lab 2 - heart & blood vessels
1/36
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
37 Terms
structure of arteries vs veins
arteries carry blood away from the heart, they have thicker, more muscular and elastic walls and smaller lumens than veins,
veins are not surrounded by muscle tissue, they rely on skeletal muscle contractions and valves in their lumens to help return blood to the heart veins carry blood towards the heart
capillaries are the tiny vessels through which gas, nutrient, and waste exchange occurs, Capillaries are so small that red blood cells must travel through one cell at a time
brachiocephalic trunk
anterior branches of the aorta are unpaired at first because the right common carotid and right subclavian arteries leave the aorta as one vessel (brachiocephalic trunk)
left common carotid and left subclavian arteries
vessels arising from the aortic arch
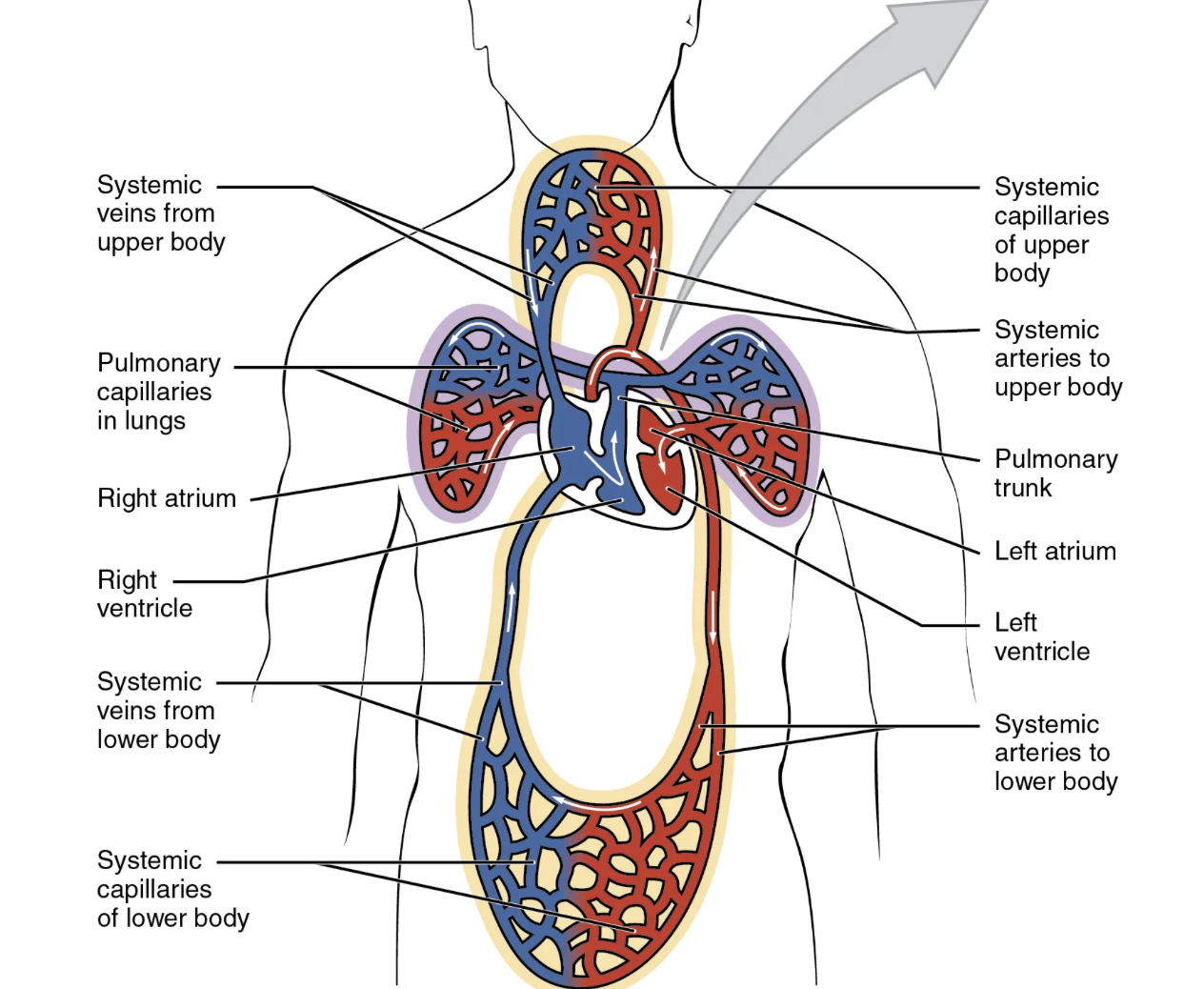
the aorta
extends inferiorly through the thoracic cavity, passing through the diaphragm and into the abdominal cavity. Most of the vessels branching off of the abdominal aorta do so as pairs (e.g., the left and right renal arteries
unpaired branching arteries
