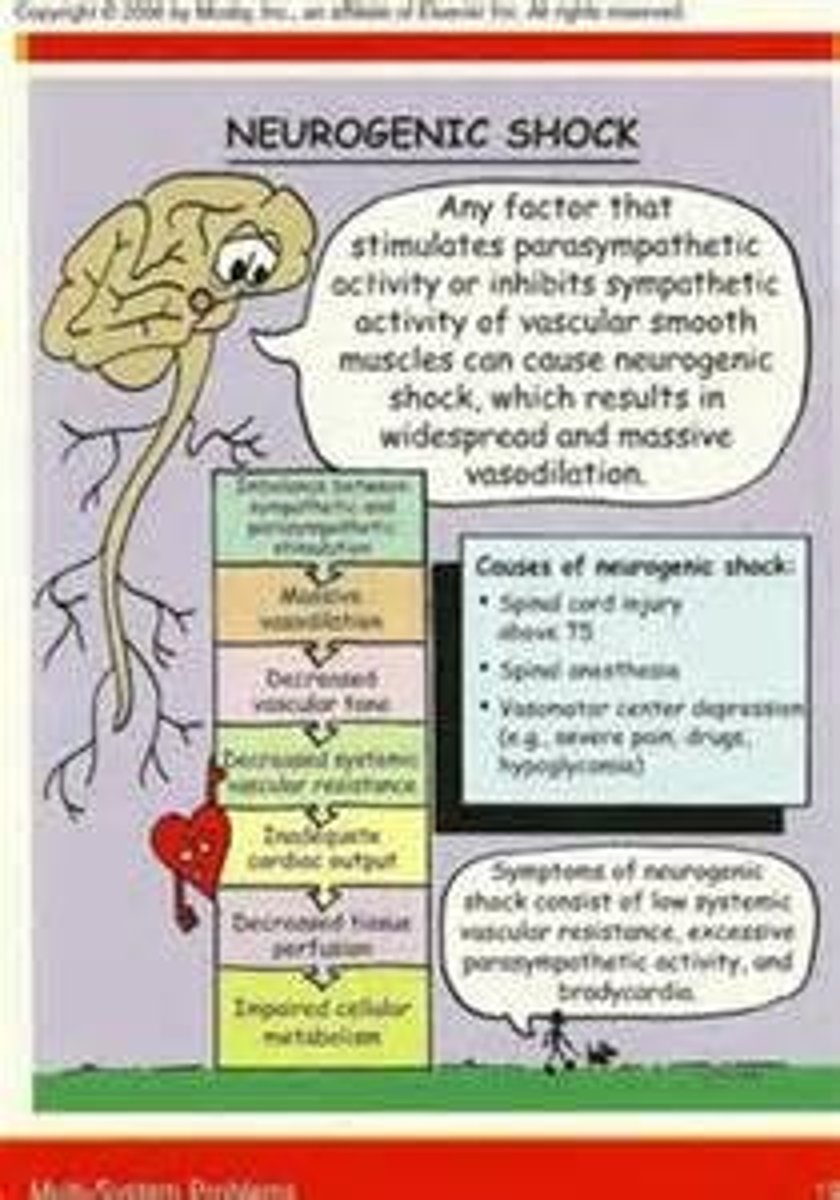
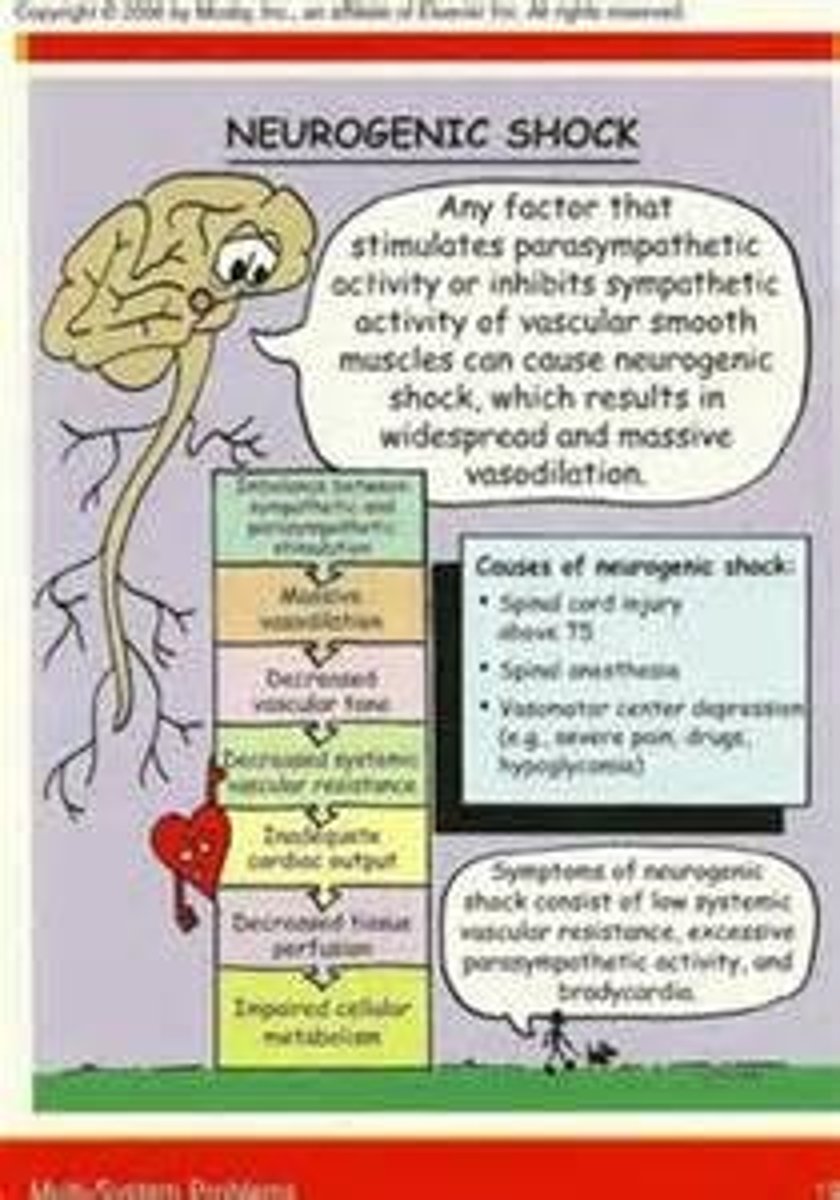
DISTRIBUTIVE: NEUROGENIC SHOCK
Hemodynamic phenomenon that occurs within 30 minutes of spinal cord injury and can last up to 6 weeks.
What are some common assessment findings of neurogenic shock?
- severe pain, hypotension, bradycardia, not temp regulation, dry skin, initially flushed -> hypothermia, vasodilation, hypotension
Causes spinal cord injury
Interventions: maintain airway (o2 intubate), cautious fluid administrations, vasopressors, atropine, stabilize spinal cord, monitor temp
Neurogenic shock lab values
Kidney function: BUN, Creatinine, GFR, ABGs
DISTRIBUTIVE:ANAPHYLACTIC SHOCK
Acute life-threatening allergic reaction to a substance
- (contrast, blood, insects, drugs, vaccines, latex)
- antibiotics can be a cause
- peanuts can be a cause
What are some common assessment findings of anaphylactic shock?
- massive vasodilation, increase in capillary permeability
- Sudden onset: dizziness, chest pain, incontinence, tachycardia, wheezing, stridor, swelling of the lips, tongue, and airway
Interventions: epinephrine, maintain airway, intubation, remove cause, bronchodilators, steroids, antihistamines
SEPTIC SHOCK
- The result of an infection
- Vasodilation, maldistribution of blood flow, myocardial depression
What are some common assessment findings of septic shock?
- Assessment findings: fever, Increased WBC, hyperglycemia, decreased systolic BP, altered mental status, decreased Respirations, if chronic could have leukopenia, or hypothermic
- Causes: improper sterility, infection, releases cytokines/body responds, UTI, pneumonia
- Interventions: antibiotics, cultures, increase fluids, prevent ulcers, O2, vasopressors, monitor
- Up to 30% in septic shock never identify cause
Septic shock lab values
Lactic acid, Procalcitonin, glucose, sed. rate, CRP, WBC, Bands, culture
Obstructive shock
- Physical Obstruction to blood flow
- Decreased Cardiac Output
What are some comment assessment findings of obstructive shock?
