Lecture Three Attachment, Trauma, and PTSD Student Version
1/59
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
60 Terms
Attachment
A deep and enduring emotional bond connecting one person to another.
Originates in infancy (or earlier) between a caregiver and child.
Shapes an individual's ability to form emotional connections throughout life
Roots of Attachment Theory
Developed by John Bowlby in the 1950s and 1960s.
Influenced by psychoanalytic theory and ethology.
Mary Ainsworth's "Strange Situation" experiment expanded and operationalized Bowlby’s concepts.
Four Primary Attachment Styles
Secure Attachment
Avoidant (Dismissive) Attachment
Ambivalent/Anxious/Preoccupied Attachment
Disorganized/Disoriented Attachment
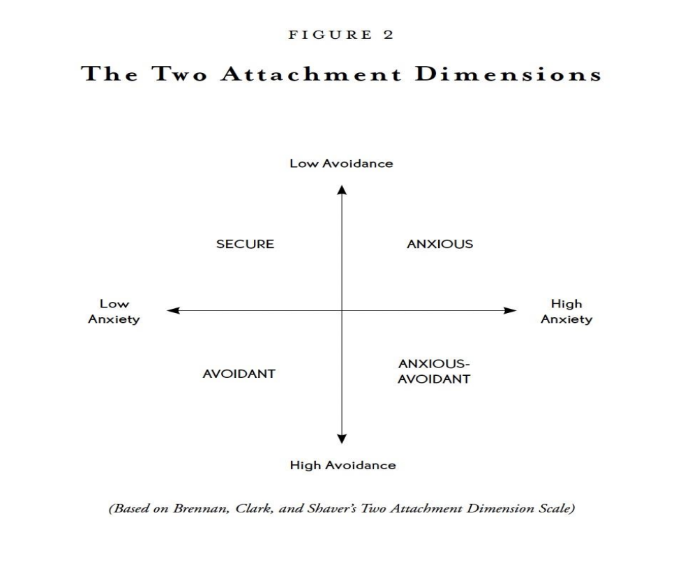
Characteristics of Secure Attachment
Comfortable with intimacy and independence.
Typically, positive view of themselves and others.
Reliable ability to engage with and seek support from caregivers.
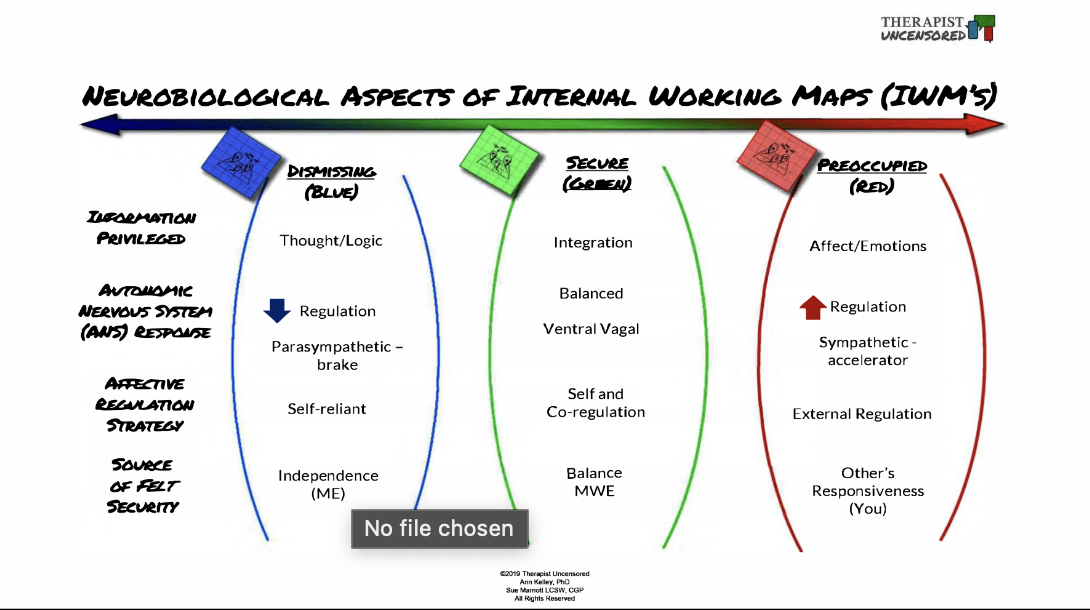
Avoidant (Dismissive)
Values independence, avoids closeness.