the celiac trunk and the superior and inferior mesenteric arteries). The abdominal aorta ends in the pelvis when it splits into the left and right common iliac arteries
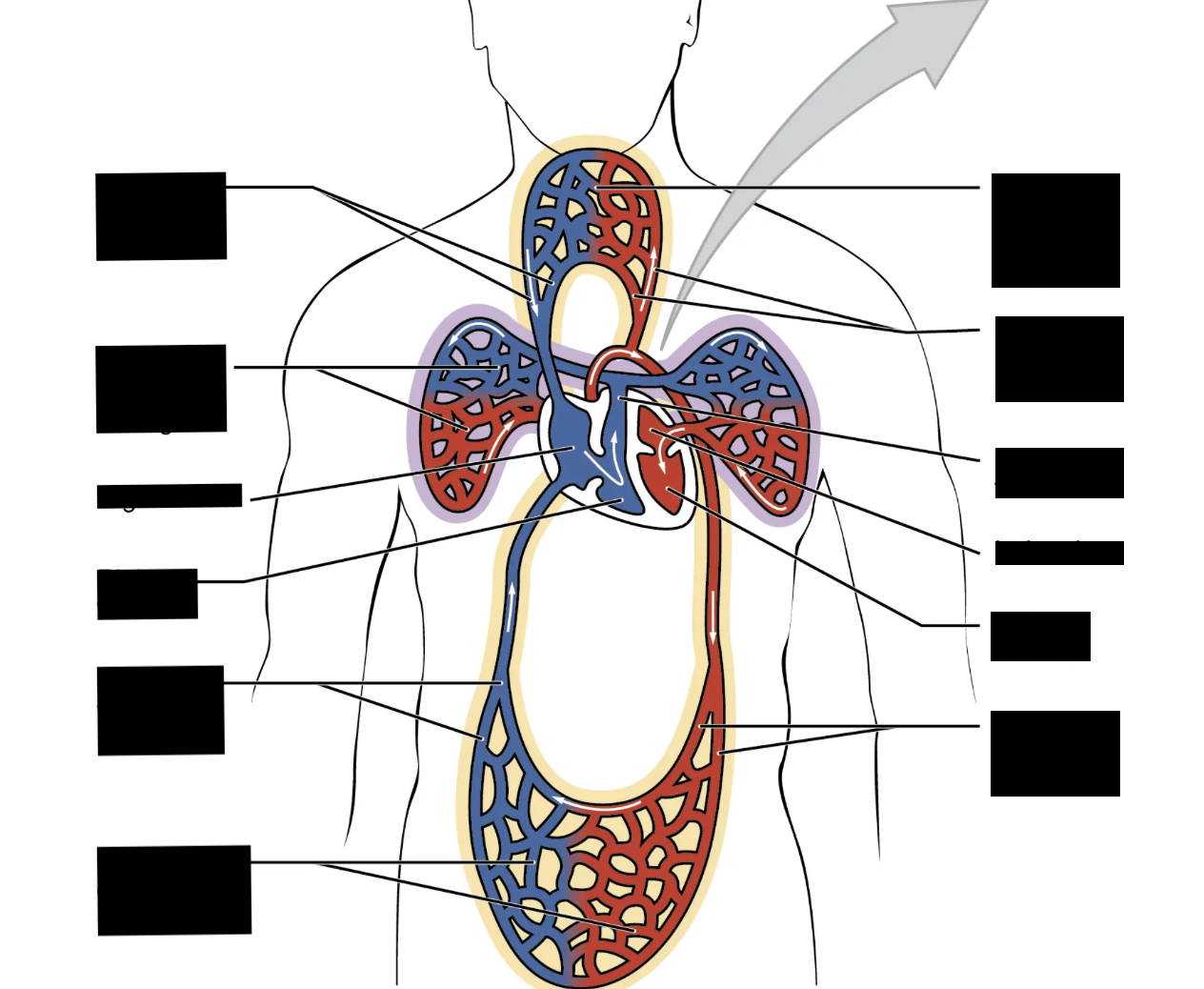
veins returning blood back to heart
A series of veins return blood from the tissues to the right atrium of the heart. Identify the superior and inferior vena cavae, left and right subclavian veins, left and right renal veins, and the left and right common iliac veins
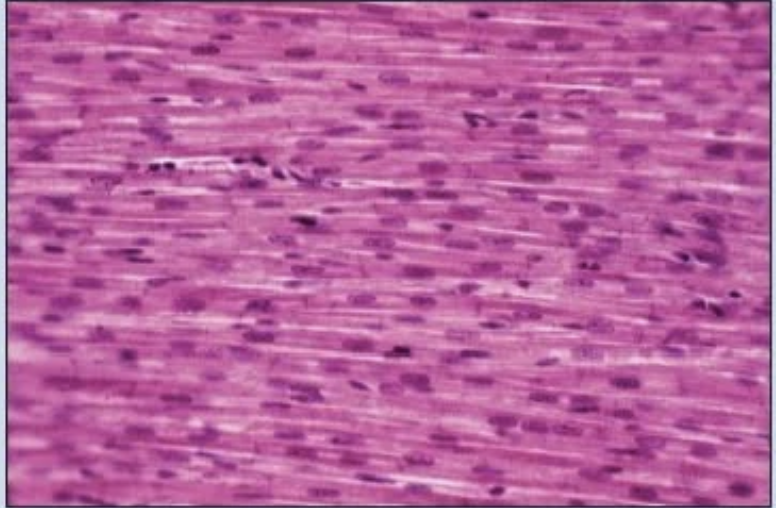
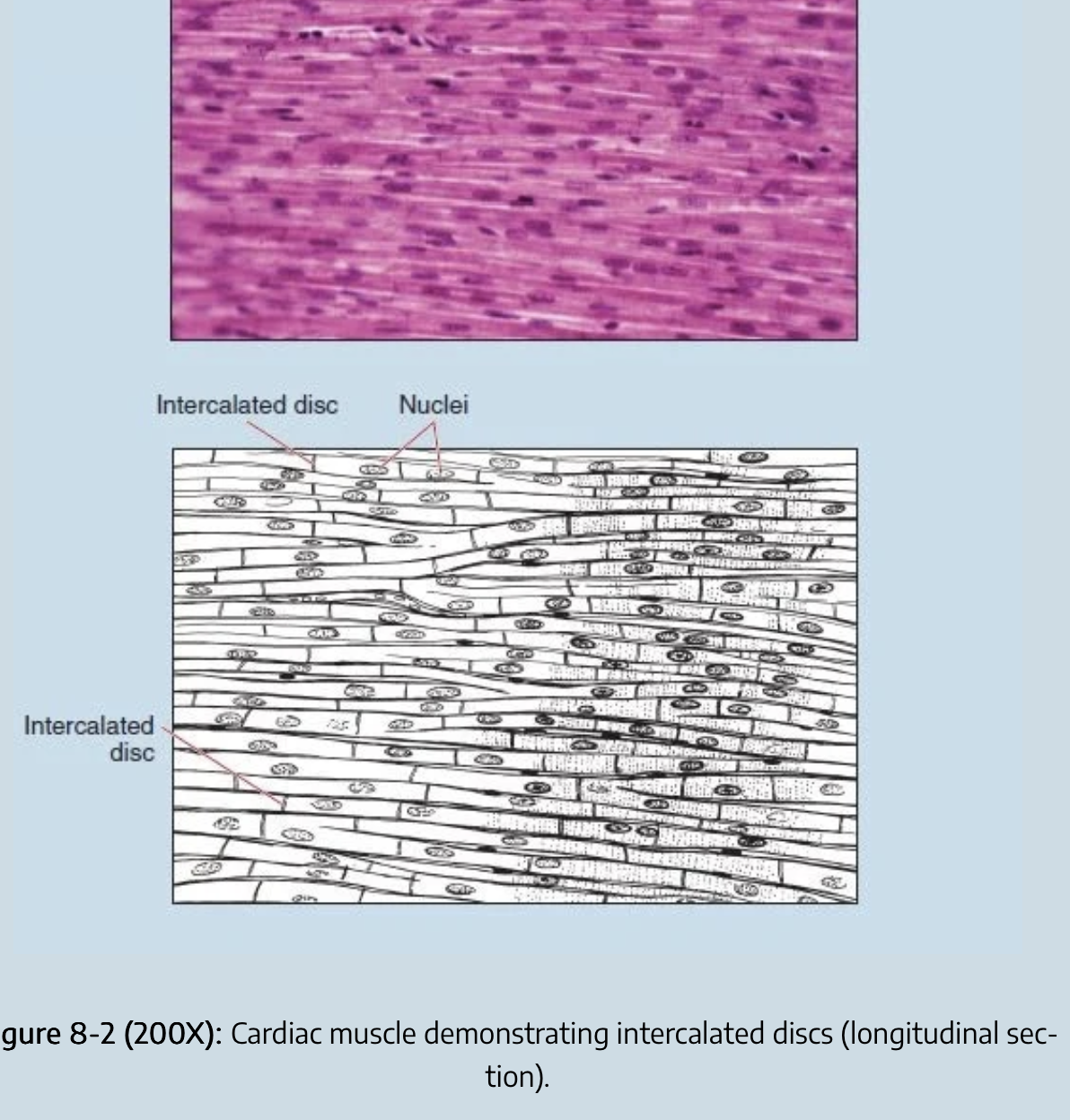
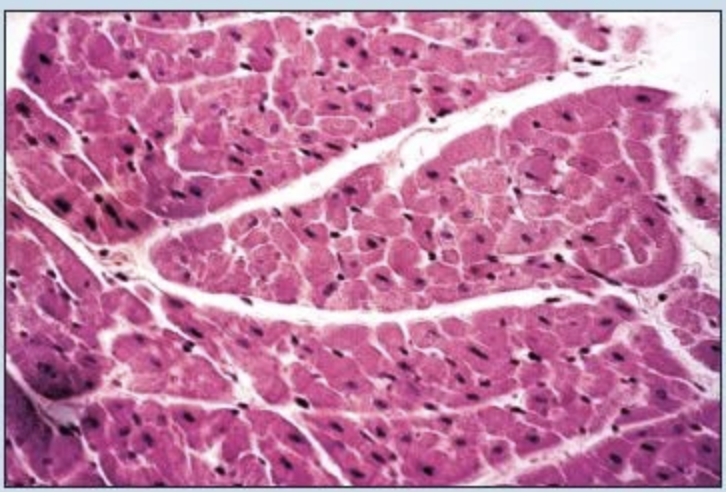
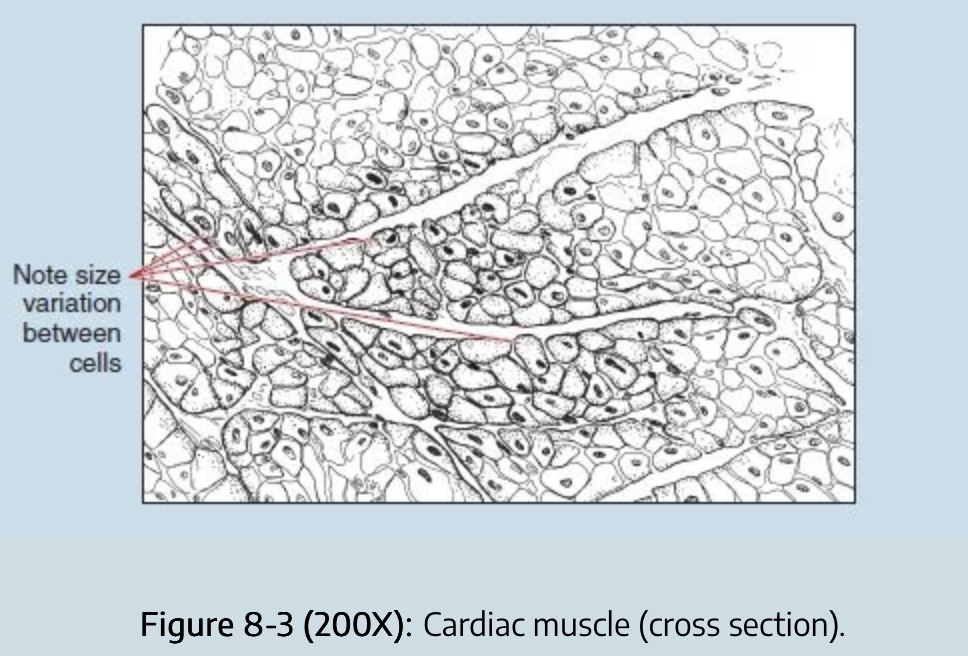
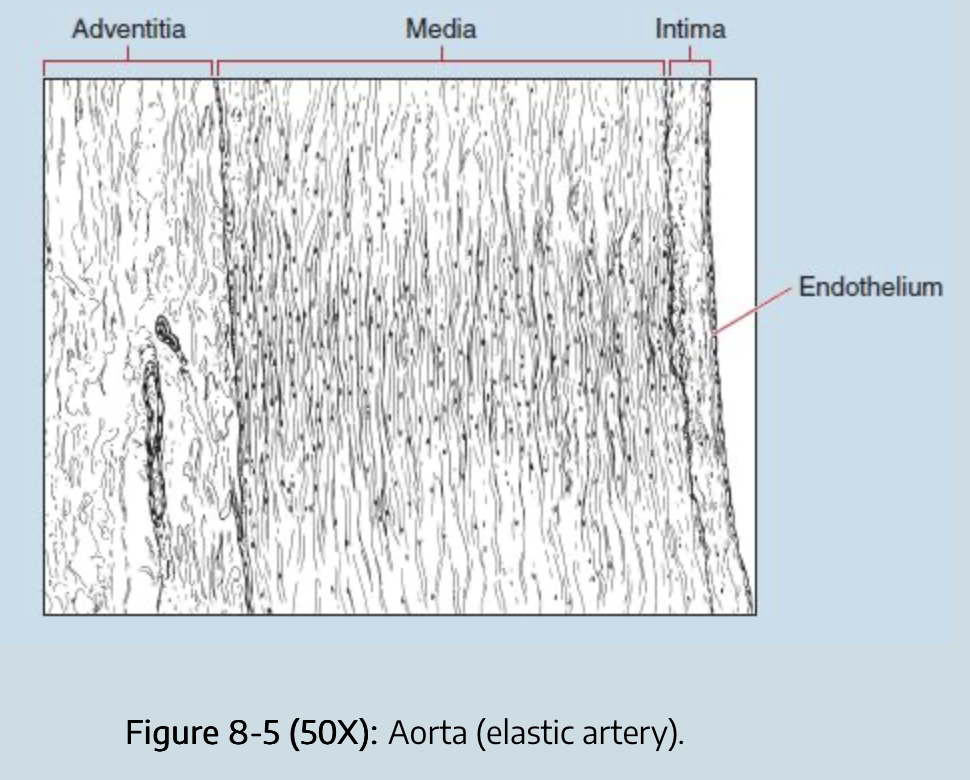
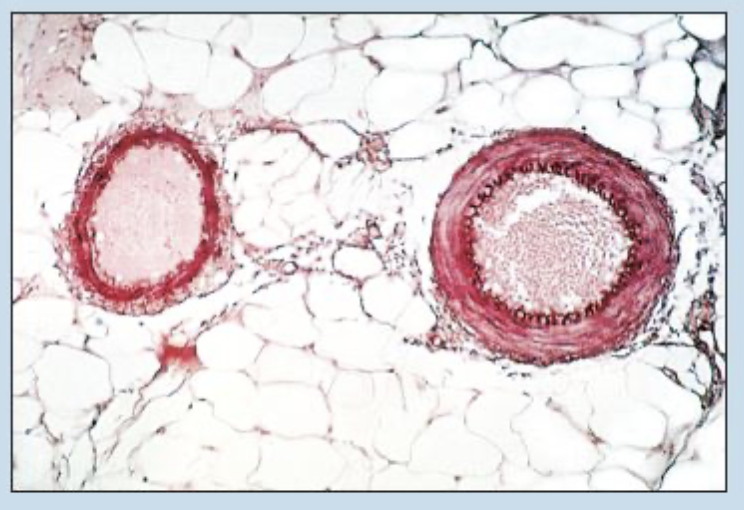