- Assessment findings: decreased CO, JVD, high afterload, paradoxical pulses, cool/clammy
- Causes: cardiac tamponade, tension pneumothorax, compartment syndrome, pulmonary Embolism, Right ventricular thrombi, anything that causes blood not to move forward (clot)
- Interventions: airway patency/ O2, intubations, treat obstructive cause, increased fluids (temp)
obstructive shock labs
lactic acid, WBCs, BUN, Creatinine, Troponin, ABGs, EKG
Signs of shock
Normal Map 70 - 110
- if below 60 have poor organ perfusion
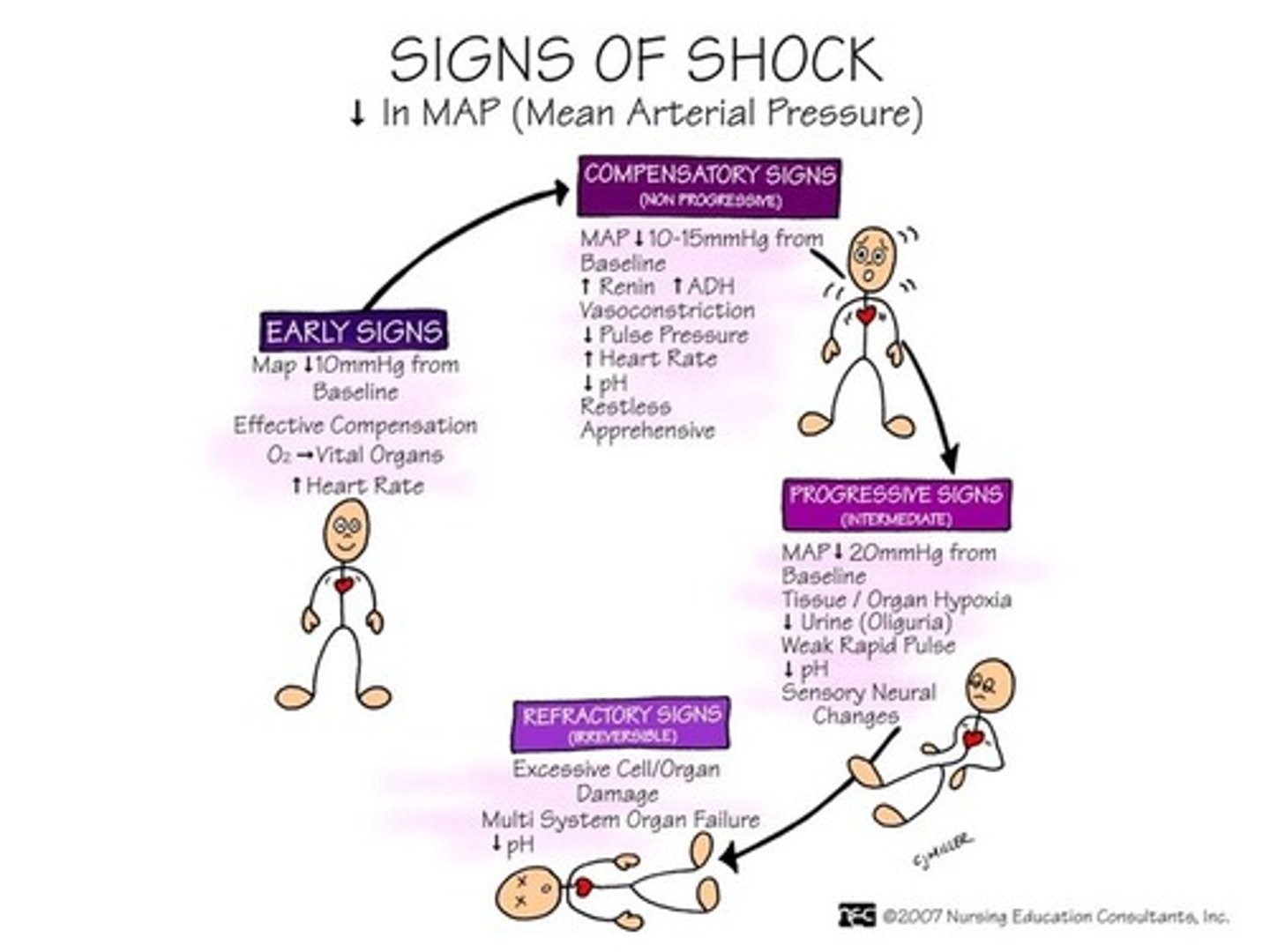
STAGES OF SHOCK: INITIAL STAGE
Usually not clinically apparent
Metabolism changes at cellular level from aerobic to anaerobic
- Lactic acid builds up and must be removed by liver
- Process requires O2, unavailable due to decreased tissue perfusion
Blood Pressure decreases - causes vasoconstriction
Which organs does the body prioritize to perfuse?
- Brain, Heart, Lungs
- So worry about kidneys and GI tract
- Changes in kidney output
- When in initial phase if fix patient should return to normal
Metabolism needs oxygen and glucose. If lose oxygen go from aerobic to anaerobic. This results in lactic acid build up which burns
STAGES OF SHOCK: COMPENSATORY STAGE
- Body can compensate for changes in tissue perfusion
- If cause of shock is corrected, patient recovers with little or no residual effects
- If cause of shock is not corrected, patient enters progressive stage
- Patient is transferred to ICU
- Major decrease in cellular perfusion
Symptoms
- Decreased BP so compensate by
* Increased HR, Vasoconstriction, Decreased U/O
- Then after:
* Stimulate SNS: so HR stays increased, Blood pressure goes up, cool, clammy skin to shunt blood flow to core.
- Then after:
* The heart will then Need more oxygen due to increased O2 heart consumption
* Eventually may shunt blood from lungs: dead air space in lungs -> issues with breathing
* If all this happens will need to enter ICU due to low BP maintenance and issues breathing.
STAGES OF SHOCK PROGRESSIVE STAGE
Clinical Assessment Findings:
- Anasarca
- Myocardial Dysfunction
- Third spacing of fluid
- Fluid moves into the alveoli
- GI System becomes ischemic
- Kidneys
- Liver Failure
1.Pulmonary system:
- Crackles, wheezing
- Fluid - alveoli (improper gas exchange)
GI: due to shunting
- constipation
- Paralytic ileus
- Absent/decreased bowel sounds
- Abdominal pain: Acid build up -> GERD, ulcers, aspiration; so will likely be on PPI
Liver failure
- Can't excrete lactic acid due no liver not getting oxygen
- Decreased Kidney perfusion
- Anasarca, third spacing
Cardiac
- Not getting enough oxygen
- Chest pain: myocardial ischemia
- Dysrhythmias: ST changes
- Edema
STAGES OF SHOCK: REFRACTORY STAGE
What are some assessment findings during the refractory stage of sepsis?
- Very very low Cardiac output: extremely low MAP (way below 60)
- Cells not being perfused
- Systemic hypoxia
- Multisystem organ failure
DIAGNOSTIC STUDIES with shock
Thorough history and physical examination
No single study to determine shock
- Blood studies
* Elevation of lactate
- 12-lead ECG, continuous ECG monitoring
- Chest x-ray
- Hemodynamic monitoring
- lactate with {sepsis}
- ECG - {cardiogenic}
- Chest X-ray: really any, anaphylactic, obstructive, septic, cardiogenic
- Hemodynamic: really all of them
LACTIC ACID: SEPTIC SHOCK
Aerobic - Anaerobic (absolute lack of oxygen)
- Lactic Acid builds-up
- Normal blood levels 0.5 - 1 mmol/L
- Sepsis criteria at above 2 mmol/L with a low blood pressure.
- Severe sepsis defined at Lactic Acid levels above 4 mmol/L
PROCALCITONIN: SEPTIC SHOCK
- Used in critically ill patients
- Levels determine if the condition is caused by a virus or bacteria
Test Result: Interpretation
- <0.05: Healthy
- 0.05 - <0.5: Systemic infection is unlikely
- 0.5 - <2.0: Systemic infection is possible but other causes (trauma, surgery, cardiogenic shock) may cause an increase
- >2.0: High likelihood to progress to sepsis
Generally in ICU
INTERVENTIONS with shock
- General management strategies
- Ensure patent is responsive
- Ensure a patent airway
- Maximize oxygen delivery
Hemoglobin levels can be dangerously low due to hypoperfusion. How can levels be increased?
- Fluids, blood, {volume expansion}
- If have issues with LOC think about oxygen
- If lose 1 ml of blood need 3 ml of isotonic solution (normal saline), if normal electrolytes and normal kidneys may use lactated ringer
VOLUME EXPANSION
Cornerstone of therapy for septic, hypovolemic, and anaphylactic shock = volume expansion
- One or two large-bore IV catheters or central venous catheter
- Isotonic Fluids
What are the priorities of the nurse while infusing isotonic fluids at a fast rate?
- With these types of shock Lose fluid so blood pressure bottoms out.
- Priority when infusing fast
* Fluid overload, Crackles, Shortness of breath, Weeping - legs, arms, Edema, Decreased LOC (lethargic) -> cerebral edema -> increased Intracranial pressure, Increased weight, Increased BP, Bounding pulses, Increased HR
The client's blood pressure remains low after fluid resuscitation. What is the next step in treatment?