Ambivalent or Preoccupied (anxious)
Seeks closeness and is anxious about abandonment
Disorganized
No clear strategy, a mix of avoidant and anxious behaviors
Implications of Attachment in Adulthood
Early attachment has an influence on all adult relationships (romantic esp.)
Impacts one's ability to form and maintain friendships.
Shapes emotional regulation, resilience, and coping mechanisms.
Trauma - Gabor Mate
The wound that you sustained as a result. Trauma is not what happens to you. Trauma is what happens inside you as a result of what happens to you
Trauma
Emotional, psychological, and sometimes physical responses to distressing events that overwhelm coping abilities.
Types of Trauma
Big T and small t
Big T
Significant events (e.g., war, natural disasters, severe abuse, life-threatening incidents).
Small t
Everyday distressing events (e.g., interpersonal conflicts, minor accidents, feelings of invalidation)
Impact of Trauma
Both types can affect mental health, behavior, and overall life experience.
Adverse Childhood Experiences (ACE) Scale
a tool developed to quantify the cumulative effects of different types of childhood traumas. The scale assesses exposure to ten types of adversity in childhood, ranging from emotional, physical, and sexual abuse to various forms of household dysfunction.
The 10 types of adversity in childhood
ACE is defined as experiencing any of the following categories of abuse, neglect, or loss prior to age 18:
Physical abuse by a parent
Emotional abuse by a parent
Sexual abuse by anyone
Growing up with an alcohol and/or substance abuser in the household
Experiencing the incarceration of a household member
Living with a family member experiencing mental illness
Domestic violence
Loss of a parent
Emotional neglect
Physical neglect
Background of ACE
The ACE study originated in a collaboration between the Centers for Disease Control and Prevention (CDC) and Kaiser Permanente's Health Appraisal Clinic in San Diego.
3 Main ACE categories
Abuse: emotional, physical, and sexual
Neglect: Emotional and Physical.
Household Dysfunction: This encompasses challenges such as having household members who were incarcerated, mentally ill, substance abusers, or if the respondent witnessed domestic violence, or lost a parent due to separation, divorce, or other
ACE Scoring
Each type of adversity encountered scores one point.
ACE scores range from 0 to 10; higher scores indicate greater exposure to childhood adversities.
ACE Health Outcomes
Numerous studies show a graded dose-response relationship between ACEs and negative health outcomes in adulthood.
As the number of ACEs increases, the risk for health problems also increases, including:
Heart disease
Diabetes
Substance misuse
Mental health conditions
Broader Implications of ACE
The ACE score aids medical professionals, therapists, and other practitioners in understanding the health and social impacts of adverse childhood experiences.
This insight highlights the importance of early intervention and prevention efforts to address the root causes of many health and social issues.
In children under the age of 6, trauma may manifest as…
Regression, language disruption, reenactment, separation anxietyc
Regression
Returning to behaviours like bed-wetting after learning to use the toilet.
Language Disruption
Forgetting how or being temporarily unable to talk due to stress.
Reenactment
Acting out the traumatic event during playtime as a way to process the experience.
Separation Anxiety
Becoming unusually clingy with a parent or caregiver, reflecting a need for security
In teenagers, trauma may manifest as…
Withdrawal, risk-taking behaviours, mood swings, difficulty concentrating, somatic complaints (key considerations: cognitive development & need for autonomy)
The influence of traumatic experiences
Early traumatic events can disrupt the development of secure attachment.
Abuse, neglect, or loss can lead to anxious, dismissive, or disorganized attachment styles.
The absence of a consistent, responsive caregiver post-trauma exacerbates insecure patterns.
neurological implications of trauma
Chronic stress and trauma can impact the amygdala, hippocampus, and prefrontal cortex.
Heightened stress response and difficulties in emotional regulation.
The brain becomes wired for survival rather than connection.