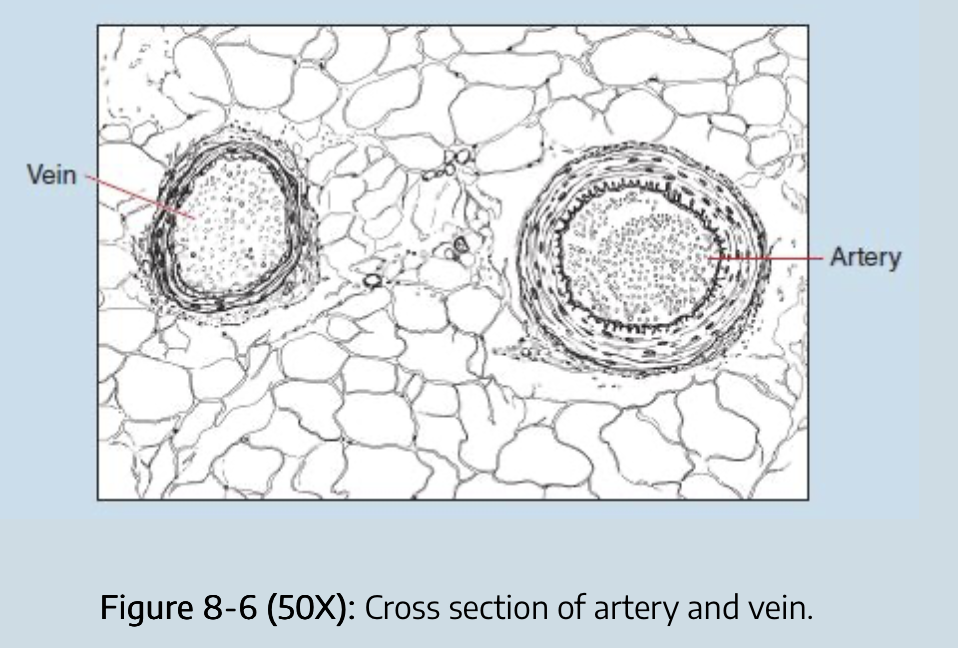
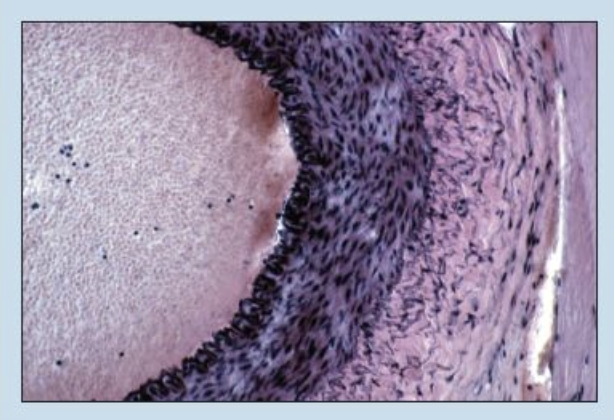
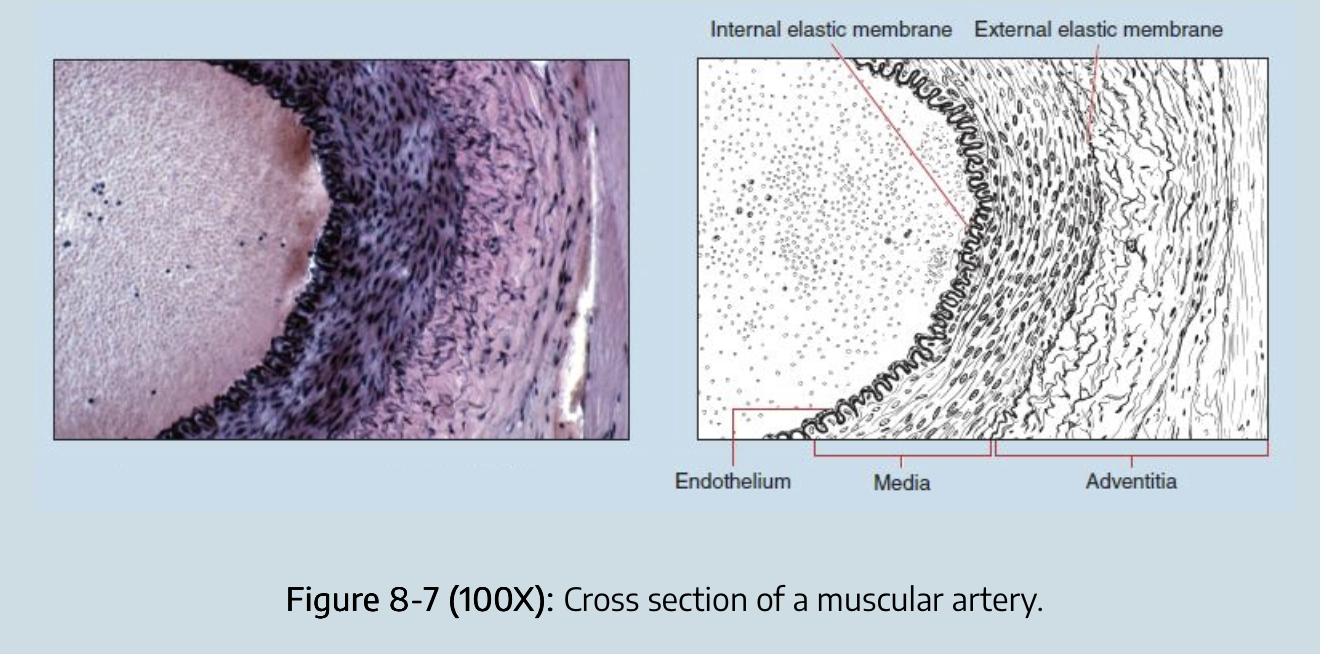
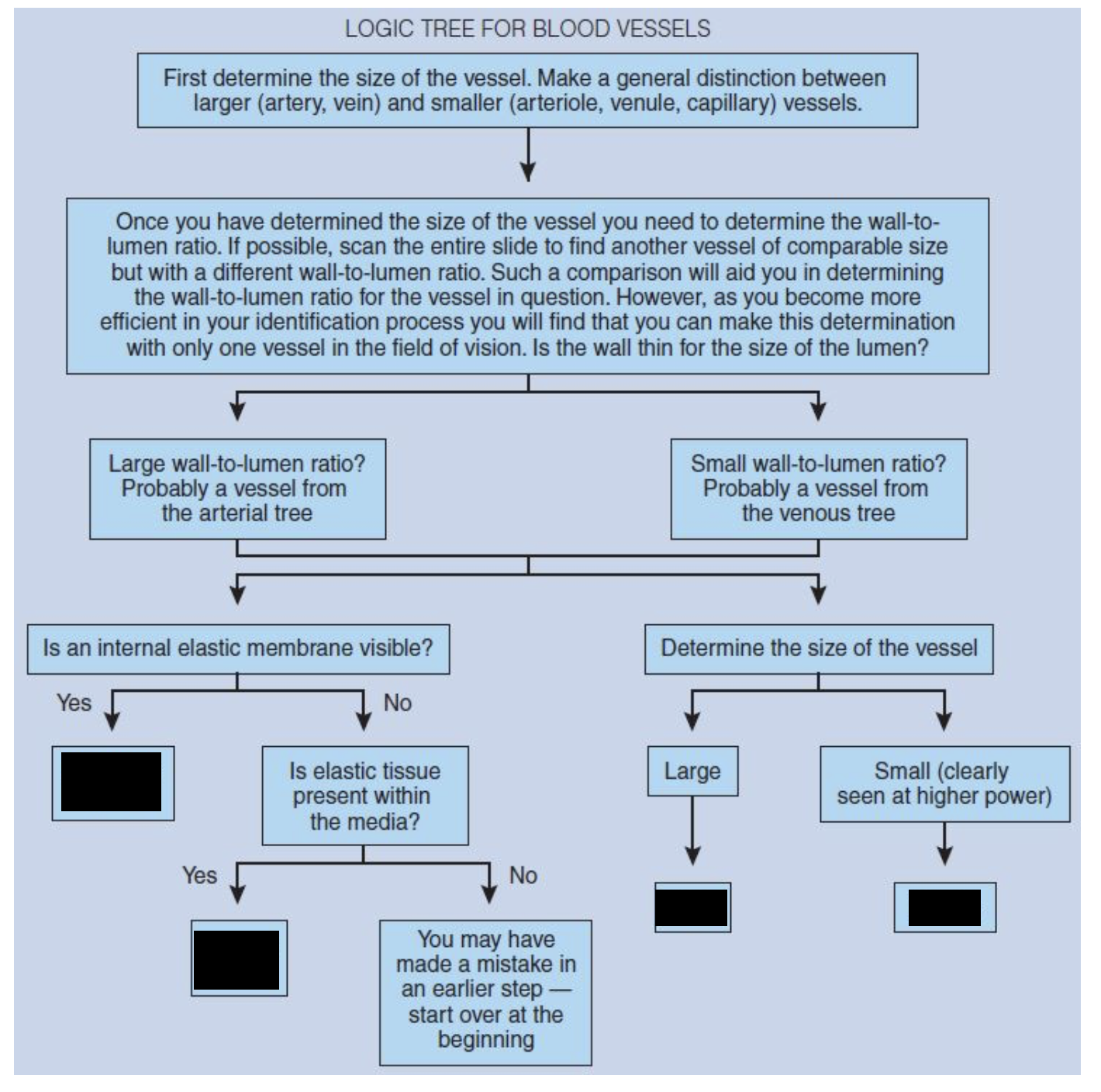
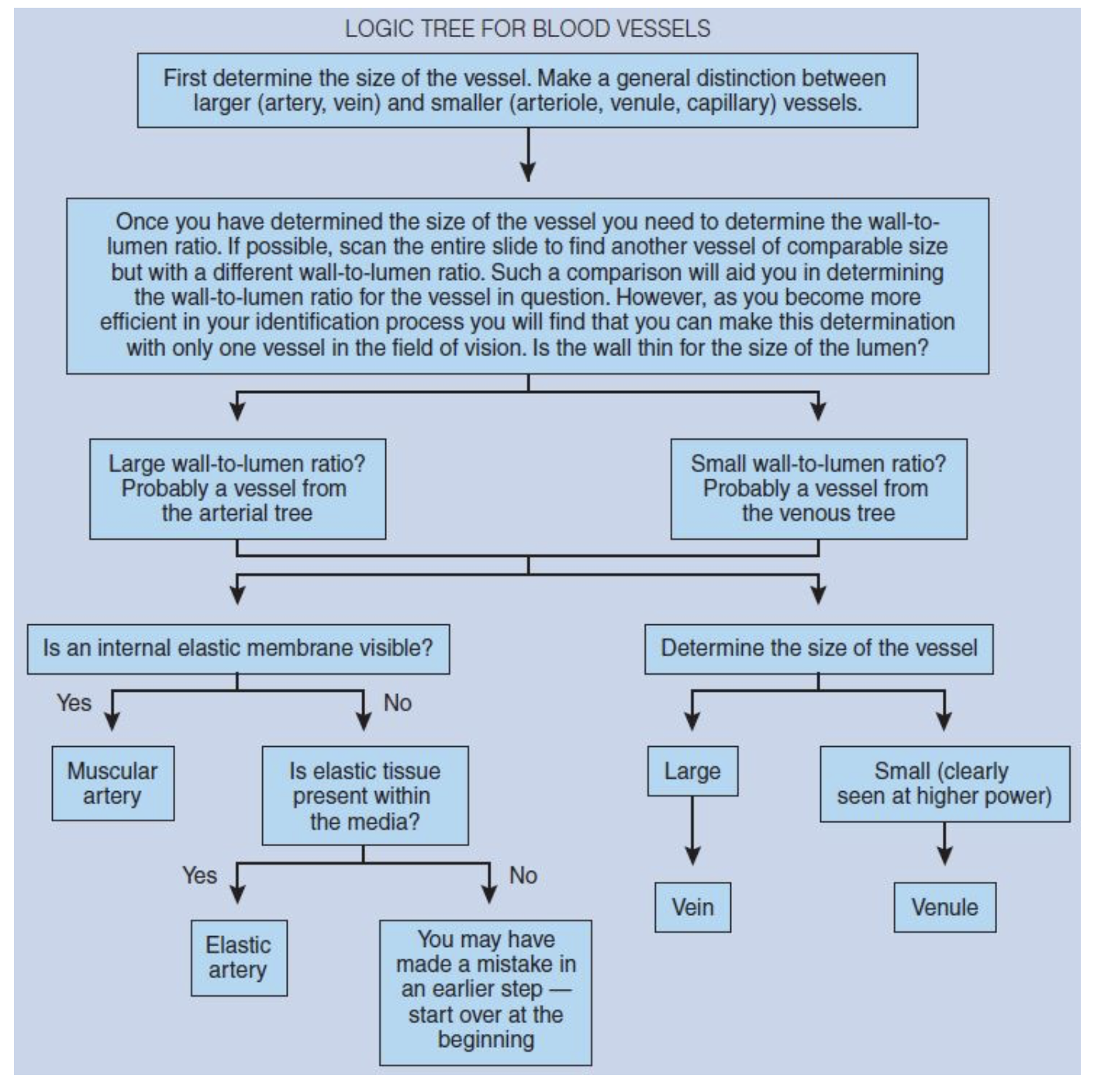
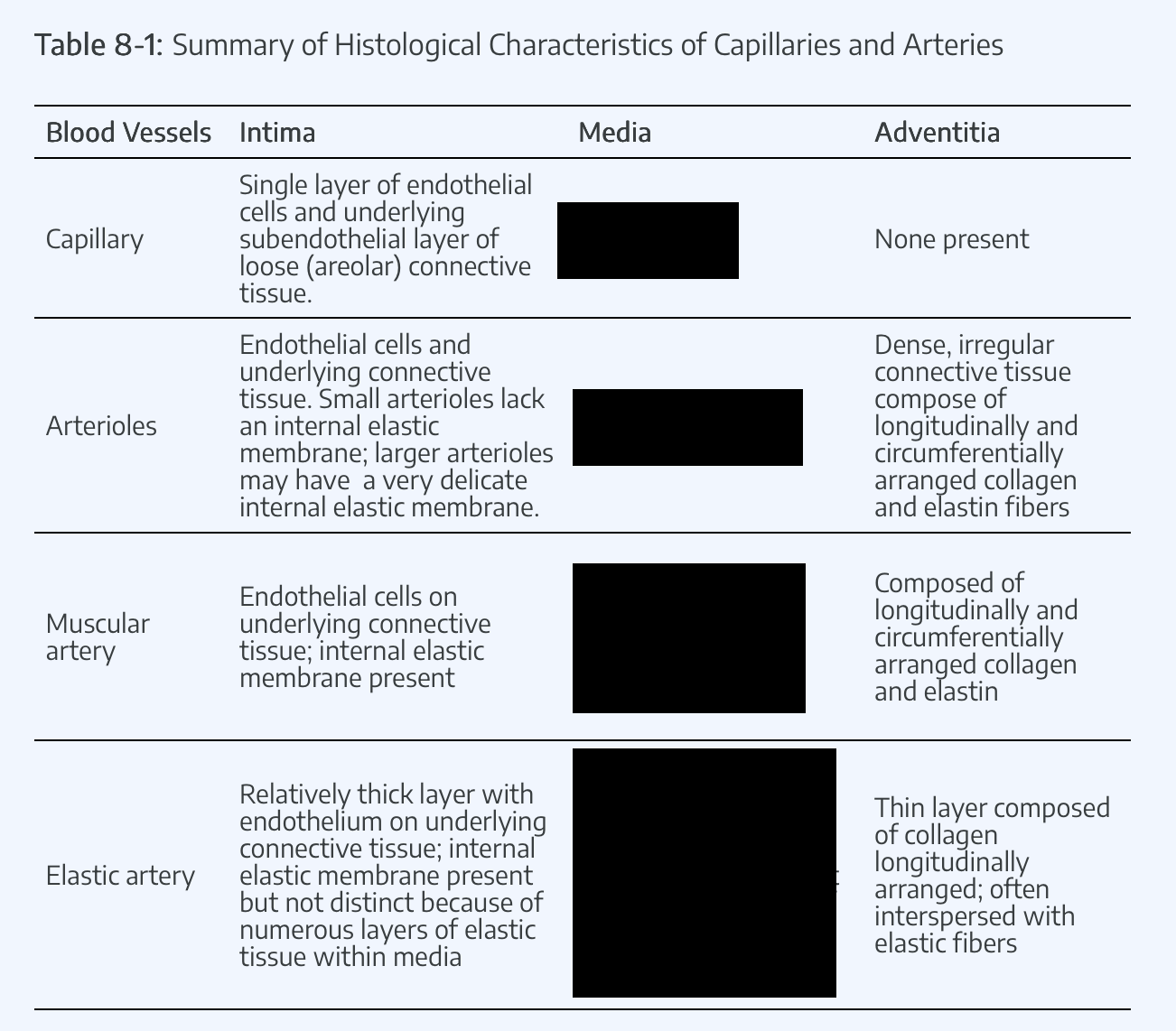
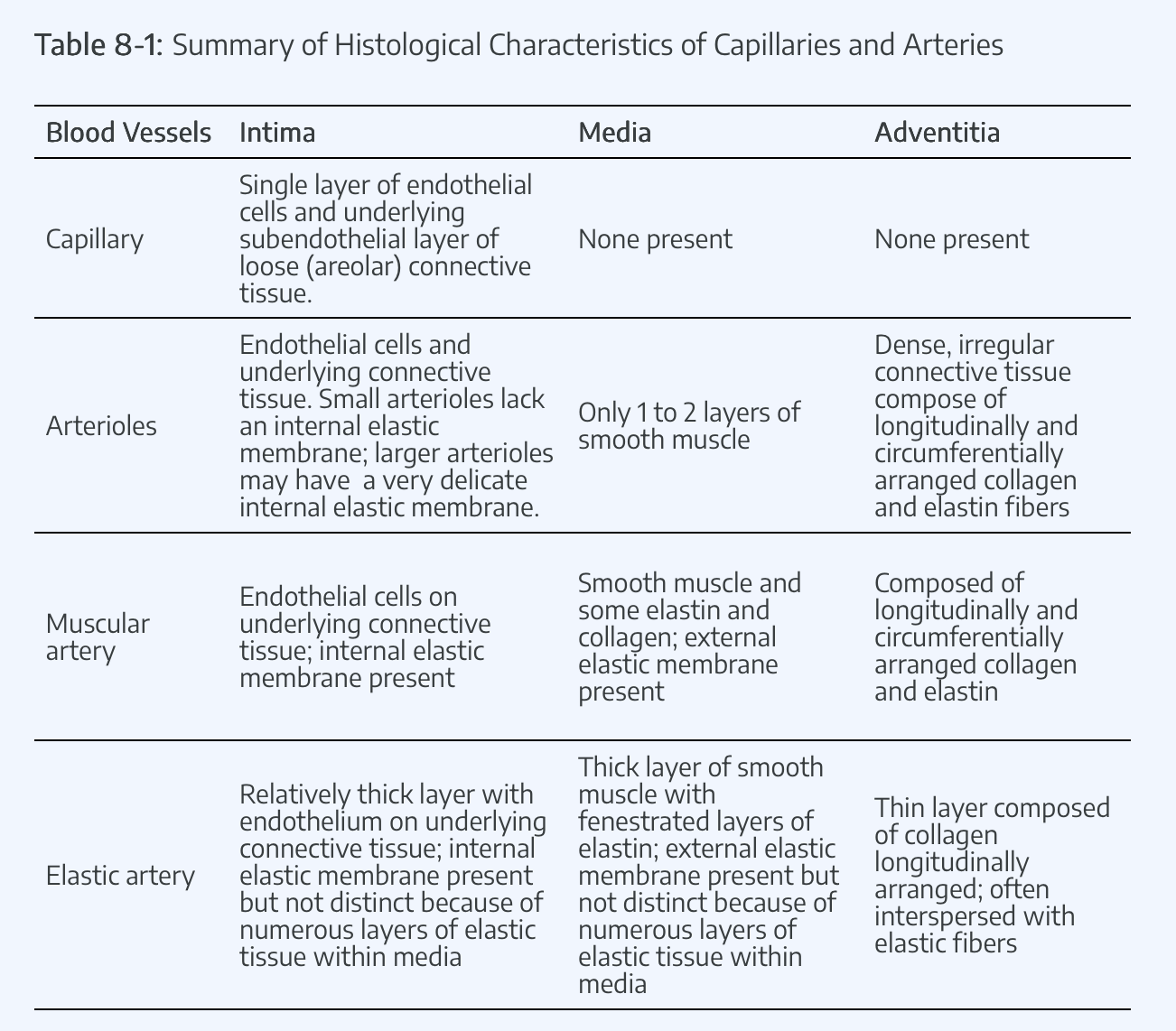
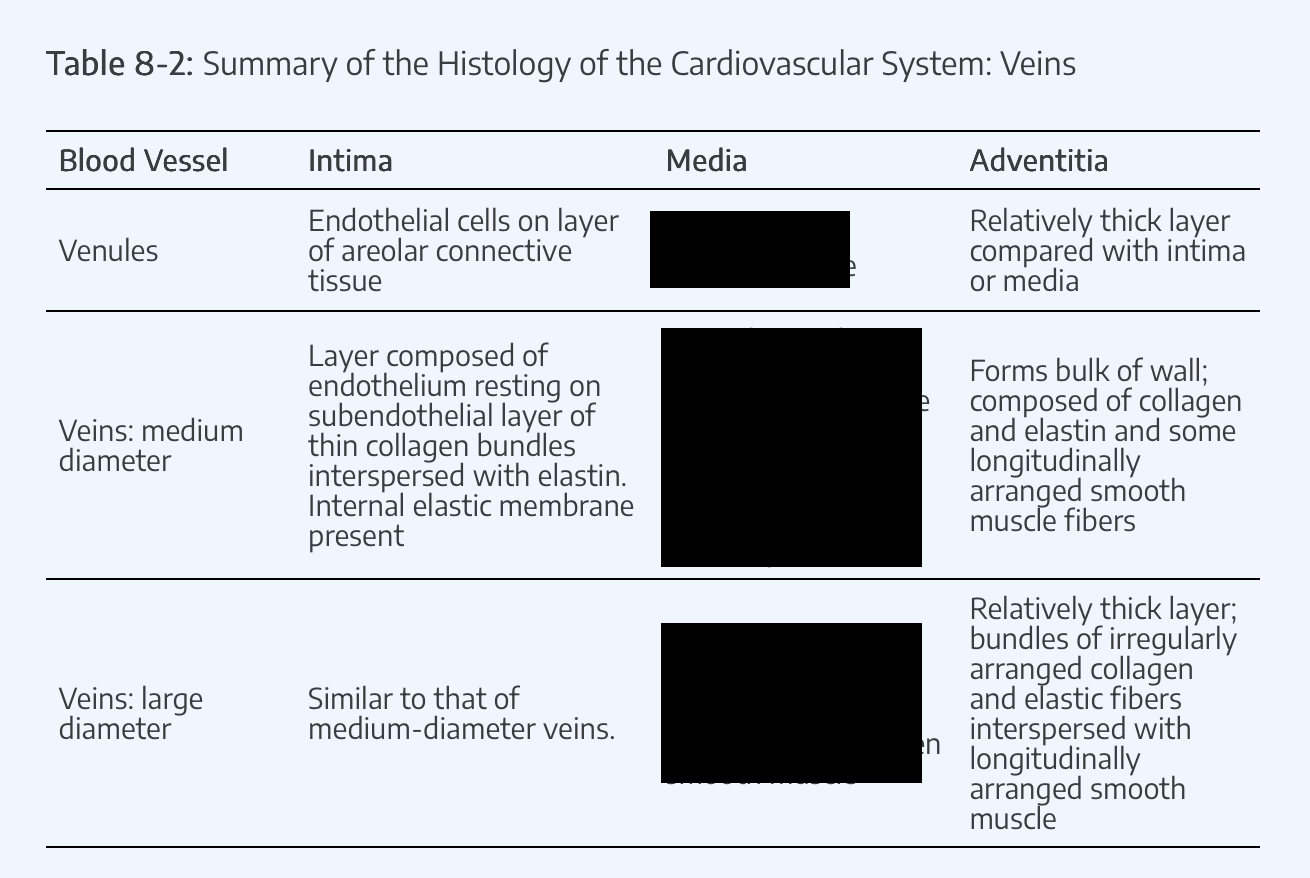
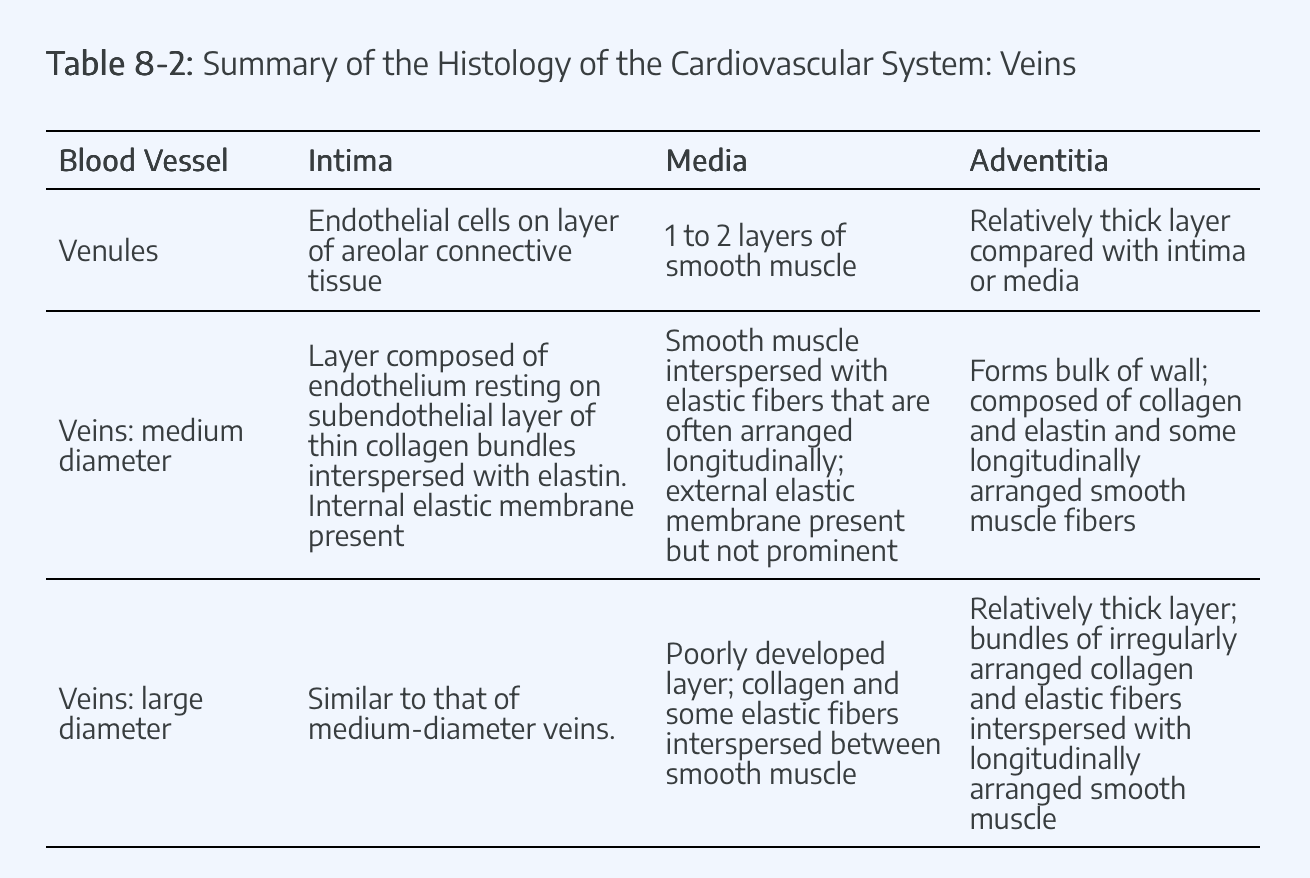
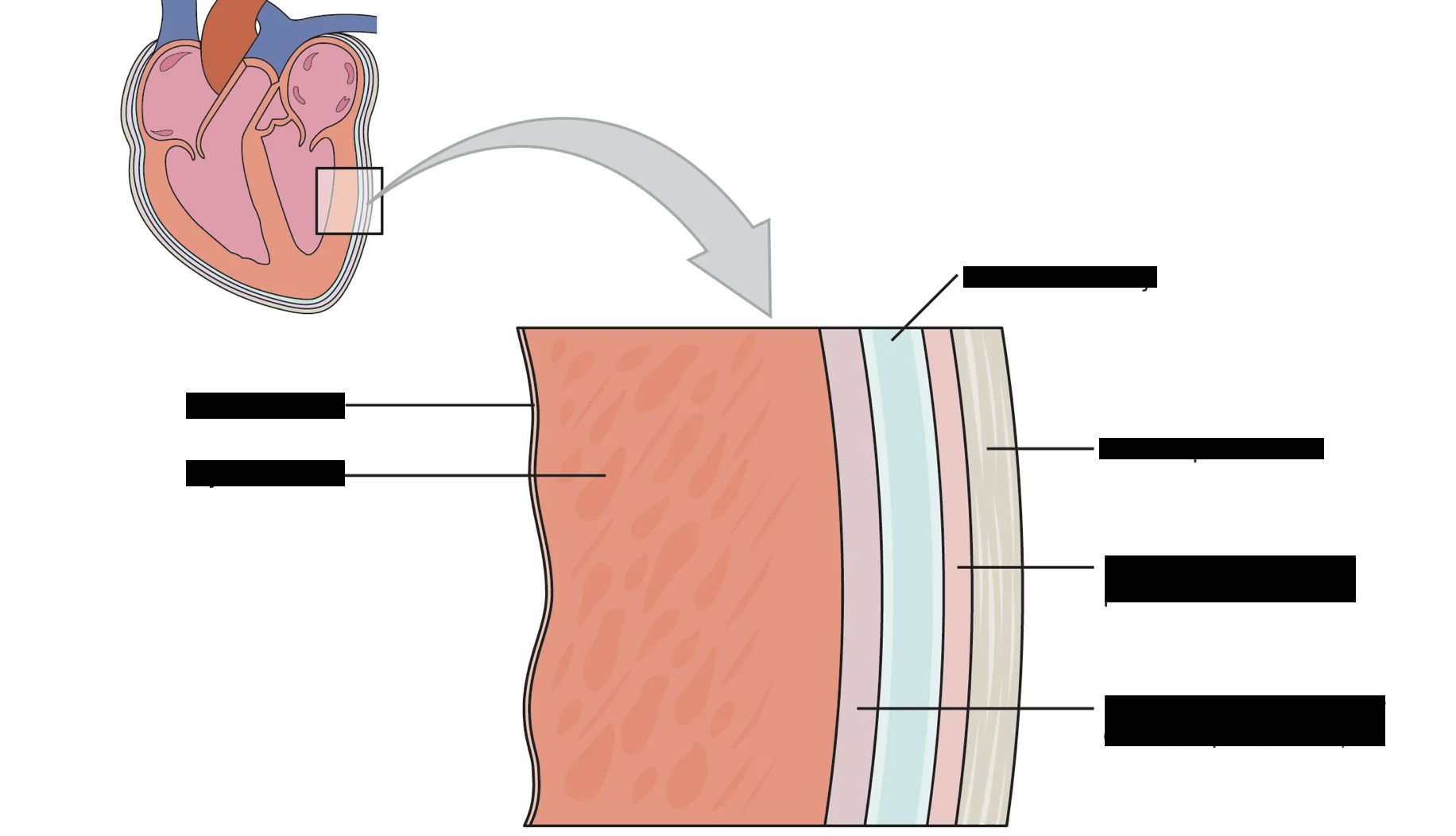
microscopic features of arteries and veins
the wall of the artery is much thicker and more muscular than that of the vein (which may be partially collapsed).