Meds: Dobutamine, Dopamine, epinephrine, hydrocortisone, Norepinephrine (Levophed), Phenylephrine, Nitroglycerin, Sodium Nitroprusside, Vasopressin
- Dopamine cause renal vasodilation to increase blood pressure and increased renal perfussion
NUTRITION in shock
Nutrition is vital to decreasing morbidity from shock
- Start enteral nutrition within first 24 hours
- Parenteral nutrition used only if enteral feedings contraindicated
Need to ensure patients well hydrated and that cells have sugar and oxygen
SIRS (SYSTEMIC INFLAMMATORY RESPONSE SYNDROME)
SIRS is widespread inflammation that can occur in infection, trauma, shock, ect. May result from or lead to MODS. Most frequently associated with sepsis.
SIRS
- Pulmonary symptoms
-> pulm edema
-> wheezes, crackles
-> Diminished lung sounds
(SpO2 -> 92%) (generally less than 92% NOT GOOD)
-> Oxygen
-> Diuretics
-> steroids
-> albuterol
MODS
2 or more organs
Respiratory system is often first organ impacts by SIRS and MODS
- ARDS - Acute Respiratory Dysfunction Syndrome
- AKI - Acute Kidney Injury
- (cardiac, liver, endocrine, gastrointestinal system, etc.)
Very poor outcomes with three or more organs involved
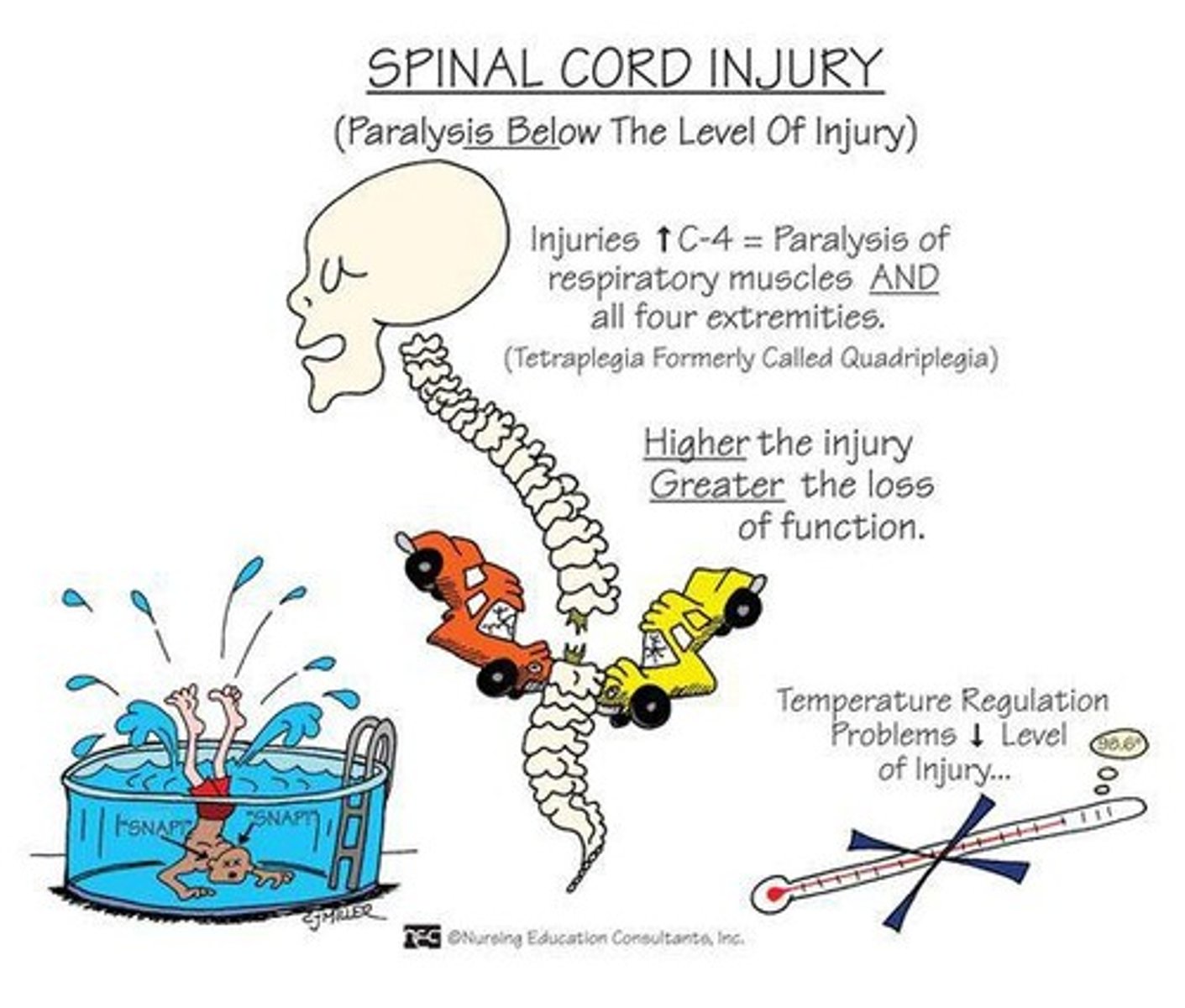
Spinal Cord Injury
- Trauma or damage to the spinal cord
- Can be temporary or permanent
- 17,000 Americans suffer an injury each year
- Can be large disruption of life, loss of function, economic impact
- Some remain at home some need nursing home care
- Gateway between brain and rest of body
- In injury gateway is broken
Preventing head injuries
- No texting while driving
- Seat belts
- Car seats
- Helmets bikes and motorcycles
- Drunk driving, impaired driving
- Using safety equipment while playing sports
common causes of head injury
Most common men 16 - 30
1.Motor vehicle accidents
2.Falls
3.Violence
4.Sports
5.Miscellaneous
Type of Injuries of spine
Primary Injury
- Initial impact (trauma, compression, gunshot wound)
* Why suffer injury originally
- Secondary Injury
* Ongoing progressive damage
* Cell death
* This can go on weeks or months after initial injury
* Hemorrhagic areas can happen within an hour - ischemia within a few hours
* Edema can cause permanent damage
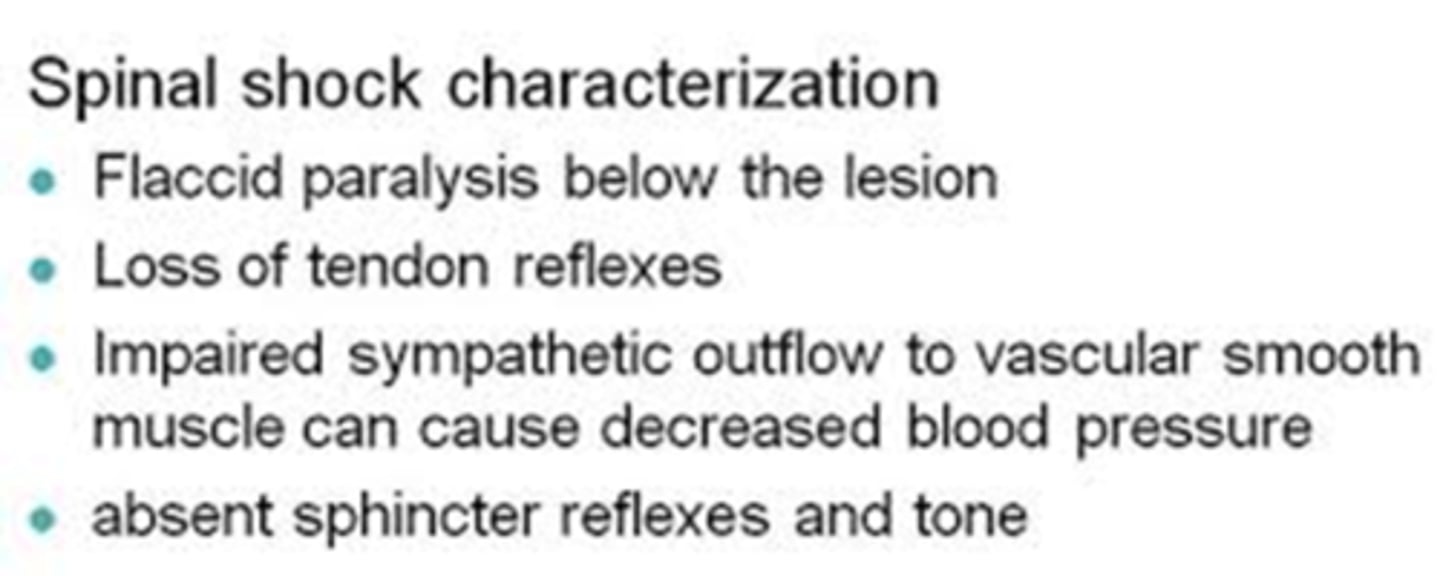
Spinal Shock
Characterized by
- ↓ Reflexes
- Loss of sensation
- Absent thermoregulation
- Flaccid paralysis below level of injury
- Lasts days to weeks
- Issue with Injury
- Transient condition that presents after acute spinal cord injury