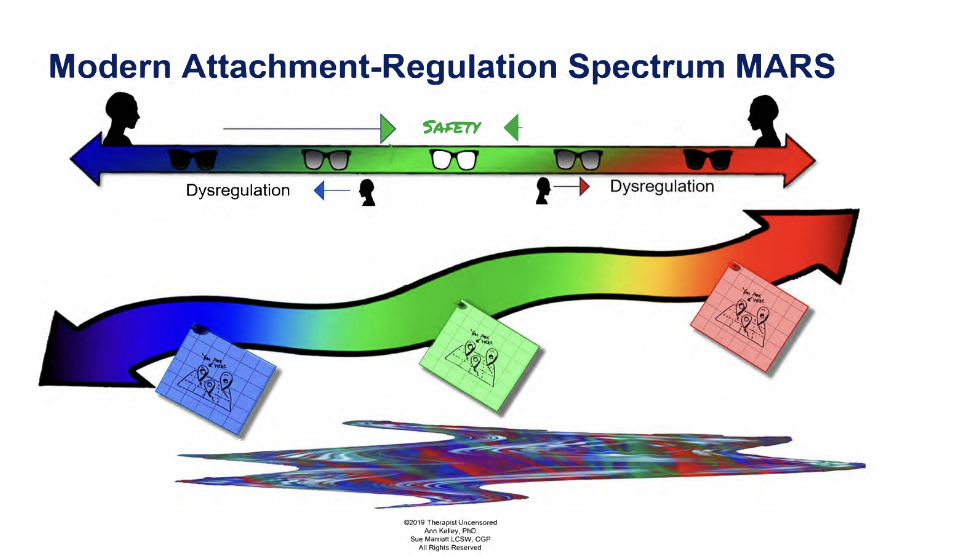
Trauma attachment and regulation
The "window of tolerance" refers to the optimal zone of arousal where an individual can function effectively (Dr. Dan Siegel)
Trauma and insecure attachments can narrow this window.
Leads to hyperarousal (fight/flight) or hypoarousal (freeze/dissociate) outside this window.
The Power of Secure Attachments in Trauma Recovery
Secure Base: Provides safety and fosters resilience.
Therapeutic Relationships: Can "rewire" attachment patterns and offer corrective emotional experiences.
Social Support: Community, friendships, and mentorships play a crucial role in recovery.
Post-Traumatic Stress Disorder (PTSD)
Can develop after experiencing a shocking, scary, or dangerous event
Normal Fear Response
Fear is part of the body's natural "fight-or-flight" response, helping us avoid or respond to danger.
Natural Reactions
It is common to feel afraid during and after frightening situations, and most people recover from their symptoms over time.
PTSD Diagnosis
Those who continue to experience symptoms beyond the normal recovery period may be diagnosed with PTSD.
Common Groups - who develop PTSD
Combat veterans
Individuals who have experienced or witnessed:
Physical or sexual assault
Abuse
Accidents
Disasters
Terror attacks
Other serious events
Secondary Trauma
Not everyone with PTSD has directly experienced a dangerous event; learning about trauma affecting a relative or close friend can also lead to PTSD.
About ___ in every 100 people will experience PTSD in their lifetime
10
_____ and ______ are more likely to develop PTSD
Women and BIPOC
Specific aspects of a traumatic event as well as some _____ and social factors (i.e., attachment history, genetic history) make some people more likely to develop PTSD.
biological
What are the Symptoms of PTSD?
Onset: Usually begin within 3 months of the traumatic event but may emerge later.
Duration: Symptoms must last more than 1 month and interfere with daily life (relationships, work).
Cause: Symptoms should not be caused by medication, substance use, or illness.
Recovery: Some recover within 6 months; others may have symptoms for a year or longer.
Symptoms of PTSD and Co-occurring Conditions
Co-occurring Conditions: PTSD often occurs with depression, substance use, or anxiety disorders.
Detachment: After trauma, it's common to feel detached, as though observing the event.
Diagnosis: A psychiatrist, psychologist, or clinical social worker can assess if symptoms meet PTSD criteria.
Criteria for PTSD Diagnosis
Symptoms must last at least 1 month and include:
At least 1 re-experiencing symptom
At least 1 avoidance symptom
At least 2 arousal and reactivity symptoms
At least 2 cognition and mood symptoms
Re-experiencing Symptoms (PTSD)
Flashbacks: Reliving the traumatic event (physical symptoms like a racing heart or sweating).