Looking at the inner wall you can distinguish the purple-stained nuclei of endothelial cells (simple squamous epithelium) attached to a layer containing elastic fibers (which appear as a bright, shiny layer).
These two layers together are known as the tunica interna.
The thickest part of the wall is called the tunica media (which consists of elastic fibers, connective tissue and smooth muscle).
The outermost layer is the tunica externa which is mainly fibrous connective tissue that prevents he artery from collapsing.
The veins consist of the same three coats (tunics).
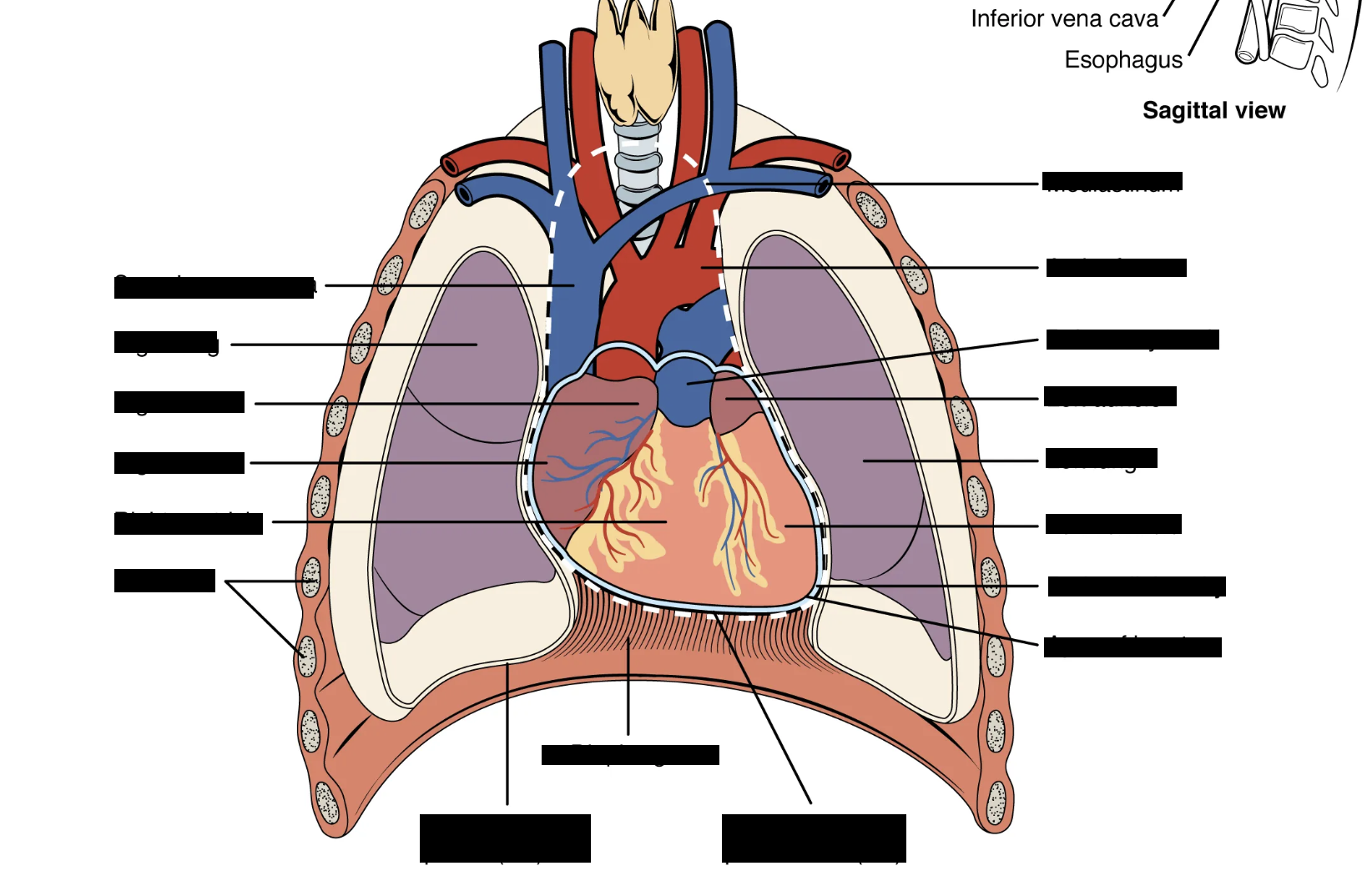
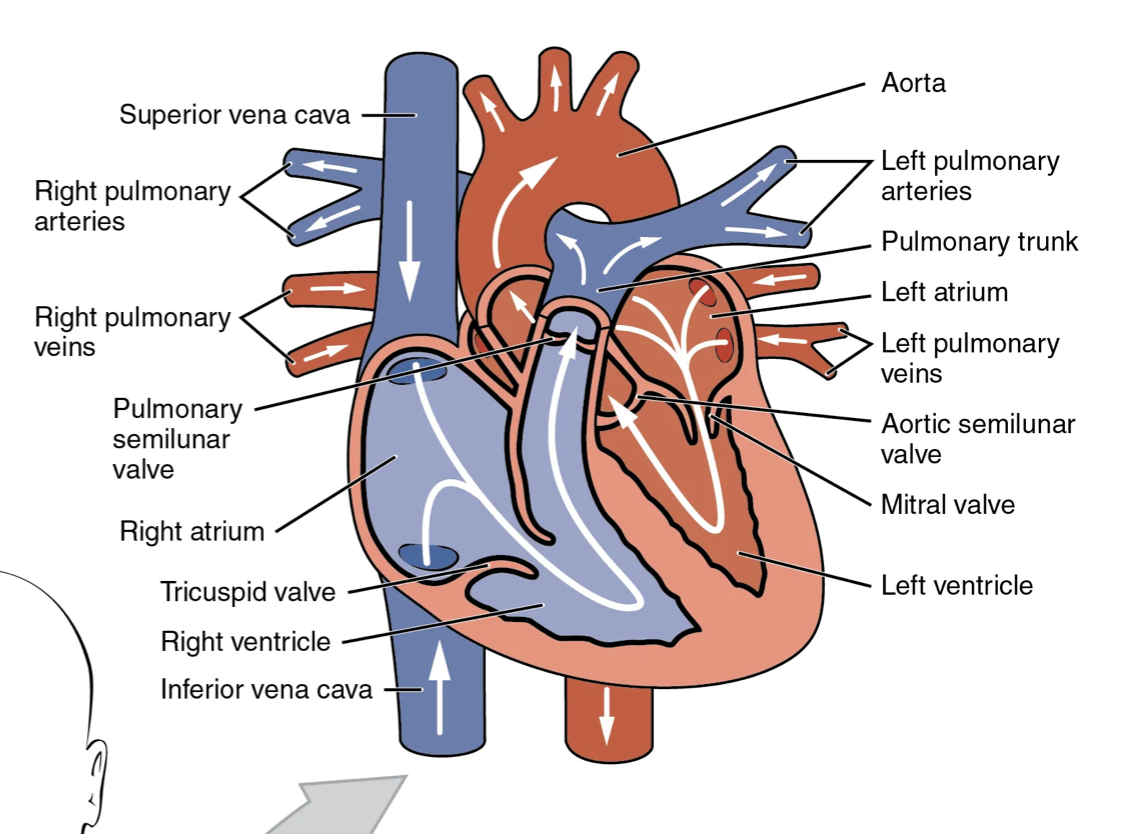