- Not a circulatory disorder
- Masks post-injury neurologic function
Assessment findings:
- loss of deep tendon reflexes
- Loss of sphincter reflexes
- Loss of sensation
- Flaccid paralysis
neurogenic shock due to spinal injury
Characterized by
- Hypotension
- Bradycardia
- Loss of SNS innervation
- Peripheral vasodilation
- Venous pooling
- ↓Cardiac output
- T5 or higher injury
- ISSUE with Circulation
- Hemodynamic result of spinal cord injury at or above T5
- Can occur within 30 minutes of spinal cord injury
- Lasts up to 5-6 weeks
- Massive vasodilation (loss of SNS vasoconstrictor tone)
- Pooling of blood in blood vessels, tissue hypoperfusion, and impaired cellular metabolism
Assessment findings:
- hypotension
- Bradycardia
- unable to regulate body temperature
- Warm at first, but then skin cools taking on temperature of the environment (poikilothermia)
Medication
- Atropine to increase Bradycardia
- Vasopressors (levophed, noroepinephrine, phenelephrine) to increase BP
- Fluids (NS) - to sustain patients
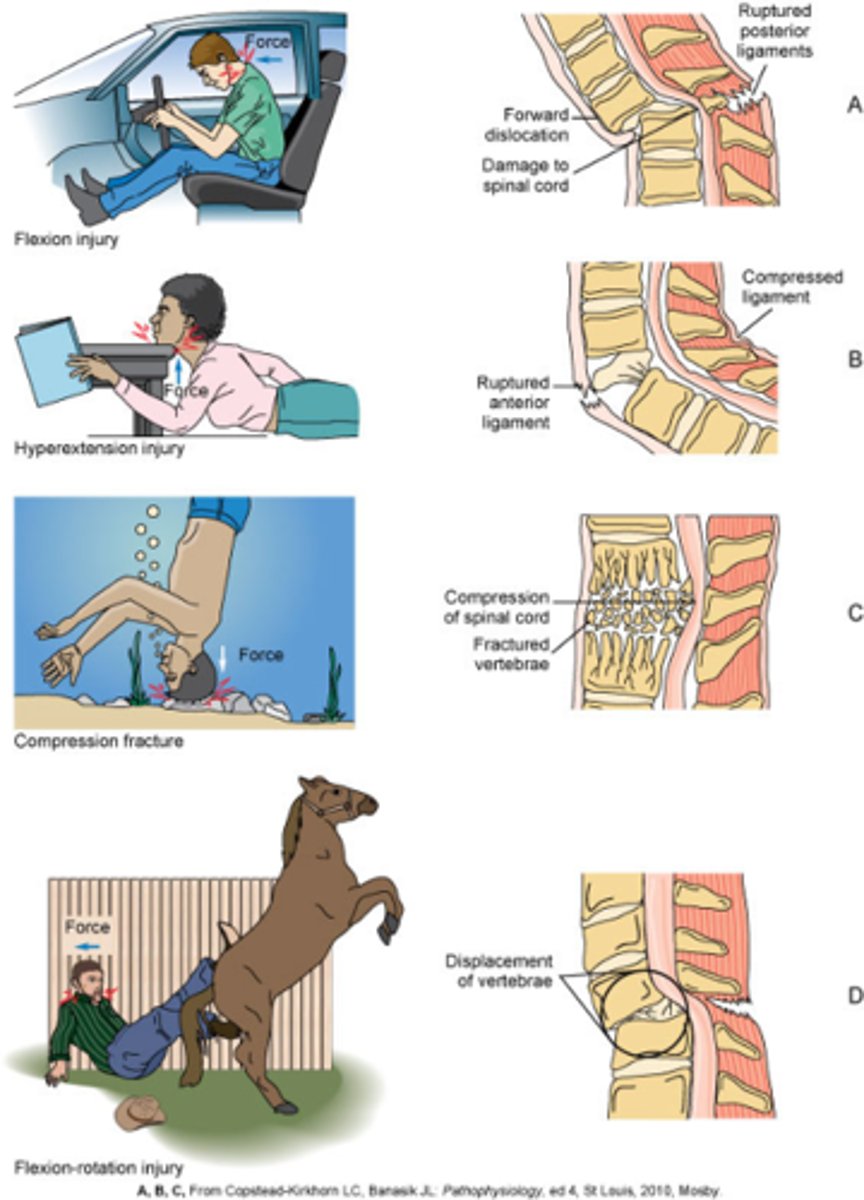
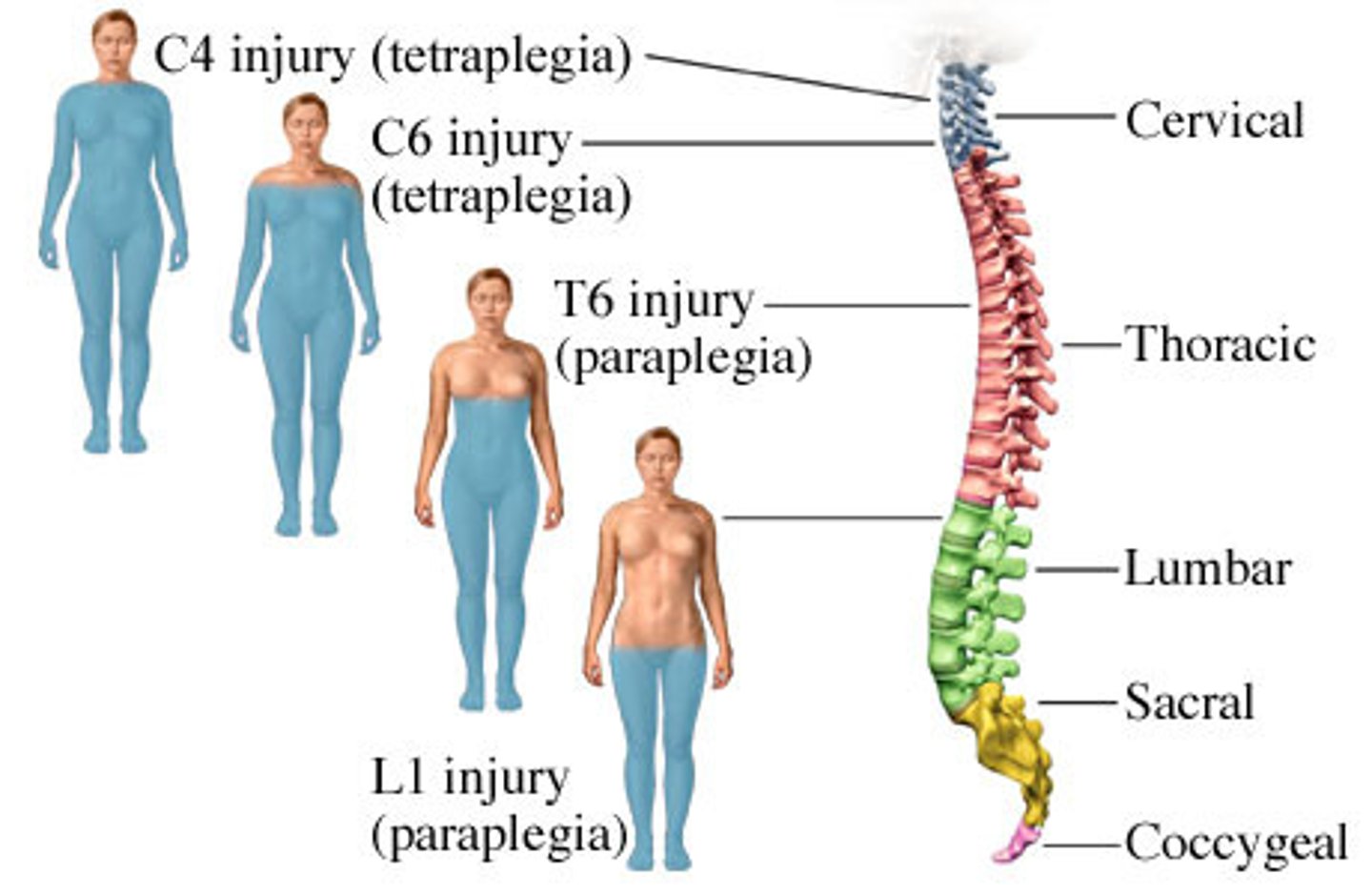
Classifications of Spinal Cord Injury
3 types
- Mechanism of Injury
* Flexion, hyperextension, compression, flexion-rotation injury
- Level of Injury
* Skeletal level
-- Neurologic level is the lowest segment of the spinal cord with normal sensory and motor function on both sides of the body
----* Tetraplegia (quadriplegia) - all four extremities
----* Paraplegia - loss of sensation of the legs
- Degree of Injury
* Complete and incomplete - motor and sensory
loss based on injury location
- Cervical - tetraplegia
- C4 level or higher - need mechanical ventilation
- Thoracic - paraplegia
- Lumbar - paraplegia (just legs effects)
- Sacral - mostly elimination concern
Mechanisms of spinal Injury
Complications from Spinal Cord Injuries
Respiratory system
- Respiratory depression, Decreased lung expansion, Decreased cough, C4 or higher will need mechanical ventilation
- Management: Augmented cough, Chest PT, Vibrating chest
- Risks: Pneumonia, Aspiration risk
- Cardiac: Decreased circulation, Decreased peripheral circulation: SNS T9
* Interventions: Pulse check, SCDs, VTE, Medications
- Urinary system: Incontinence, Neurogenic bladder, UTI
* Interventions: Catheter, Suprapubic Cath, Bladder scan, Antibiotics and cultures if needed
Spinal Cord Injuries
How would the GI system and Integumentary systems be affected by a spinal cord injury?