Reoccurring Memories or Dreams: Related to the event.
Distressing Thoughts: Triggered by reminders.
Physical Stress Signs: When recalling the trauma.
Triggers: Words, objects, or situations can cause these symptoms.
Avoidance Symptoms (PTSD)
Avoiding: Places, events, or objects that remind of the trauma.
Avoiding Thoughts/Feelings: Related to the event.
Changes in Routine: For example, avoiding driving after a car accident.
Arousal and Reactivity Symptoms (PTSD)
Startled Easily: Feeling tense, on edge, or on guard.
Difficulty: Concentrating, falling asleep, or staying asleep.
Irritability: Angry or aggressive outbursts.
Risky Behavior: Engaging in reckless or destructive activities.
Interference: With daily life (sleep, eating, concentration).
Cognition and Mood Symptoms (PTSD)
Memory Issues: Trouble recalling key aspects of the event.
Negative Thoughts: About oneself or the world.
Blame: Distorted thoughts leading to self-blame.
Ongoing Negative Emotions: Fear, anger, guilt, shame.
Loss of Interest: In previous activities.
Social Isolation: Feeling detached from friends or family.
Difficulty Feeling Positive Emotions: Such as happiness or satisfaction.
Not Everyone Develops PTSD
Many factors influence this, some before, during, and after the trauma.
Risk Factors for developing PTSD
Exposure to "little t" or "big T" traumas.
Developmental Trauma: Childhood trauma.
Intense Emotions: Feeling horror, helplessness, or extreme fear.
Lack of Social Support: After the event.
Additional Stress: Loss of a loved one, injury, job, or home.
History of Mental Illness or Substance Use: Personal or family history (epigenetics).
Resilience Factors
May reduce the likelihood of developing PTSD:
Social Support: Seeking help from friends, family, or support groups.
Self-Acceptance: Feeling okay with your response to the trauma.
Coping Strategies: For dealing with and learning from the event.
Preparedness: Responding to upsetting events, despite feeling fear.
Key Treatments for PTSD
Psychotherapy: Talk therapy addressing emotions, thoughts, and behaviors.
Somatic Therapy: Body-based therapy focusing on trauma held in the body.
Medication: Often antidepressants, especially SSRIs.
Personalized Care
An experienced mental health professional tailors treatment to symptoms and needs.
Complex Cases
Those living with ongoing trauma (e.g., abusive relationships) need treatment that addresses both the situation and PTSD symptoms.
Co-occurring Conditions:
PTSD often overlaps with panic disorder, depression, substance use, or suicidal thoughts, which also need treatment.
Psychotherapy for PTSD
Goal: Identify and change troubling emotions, thoughts, and behaviors.
Types: Individual or group sessions, lasting 12-24 weeks or more.
Focus: Some therapies target PTSD symptoms directly; others address social, family, or job issues.
Effective Therapies for PTSD
EFT: Emotion-Focused Therapy.
DBT: Dialectical Behavior Therapy.
EMDR: Eye Movement Desensitization and Reprocessing.
CPT: Cognitive Processing Therapy.
Psychedelic-Assisted Therapy: Emerging treatment option.
Somatic Therapy for PTSD
Body-Focused Approach: Based on the idea that trauma manifests physiologically.
Somatic Experiences: Focuses on body sensations rather than just cognitive or emotional symptoms.
Developed by: Dr. Peter Levine.
Medications for PTSD
SSRIs: Selective serotonin reuptake inhibitors (antidepressants) commonly prescribed for PTSD.
Benefits: Help reduce sadness, worry, anger, and emotional numbness.
Other Medications: Can address specific symptoms like sleep problems and nightmares.
Psychedelics: A promising new avenue for PTSD treatment.
Complex PTSD (C-PTSD)
Definition: Arises from prolonged or repeated traumatic events, such as childhood abuse, torture, or domestic violence.
Symptoms: Includes all PTSD symptoms plus:
Difficulty regulating emotions.
Negative self-image (shame, guilt, feelings of worthlessness).
Difficulty forming and maintaining close relationships.