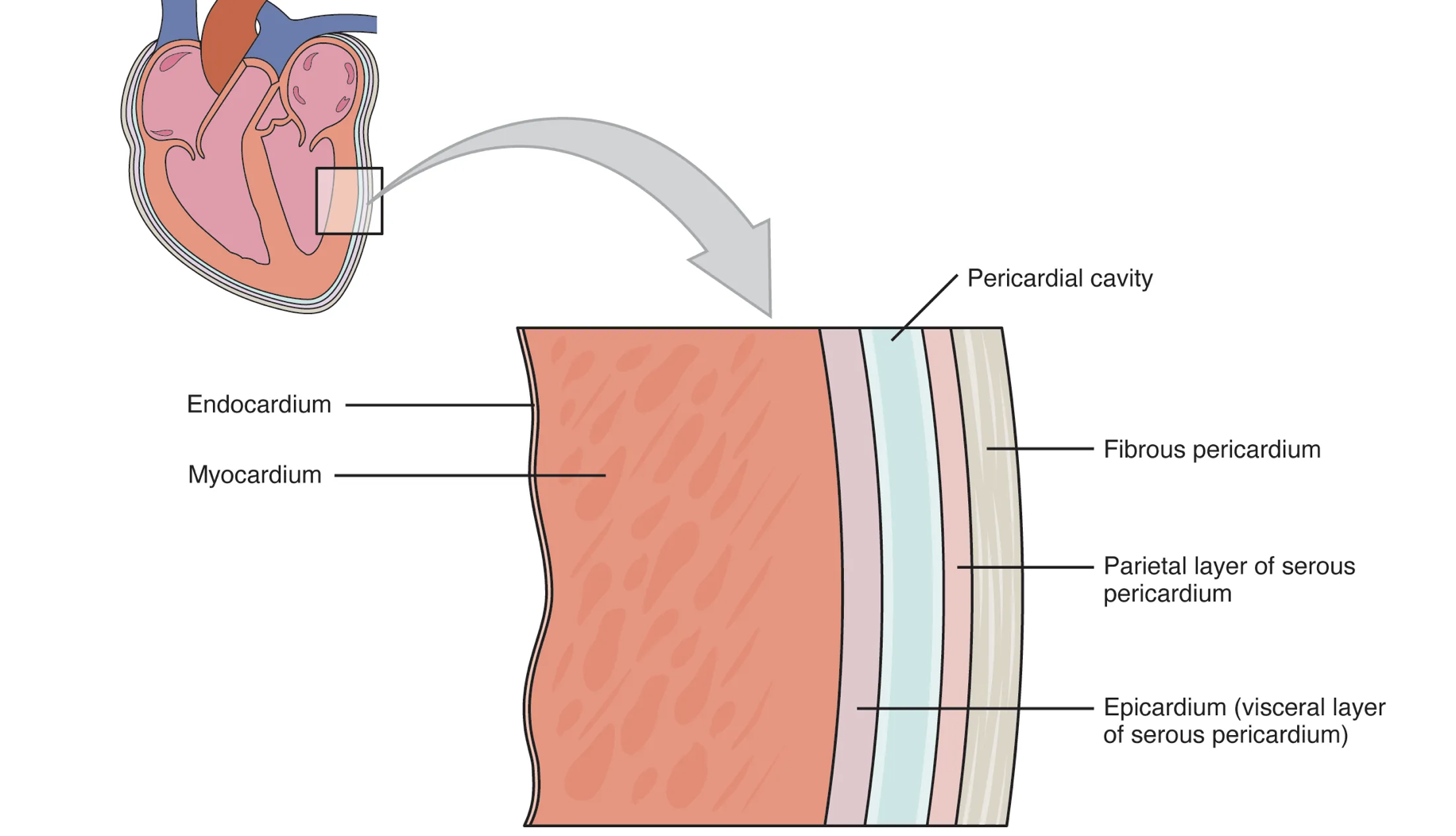
the heart
The heart is a muscular, double pump that is responsible for moving blood throughout the body. It is
located in the area of the thoracic cavity called the mediastinum (between the lungs)
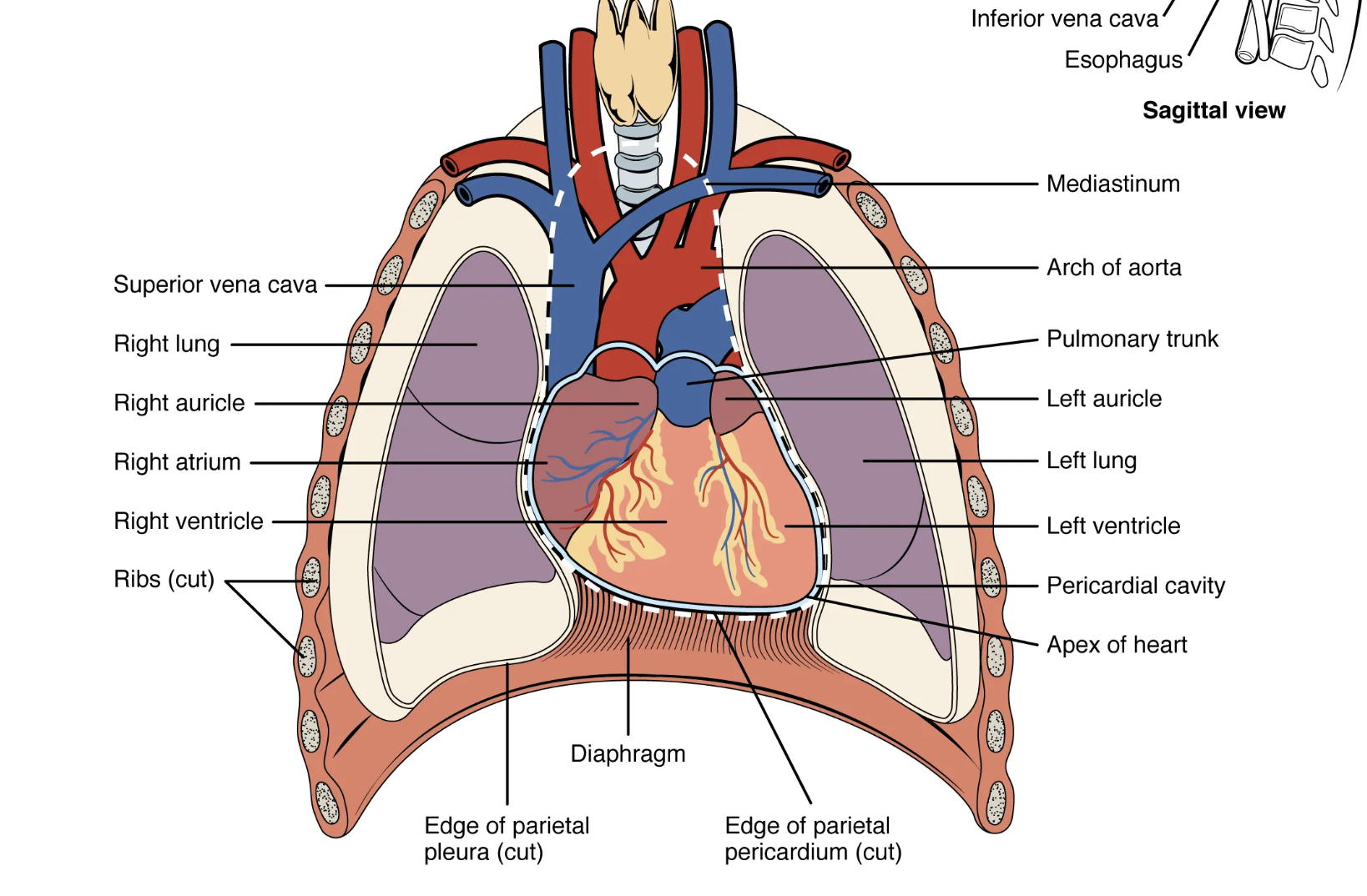
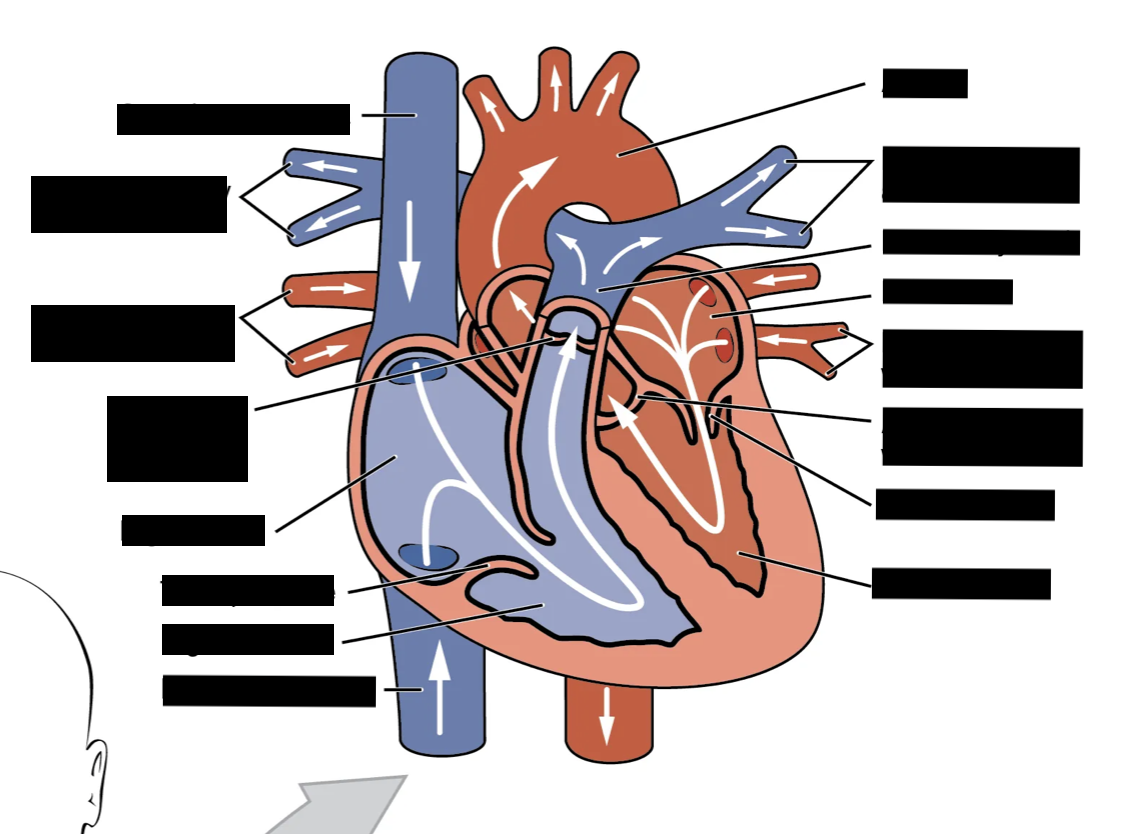
The Cardiac Cycle
consists of all events associated with the flow of blood through the heart during a single heartbeat
1 - Blood returning from circulation enters the right atrium via the inferior and superior vena cavae while blood returning from the lungs (pulmonary circulation) enters the left atrium via the pulmonary veins.