GI
- Decreased motility
- Blockages/constipation
- Ileus
- Stress ulcers
- Aspiration
- Intervention: PPI (Pantoprazole - IV), Laxative, NG tube, Ostomy, Speech therapy, Occupational therapy, Mobility as possible
Skin
- Breakdown
- Pressure injury
- Infections
- Dry skin
- Intervention: Skin assessment, Repositioning/turning, Hygiene, Increase protein, moisturizer
Metabolic Concerns with spinal injury
Electrolytes imbalance from NG tube and suctioning
- Weight loss is common
- High protein diet
Which type of acid-base issue would the nurse expect?
- Metabolic alkalosis - getting rid of body acid in stomach
Diagnostic Studies with spinal injury
- CT scan is the preferred
- MRI soft tissue
- Doppler studies for DVT
Immediate Goals after an Injury to the spine
Patient airway
Adequate circulating blood volume
- Check pulse, cap refill, BP, Heart rate, urinary output
Preventing secondary injury
- Recommended immobilization includes a backboard and straps
* Not always recommended with penetrating trauma
* Don't want vertebra to move and cause more damage
Treatments after spinal injury
Non-operative
- Stabilization - eliminate movement to cause more damage while healing
Surgical therapy - many options to stabilize spine, reduce compression, anterior approach and posterior approach
Medication Therapy with spinal injury
Low-molecular-weight heparin
- Prevent VTE
Vasopressor agents
- Maintain mean arterial pressure >85-90 mm Hg
- Significant risk of complications
Want to perfuse spinal cord to help heal and maybe reverse if spinal shock
Phenylephrine and levophed
- Can have cardiac complications when trying to keep MAP > 85
* Dysrhythmias
-- V. Tach
-- A. Fib
* Elevated troponin levels
Respiratory Dysfunction with spinal injury
First 48 hours are most critical.
Assessment
- lung auscultation
- SpO2
- shallow breathing (issue with effort)
Risk for aspiration
- leave head of bed up
Want to help get mucus up to prevent pneumonia
Cardiovascular Instability with spinal injury
Low BP
Low HR
Dysrhythmias
Bladder and Bowel Management with spinal injury
Neurogenic bladder - Foley, no sensation of full bladder bladder can rupture
- CAUTI
- Intermittent catheterization
Bowel Program
-Neurogenic bowel - no voluntary or involuntary reflex
Spasticity with spinal injury
- Can be both beneficial and undesirable
- Ashworth and modified Ashworth scales
- Treatment
* ROM exercises
* Antispasmodic drugs
* baclifen
* Botulinum toxin injections
Involuntary movement
- can cause contractions
- keeps muscles moving
Autonomic Dysreflexia with spinal injury
Massive uncompensated cardiovascular reaction mediated by sympathetic nervous system
- SNS responds to stimulation of sensory receptors - parasympathetic nervous system unable to counteract these responses.
- Hypertension and bradycardia
Causes: Kinked catheter, Tight clothes, Fecal impaction, Kidney stones
- Results In: Flushing above injury, Decrease in HR, Increase in BP
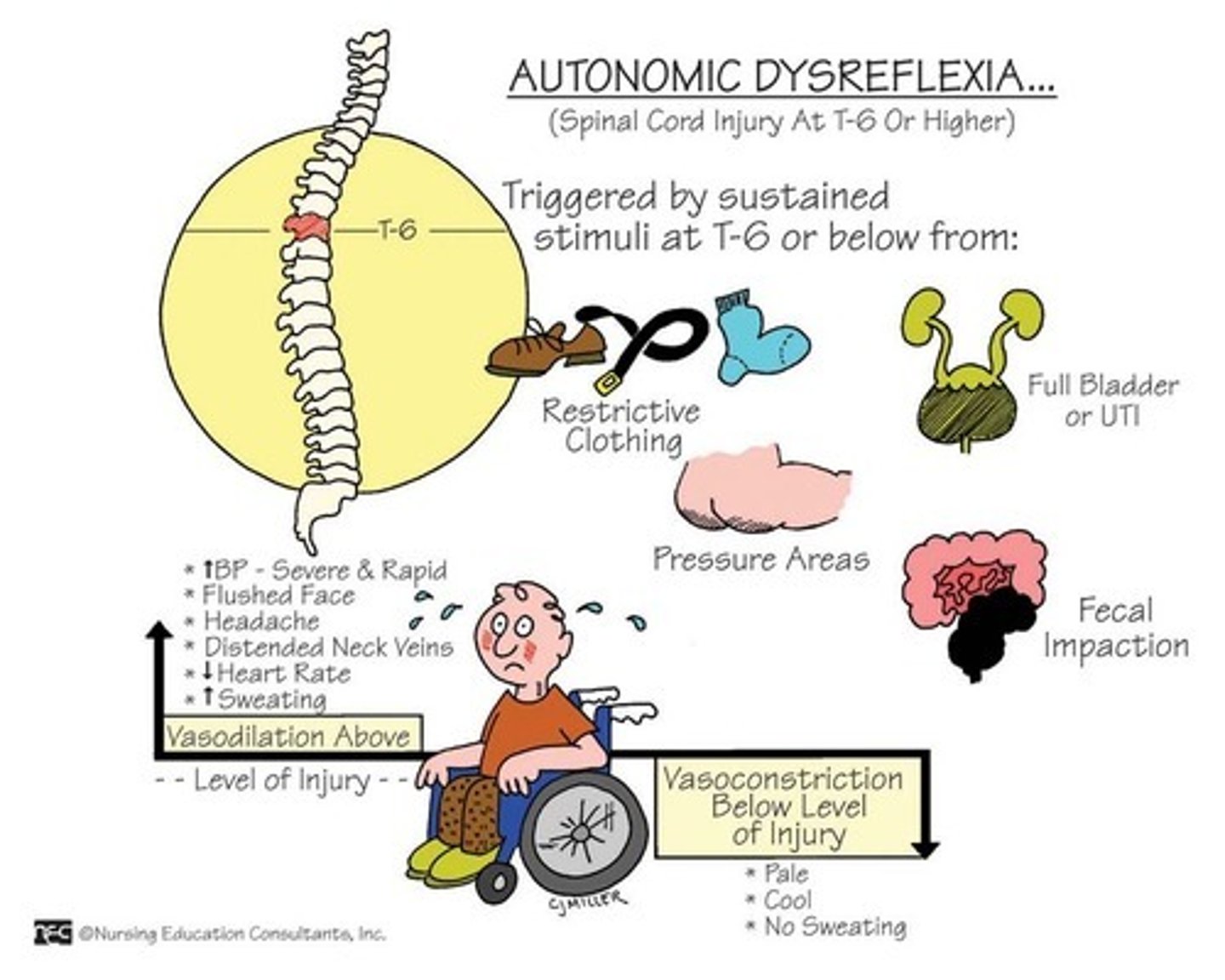
Autonomic Dysreflexia manifestations
Most common precipitating factor is distended bladder or rectum
Manifestations
- Hypertension (up to 300 mm Hg systolic)
- Throbbing headache
- Marked diaphoresis above level of injury
- Bradycardia (30 to 40 beats/minute)
- Sit patient upright
- Loosen anything that is tight
- Socks
- belt
Manifestations
- Flushing of skin above level of injury
- Blurred vision or spots in visual field
- Nasal congestion
- Anxiety
- Nausea
Autonomic dysreflexia nursing interventions
Nursing interventions
- Elevate head, sit upright
- Notify HCP
- Assess for and remove cause
- Immediate catheterization
- Remove stool impaction if cause
- Remove constrictive clothing/tight shoes
- Monitor and treat BP
- Patient and caregiver teaching
Rehabilitation with Spinal Injury
- Respiratory
- Bladder - Long term catheter placement and care
- Bowel - bowel programs
- Spasticity - involuntary movements
- Skin care
- Pain Management
- Sexuality
- Grief and Depression
components of intra cranial area
Components
- brain, blood, cerebral spinal fluid
What causes increased ICP?
Causes:
- trauma to head
- strokes
- meningitis
- leaning over
- sneezing, coughing
- eating too much
Transient increases are normal. (pressure fluctuates a little bit)
Brain hematoma
Bleeding in the brain
Pressure pressing brain into skull
Widened pulse pressure
- normal should be 40 - 60 mm Hg
- widened pulse pressure causes Decreased Cardiac Output
- so worry about Decreased Perfusion to the Brain
Can easily be hypothermic
Can have decreased Respirations
both due to pressure/damage to brain stem
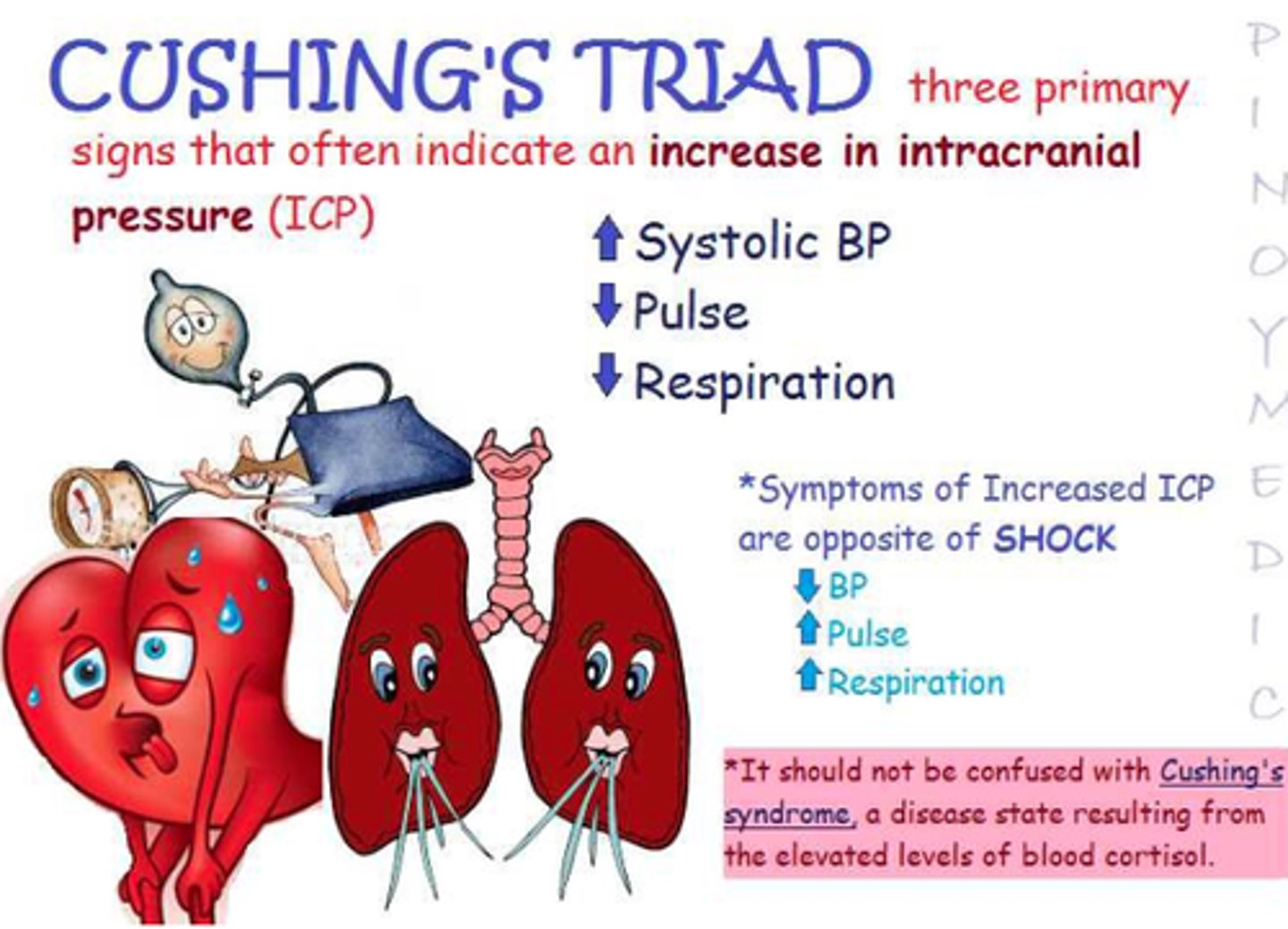
Brain could go into Cushing's triad
- Systolic HTN, Widened pulse pressure
- Decreased HR (bradycardia)
- Irregular breathing pattern (Decreased respirations)
- {IF THIS HAPPENS IN NEUROLOLOGIC EMERGENCY AND CAN'T COMPENSATE}
STAGES OF INCREASED ICP
- Stage 1: Total compensation
* hit head but feel fine
- Stage 2: ↓ Compensation; risk for ↑ICP
* starting to have changes
- Stage 3: Failing compensation; clinical manifestations of ↑ ICP (Cushing's triad)
* have Cushing's triad symptoms
- Stage 4: Herniation imminent → death
HERNIATION AND CEREBRAL EDEMA
Brain is enlarging and coming out of where shouldn't
Edema - swelling due to pressure and fluid on the brain
LOC Changes with increase in ICP
LOC Changes
- confusion - agitation
- lethargy
- difficulty arousing
- loss of consciousness
- disoriented
- comatose
- changes in pupils (sluggish, blown pupil)
- Vomiting
- hyperthermia
NURSING ASSESSMENT FINDINGS with ICP
Change in level of consciousness
- Flattening of affect → coma
Change in vital signs
- Cushing's triad (widened pulse pressure, bradycardia, irregular respirations)
- Change in body temperature (will get hyperthermic)
Cushings Triad
Signs of increased intracranial pressure:
1. hypertension
2. bradycardia
3. irregular respirations
NURSING ASSESSMENT FINDINGS with increased ICP
- Compression of oculomotor nerve (Oculomotor nerve (cranial nerve 3))
* Unilateral pupil dilation
* Sluggish or no response to light
* Inability to move eye upward
* Eyelid ptosis
- ↓ In motor function
- Hemiparesis/hemiplegia
- Decerebrate posturing (extensor)
- Indicates more serious damage
- Decorticate posturing (flexor)
DIAGNOSTIC STUDIES
- CT scan / MRI / PET
- EEG (electrical activity in the brain)
- Cerebral angiography (perfusion)
- ICP and brain tissue oxygenation measurement
- Transcranial doppler studies
- Evoked potential studies
- NO lumbar puncture
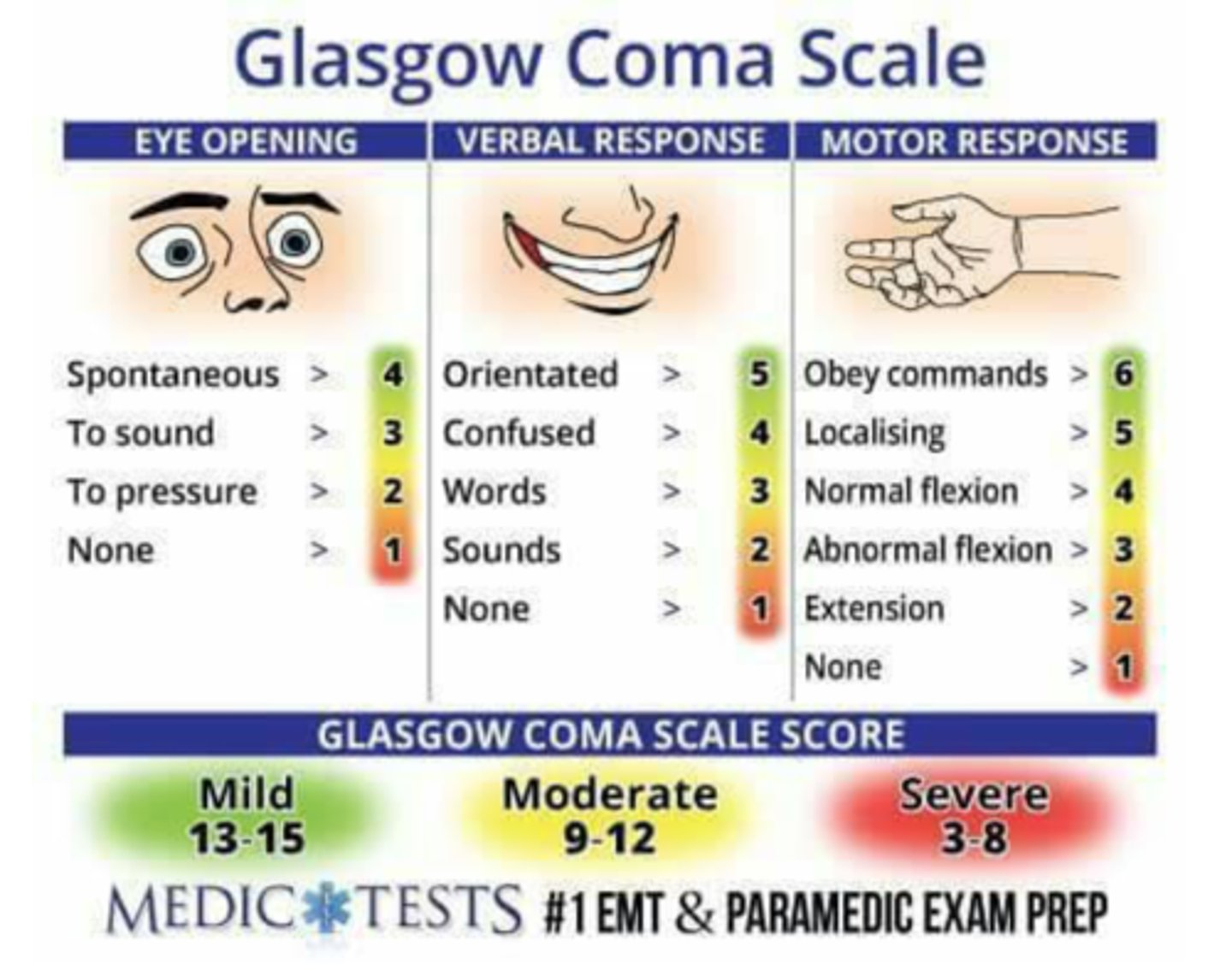
MEASUREMENT OF ICP
Guides clinical care
Indications
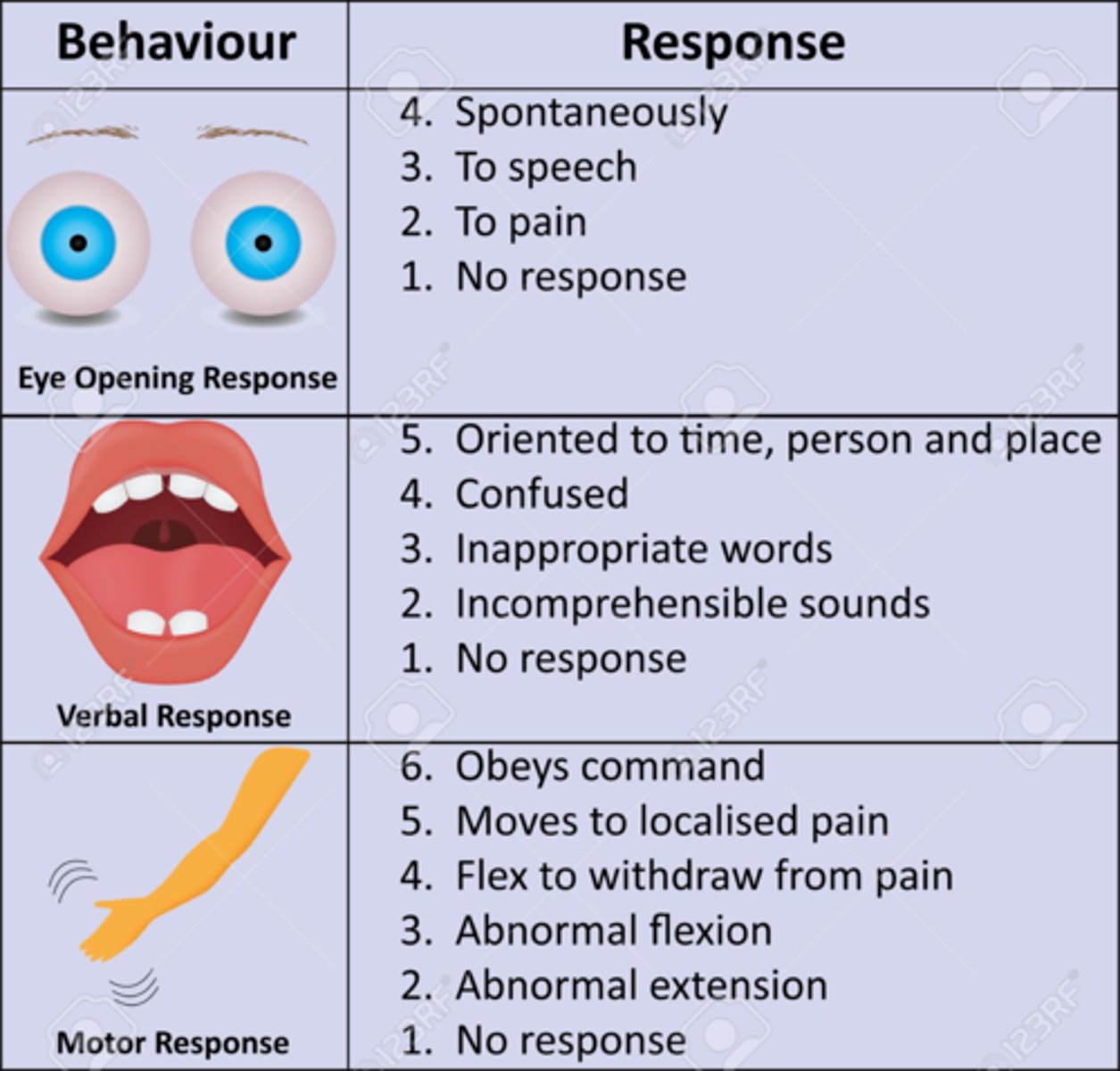
- Glasgow Coma Scale of ≤8
- Abnormal CT scans or MRI
Pupillary changed with increased ICP