- At this time, the walls of both atria and ventricles are relaxed (atrial and ventricular diastole).
-Blood flows through the atria and directly into the ventricles during diastole.
-his accounts for about 75-80 % of the filling of the ventricles. Atrial contraction (next) accounts for the rest of the filling
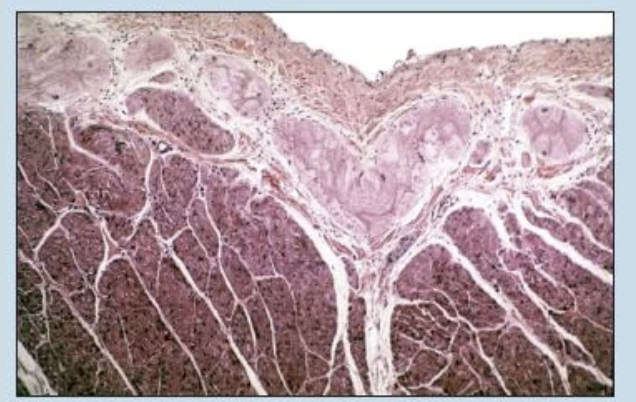
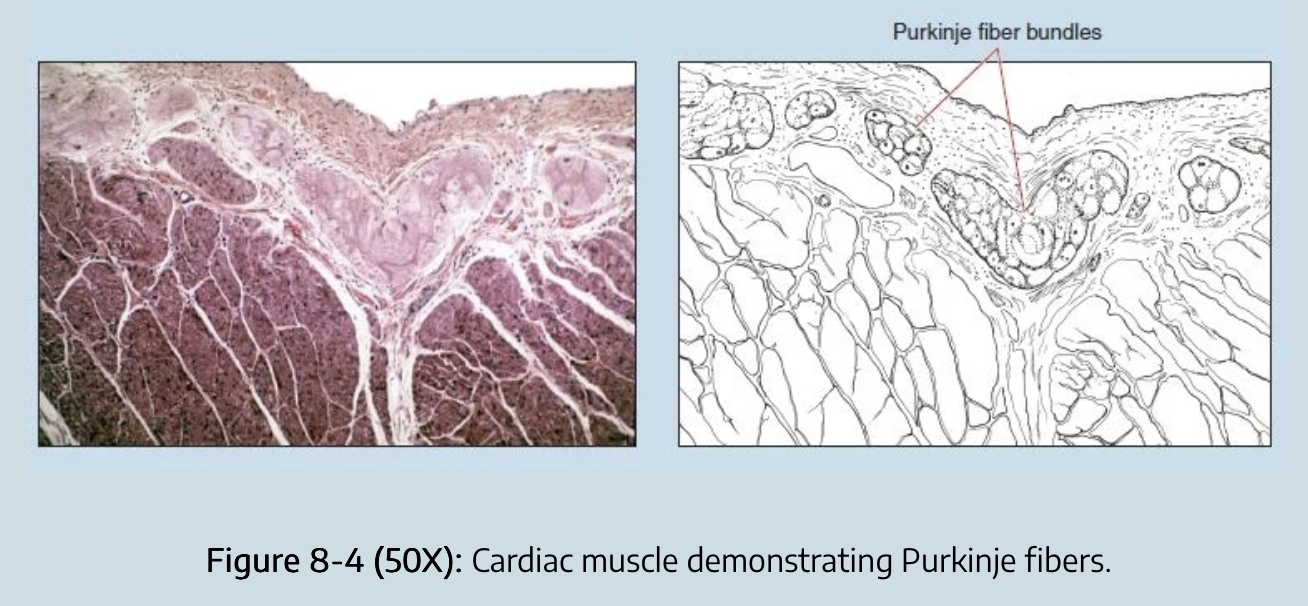
2 - The sinoatrial (SA) node (the pacemaker of the heart) initiates an action potential (depolarization) that propagates throughout the atria, causing the atria to contract.
-The discharge of the SA node signals the end of atrial diastole and the beginning of atrial systole.
3 - The action potential from the SA node stimulates the atrioventricular (AV) node and just as the atria are relaxing (atrial diastole beginning), the spread of excitation from the AV node along the AV bundle, bundle branches, and Purkinje fibers stimulates the ventricles to begin contraction (ventricular systole)
-Rising pressure as the ventricles fill causes the AV valves to close
4 - As ventricular contraction continues, the increasing blood pressure opens the aortic and pulmonary semilunar valves and blood is ejected into the systemic and pulmonary circulations, respectively.
5 - As the ventricles begin to relax again (ventricular diastole), back pressure from the aorta and pulmonary arteries closes the semilunar valves and the whole cardiac cycle begins again.
two methods of monitoring components of the cardiac cycle.
Auscultating the heart using a stethoscope and recording an electrocardiogram
auscultation
stethoscope
Auscultation is used to detect valve abnormalities that produce abnormal heart sounds - heart murmurs.
“Lubb”, occurs when the AV valves are forcefully shut during ventricular systole
“Dupp”, occurs when the semilunar valves close as the pressure in the ventricle drops during diastole.
here is a brief pause before the sounds are repeated. Abnormal sounds are heard when valves close incompletely (incompetence) or scarring prevents valves from opening properly (stenosis)
Heart sounds can also be transduced electronically and displayed in the form of a phonocardiogram
best use of a stethoscope
To hear the heart sound made by:
the aortic semilunar valve, place the stethoscope over the right second intercostal space next to the sternum.
the pulmonary semilunar valve, use the same position on the left side of the chest.
the tricuspid (right AV) valve is heard over the left fifth intercostal space next to the sternum.
the bicuspid (left AV) valve can be heard over the fifth intercostal space
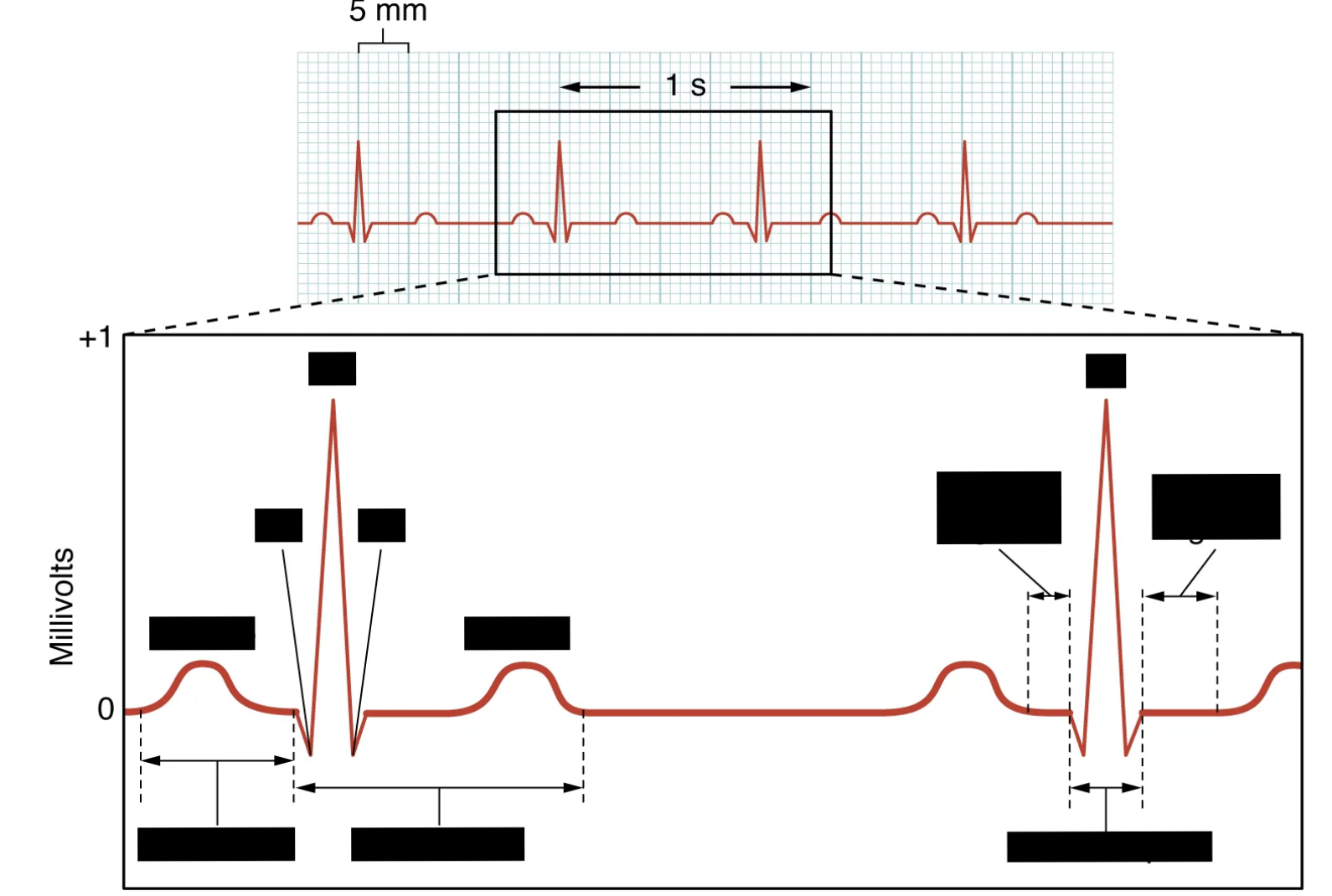
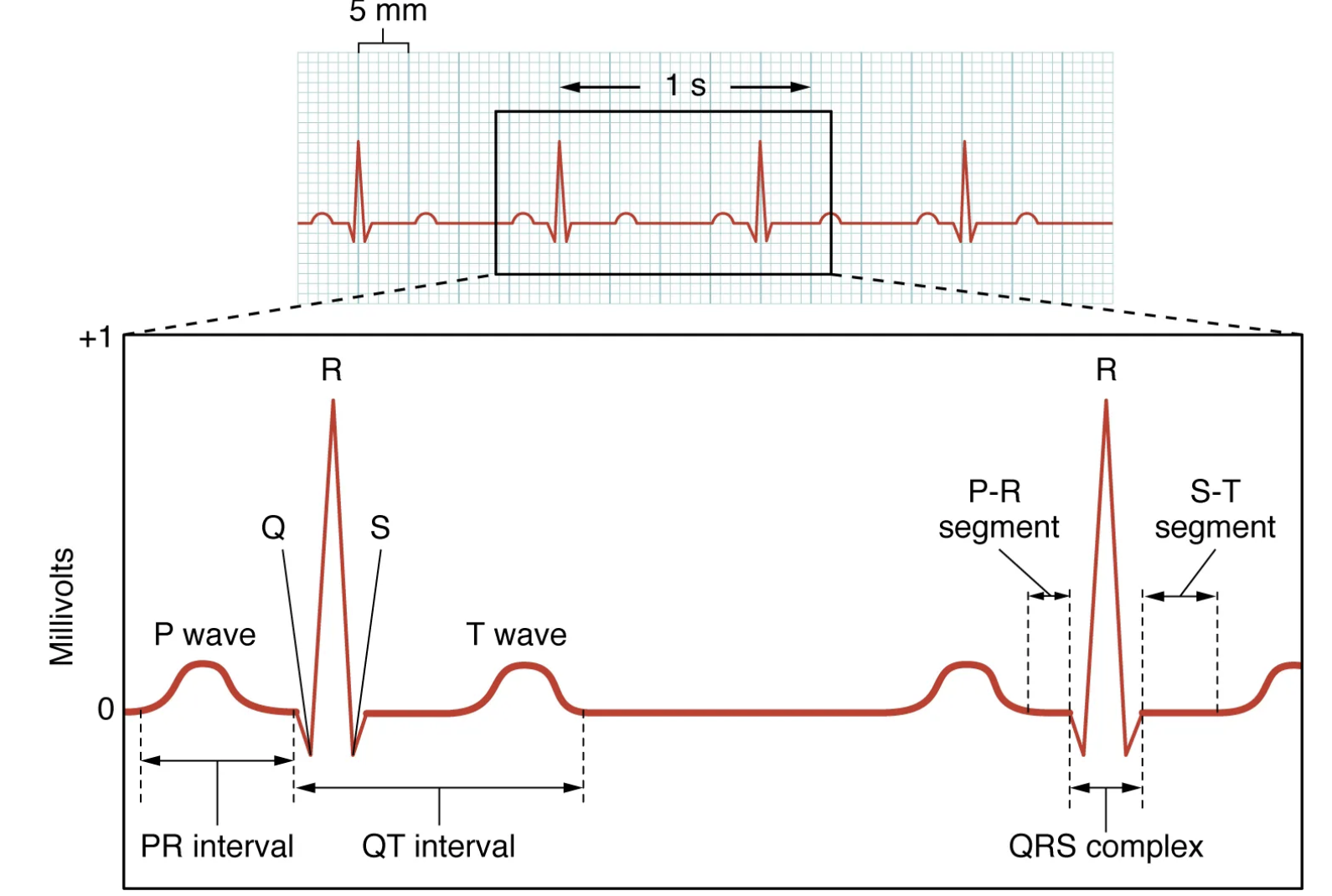
THE ELECTROCARDIOGRAM
The electrocardiogram provides information about heart rate, rhythm, state of the myocardium, the presence or absence of either hypertrophy, ischemia, or necrosis,and abnormalities in conduction or distribution.
The electrocardiogram may also reflect the presence of various drugs or the effects of disturbed electrolytes. Specific abnormalities accompanying pericarditis and malignant diseases of the heart are sometimes detected.
A normal electrocardiogram readout may be obtained in the presence of a variety of chronic heart disorders, but this is not usually the case.
How does a electrocardiogram work?
impulse passes through the heart, electrical currents spread into the tissues surrounding the heart, and a small proportion of these spread all the way to the surface of the body. electrodes are placed on the body on opposite sides of the heart, the potential difference generated across the body can be detected and recorded on a machine called an electrocardiograph - the recoding is called electrocardiogram or ECG/EKG
ECG waves
“P” - shows the voltage changes caused by the depolarization of the atria prior to contraction