- Puipils equal and react normally
- Pupil reacts to light (slowly or briskly)
- Dilated pupil (compressed cranial nerve III)
- Bilateral dilated, fixed pupils (ominous sign)
- Pinpoint pupils (pons damage or drugs)
MEASUREMENT OF ICP devices
- Ventriculostomy
* Catheter inserted into lateral ventricle
- Coupled with an external transducer
Ventriculostomy is gold standard for measuring ICP (normal is 5 - 15)
- can monitor ICP and drain fluid (CSF)
- in the ICU
Apparatus would need to be zeroed
- if not could have incorrect reading
Huge infection risk
- infection precautions
- chlorohexidine to site
- prophylactic antibiotics
- monitor WBC count (neutrophils)
DRUG THERAPY for increased ICP
Drug Therapy
- Mannitol (Osmitrol)
* Plasma expansion
* Osmotic effect
* Monitor fluid and electrolyte status
- Hypertonic saline (use with caution)
* Moves water out of cells and into blood
* Monitor BP and serum sodium levels
-- Risk for fluid overload
Mannitol is diuretic that is used for intracranial pressure by pulling fluid off of brain
Monitor potassium, sodium, and may calcium
- Corticosteroids
* Monitor fluid intake, serum sodium and glucose levels
* Concurrent antacids, H2 receptor blockers, proton pump inhibitors
Decrease inflammation everywhere including the brain
- worry because increase glucose
- if dev. Cushing could have increased sodium which increase fluid and could have decrease potassium
At risk for ulcers so will be on antacids, H2, PPI
Additional:
- Antiseizure medications: risk for seizure
- Antipyretics: risk for hyperthermia
- Sedatives: if combative
- Analgesics: if have pain
- Barbiturates: If at risk of seizures but want to use carefully
NUTRITION with increased ICP
Nutritional Therapy
- Hypermetabolic and hypercatabolic state ↑ need for glucose
- Enteral (if possible) or parenteral nutrition
- Early feeding (within 5 days of injury)
- So can get glucose and heal faster
NURSING PRIORITIES with increased ICP
Respiratory function
- Maintain patent airway
- Elevate head of bed 30 degrees
- Suctioning needs
- Minimize abdominal distention
- Monitor ABGs (CO2 levels)
- Maintain ventilatory support
- Worry about #1 airway, so elevate bed to {30 degrees}. But no more than 30 degrees.
- Need to make sure if they actually need to be suctioned because coughing can increase ICP
Fluid and electrolyte balance
- Monitor IV fluids
- Daily electrolytes
Monitor and minimize increases in ICP
PATIENT POSITIONING with increased ICP
HOB elevated appropriately
- Prevent extreme neck flexion
- Turn slowly
- Avoid coughing, straining, Valsalva
- Avoid hip flexion
- 30 degrees
what is a seizure and what are some causes?