QRS “complex” - shows the voltage changes caused by the depolarization of the ventricles prior to contraction
T wave - the repolarization of the ventricles
waves represent the electrical activity in the heart, not the muscular activity. Contraction occurs as a result of the depolarization, thus after the depolarization
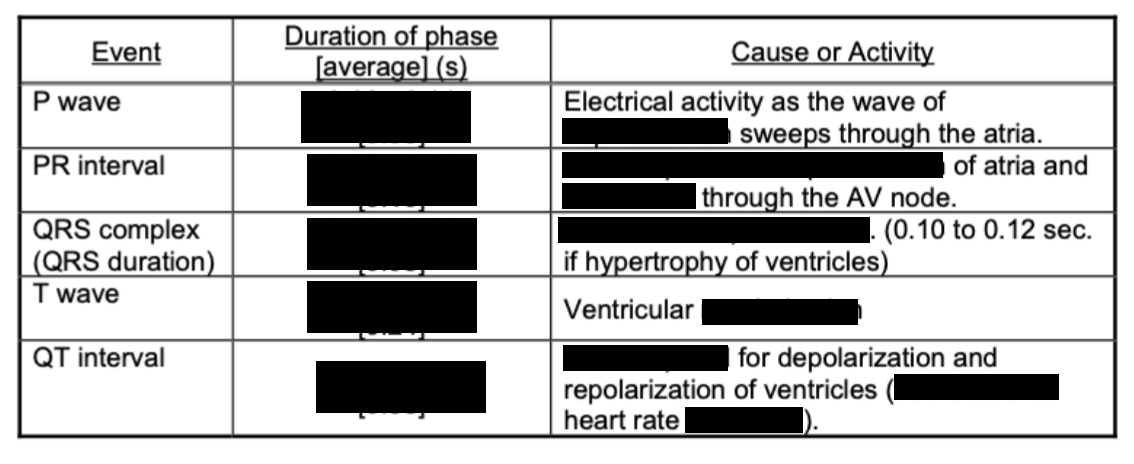
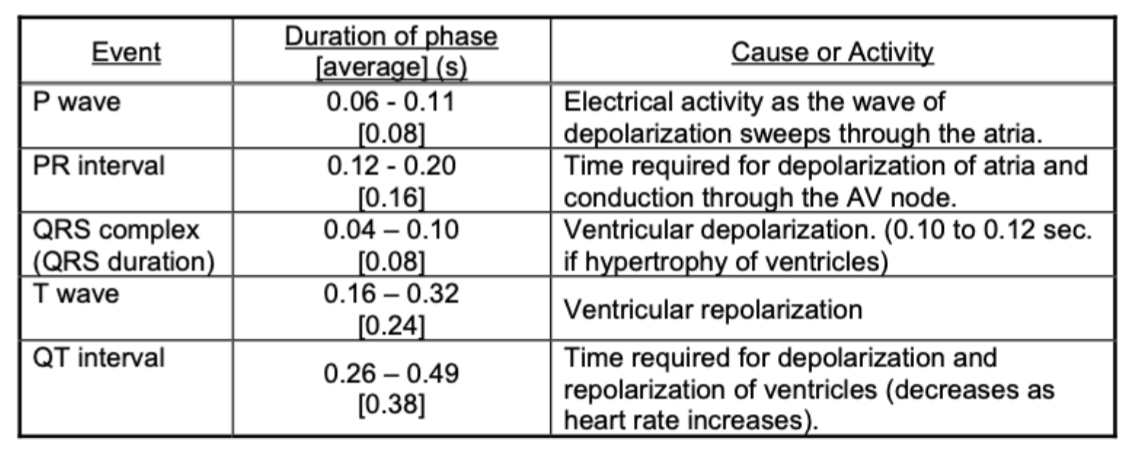
interpretation of ECG strips
Determine the number of P or R waves in a particular number of seconds and correct this number to get beats per minute.
You need to know the speed at which the chart paper was moving to determine heart rate.
A normal resting heart rate for an adult is about 75 beats per minute. The normal maximum exercise heart rate for young adults is about 190 beats per minute.
when the ECG paper is recording at the higher speed, each 1 mm square on the paper is equivalent to 0.04 s.
pulse rate
The alternating expansion and elastic recoil of an artery with each contraction (systole) and relaxing (diastole) of the left ventricle is called pulse. The radial artery at the wrist is the most common place for detecting and measuring pulse rate
averages about 70-80 beats per minute at rest; however, the pulse rate changes with the time of day, temperature, emotions and many other factors. There may also be correlations with age, sex, weight, and physical conditions
blood pressure
gives information regarding the heart’s pumping efficiency as well as the condition of the blood vessels
The systolic pressure, which you will record from the brachial artery (above the elbow), is measured during the contraction (systole) of the ventricles. Diastolic pressure is measured when the heart muscles are relaxed (diastole).
normal resting systolic pressure is 120 mm Hg; the normal diastolic pressure is 70-80 mm Hg
individuals with low blood pressure tend to live longer
Normal and optimal pressures for women are 8-10 mm less than those for men. Pressures increase with activity and systolic pressure may reach 200 mm during vigorous exercise.
Hypertension
(high blood pressure) occurs when the arteries lose their elasticity due to atherosclerosis or other conditions.
A systolic pressure of 140 mm Hg or greater and/or a diastolic pressure of 90 mm Hg or greater indicates hypertension.
An elevated systolic pressure tends to indicate hypertension in older adults (50+) while an elevated diastolic pressure indicates the condition in younger adults.
recording BP
using a sphygmomanometer and a stethoscope (orthe digital sphygmomanometers) recorded as systolic/diastolic (e.g., 120/80). The difference between the two is referred to as pulse pressure. An increase in the pulse pressure is always an indication of increased inelasticity of arteries due to conditions such as atherosclerosis.
Korotkoff sounds
The disappearance of sounds, referred to as Korotkoff sounds, in an artery occluded by a blood pressure cuff. The timing of these sounds is correlated with pressure readings on the sphygmomanometer gauge
how does a BP monitor work?
the pressure in the cuff is first elevated approximately 30 mm above arterial systolic pressure, to completely occlude (block) the artery. then the cuff pressure is gradually reduced
As long as this pressure is higher than systolic pressure, the brachial artery remains collapsed and no blood flows into the lower artery during any part of the pressure cycle, no Korotkoff sounds are heard in the lower artery
when the pressure falls below the systolic pressure, blood spurts through the artery beneath the cuff, during peak of systolic pressure.
you begin to hear faint tapping sounds in the artery, in synchrony with the heartbeat. As soon as these sounds are heard, the level is approximately equal to the systolic pressure and the pressure indicated on the dial should be recorded
as the pressure of the cuff is reduced, Korotkoof sounds get louder then fade away.