- Fever
- Glucose
- Damage
- Anything that can alter pathway in brain
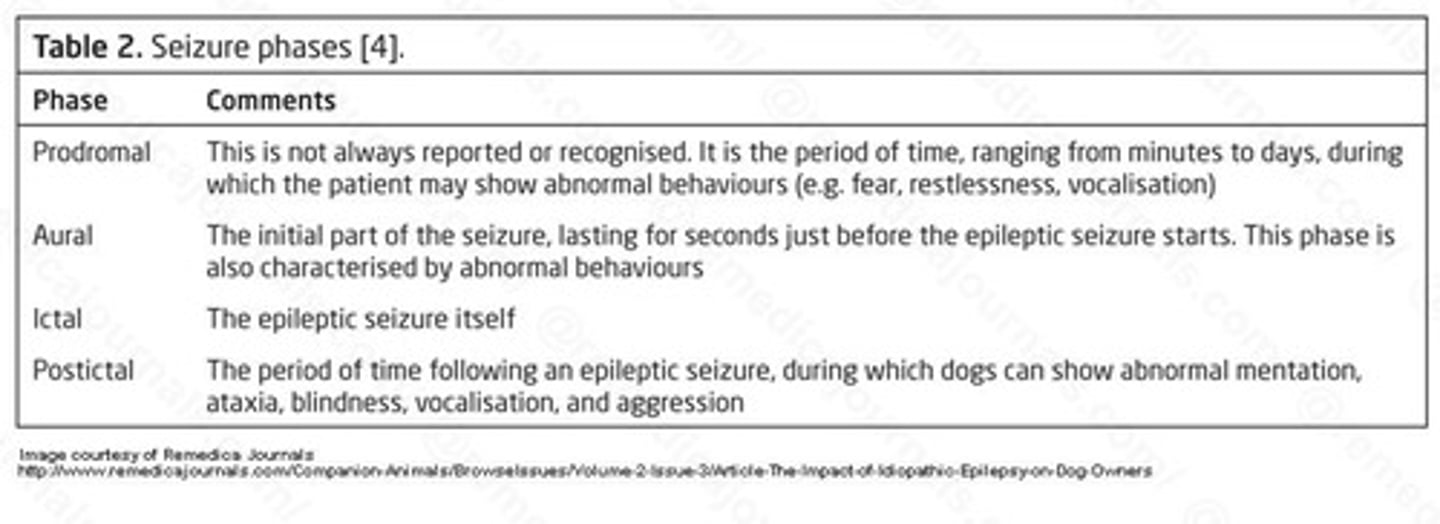
Clinical Manifestations of Seizures
May progress through several phases
- Prodromal phase
- Aural phase
- Ictal phase
-Postictal phase
Complications of Seizures
Status epilepticus (SE)
- State of continuous seizure activity or condition when seizures recur in rapid succession without return to consciousness between seizures
* Any seizure lasting > 5 minutes
* Neurologic emergency
* Can occur with any type of seizure
Have one seizure after another
Medication of choice diazepam or lorazepam
what is the priority during the seizure
- During a seizure, what is the priority of the nurse?
During a seizure
- Maintain patent airway
- Protect patient's head
- Turn patient to the side
- Loosen constrictive clothing
- Ease patient to floor
- Do not restrain patient
- Do not place objects in patient's mouth
Nursing Assessment with seizure
- Bitten tongue, soft tissue damage, cyanosis
- Abnormal respiratory rate
- Apnea (ictal)
- Absent or abnormal breath sounds
- Airway occlusion
- Hypertension, tachy/bradycardia
- Bowel/urinary incontinence, excessive salivation
- Weakness
- Excessive Somnolence
Diagnostic Studies of Seizures
EEG
- May help determine type of seizure and pinpoint seizure focus
- Many patients do not have abnormal findings
- Not definitive because many patients may not have abnormal findings
CBC, Chemistry Panel
CT or MRI in new-onset seizure to rule out structural lesion
Cerebral angiography
- Diagnosing seizure type is necessary to determine appropriate treatment
Chemistry - worry about electrolytes (sodium)
CBC - RBC (anemia can cause issues with oxygenation)
CT/MRI look for tumors
Drugs for Seizures
Seizure disorders are primarily treated with antiseizure drugs
- Goal of therapy is preventing seizures with minimum toxic side effects from drugs
- Cure is not possible
- Antiseizure drugs should not be discontinued abruptly as this can precipitate seizures
- Common side effects involve the CNS and include diplopia, drowsiness, ataxia, and mental slowing
- Can get really drowsy
- Compliance can be an issue
Primary drugs for treatment of generalized tonic-clonic and focal seizures
- Phenytoin (Dilantin)
- Carbamazepine (Tegretol)
- Phenobarbital (Luminal)
- Divalproex (Depakote)
- Primidone (Mysoline)
Primary drugs used to treat absence and myoclonic seizures
- Ethosuzimide (Zarontin)
- Divalproex (Depakote)
- Clonazapam (Klonopin)
•Broad spectrum drugs can be effective for multiple seizure types
- Gabapentin (Neurontin)
- Topiramate (Topamax)
- Lamotrigine (Lamictal)
- Tiagabine (Gabitril)
- Levetiracetam (Keppra)
- Zonisamide (Zonegran)
Pregabalin (Lyrica)
Additional treatment for focal seizures that are not successfully controlled with a single medication
Status epilepticus
- Initially, rapid-acting IV lorazepam (Ativan) or diazapam (Valium)
- Followed by long-acting drugs
Surgical Interventions for seizures
Vagal nerve stimulation
- Adjunct to medications when surgery is not feasible
- Exact mechanism not known
- Thought to interrupt synchronization of epileptic brain-wave activity and stop excessive discharge of neurons
Surgery is an option for many with uncontrolled epilepsy
- Anterior temporal lobe resection
- About 70%-80% are seizure free after this procedure
- 10%-20% have marked reduction in seizure activity
In the emergency department setting, which are the priority focused assessments that should be performed first?
Airway, breathing, circulation order depending on patient
Emergency nursing order of priorities
ABCDEFG...
- Alertness and airway
- Breathing
- Circulation
- Disability
- Exposure and environmental control
- Full set of vitals and family presence
- Get monitoring devices, give comfort
Emergency Nursing - primary nursing
Focuses on
- Airway, breathing, circulation (ABC)
- Disability, exposure, facilitation of adjuncts and family, get resuscitation adjuncts
Uncontrolled external hemorrhage
- Reprioritized to
- Direct pressure
- Pressure dressing
If life-threatening conditions related to ABCs are identified during primary survey, interventions are started immediately and before proceeding to the next step of survey
Alertness and airway
- Determine LOC
- Assess patient response to verbal and/or painful stimuli
- AVPU
* A=alert
* V=responsive to voice
* P=responsive to pain
* U=unresponsive
- LOC, pupillary response (PERRLA), chest rise, lung sounds, vitals (O2) (resp), airway obstruction, patent airway
- sniffing position, O2 if indicated, spine stabilization, Intubate/establish airway
Breathing
- assess ventilation, lung sounds, chest expansion, O2
- O2, intubate, chest tube
Circulation
- pulse, heart rate, cap refill, assess for signs of bleeding
- control bleeding, ensure circulation
Disability
- neuro check, mobility, pain, cranial nerve, speech
- x-ray or imaging, pain control, reorientation, headache, cast, splint
Exposure and environmental control
- safety, rapid triage/vitals, safety scan, neuro exam, ortho consults, hypo/hyperthermia
- labs, xray, spine immobilization, wound irrigation, hypo/hyper thermia manament
Full set of vitals and family presence
- what to do if code and family presence as a result
Get monitoring devices, give comfort
- labs -> CBC (bleeding), type and cross blood, blood sugar, glucose, pregnancy test, urinalysis, CMP, EKG, troponin
- monitor cardiac status -> telemetry
- Pain assessment: opioids, NSAIDS, ketorolac
- NG tube -> if head injury or facial trauma
- O2 + Ventilation -> cont. pulse ox
Airway obstruction
Cause of nearly all immediate trauma deaths
- Irritability, restlessness, gurgling, decreased sats, increased HR, Increased RR, Inspiratory stridor, grabbing at neck, drooling, tripod, accessory muscles, cyanosis
Treatment with airway issues in primary survey
- Open airway
- Suction and/or remove foreign body
- Insert nasopharyngeal or oropharyngeal airway
- In unconscious patients only
- Endotracheal intubation
What are the priority assessments in assessing breathing/ventilation?
Primary assessment for assessing breathing/ventilation
- Chest rise and fall, SPo2, accessory muscles, resp rate, auscultate, symmetry, Capnography, tripod, gasping, sit up, coughing
Concerning lung sounds primary survey
Concerning lung sounds
- Anything adventitious
What are the priority assessments in assessing circulation?
Pulses, color, temp, edema, BP, cap refill, SPo2, HR, LOC changes, fluid (NS), vasopressors, blood
Neurological Assessment with primary survey
Neurological Assessment
- Measured by patient's level of consciousness
- Glasgow Coma Scale
* Standardized for consistent communication among care team members
- Pupils
Secondary Survey
Brief, systematic process to identify all injuries
- History
- Head, neck, and face
- Chest
- Abdomen and flanks
- Pelvis and perineum
- Extremities
- Inspect posterior surfaces
- Just keep reevaluating
secondary surgery - History and head-to-toe assessment
- Obtain history and mechanism of injury, or illness from patient, caregivers, friends, bystanders, and emergency personnel
- Provides suggestions for specific assessment and intervention